1. Introduction
Acute chest pain with the suspicion of acute coronary syndrome (ACS) is a common reason for alerting emergency medical services (EMS) with an incidence of 90-312 per 100,000 inhabitants per year in Europe [
1,
2]. The electrocardiogram (ECG) is the diagnostic cornerstone of ACS, especially for the detection of an ST elevation myocardial infarction (STEMI) with an incidence ranging from 44 to 142 per 100,000 inhabitants per year [
1,
3].
Patients with suspected ACS can be a challenge for EMS. Sonification, i.e. in the presented context an auditory representation of the ECG signal, has the potential to play an important role as a new supporting tool for the surveillance of the time course of the ST segment during (out of hospital) care of patients with suspicion of myocardial infarction according to a recent study [
4,
5]. In addition, it has recently been reported on the high accuracy of the sonification-assisted classification of different levels of ST elevations and the accurate discrimination from Non-ST elevation [
6].
Sonification is the reproducible, systematic transformation of data to sound and can be used for process monitoring, data analysis or conveying information [
7]. Thereby, the sonification of biosignals is a sub-area with applications for supporting diagnostics, particularly the rapid detection of transients [
8,
9,
10,
11]. In our context, the ECG is used to be transformed into sounds [
4,
12,
13]. Further examples of biosignal sonifications, mentioned here to illustrate the concept, include the oxygen saturation signal measured by pulse oximetry and the QRS tone. Similar to ST elevation, the QRS tone of the ECG is a particular aspect of a biosignal whose measurement belongs to the standard repertoire of medical methods. In our context, proper auditory representations of ST segments of the ECG can yield a spectrum of sounds that allows an accurate discrimination of isoelectric from elevated ST segments [
5]. The sonifications used for this study were developed and optimized to transfer the information contained in the biosignals to the EMS crew or, more generally, to an evaluator team [
6] and will be described in
Section 3.
By default rhythm disturbances need to be monitored continuously by one to three leads in order to treat pathological cardiac arrhythmias immediately upon occurrence. However, changes of the ST segment are not covered by this method, but are important for the detection of STEMI. In cases of ACS, fluctuating symptoms are often characterized by transient ECG changes [
11]. For these cases, according to the current ESC guidelines [
3], a 12 lead ECG has to be recorded on scene within ten minutes after arrival, but routinely only at one point in time [
3], which poses a risk of misinterpreting transient ECGs. Furthermore, the evaluation result of the ST segment is dependent on the patient’s age and sex, particularly with respect to leads V2 and V3, according to the current ESC guidelines [
3]. It is therefore important to gain expertise and practical skills through intensive training programs in order to ensure correct and timely diagnoses. Particularly, if an ST elevation or other signs of coronary occlusion are present in the ECG, an immediate revascularization is required. Proper treatment includes prompt delivery of medication on scene and urgent heart catheterization. Therefore, optimally the treating hospital should offer 24/7 acute revascularization therapy.
Encouraged by findings of a feasibility study [
5] and evidence for an excellent classification by means of sonification [
6], the hypothesis for the current study was raised: In the presence of a transient STEMI, sonification-assisted diagnosis, when being compared to the standard diagnosis based on a visual ECG-display, reduces the time to diagnosis and increases diagnostic sensitivity in patients with an initially isoelectric ST segment and spontaneously occurring chest pain.
2. Results
2.1. Sonification-Assisted ECG Surveillance Leads to Shortened Time Delay from Onset of STEMI to Reporting of Diagnosis
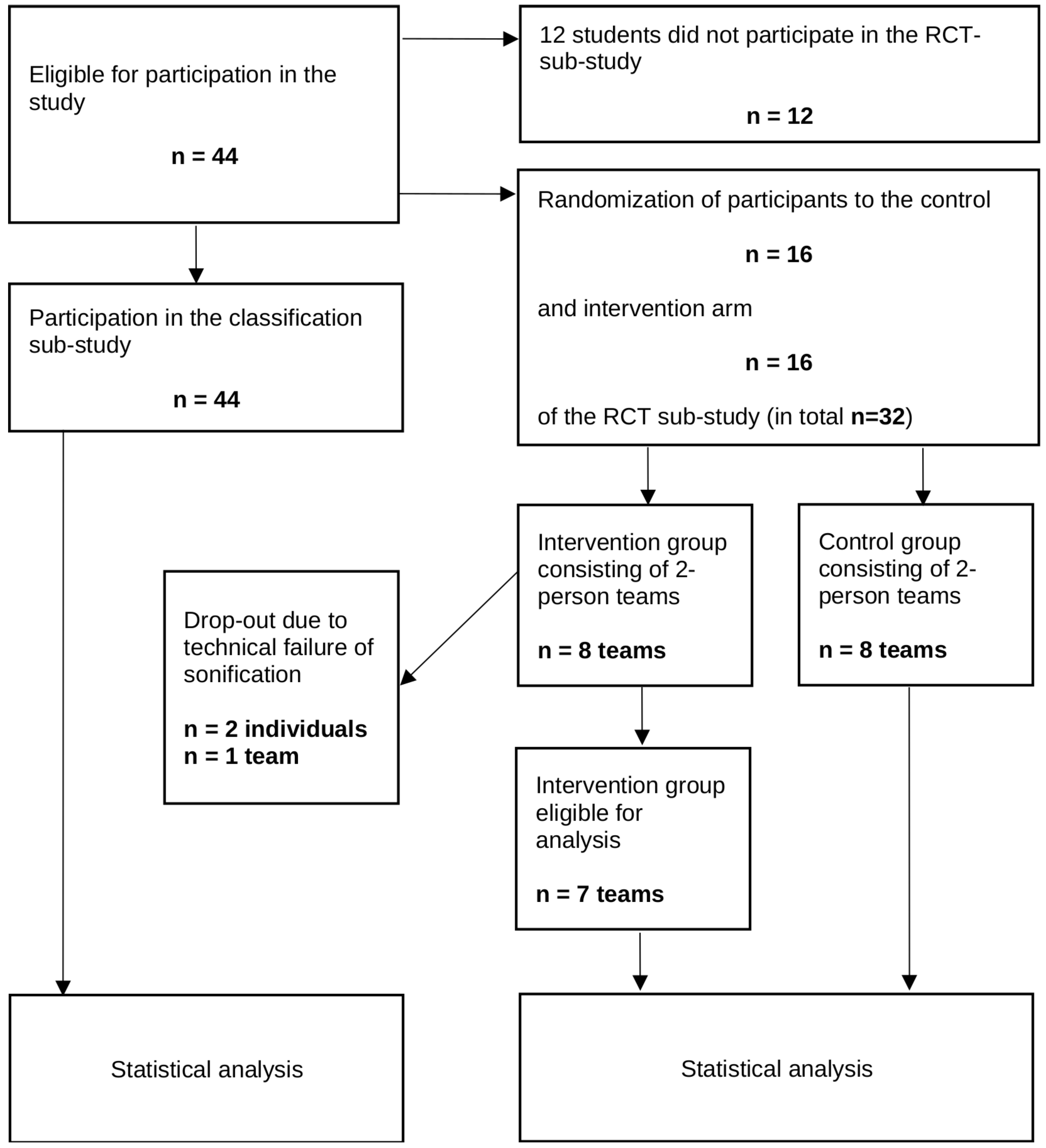
This section is devoted to a quantitative analysis of the difference in outcome between the two emergency training groups being compared. The primary outcome measure is the duration from setting up the first ECG to the appropriate STEMI diagnosis by the training participants. One training team that faced a technical error which prevented sonification is excluded from the analysis because an intention-to-treat procedure makes no sense here due to the possible distortion of the result caused by the failure. Thus, 8 teams of two with classic diagnosis (control) and 7 teams of two with sonification-assisted diagnosis (index group) are compared (see
Figure 1).
Table 1 contains summary statistics for demographic and self-assessment parameters of the evaluable RCT participants. Also contained is the date (measured in days from start of the trial) of the training session. Of note, the summary statistics of date have been calculated on the basis of the 15 training teams of two (8 control and 7 index groups), not on an individual basis to avoid irrelevant duplicates. The summary table is stratified by parameter “sonification” indicating the participation in the intervention or in the control group during the training session and does contain the results of univariable tests which confirm the two groups to be structurally similar with the exception of date showing a relevant difference. Please see the Methods
Section 3 for a detailed description of the covariates.
Table 2 summarizes the outcome variables of the 15 training groups of two, which are the time points of certain actions to be carried out by the students or, where appropriate, the delay times between activities, respectively. Time points of initiation of a first and a second ECG (labelled ECG1 and ECG2) as well as time of diagnosis are reported directly as well as mutual delay times between these events due to the according definitions of the relevant outcome variables. In addition,
Table 2 contains the time points of reporting the diagnosis to the rescue control center and the time points of pharmaceutic and non-pharmaceutic interventions initiated by the participants. The treatment activities are mentioned for descriptive reasons but also because they are relevant for future qualitative and quantitative research questions.
Although correctly randomized, the average dates of the training sessions (cf.
Table 1) differ considerably between the two study arms. Date, therefore, has been considered as confounding variable but did not show a significant effect in an adjusted multivariable regression. However, due to the proper adjustment for date, the effect of the intervention (i.e. sonification) is slightly lowered (main sonification effect
; date effect
).
Time delay from initiation of the first ECG to diagnostic inference is considered to be one of the primary outcomes of the trial.
Table 3 contains the results of a multivariable regression of this outcome on intervention (i.e. sonification), date, and on 8 other independent variables or predictors, i.e. the scores from the survey questionnaires. Although the regression is underpowered according to so many covariates, it still serves to generate hypotheses. Of note, individual scores taken from the questionnaires were summed for the two members of each training group. As the main effect, sonification-assisted diagnosis does have a clinically highly relevant shortening impact on delay time from the start of first ECG to the diagnostic inference, although missing statistical significance (
) in this underpowered regression model. However, none of the characteristics (gender, preknowledge, attitude toward sonification etc) expressed by the covariates was found to significantly alter the delay. Even the significantly better performance of female participants found in the classification study [
6] no longer shows any superiority in this realistic emergency simulation.
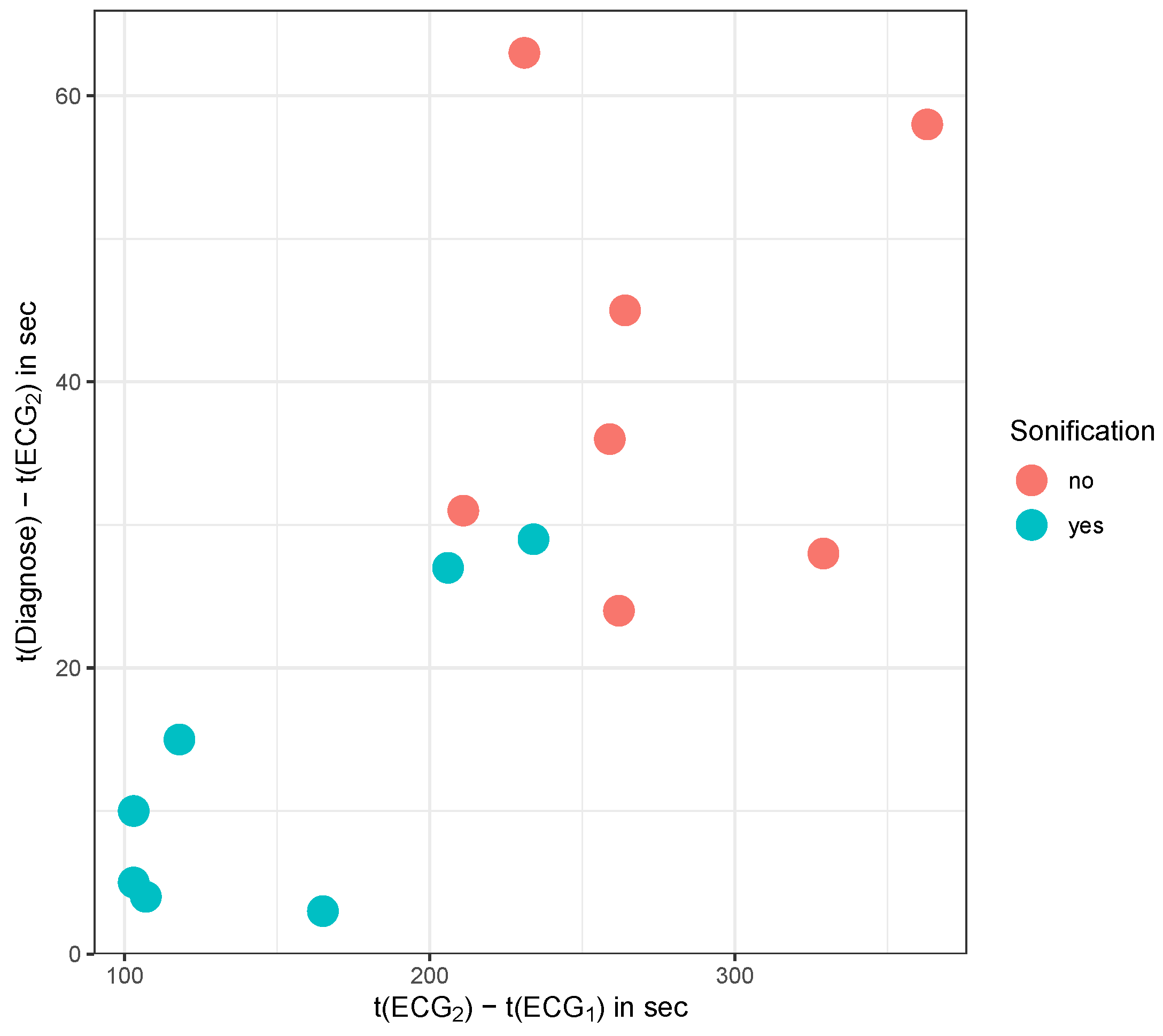
Regressions of the other two outcomes (delay between ECG1 and ECG2, delay between ECG2 and diagnosis) on the same predictors lead to similar inferences, which is why we refrain from showing the full regression tables. However, one small peculiarity can be observed. As observed with respect to classification (cf. [
6]), Q4 actually does unfold a marked impact (
on the delay time between ECG2 and diagnosis. In line with previous findings [
6], we conclude that a general stress-free attitude towards emergency situations correlates with an improved outcome. Finally, the delays from ECG1 to ECG2 and the delays from ECG2 to diagnosis are strongly correlated with Pearson’s correlation coefficient turning out to be
(see
Figure 2).
Thus, it can be concluded that sonification reduces both the delay time from ECG1 to ECG2 and the subsequent duration from ECG2 to STEMI diagnosis. The total duration from ECG1 to diagnosis differs significantly between index and control group. A weak impact of psychological conditions on the duration from ECG2 to diagnosis can be observed. The trial has not been powered to reveal a multiple impact of covariates, therefore, the results point to trends to be validated in larger trials.
2.2. Sub-Group Analysis Indicates a Match Between Perceived and Actual Benefit of Sonification
Only participants in the sonification group have been asked sonification-specific questions FB3-FB7. A regression of the delay time between ECG2 and diagnosis on these 5 scores results in estimates listed in
Table 4. Thereby, FB7 was omitted because the corresponding coefficient cannot be estimated due to the low variability of this covariate.
A positive attitude toward sonification (FB5, FB6) does influence delay time, however the effects go in different directions. An increasing disagreement with the statement that “sonification was helpful in making the diagnosis” (FB5) did significantly () increase the delay time, i.e. considerably worsens the performance during the emergency scenario. To the contrary, disagreeing with “I conceive the sound of sonification as pleasant” (FB6) appears to counterintuitively significantly () decrease delay time (improves performance).
We refrain from showing the estimates of regressions for the other delay variables since none of them show significant dependence of the outcome on scores FB3 to FB7, however the effects of FB5 and FB6 appear to go into the same directions. We conclude with due caution, that the second delay (between ECG2 and diagnosis) is somewhat increased as a consequence of a pleasant attitude towards sonification which may point to an increased sovereignty that gives rise to a watch-and-wait strategy thus mediated. Of note, there is no effect of date observable within this subgroup analysis. These preliminary findings of this sub-group analysis have to be addressed in suitably designed follow-up studies.
3. Material and Methods
3.1. ST Elevation Sonification of ECG Signals
Sonification is a versatile technique of converting measured (temporal) signals into acoustic signals and the sonification method can be tuned to support different goals such as exploratory data analysis, diagnosis, sensitivity to changes in monitoring or classification. For the ECG application, sonification methods can be defined to enhance detection of cardiac arrhytmia, heart rate variability, discrimination of cardiac pathologies or specific aspects such as ST elevation. To target the latter aspect, a sonification method is required that is specifically designed to convey patterns related to ST elevation/suppression. A set of designs has been discussed in [
6] and one of it has been selected for further evaluation, briefly summarized in the following.
In emergency situations, two main demands on the sonification design compete, namely the clear salience of physiologically significant features and the suppression of intrusive noises. Therefore, design criteria and validation have been based on expert reviews involving sonification interface designers, clinical partners and non-clinical colleagues with different expertises. Key criteria for selecting the appropriate design and setting have been comprehensibility, dominant perceptual quality, aesthetics/pleasantness, memorizability, compatibility with environmental sounds, backgrounding and saliency, and universality. Subsequently, the instantaneous auditory representation of each electrical cardiac activity and the distributed representation have been combined and adaptively tuned until an acceptable target representation was achieved.
The sonification method finally chosen is a so called event-based parameter-mapping sonification in which features, such as the ST elevation in all 12 leads of the ECG in this case, are extracted and properly mapped on parameters of a sound generator to create structured non-verbal audio signals. These signals are presented along with the QRS-tone of the pulse oximeter to enrich the already available carrier of information with task-specific details. Thus, an ST elevation sonification method was conceived, developed, and tested as described in full in [
6]. Various designs are described there, of which a design called “Grouped Lead Scans” was selected for this study with mappings defined as following:
From the 12 lead ECG, two lists of each 6 voltages derived from the leads are defined. List L1: , and list L2: . For each lead, the corresponding ST segment value, , is estimated and assigned to one of 5 levels according to the following cutoff rule: (s2) strongly suppressed, i.e. , (s1) moderately suppressed, i.e. , (IE) close to isoelectric with , (e1) moderately elevated, i.e. , (e2) strongly elevated, i.e. .
A sequence of short pitched tones (duration
d, fundamental frequency
f) of given brightness (number of harmonics
n) and level (
l, in
) is generated for both sets L1 and L2 using an inter-tone interval of
. The tones are pitched relative to the pitch
of the QRS tone by (
) semitones corresponding to the 5 cases (s2, s1, IE, e1, e2). The duration
d is set to
according to the 5 cases such that more extreme ST segment values become more salient. Correspondingly, brightness is defined by using
harmonic overtones, such that ST segments which deviate clearly from IE perceptually stand out. Further, each tone’s level is adjusted by
accordingly. Finally, we use
to control the curvature of the corresponding tone’s fade-out envelope such that tones for more extreme st values have a less steep fade out (cf. [
6] for details).
The structured audio message (sequence of 6 tones) for set L1 is triggered by every 8th electrical cardiac activity QRS tone. The sequence for set L2 is triggered two electrical cardiac activities after the L1 sequence, such that both sets of 6 notes can be easily discerned. Listeners thus receive adequately detailed yet aggregated information of the 12 lead ST segment values via two packets of 6 tones, the first for the limb leads along the inverse Cabrera circle with inverted aVR as -aVR, the second for the precordial leads from V1 to V6.
For the stimuli used in the study, we used the Laerdal™Resusci Anne
® Advanced SkillTrainer system with a pulse rate of
, and oxygen saturation resulting in QRS tones of fundamental frequency
. Note that the ST-tone’s frequencies
f for any given reference frequency
and semitone offset
k is computed by frequency
. Audio examples for several STEMI classes, specifically for an ECG with normal ST segments, anterior STEMI (weak, moderate, severe) and inferior STEMI (weak, moderate, severe) are provided as supplementary material in a previous publication [
6], where the results of an expert evaluation process and of a classification study is presented.
3.2. Study Protocol
3.2.1. Overview
The overall study, the second part of which is discussed here, was designed as a two-part emergency training program, with the first part focusing on the correct classification of different ST elevations based on the acoustically presented ECGs. The second part was designed as a randomized control trial (RCT) in which two groups of students underwent a rescue scenario in a realistic emergency simulation either using the standard diagnostic method (control arm) or with sonification support (intervention arm). The compelling results of the first part of the study, the classification part, which preceded the RCT, have recently been published [
6] and provided the highest level of evidence to justify the RCT. Moreover, since all students participating in the RCT also participated in the preceding classification part, it also served as a preparatory unit and should therefore also be recapitulated here briefly.
As part of the study, basic epidemiological parameters had been collected and questionnaire-based surveys were carried out. A first survey regarding self-ratings based on a 5-point Likert scale of previous experience with emergency situations and musical expertise, as well as questions concerning the general attitude toward sonification took place before the two main parts of the study (classification study and RCT, respectively). A second survey was carried out after the training program (the RCT). Specifically, within the intervention arm only, the second survey addressed the assessment of sonification during the emergency training session (cf. paragraph below for the questionnaires).
3.2.2. Participants
After the complete requirements of the ethics committee were met on 23/01/2023, data acquisition began, which ended in 06/2023. The entire study cohort consisted of 44 students from the faculty of medicine of the Ruhr University Bochum (RUB) in Germany (9th and 10th semester) who were assigned to a three day training program in emergency medicine. The emergency simulations took place in groups of two over the study period. All students received a 10-minute review about diagnosing and treating ACS in pre-hospital care. Since sonification of ST segments is a method previously unknown in practice, the students were given an introduction to this novel methodology, particularly with respect to ECG sonification. To this end, all participants received a
introduction video about sonification, its support of ECG monitoring and the motivation of our research. As part of the introduction we presented audio examples of ECGs either in isoelectric mode or with significant elevation of the ST segment to the students. Results of a previous study, which formed the basis for the aforementioned introduction, have recently been published [
6].
The local ethics committee of the Ruhr University Bochum, situated in Bad Oeynhausen, Germany gave approval (file no.: 2022-1017). The study followed the principles of Helsinki. Informed consent was obtained from all participants.
3.2.3. Classification Task
Before the simulation study, all 44 students participating in the entire training program took part in a classification study, the results of which have recently been published [
6] and are briefly summarized in the following. Regarding the classification of sonified ECG sequences, discrimination of IE (the healthy class) from all other (STEMI) classes yielded both a perfect specificity and a perfect sensitivity of 1 within 660 classification instances. With respect to the exact classification of all 5 classes (IE, inferior/anterior, and moderate/severe STEMI) an overall accuracy of 0.82 (0.79, 0.85) and an intraclass coefficient of
was estimated. Female students performed significantly better than male. The performance significantly improved in the course of the presentation of three similar classification tasks. This excellent result led to raise the hypothesis that sonification is also superior to standard diagnosis in practical EMS operation. As this classification task preceded the RCT, it must also be understood as part of the preparation for the emergency simulation, particularly with respect to the intervention arm. However, structural equality of the two study arms is ensured, as all students completed the classification task.
3.2.4. Survey to Determine Relevant Self-Assessments and Attitudes
At the beginning of the study, questionnaire-based surveys were carried out. The resulting self-assessments and attitudes are partly included as independent variables in regressions to determine the effectiveness of sonification in a realistic emergency setting. On the other hand, they are listed here for the sake of completeness. A first survey regarding score-based self-assessments of previous experience with emergency situations and musical expertise, as well as questions concerning the general attitude toward sonification took place before the study was carried out. Specifically we asked for subject’s agreement with the following statements on a Likert scale from 1 (not at all) to 5 (completely agree):
Q1: I had experience with pre-clinical emergencies
Q2: I have participated to more than 3 emergency trainings
Q3: I feel confident when handling emergency situations
Q4: For me, emergency situations cause negative stress
After the perception test, but before the scenario study, which is the focus below, we asked for subject’s agreement based on the same Likert scale as above with the following 3 statements:
SQ1: Sonification is pleasant to listen to
SQ2: The sonification is informative, i.e., it enables to identify ST elevation changes in the ECG
SQ3: I can imagine to listen to these sonifications for a longer time period
3.2.5. Simulated Medical Emergency Scenario
The randomized controlled simulation study (sonification as the intervention) investigated the use of sonification under more realistic conditions within the context of an emergency medical scenario with the task to detect an ACS. Thirty-two participants have been randomly assigned by means of a balanced envelope randomization method to either the intervention or the control group such that both study arms each consisted initially of eight teams of two.
When planning the sample size, a realistic expected size of the student cohort of at least , i.e. teams of two per study arm, was assumed. Due to the conceptual difference in diagnostic information processing, given the continuous signal transmission, we assumed a huge effect size, however, set a somewhat more moderate value for the power analysis with an effect size of 1.25. Under these conditions, a two-sided t-test with a significance level of 0.05 yields a power of 0.76, which is sufficient for an exploratory study. With the actual number of cases of 8 per study arm, the minimum requirement for an exploratory study was still met, especially since the expected effect size was chosen to be rather moderate.
Both groups recorded a 12-lead ECG according to the current ESC guidelines, whereby the ECG signals were also presented audibly based on sonification of key properties of ST segments in the intervention group. Initially, the ECG had no evidence of ST elevation. Ninety seconds later the mannequin mentioned additional symptoms (chest pain and dyspnea) which were suggestive to the development of a STEMI and, therefore, should indicate a recording of a second 12-lead ECG. The second ECG presented an anterior STEMI, whereby, as with the first ECG, the second ECG in the intervention group was also presented with sonification.
The primary endpoint was the time gap from the first ECG to the establishment of the correct STEMI diagnosis. The time gap from the second ECG to the establishment of the correct diagnosis served as a secondary endpoint within a subgroup analysis of the intervention arm only. The mutual time delays between the two ECGs, as well as between all major actions (ECG1, ECG2, diagnostic inference, start of treatment, report to rescue control center) carried out serve as secondary endpoints.
Despite the randomized assignment, structural differences in prior knowledge and previous experience can have an impact on the outcome. Therefore, additional relevant parameters were collected via a questionnaire for an adjustment of confounders. Additional questions were asked to determine relevant predictors of performance within the intervention arm. Assessment results on hearing quality, positive benefit, and the impact on the own behavior serve as predictors for a qualitative assessment of the sonification-assisted emergency setting in terms of a subgroup analysis.
Due to a technical failure of the sonification equipment, one team dropped out of the intervention arm, leaving
intervention teams eligible for the analysis. The complete flow chart of the entire study, including the classification task, is depicted in
Figure 1.
3.2.6. Medical Scenario Description
The simulated medical scenario depicted in
Figure 3 involved a sixty-six-year-old male patient who called the EMS with left chest pain that had persisted for about an hour and was accompanied by nausea and malaise. In other words, he exhibited a number of symptoms that required attention from the EMS.
As mentioned, each emergency team consisted of two medical students. The patient was represented by the Laerdal™Resusci Anne® Advanced SkillTrainer. No other persons were actively involved. The information (patient’s voice) was provided by one of the supervising tutors from the “background”. The scenario took place in a training center where a patient’s apartment was simulated. Before the actual scenario started, each team received a brief introduction and was informed about the patient’s symptoms and basic data (name, age, gender). The test subjects had a maximum of 13 minutes to complete the case study.
The emergency equipment consisted of an emergency suitcase, a suction pump, an oxygen bottle and a patient monitor/defibrillator device (Lenovo ThinkPad with Laerdal-Patient-Monitor-Software).
3.2.7. Medical Assessment
For diagnosis and care, the emergency team should carry out the following measurements and had to perform a series of tasks:
establishment of basic monitoring (blood pressure measurement, oxygen saturation, 4-lead ECG) for measuring vital parameters
recording of a 12-lead ECG (initially presented with an isoelectric ST segment)
recording of a second ECG (now presented with significant elevation of the ST segment 90 seconds after the first ECG, indicative for an anterior STEMI)
recognizing the ST elevation (myocardial infarction)
correct selection and application of the indicated drugs
report to the rescue control center and referring the patient to the nearest appropriate hospital with the option of immediate cardiac catheterization
After establishing the ECG measurement device (i.e. after properly attaching all electrodes) the ECG signal corresponding to a healthy ECG with isoelectric ST segment was visually displayed to all teams, additionally within the intervention arm simultaneously by sonification.
Ninety seconds after the start of the measurement, the ECG turned into an ST elevated ECG signal on the cardiac monitor and, applicable for the intervention group only, the sonification changed into an auditory signal corresponding to the ST elevated ECG. Upon request, the patient expressed that the symptoms which initiated the emergency call worsened.
As a consequence of these changes in conditions, the medical team was expected to recognize the ST elevation, correctly select and apply the indicated drugs, pre-announce and admit the patient to an appropriate hospital.
3.2.8. Assessment of the Scenario by the Study Participants
After finishing the simulated medical scenario, the participants were asked to complete a second questionnaire. Using a 5-point Likert scale from one (1) corresponding to “strongly agree” through five (5) corresponding to “strongly disagree”, the following statements had to be assessed (FB3 through FB7 intervention group only):
FB1: I acted confidently during the emergency simulation
FB2: I felt stressed during the emergency simulation
FB3: Sonification influenced my individual medical performance
FB4: Sonification provided a sense of security
FB5: Sonification was helpful in making the diagnosis
FB6: I conceived the sound of the sonification as pleasant
FB7: The use of sonification as a supporting tool in everyday life is conceivable
3.3. Statistical Methods
A multivariable linear regression is used to compare the performance of the two study groups (sonification-assisted versus traditional diagnosis as described above). Primary outcome is the time delay from start of the first ECG recording until diagnostic inference. In addition, the delay between the two ECG recordings is conceived as a secondary outcome. Correlations between the delays are reported using Pearson’s coefficients and graphically depicted. In a sub-group analysis applied only to the sonification group, the effect of rating the usefulness of sonification and other self-assessment parameters on the outcome is evaluated.
Univariable 2-sample comparisons are based on t-tests for metric data and Fisher’s exact test or chi-squared test for categorical data. Significance level is chosen to be 5% and precision is reported using 95%-confidence intervals.
Statistical analyses and creation of graphs and tables were carried out with statistical programming language R [
14].
4. Discussion
Sonification, i.e. the transformation of data into sound, can serve many different purposes [
8]. For example, for blind persons, it opens up opportunities to perceive events that would otherwise remain hidden from them. Here we discussed an application in medical diagnostics that is essentially intended to lower the cognitive load of the medical staff, particularly in stressful situations. Instead of directly addressing the cognitive load, we followed best practice principles of evidence based medicine and used a patient relevant outcome: delay time from starting the diagnostic procedure to the final establishment of the diagnostic result.
We applied sonification as a monitoring instrument in EMS, specifically to assess the dynamics of ST segment elevations and detect their pathological manifestations. On the one hand, it has been discussed earlier that an auditory display of temporal signals is particularly appropriate to detect dynamically changing patterns in these signals due to the according sensitivity of the ear [
8]. On the other hand, the acoustic perception is known to be more strongly coupled to the limbic system when being compared to the visual perception [
15], which is why sonification might be conceived as a less objective epistemic instrument. However, this emotional component may even turn into an advantage in emergency situations. Obtaining meaningful information in this respect, ultimately in order to optimize the acoustic design, was subject of numerous earlier publications (e.g. [
8,
9,
10,
12]) and this objective was also pursued in the present work. We addressed emotional and perceptional aspects by conducting accompanying surveys in order to model the resulting scores for various attitudes as influencing factors. The exact significance of the observed dependencies of the scores on the outcomes with respect to the improvement of the sonification design should be determined in follow-up studies, which should also be designed to optimize the emergency training sessions.
To our knowledge, our study is the first RCT to address the superiority of a sonification-assisted diagnosis compared to a visually-based standard diagnosis and to yield a significant result in a realistic emergency scenario. No doubt, every second it takes to derive the final STEMI diagnosis within the scope of an EMS counts. The effect is considerably large, such that it gained statistical significance despite adjustments for confounders and a small samples size.
5. Limitations and Conclusions
The present study is based on a relatively small sample size. Nevertheless, due to a strong average population effect, it was even possible to adjust for date as a possible confounder while preserving the significance and even take additional predictors into account and still achieve a convincing result with regard to the main effect. Overall power suffered from the unexpectedly unbalanced temporal allocations to the two study arms, which necessitated a correction for the start time of the training sessions in order to correct a possible bias through different learning gains in the two groups. Future studies, therefore, should consider stratified randomization. Moreover, the study was not sufficiently powered to obtain significant results with respect to the impact of individual characteristics that may influence the outcome within the sonification group. However, predictors with a relevant influence on the outcome (reduction of the time needed to achieve the diagnosis) were identified, even if these were below the significance threshold. The impact of individual attitudes toward sonification in general and self-confidence in emergency situations, to name but a few, provide very valuable information for improving sonification design parameters and this was indeed one of the intentions of the study presented.
With regard to a possible application in real emergency operation, the most significant limitation of the present study is given by the preliminary, ethically necessary restriction to a simulated emergency situation for medical training. To conclude, the compelling advantage of sonification-assisted STEMI diagnosis now provides sufficient evidence for the ethical and medical justification of an RCT in real-world settings.
Author Contributions
JT: Conceptualization, Methodology, Supervision, Formal Analysis, Investigation, Data Collection and Interpretation, Writing; FT: Conceptualization, Methodology, Formal Analysis, Investigation, Data Collection and Interpretation, Writing; SG: Methodology, Conceptualization, Supervision, Writing; JP: Resources, Data Collection and Interpretation, Writing; HHD: Formal Analysis, Methodology, Interpretation, Writing; TW: Supervision, Formal Analysis; TH: Conceptualization, Methodology, Supervision, Software, Formal Analysis, Investigation, Writing; All authors discussed the results and contributed to the final manuscript.
Institutional Review Board Statement
The local ethics committee of the Ruhr University Bochum, situated in Bad Oeynhausen, Germany gave approval (file no.: 2022-1017). The study followed the principles of Helsinki. Informed consent was obtained from all participants.
Informed Consent Statement
The publication rights of text and all figures are held by the authors. All authors read the final version of the manuscript and gave consent for publication.
Data Availability Statement
Sonification related materials have been published as open access supplementary documents to [
6].
Acknowledgments
We dedicate this article to our late mentor and supervisor Jochen Hinkelbein, who passed away shortly before the publication was finalized due to a tragic accident.
Conflicts of Interest
There are no competing interests. The authors have no relevant financial or non-financial interests to disclose.
References
- Widimsky, P.; Wijns, W.; Fajadet, J.; de Belder, M.; Knot, J.; Aaberge, L.; Andrikopoulos, G.; Baz, J.A.; Betriu, A.; Claeys, M.; et al. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. European Heart Journal 2010, 31, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Eckle, V.; Lehmann, S.; Drexler, B. Prehospital management of patients with suspected acute coronary syndrome. Med Klin Intensivmed Notfmed 2021, 116, 694–697. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- Aldana Blanco, A.L.; Grautoff, S.; Hermann, T. ECG sonification to support the diagnosis and monitoring of myocardial infarction. Journal on Multimodal User Interfaces 2020, 14, 207–218. [Google Scholar] [CrossRef]
- Aldana Blanco, A.L.; Hermann, T.; Tiesmeier, J.; Persson, J.; Grautoff, S. Sonfication enables continuous surveillance of the ST segment in the electrocardiogram. American Journal of Emergency Medicine 2022, 58, 286–297. [Google Scholar] [CrossRef] [PubMed]
- Hermann, T.; Grautoff, S.; Tielking, F.; Persson, J.; Diebner, H.H.; Tiesmeier, J. ST Elevation Sonification of a 12-Lead ECG for the Assessment, Diagnosis, and Monitoring of ST Elevation Myocardial Infarction. Sensors 2025, 25. [Google Scholar] [CrossRef] [PubMed]
- Hermann, T. Taxonomy and Definitions for Sonification and Auditory Display. In Proceedings of the Proceedings of the 14th International Conference on Auditory Display (ICAD 2008); Susini, P., Warusfel, O., Eds.; Paris, France, 2008. [Google Scholar]
- Hermann, T.; Hunt, A.; Neuhoff, J.G. (Eds.) The Sonification Handbook; Logos Publishing House: Berlin, Germany, 2011; pp. 1–586. [Google Scholar]
- Mihalas, G.; Andor, M.; Tudor, A.; Paralescu, S. Can Sonification Become a Useful Tool for Medical Data Representation? Stud Health Technol Inform 2017, 245, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Iliev, I.; Tabakov, S.; Petrova, G. Audio-Conversion of Biomedical Signals - A Possible Approach to Improve Remote Monitoring of Elderly and Visually Impaired People. Stud Health Technol Inform 2023, 306, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Reindl, M.; Lechner, I.; Reinstadler, S.J.; Metzler, B. Transient STEMI – No STEMI at all? International Journal of Cardiology 339, 12–13. [CrossRef] [PubMed]
- Kather, J.N.; Hermann, T.; Bukschat, Y.; Kramer, T.; Schad, L.R.; Zöllner, F.G. Polyphonic sonification of electrocardiography signals for diagnosis of cardiac pathologies. Scientific Reports 2017, 7, 44549. [Google Scholar] [CrossRef] [PubMed]
- Krasteva, V.; Iliev, I.; Tabakov, S. Application of Convolutional Neural Network for Decoding of 12-Lead Electrocardiogram from a Frequency-Modulated Audio Stream (Sonified ECG). Sensors 2024, 24. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024. [Google Scholar]
- Frühholz, S.; Trost, W.; Grandjean, D. The role of the medial temporal limbic system in processing emotions in voice and music. Progress in Neurobiology 2014, 123, 1–17. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).