Submitted:
01 September 2025
Posted:
02 September 2025
You are already at the latest version
Abstract
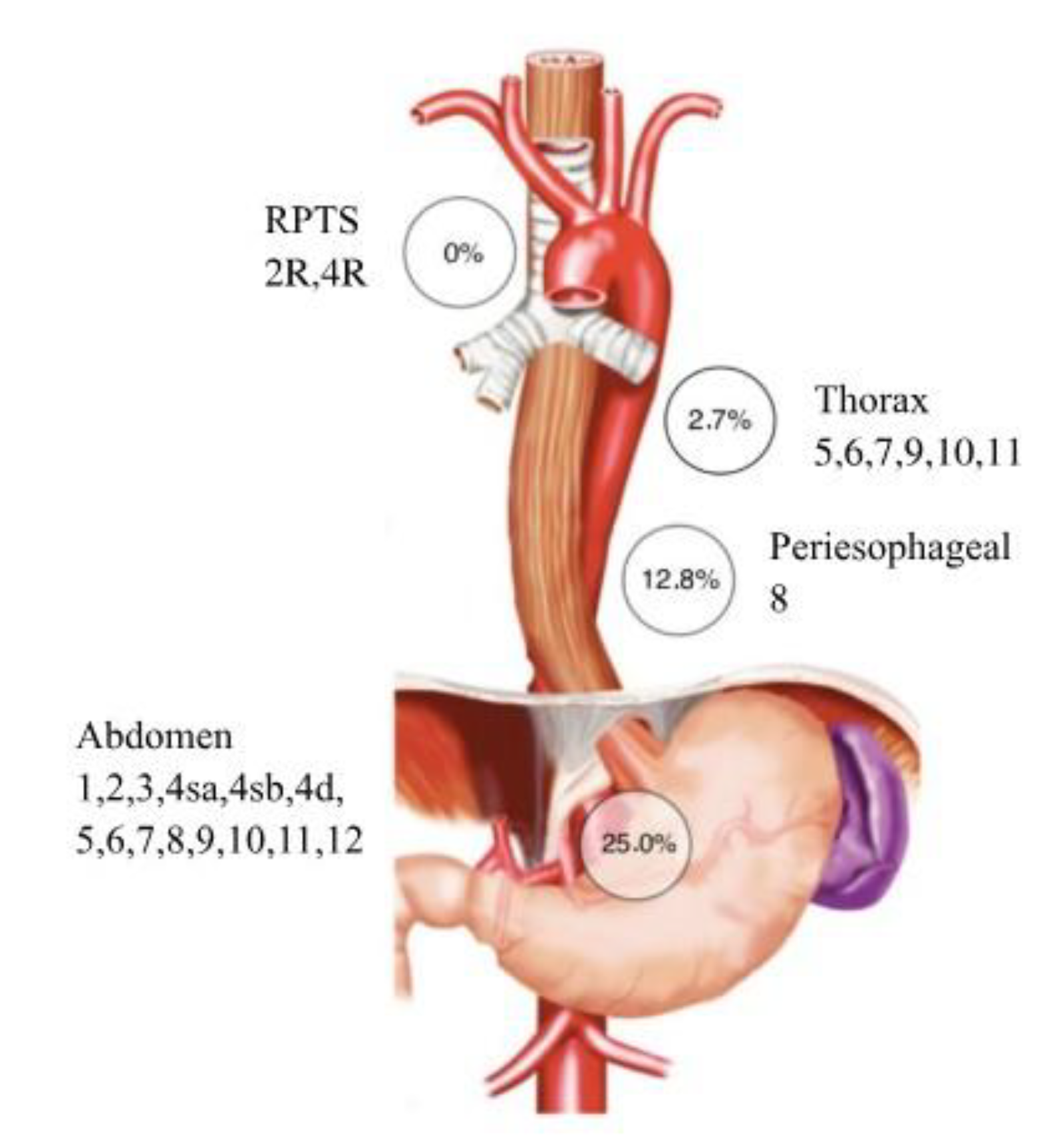
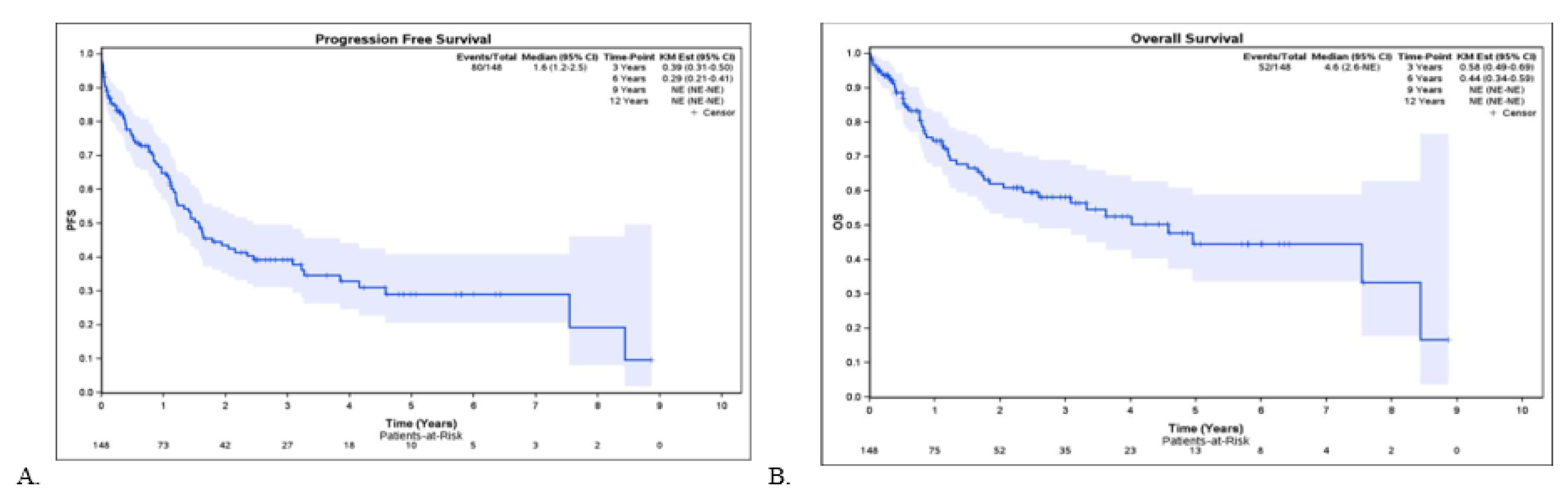
The benefit of extensive lymphadenectomy including the right paratracheal station (RPTS) in the upper mediastinum for esophagogastric junction (EGJ) adenocarcinoma remains controversial. Upper mediastinal lymph node (LN) involvement has been associated with esophageal invasion length, representing a potential research area. This study aimed to assess the rate of RPTS LN involvement in EGJ adenocarcinoma and its correlation with esophageal invasion length, as well as potential impacts on survival and postoperative complications. Patients undergoing two- or three-field esophagectomy with lymphadenectomy extended to the RPTS between 2006 and 2023 were retrospectively included. Patient, tumor, operative, and postoperative data were collected. Among 321 esophagectomies, 147 met inclusion criteria. Median esophageal invasion length was 3 cm. No patients (0%) had LN metastasis in the RPTS, regardless of invasion length (>4 cm or ≤4 cm). Postoperative complications occurred in 41.5% of patients, most commonly weight loss >10% (29.2%), pleural effusion (21.1%), and infectious pneumonitis (19.7%). Five-year overall and disease free survival rates were 44% and 29%, respectively. Our findings suggest that extending lymphadenectomy to the right paratracheal space fails to detect lymph node invasion in patients with esophageal invasion greater than or less than 4 cm in patients with esophageal adenocarcinoma.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Clinical Data and Study Objectives
2.3. Lymphadenectomy
3. Results
3.1. Study Population
3.2. Pathology Lymph Node staging, RPTS Status, and Outcomes
3.3. Postoperative Complications
Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA : A Cancer Journal For Clinicians [Online]. Feb 4, 2021; 71(3): 209-49. Available at. [CrossRef]
- 2024.
- Zhang, Y. Epidemiology of esophageal cancer. World Journal Of Gastroenterology [Online]. Jan 1,2013; 19(34): 5598. Available at. [CrossRef]
- Uhlenhopp D, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clinical Journal Of Gastroenterology [Online]. 23 Sep 2020; 13(6): 1010-21. Available at. [CrossRef]
- Obermannová RL, Leong T. ESMO Clinical Practice Guideline interim update on the treatment of locally advanced oesophageal and oesophagogastric junction adenocarcinoma and metastatic squamous-cell carcinoma. ESMO Open [Internet]. 2025 Feb 1;104134. Available at. [CrossRef]
- Chevalier. B. Respiratory complication of trans-thoracic esophagectomies for cancer [Thesis]. Bordeaux (FR): Université de Bordeaux; 2004 Oct 9. Available at :https://dumas.ccsd.cnrs. 0108.
- Mariette C, Piessen G, Briez N, Triboulet J. The Number of Metastatic Lymph Nodes and the Ratio Between Metastatic and Examined Lymph Nodes Are Independent Prognostic Factors in Esophageal Cancer Regardless of Neoadjuvant Chemoradiation or Lymphadenectomy Extent. Annals Of Surgery [Online]. Feb 1, 2008; 247(2): 365-71. Available at. [CrossRef]
- Lerut T, Coosemans W, Decker GA, De Leyn P, Moons J, Nafteux P, et al. Surgical techniques. Journal Of Surgical Oncology [Online]. 18 Nov 2005; 92(3): 218-29. Available at. [CrossRef]
- Kurokawa Y, Hiki N, Yoshikawa T, Kutsukake K, Ito Y, Ohi M, et al. Mediastinal lymph node metastasis and recurrence in adenocarcinoma of the esophagogastric junction. Surgery [Online]. , 2015; 157(3): 551-5. Available at, 1 March. [CrossRef]
- Kurokawa Y, Takeuchi H, Doki Y, Mine S, Terashima M, Yasuda T, et al. Mapping of Lymph Node Metastasis From Esophagogastric Junction Tumors. Annals Of Surgery [Online]. , 2019; 274(1): 120-7. Available at, 8 August. [CrossRef]
- Kitagawa Y, Ishihara R, Ishikawa H, Ito Y, Oyama T, Oyama T, et al. Esophageal cancer practice guidelines 2022 edited by the Japan Esophageal Society: part 2. Esophagus [Online]. , 2023; 20(3): 373-89. Available at, 30 March. [CrossRef]
- Mann C, Berlth F, Hadzijusufoviç E, Tagkalos E, Uzun E, Codony C, et al. Extended lower paratracheal lymph node resection during esophagectomy for cancer – safety and necessity. BMC Cancer. 2022 ;22(1). Available at, 24 May. [CrossRef]
- Anderegg M, Lagarde SM, Jagadesham VP, Gisbertz SS, Immanuel A, Meijer SL, et al. Prognostic significance of the location of lymph node metastases in patients with adenocarcinoma of the distal esophagus or gastroesophageal junction. Ann Surg. 2016 Nov 1;264(5):847-53. [CrossRef]
- Mine S, Sano T, Hiki N, Yamada K, Nunobe S, Yamaguchi T. Lymphadenectomy around the left renal vein in Siewert type II adenocarcinoma of the oesophagogastric junction. Br J Surg. 2012 Nov 23;100(2):261-6. Available at. [CrossRef]
- Matsuda T, Kurokawa Y, Yoshikawa T, Kutsukake K, Misawa K, Ohi M, et al. Clinicopathologicalcharacteristics and prognostic factors of patients with Siewert type II esophagogastric junction carcinoma: A retrospective multicenter study. World J Surg. 2016 Feb 29;40(7):1672-9. Available at. [CrossRef]
- Kurokawa Y, Hiki N, Yoshikawa T, Kutsukake K, Ito Y, Ohi M, et al. Mediastinal lymph nodemetastasis and recurrence in adenocarcinoma of the esophagogastric junction. Surgery. 2015 Mar :1;157(3):551-5. Available at. [CrossRef]
- Luo P, Chen X, Yang Y, Zhang R, Kang X, Qin J, et al. Lymph node metastases in middle and upper mediastinum of Siewert type II adenocarcinoma: A real-world retrospective study. Cancer Med. 2024 Feb1;13(4). Available at. [CrossRef]
- Yamashita H, Seto Y, Sano T, Makuuchi H, Ando N, Sasako M. Results of a nationwide retrospective study of lymphadenectomy for esophagogastric junction carcinoma. Gastric Cancer. 2016 Oct 28;20(S1):69- 83. Available at. [CrossRef]
- Parry K, Haverkamp L, Bruijnen R, Siersema PD, Ruurda JP, Van Hillegersberg R. Surgical treatment of adenocarcinomas of the gastro-esophageal junction. Ann Surg Oncol. 2014 Sep 5;22(2):597-603. Available at. [CrossRef]
- D’Journo XB, Doddoli C, Michelet P, Loundou A, Trousse D, Giudicelli R, et al. Transthoracicesophagectomy for adenocarcinoma of the oesophagus: standard versus extended two-field mediastinal lymphadenectomy? Eur J Cardiothorac Surg. 2005 Apr 1;27(4):697-704. Available at. [CrossRef]
- Hulscher JBF, Van Sandick JW, De Boer AGEM, Wijnhoven BPL, Tijssen JGP, Fockens P, et al. Extended Transthoracic Resection Compared with Limited Transhiatal Resection for Adenocarcinoma of the Esophagus. New England Journal Of Medicine/The New England Journal Of Medicine [Online]. 21 Nov 2002b; 347(21): 1662-9. Available at. [CrossRef]
| n = 147 | |
|---|---|
| Age, yr Median (range) |
69.0 (64.0-75.0) |
| Sex Male Female |
129 (87.8%) 18 (12.2%) |
| Tumor size*, cm Median (range) |
2.7 (1.8-4.5) |
| Length of the esophageal involvement*, cm at endoscopy Median (range) |
3.0 (1.5-5.0) |
| Patients with esophageal length involvement < 4 cm ≥ 4 cm Unknown |
53 (36.1%) 38 (25.9%) 56 (38.1%) |
| Tumor epicenter Siewert I Siewert II Siewert III Unknown |
55 (37.4%) 43 (29.3%) 9 (6.1%) 40 (27.2%) |
| Clinical Tumor stage (cT) Tx T0 T1 T2 T3 T4 |
2 (1.4%) 0 (0.0%) 17 (11.6%) 29 (19.7%) 96 (65.3%) 3 (2.0%) |
| Clinical Node stage (cN) Nx N0 N1 N2 N3 |
11 (7.5%) 47 (32.0%) 74 (50.3%) 13 (8.8%) 2 (1.4%) |
| Clinical Metastasis stage (cM) Mx M0 M1 |
106 (72.1%) 41 (27.9%) 0 (0.0%) |
| Neoadjuvant treatment Yes No |
118 (80.3%) 29 (19.7%) |
| TRG (patients with neoadjuvant treatment) Grade 1 Grade 2 Grade 3 Grade 4 Grade 5 Not assessed |
15 (10.2%) 18 (12.2%) 26 (17.7%) 31 (21.1%) 7 (4.8%) 21 (14.3%) |
| Invasion at pathology Lymphatic Vascular Nerve Unknown |
56 (38.1%) 22 (15.0%) 36 (24.5%) 33 (22.4%) |
| Surgical techniques Two- field: Laparo-thoracic approach Three- field: Laparo-thoraco-cervical approach |
140 (95.2%) 7 (4.8%) |
| Type of resection R0 R1 R2 Unknown |
127 (86.4%) 19 (12.9%) 0 (0.0%) 1 (0.7%) |
| Pathological T stage (pT) Tx T0 T1 T2 T3 T4 |
2 (1.4%) 0 (0.0%) 42 (28.6%) 24 (16.3%) 65 (44.2%) 14 (9.5%) |
| Pathological N stage (pN) Nx N0 N1 N2 N3 |
2 (1.4%) 76 (51.7%) 32 (21.8%) 19 (12.9%) 18 (12.2%) |
| Pathological M stage (pM) M0** M1 |
144 (98.0%) 3 (2.0%) |
| Number of retrieved Lymph Nodes on operative specimen* Median (range) |
26.0 (20.0-32.0) |
| Adjuvant treatment Yes No Unknown |
57 (38.8%) 74 (50.3%) 16 (10.9%) |
| Total patients n=147 |
pN0 n=77 (52.4%) |
pN+ n=70 (47.6%) |
|
|---|---|---|---|
| Specified LN stations in pathology report | 145 (98.6%) | 75 (51.0%) | 70 (47.6%) |
| Thoracic nodes | 86 (58.5%) | 21 (14.3%) | |
| RPTS (st 2R, 4R) | 108 (73.5%) | 0 (0.0%) | |
| Subaortic (st. 5) Para-aortic (st. 4) Subcarinal (st. 7) Triangular ligament (st. 9) Hilar (st. 10) Interlobar (st. 11) |
125 (85.0%) |
4 (2.7%) |
|
| Peri-esophagus (st. 8) | 64 (43.5%) | 19 (12.9%) | |
| Abdominal |
51 (34.7%) |
37 (25.2%) |
|
| Perigastric(st.1, 2, 3, 4sa, 4sb, 4d, 5, 6, 7) Common-hepatic artery (st. 8) Celiac (st. 9) Splenic hilum and splenic-artery (st. 10,11) Hepatoduodenal ligament (st. 12) | |||
| Unspecified LN stations in pathology report | 2 (1.36%) | 2 (1.36%) | 0 (0.0%) |
| . | Esophageal invasion length <4 cm (n=53) | Esophageal invasion length ≥4 cm (n=38) | Missing or uncertain data (n=56) |
|---|---|---|---|
| Total lymph nodes* |
26.5 | 26.2 | 26.1 |
| Metastatic lymph nodes* mean |
2.7 |
2.1 |
2.6 |
| LNR | 10.3% | 7.9% | 10% |
| 5-year OS | 43% | 53% | 40% |
| 5-year DFS | 31% | 21% | 17% |
| 5-year OS | 44% | ||
| 5-year DFS | 29% | ||
| n = 147 | |
|---|---|
| Postoperative Complications Yes No Type of postoperative complication Weight loss ≥ 10% Pleural effusion Infectious pneumonia Anastomotic leak Acute respiratory distress syndrome Atelectasis Empyema Chylothorax Hemothorax Cardiac arrest Conduit ischemia Recurrent laryngeal nerve paralysis |
61 (41.5%) 86 (58.5%) 43 (29.2%) 31 (21.1%) 29 (19.7%) 18 (12.2%) 15 (10.2%) 10 (6.8%) 7 (4.8%) 3 (2.0%) 3 (2.0%) 2 (1.4%) 0 (0.0%) 0 (0.0%) |
| Clavien-Dindo Classification 1 2 3a 3b 4a 4b 5 |
8 (5.4%) 11 (7.5%) 13 (8.8%) 16 (10.9%) 2 (1.4%) 2 (1.4%) 9 (6.1%) |
| Pleural drainage | 19 (12.9%) |
| Surgical reintervention Yes No |
16 (10.9%) 131 (89.1%) |
| Readmission to ICU Yes No |
19 (12.9%) 128 (87.1%) |
| ICU stay duration (days), Median |
1.2 (0 – 34) |
| 30-day mortality | 5 (3.4%) |
| 90-day mortality | 9 (6.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




