1. Introduction
There is currently no consensus of opinion relating to whether instrumentation should be stopped at L5 or S1 when performing long-segment fusion in patients with adult spinal deformity [
1]. When fusion is stopped at L5, postoperative complications may include degeneration of adjacent segments, especially at L5-S1 disc level, which may lead to radiculopathy or distal junctional failure2. Finally, patients with the complications will require additional L5-S1 spinal fusion with pelvic fixation1,2.
Laminar hooks have been used to facilitate the distal junction of long-level instrumentation since the 1990’s3. Existing publications report that laminar hook can be applied without fluoroscopic control, are associated with less blood loss than other techniques, and can maintain a stability similar to that of a pedicle screw system4. In addition, experimental research by Hasegawa et al. demonstrated that the combination of a pedicle screw system and laminar hook can achieve firm fixation when used to treat an osteoporotic spine5. However, do date, there has been no study on how laminar hook affects the adjacent segment degeneration.
In this study, we aimed to investigate the clinical indication of the L5 laminar hook and its effect on adjacent segment degeneration when performing long-segment fusion terminating at L5 in patients with degenerative sagittal imbalance (DSI).
2. Materials and Methods
2.1. Study Design and Participants
This was a retrospective analysis of patients with DSI who underwent surgery to correct spinal deformities at our institution. Institutional Review Board approval was granted for this study to proceed (KHNMC 2024-04-007). We reviewed 265 patients with DSI who underwent deformity corrective surgery performed by a single surgeon between March 2017 and June 2019. The inclusion criteria were as follows: (1) age ≥ 60 years; (2) preoperative Pfirrmann grade [
6] ≤ 3 at L5-S1 segment; (3) upper instrumented vertebra (UIV) at ≥ T12 and lower instrumented vertebra (LIV) at L5; and (4) a minimum follow-up period of ≥ 2 years. The exclusion criteria were as follows: (1) sacralization of L5, (2) a previous history of L5-S1 surgery; (3) diagnosed with degenerative lumbar scoliosis; and (3) gait impairment due to a musculoskeletal disease or congenital anomalies. Finally, only 112 patients were included in this study. The patients were divided into two groups: Group I (applied with laminar hook) and Group II (not applied with laminar hook). For further analysis to determine the indication of L5 lamina hook, Group I patients were divided into the following two groups: Group A (preserved L5-S1 disc) and Group B (exacerbated L5-S1 disc).
2.2. Radiographic Analysis
Preoperative and postoperative (immediate and 2 year postoperative) standing lateral radiographs of the whole spine were retrieved and viewed using the ZeTTA PACS Viewer version 2.0.2.6 (TaeYoung Soft Co., Ltd., South Korea). We then measured a range of radiographic sagittal spinopelvic parameters: C7 sagittal vertical axis (C7SVA), thoracic kyphosis (TK), thoracolumbar kyphosis (TLK), lumbar lordosis (LL), pelvic tilt (PT), sacral slope (SS), pelvic incidence (PI), and PI-LL mismatch.
2.3. Disc Status
The status of the lumbosacral discs (L5-S1) on magnetic resonance imaging (MRI) was evaluated using the Pfirrmann. Based on previous study by Cannizzaro et al. [
7], we classified Pfirrmann grade 1, 2, and 3 as ‘healthy disc’ and grade 4 and 5 as ‘degenerated disc’. Disc status was re-evaluated 2 years postoperatively.
2.4. Statistical Analysis
Preoperative radiographic sagittal spinopelvic parameters and the L5-S1 disc status were compared immediately and 2 years postoperatively using a t-test. Receiver operating characteristic (ROC) curves were generated to determine the cut-off values for specific parameters associated with the progression of L5-S1 disc degeneration. Statistical analyses were performed using SPSS version 21.0 for Windows (IBM Corp., Armonk, NY, USA), and p <0.05 was regarded as significant.
3. Results
3.1. Demographic Data
Of the 112 DSI patients included in the study, 64 (57.1%) had been treated with L5 laminar hook, while 48 (42.9%) were not. The average age in the two groups was 73.5 ± 7.19 and 72.86 ± 6.20 years, respectively, and most were women (Group I: 28/64 vs Group II: 20/48). There was no significant difference between the body mass index (BMI) and bone mineral density (BMD) in either group (p>0.05). For both Groups I and II, the upper instrumented vertebra (UIV) was predominantly located at T11 (Group I: n=28, 43.8% vs Group II: n=16, 33.3%) or T12 (Group I: n=22, 34.4% vs Group II: n=24, 50%). The primary diagnoses leading to previous surgical planning were similar between the two groups: multi-level spinal stenosis (Group I: 50/64, 75% vs Group II: 36/48, 75%), multiple-level fractures (Group I: 8/64, 12.5% vs Group II: 6/48, 12.5%), iatrogenic flatback (Group I: 2/32, 6.3% vs Group II: 4/48, 8.3%), and post-traumatic kyphosis (Group I: 2/64, 3.1% vs Group II: 2/48, 4.2%); there was no significant difference between the two groups (p>0.05) in this respect. Most of the patients had a PI >45° (94/112, 84%); there was no significant difference between the two groups in this respect (p>0.05). (
Table 1)
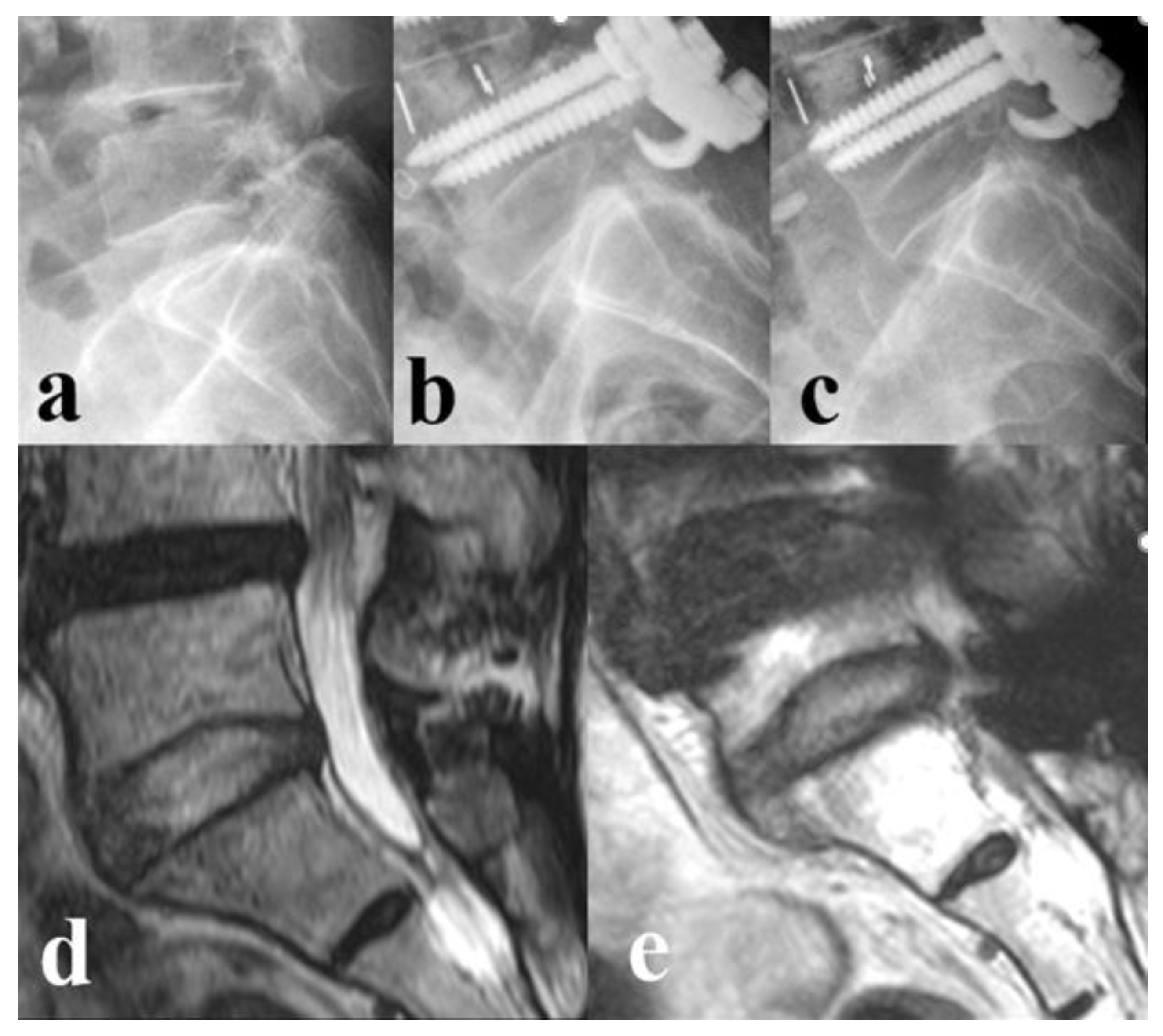
3.2. Disc Status
Immediate postoperative status of the L5-S1 discs was considered healthy (Pfirrmann grade 1, 2, or 3) for both groups (100%). Two years post-surgery, a significantly higher number of patients in Group II had developed L5-S1 disc degeneration (n=36/48, 75%) when compared to that in Group I (n=14/64, 21.9%) (p<0.001). (
Table 2)
3.3. Sagittal Spinopelvic Parameters
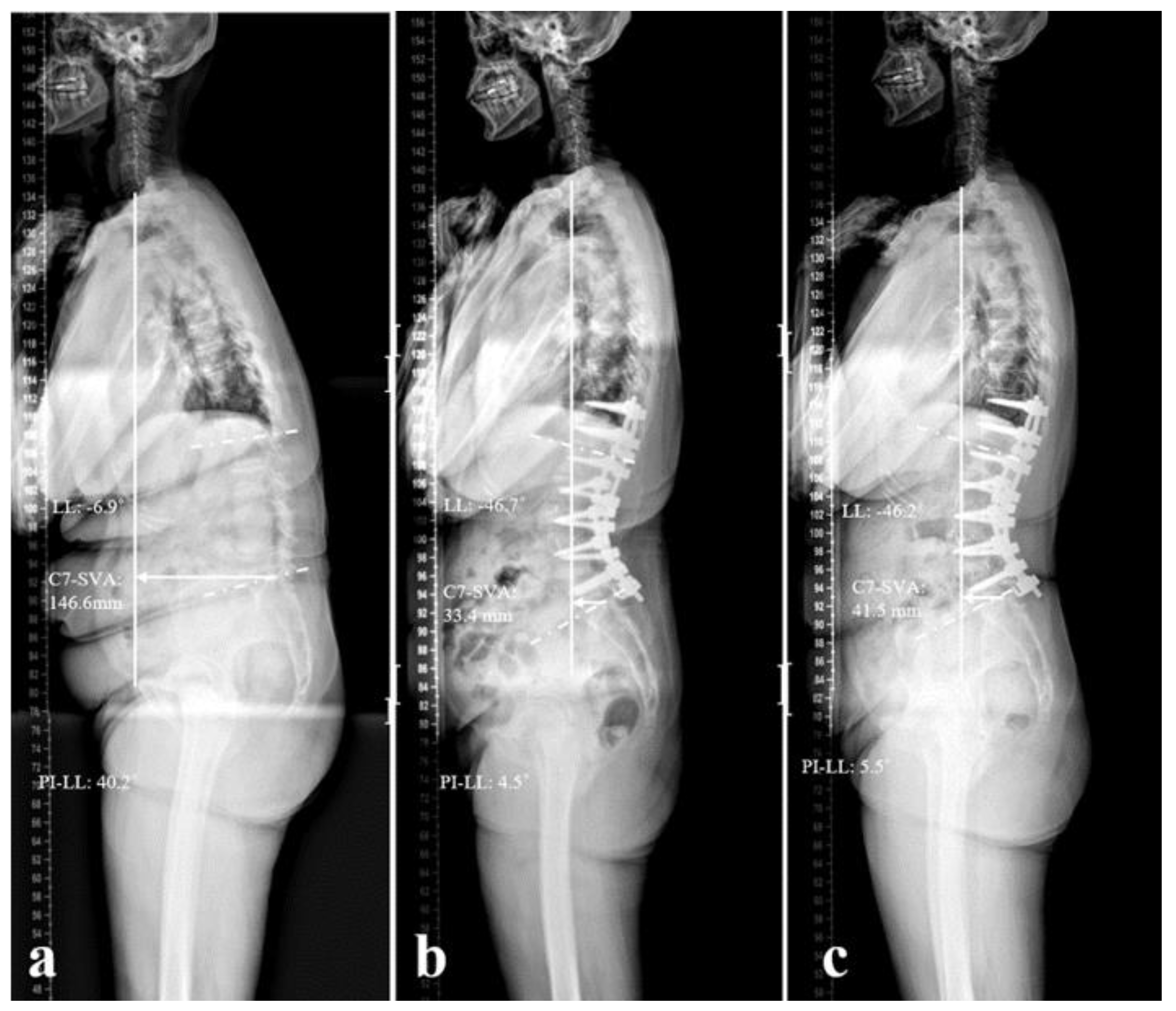
The patients in Group I had more severe preoperative sagittal imbalance than those in Group II (C7SVA: 174.6±45.5 vs 52.9±65.1 mm; LL: -11.6±19.3 vs -22.8±23.6º; PI-LL: 44.4±17.5 vs 29.1±21.2º; p<0.05). For both groups, radiographic parameters had improved significantly post-surgery, and there was no significant loss of correction when assessed at the 2 years follow-up. The degree of correction for C7SVA, LL, and PI-LL mismatch in Group I was significantly greater than that in Group II (C7SVA: -136.2±68.6 vs -29.3±75.8 mm; LL: -40.5±15.4 vs -25.4±21.3º; PI-LL: -40.5±15.3 vs -24.8±21.4º; p<0.05). (
Table 3)
3.4. Subgroup Analysis
Subgroup analysis of the patients in Group I, based on the L5-S1 disc status after 2 years of follow-up, failed to identify significant differences for most demographic data. However, the patients in Group A (preserved disc, n=50) had a significantly lower BMI than those in Group B (exacerbated disc, n=14) (24.11±3.52 vs 27.94±4.39; p=0.038). (
Table 4)
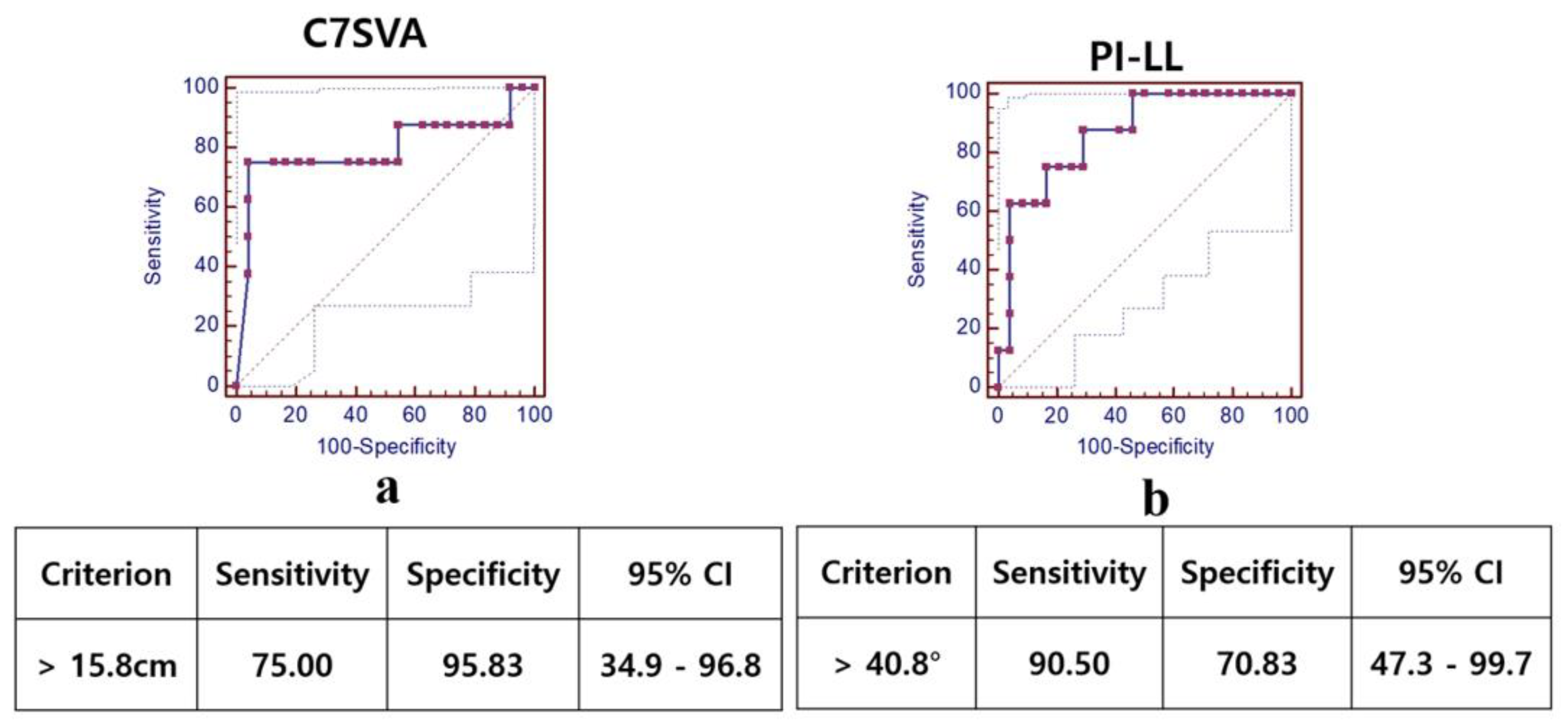
Preoperatively, patients in Group B exhibited a more severe sagittal imbalance than those in Group A (C7SVA: 205.8±109.4 vs 158.9±94.1 mm; PI-LL: 51.9±14.4 vs 40.7±18.1º; p<0.05). (
Table 5) ROC curves were generated to determine the optimal preoperative cut-off values for C7SVA and PI–LL mismatch: 15.8 cm (95% CI: 0.35–0.97) and 40.8° (95% CI: 0.47–0.99), respectively. The AUC was 0.77 for C7SVA and 0.80 for PI–LL. At these thresholds, the sensitivity and specificity for C7SVA were 75.0% and 95.8%, while those for PI–LL were 90.5% and 70.8%. (
Figure 1).
4. Discussion
The laminar hook was first introduced as an adjunct to the pedicle screw and rod system [
3,
4,
5] and is commonly used to treat thoracolumbar fractures as it allows for short-segment pedicle fixation while preserving the spinal motion segments [
8]. The application of a supra-laminar hook for the proximal segment of spinal fusion can protect the superior pedicle screws and reduce the risk of disease in the adjacent segment by gradually distributing stress between fused and unfused segments. This method can be used to prevent proximal junctional failure by allowing a ‘soft landing’ when used in the UIV. On the other hand, the role of a laminar hook in the distal segment is to protect the distal pedicle screws [
8,
9]. Sun et al. [
10] reported that augmenting the pedicle screws with infra-laminar hook in the same vertebra at the distal construct improved the pullout strength of the screws by 21%. However, few studies have investigated the effects of laminar hooks in terms of correcting sagittal imbalance and preventing disc degeneration in patients with DSI. In the current study, we evaluated the effects of a laminar hook at L5 on sagittal parameters and the status of L5-S1 when used to manage patients with DSI.
In the current study, the mean age of patients in both groups was over 70 years, with relatively healthy intervertebral discs at the L5-S1 level and without severe osteoporosis. Given that elderly patients generally exhibit lower levels of physical activity compared to younger individuals, we opted to use a laminar hook or end up at L5 to correct sagittal imbalance during preoperative planning, rather than expanding to S1 or pelvic. Previous studies [
11] have demonstrated a clear trend of increased disc degeneration at the L5-S1 level with higher occupational loading. Furthermore, most patients in this study were diagnosed with spinal stenosis accompanied by flatback deformity. The fusion levels were comparable between the two groups, and as a result, the perioperative processes were largely similar. In a previous study, De Jonge et al. al. [
12] analyzed the effects of posterior multi-segmented spinal hooks on sagittal correction in patients with idiopathic scoliosis; these authors successfully preserved and restored normal LL by applying spinal hooks. Another study demonstrated that the use of laminar hook for the surgical correction of thoracolumbar fractures could achieve significant correction of local kyphosis and effectively maintain the initial correction [
8]. Previous studies showed that the application of a hook could obtain more corrective angles because the laminar hook-rod interface in the distal segment serves as a cantilever beam to achieve better sagittal correction [
9]. In accordance with the guidelines generated by previous research [
2], during their preoperative planning, surgeons tend to opt for the L5 laminar hook to treat patients with a more severe sagittal imbalance (a larger C7SVA, lower LL, and worse PI-LL mismatch). Postoperatively, the patients in both of our groups achieved significant sagittal balance correction, an outcome that was maintained over the 2 years follow-up period. In addition, we observed that the patients in Group I achieved a greater degree of correction; this was because these patients had more severe preoperative sagittal imbalance. Although we were unable to establish the superiority of the laminar hook for surgical correction, we conclude that laminar hooks can effectively restore severe sagittal imbalance and maintain balance (
Figure 2).
Disc degeneration, retrolisthesis, or stenosis in adjacent segments are well-known risk factors for adjacent segmental degeneration (ASD) [
13,
14]. Cannizzaro et al. [
7] reported the risk factor of ASD according to Pfirrmann grade in disc degeneration of adjacent segments, and based on this, we classified Pfirrmann grade 1, 2, and 3 as ‘healthy status’ and grade 4 and 5 as ‘degenerated status’ in this study. Previous studies [
15,
16] reported that the rates of post-surgical L5-S1 disc degeneration were approximately 58% and 69% following long-level surgery that stopped at L5. In the present study, 75% of patients in Group II experienced post-surgical L5-S1 disc degeneration (from ‘healthy status’ to degenerated status’) within two years of surgery, which was a higher proportion than that reported in previous studies. We believe that our worse results were due to the fact that the patients in our study were elderly (72.86±6.20 years of age), had a high BMI (26.86±4.67 kg/m2), and had a long fusion level; these are all known preoperative risk factors for disc degeneration [
17]. Previous studies demonstrated that the addition of laminar hooks in a pedicle screw-rod construct increased pullout resistance and contributed to load sharing or stress distribution between the instrumented segment and the adjacent level without affecting the segments with normal motion [
8,
9,
18]. In addition, laminar hooks have a less rigid attachment to the instrumented vertebrae, thus allowing the spine to adjust and form a smooth transition with the adjacent segment. Laminar hooks also help to counteract dorsally directed, craniocaudal, and mediolateral forces on pedicle walls during surgical correction [
9]. In addition, laminar hooks increase the bone-implant contact surface area, thus facilitating resistance against dorsally directed forces at the distal segment [
18]. Collectively, our results showed that the L5 laminar hook prevented subsequent L5-S1 disc degeneration when used for long-level fusion (
Figure 3).
In our analysis, we found that the L5 laminar hook could effectively prevent degeneration of the distal adjacent disc; however, exacerbation was detected in seven patients (21%). In our subgroup analysis of Group I (in which a laminar hook was applied), the patients in Group B (exacerbated disc) had a significantly higher BMI than those in Group A (preserved disc). This suggests that the benefit of laminar hooks for the prevention of L5-S1 degeneration is limited to patients with higher BMI levels. Furthermore, our comparison of sagittal spinopelvic parameters revealed significantly greater C7SVA and worse PI-LL mismatch values for patients in Group B. Further analysis indicated that the cutoff threshold values for C7SVA and PI-LL mismatch were 15.8 cm and 40.8º, respectively. These data imply that the use of L5 laminar hooks may not prevent L5-S1 degeneration in patients with a high BMI and in those in whom the upper limits of C7SVA and PI-LL mismatch are exceeded. Furthermore, fusion to a more distant S1 or pelvic level may be indicated in patients with DSI.
In the present study, we investigated the utilization of laminar hooks in the management of patients with DSI and evaluated the impact of this technique on sagittal balance correction and its potential ability to prevent disc degeneration in the distal segment. However, there were several limitations to our study that need to be considered. First, this was a retrospective study with a relatively small sample size. A large randomized controlled study of the long-term surgical outcomes of the suggested surgical treatments should now be performed. Second, we were unable to acquire data relating to the complications of patients who had been treated with laminar hooks from the available medical records. Previous studies have reported the occurrence of laminar fractures and spinal stenosis, especially when two laminar hooks were applied; furthermore, the loss of integrity in the ligamentum flavum can lead to sagittal decompensation [
10]. Third, we didn’t evaluate the coronal plane, because we excluded the patients diagnosed with degenerative lumbar scoliosis, which would change our preoperative planning. Furthermore, a previous meta-analysis study demonstrated that long fusion terminating at L5 or the sacrum was similar in scoliosis correction, moreover, complication rate, revision rate, and improvement in pain and disability in patients with adult spinal deformity [
19]. 5. Conclusions
The use of an L5 laminar hook for the surgical correction of DSI can allow spinal surgeons to spare the sacropelvic region during long-level fusion. Furthermore, laminar hooks can provide an effective degree of correction in sagittal balance and may potentially prevent the progression of L5-S1 disc degeneration. Our data suggest that patients with a high BMI and severe sagittal imbalance may not benefit from L5 laminar hooks. The threshold for application of L5 laminar hooks was a preoperative C7SVA and PI-LL mismatch of < 15.8 cm and 40.8°, respectively.
Author Contributions
Conceptualization, Y.-C.K., S.-M.K. and X.J.L.; methodology, X.J.L.; formal analysis, S.-M.K.; data curation, S.-M.K. and I.-S.S.; writing—original draft preparation, S.-M.K. and X.J.L.; writing—review and editing, S.-M.K.; visualization, I.-S.S.; supervision, Y.-C.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (protocol code KHNMC 2024-04-007).
Informed Consent Statement
Patient consent was waived by the Institutional Review Board due to the retrospective nature of the study.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DSI |
Degenerative sagittal imbalance |
| C7SVA |
C7 sagittal vertical axis |
| LL |
Lumbar lordosis |
| PI |
Pelvic incidence |
| BMI |
Body mass index |
| TK |
Thoracic kyphosis |
| TLK |
Thoracolumbar kyphosis |
| PT |
Pelvic tilt |
| SS |
Sacral slope |
| ROC |
Receiver operating characteristic |
References
- Edwards CC, 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG: Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976) 2004, 29(18):1996-2005.
- Taneichi H, Inami S, Moridaira H, Takeuchi D, Sorimachi T, Ueda H, Aoki H, Iimura T: Can we stop the long fusion at L5 for selected adult spinal deformity patients with less severe disability and less complex deformity? Clinical neurology and neurosurgery 2020, 194:105917.
- Margulies JY, Casar RS, Caruso SA, Neuwirth MG, Haher TR: The mechanical role of laminar hook protection of pedicle screws at the caudal end vertebra. Eur Spine J 1997, 6(4):245-248.
- Wilke HJ, Kaiser D, Volkheimer D, Hackenbroch C, Püschel K, Rauschmann M: A pedicle screw system and a lamina hook system provide similar primary and long-term stability: a biomechanical in vitro study with quasi-static and dynamic loading conditions. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2016, 25(9):2919-2928.
- Hasegawa K, Takahashi HE, Uchiyama S, Hirano T, Hara T, Washio T, Sugiura T, Youkaichiya M, Ikeda M: An experimental study of a combination method using a pedicle screw and laminar hook for the osteoporotic spine. Spine 1997, 22(9):958-962; discussion 963.
- Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N: Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001, 26(17):1873-1878.
- Cannizzaro D, Anania CD, De Robertis M, Pizzi A, Gionso M, Ballabio C, Ubezio MC, Frigerio GM, Battaglia M, Morenghi E et al: The lumbar adjacent-level syndrome: analysis of clinical, radiological, and surgical parameters in a large single-center series. J Neurosurg Spine 2023, 39(4):479-489.
- Leduc S, Mac-Thiong JM, Maurais G, Jodoin A: Posterior pedicle screw fixation with supplemental laminar hook fixation for the treatment of thoracolumbar burst fractures. Can J Surg 2008, 51(1):35-40.
- Lentz J, Mun F, Suresh K, Groves M, Sponseller PJJ: How and When to Use Hooks to Improve Deformity Correction. 2021, 3(4).
- Sun E, Alkalay R, Vader D, Snyder BD: Preventing distal pullout of posterior spine instrumentation in thoracic hyperkyphosis: a biomechanical analysis. Journal of spinal disorders & techniques 2009, 22(4):270-277.
- Salo S, Hurri H, Rikkonen T, Sund R, Kröger H, Sirola J: Association between severe lumbar disc degeneration and self-reported occupational physical loading. J Occup Health 2022, 64(1):e12316.
- de Jonge T, Dubousset JF, Illés T: Sagittal plane correction in idiopathic scoliosis. Spine 2002, 27(7):754-760.
- Okuda S, Nagamoto Y, Matsumoto T, Sugiura T, Takahashi Y, Iwasaki M: Adjacent Segment Disease After Single Segment Posterior Lumbar Interbody Fusion for Degenerative Spondylolisthesis: Minimum 10 Years Follow-up. Spine (Phila Pa 1976) 2018, 43(23):E1384-E1388.
- Yugue I, Okada S, Masuda M, Ueta T, Maeda T, Shiba K: Risk factors for adjacent segment pathology requiring additional surgery after single-level spinal fusion: impact of pre-existing spinal stenosis demonstrated by preoperative myelography. Eur Spine J 2016, 25(5):1542-1549.
- Cho KJ, Suk SI, Park SR, Kim JH, Choi SW, Yoon YH, Won MH: Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2009, 18(4):531-537.
- Kuhns CA, Bridwell KH, Lenke LG, Amor C, Lehman RA, Buchowski JM, Edwards C, 2nd, Christine B: Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5-S1 disc, minimum 5-year follow-up. Spine (Phila Pa 1976) 2007, 32(24):2771-2776.
- Wang T, Ding W: Risk factors for adjacent segment degeneration after posterior lumbar fusion surgery in treatment for degenerative lumbar disorders: a meta-analysis. J Orthop Surg Res 2020, 15(1):582.
- Steinmetz B, and Benzel. In: Benzel’s Spine Surgery Elsevier Health Sciences. edn.; 2021.
- Jia F, Wang G, Liu X, Li T, Sun J: Comparison of long fusion terminating at L5 versus the sacrum in treating adult spinal deformity: a meta-analysis. Eur Spine J 2020, 29(1):24-35.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).