1. Introduction
With increasing aging populations, the patients with adult spinal deformity (ASD) have been frequently treated conservatively or surgically. The clinical symptoms of ASD include an intractable low back pain, impaired standing and walking ability, trunk or gazing disturbance, shortness of breath, eating disorder or gastroesophageal reflux, and psychological stress [
1]. The neurologic disturbances also exhibit the pain in lower extremities and intermittent claudication.
The quality of life in ASD patients are severely impaired when compared to other chronic medical disorders [
2,
3]. Pellise F, et al. compared physical and mental SF-36 scores between ASD and other chronic disorders from 24946 people data base, demonstrating lower physical and mental scores than those in disorders of diabetes, chronic lung disease, and congestive heart failure [
2]. Bess S, et al. also reported lower physical SF-36 scores of symptomatic ASD than those of united states total population, depression, diabetes, and hypertension [
3]. The further impact was demonstrated in which physical SF-36 score of ASD was equivalent to that of cancer patient.
For severely disabled patients, the surgical correction and fusion surgeries were usually performed. The effectiveness of surgical treatment has been discussed and evaluated whether the surgical treatment improved the patients’ quality of life, or not [
4,
5]. Paulus et al. conducted the systematic review of thirteen studies evaluating cost and value of spinal deformity surgery [
4]. Using the measures of SRS-22 and ODI, they concluded that ASD patients benefited from surgical treatment compared to nonsurgical treatment. The nonsurgical treatment didn’t seem to be cost-effective and didn’t have a positive impact on quality of life in ASD patients. Acaroglu et al. evaluated 968 ASD patients’ data base and compared the effectiveness of surgery between surgical and nonsurgical groups [
5]. They demonstrated the superior effectiveness of 54 % in surgical group when compared to 9.7% in nonsurgical group.
Although the surgery improves the quality of life in ASD patients, the corrective ASD surgeries have accompanied with several complications [
6,
7]. Smith et al. reported a total of 70% complication rates in posterior-based ASD surgeries with 52% in perioperative and 43% in delayed [
6]. Sciubba et al. investigated 11692 pts of ASD and reported 55% of overall complication rate [
7]. They demonstrated that the higher complication rate was detected in three-column osteotomy surgeries.
Within a recent decade, several innovative surgical modalities have been developed to minimize the surgical invasiveness for ASD surgeries. Hynes et al. developed the oblique lateral interbody fusion (OLIF) technique minimizing the conventional ALIF surgery using a special tubular retractor (Medtronics, Memphis TN) [
8]. The percutaneous pedicle screw (PPS) technique was successfully developed by Foley and the deformity correction with PPS was introduced by Anand et al. [
9,
10]. We have started OLIF surgery for L1-5 since 2012 with combined use of PPS for ASD surgeries. Although the successful clinical results with minimized invasiveness have been obtained, there still have been mechanical complications of rod fracture, proximal and distal junctional kyphosis, and pseudarthrosis seen in the series of patients. To better solve these problems, L5/S1 OLIF (OLIF51) was employed since 2015 instead of using L5/S1 transforaminal interbody fusion (TLIF) [
11,
12].
The objective of this study was to compare the clinical and radiologic results of anterior and posterior combined correction surgery for ASD between the use of OLIF51 versus L5/S1 TLIF.
2. Materials and Methods
A total of 117 patients treated by anterior-posterior combined surgery with OLIF25 were enrolled in this study. The average age at surgery was seventy-six years old (54-86). In all patients, the two-stage surgery of multiple OLIFs followed by all percutaneous pedicle screw (PPS) correction (circumferential MIS) or combination of PPS and mini-open posterior correction was performed (
Figure 1). Eighty-two patients received TLIF at L5/S1 (51TLIF group), and thirty-five patients received OLIF at L5/S1 (OLIF51 group). In 51TLIF group, OLIF at L1-5 surgery was conducted at the first-stage, and the second-stage surgery included mini-open TLIF at L5/S1 using local bone and 18-degree lordotic cage (Capstone control, Medtronics, Memphis TN) and correction with PPSs from lower thoracic to pelvis. The OLIF51 group received L1-S1 OLIFs for the first-stage, followed by all PPS correction and fixation from lower thoracic to pelvis (Circumferential MIS:cMIS). The graft materials used were rectangular PEEK cage (Clydesdale, Medtronics, Memphis TN) with demineralized bone matrix (DBM) soaked with aspirated bone marrow for OLIF25, and 10-degree lordotic PEEK cage (MectaLIF, Medacta international, San Pietro, Switzerland) or 12 or 18-degree lordotic cage (Sovereign, Medtronics, Memphis TN) with demineralized bone matrix (DBM) soaked with aspirated bone marrow for OLIF at L5/S1 (
Figure 2). All surgeries were conducted with use of surgical navigation and O-arm (Stealthstation 7, Medtronics, Memphis TN).
The evaluated parameters were a total operation time (mins, OT), estimated blood loss (ml, EBL), and early and late complications. The following radiologic parameters were measured preoperatively and at follow-up: Sagittal vertebral axis (SVA ; mm), Coronal vertebral axis (CVA; mm), Lumbar lordosis (LL; deg), Lower lumbar lordosis (LLL; mm), Sacral slope (SS; deg), Pelvic incidence –lumbar lordosis mismatch (PI-LL; deg), Pelvic tilt (PT ; deg), segmental lordosis at L5/S1, and coronal tilt of L5 vertebra. The clinical outcomes were evaluated with JOABPEQ effectiveness rate [
13], and visual analogue scale (VAS) preoperatively and at follow-up. The patient demographics shown in
Table 1 demonstrated no significant difference between two groups (
Table 1).
Table 1.
Patient background demographics.
Table 1.
Patient background demographics.
| |
OLIF51 |
TLIF |
| Patient number |
35 |
82 |
| Age at Surgery |
75.0 (54-85) |
75.0 (64-86) |
| Gender (Male: Female) |
5 : 30 |
14: 68 |
| Weight (kg) |
48.3 (32-68) |
49.5 (32-72) |
| Height (m) |
1.50(1.8-1.64) |
1.51 (1.30-1.69) |
| BMI (%) |
21.6 (13.6-30.0) |
21.7 (15.8-30.2) |
| Scoliosis Cobb angle (deg) |
29.0 (0-72) |
25.1 (3.8-45.2) |
| CVA (mm) |
33.9 (0-112.7) |
51.2 (19.7-123.5) |
| SVA (mm) |
149.0 (0-691.0) |
148.0 (10.5-349.2) |
| PT (deg) |
47.8 (22.7-69.3) |
52.2 (38.9-68.7) |
| LL (deg) |
9.5 (-38.0-50.1) |
7.6 (-29.3-37.0) |
| PI-LL (deg) |
39.4 (0-77.6) |
44.6 (4.3-91.5) |
| Seg. Lordosis at L5/S1 (deg) |
11.3 (-3.0-29.7) |
10.5 (-1.1-22.2) |
| Fixed segments |
7.7 (3-10) |
8.1 (4-12) |
| OLIF segments |
4.6 (1-5) |
3.9 (2-6) |
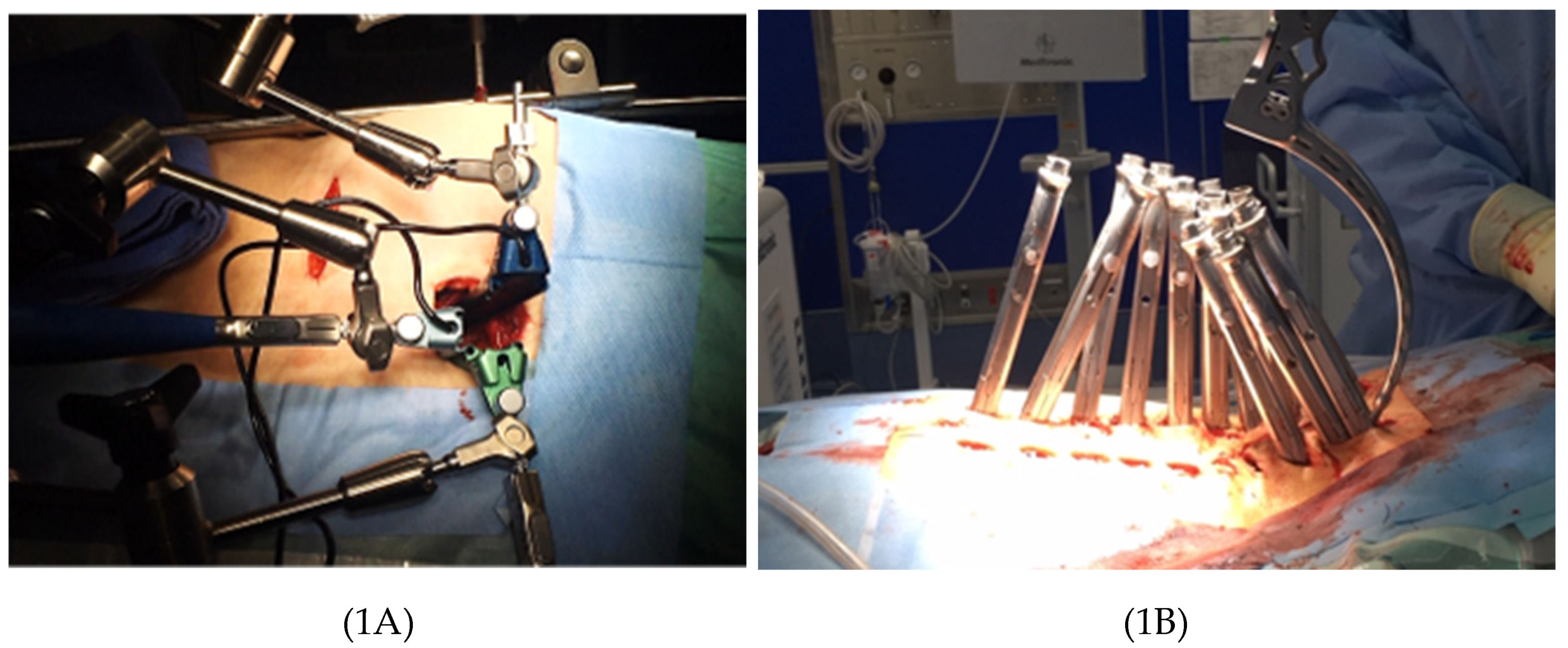
Figure 1.
Circumferential MIS procedure with multiple OLIFs and all percutaneous posterior correction. 1A: OLIF51 procedure utilizes the specially designed triple-arm retractor. 1B: All percutaneous posterior correction procedure.
Figure 1.
Circumferential MIS procedure with multiple OLIFs and all percutaneous posterior correction. 1A: OLIF51 procedure utilizes the specially designed triple-arm retractor. 1B: All percutaneous posterior correction procedure.
Figure 2.
OLIF51 with use of Sovereign hyperlordotic cage fixed with integrated screws and demineralized bone matrix soaked with aspirated bone marrow.
Figure 2.
OLIF51 with use of Sovereign hyperlordotic cage fixed with integrated screws and demineralized bone matrix soaked with aspirated bone marrow.
3. Results
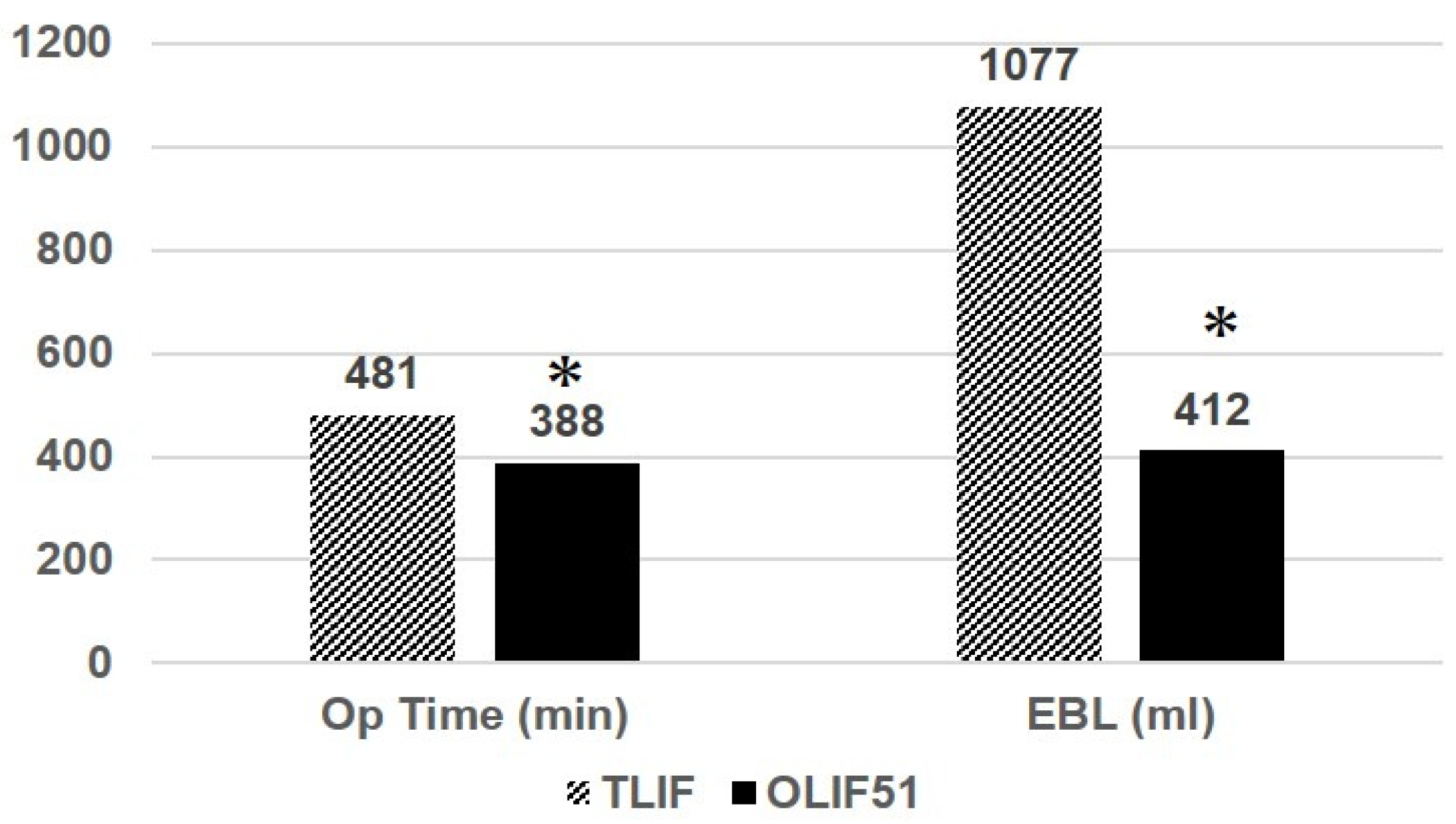
The average follow-up periods were 41 months (16-84) in 51TLIF group and 26 months (13-42) in OLIF51 group. The average fixed vertebrae were 8.1(4-12) in 51 TLIF group, and 8 (4-10) in OLIF51 group respectively. The average OT was 481 mins (278-739) and 388 mins (267-608) in 51 TLIF and OLIF51 groups, respectively (P<0.05) (
Figure 3). The average EBL was 1077.9 ml (220-2644) and 411.7 ml (120-1708) in 51TLIF and OLIF51 groups, respectively (P<0.01). The coronal cobb angle was 25.1 degrees (4-45) and 29.0 degrees (2-72) in 51TLIF and OLIF51 groups, preoperatively, and corrected to 9.5 degrees (1-23) and 10.0 degrees (1-26) respectively at follow-up (NS) (
Table 2). The thoracic kyphosis was 20.9 degrees (1-78) and 23.8 degrees (2-73) in 51TLIF and OLIF51 groups, preoperatively, and corrected to 36 degrees (13-58) and 38.3 degrees (18-59) respectively at follow-up (NS). The average CVA was 51.2 mm (19-123) and 33.9 mm (0-112) in 51TLIF and OLIF51 groups, preoperatively, and corrected to 29.2mm (0-53) and 17.0 mm (0-58) at follow-up (NS). The average SVA was 148 mm (10-349) and 149 mm (0-691) in 51 TLIF and OLIF51 groups, preoperatively, and corrected to 33.7 mm (-33.1-112) and 26.9 mm (-35-99) at follow-up (NS). The average SS was 21.4 deg. (11.6-33.4) and 17.0 deg. (-28-44) in 51 TLIF and OLIF51 groups, preoperatively, and corrected to 28.3 deg. (15.0-35.4) and 30.0 deg. (11.0-50.5) at follow-up (NS). The average PT was 30.9 deg. (18.3-48.1) and 31.2 deg. (14.0-54.0) in 51 TLIF and OLIF51, preoperatively and corrected to 16.7 deg. (4.9-36.0) and 19.0 deg. (-3.0 -35) at follow-up (NS).
The average lumbar lordosis (LL) was 7.6 deg. (-29.3-37.3) and 9.5 deg. (-38.0 -50.1) in 51TLIF and OLIF51, preoperatively and corrected to 45.4 deg. (33.2 -58.9) and 46.9 deg. (22.0 - 65.0) at follow-up (NS). The average PI-LL was 44.6 deg. (4.3-91.5) and 39.4 deg. (0-77.6) in 51 TLIF and OLIF51, respectively, and corrected to 6.9 deg (-9.6-33.6) and 2.5 deg. (-23.7-24.0) at follow-up (P<0.05). The average LLL was 18.1 deg. (-10.4-34.8) and 20.0 deg. (-26.7-47.2) in 51TLIF and OLIF51, preoperatively and corrected to 28.8 deg. (21.0-34.0) and 34.9 deg. (13-51.7) at follow-up (P<0.01). The average lordotic angle at L5/S1 was 10.5 deg. (-1.1-22.2) and 11.3 deg. (-3-29.7) in 51 TLIF and OLIF51, respectively and corrected to 16.0 deg. (4.5-21.0) and 19.8 (5.6-44.1) at follow-up (P<0.01). The average coral tilt angle of L5 to S1 was 5.4 deg (0.6-14.5) and 6.0 deg (0-23) in 51TLIF and OLIF51, preoperatively and corrected to 4.3 deg. (0-10.5) and 2.5 deg. (0-8.0) at follow-up (P<0.01).
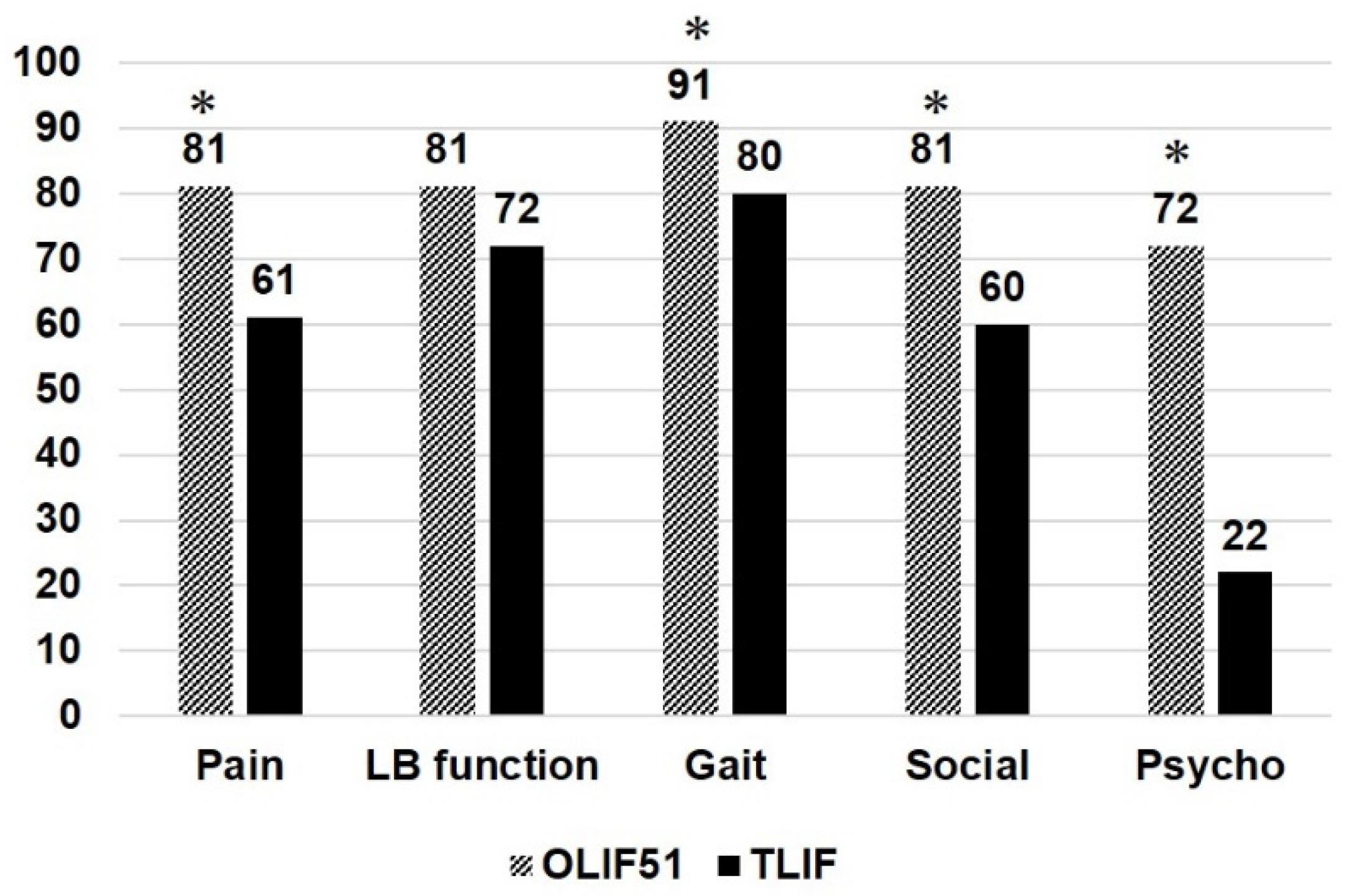
The
Figure 4 showed JOABPEQ effectiveness rate (%) in 51TLIF and OLIF51 group, demonstrating several significant differences between two groups. The effectiveness rate in OLIF51 was higher in pain, gait, social and psychologic domains when compared to 51 TLIF group (P<0.05). The
Table 3 showed the VAS changes of two groups between preoperative and at follow-up. The both groups demonstrated significant reductions of VAS value after surgery, however, there were no statistical differences between two groups.
In terms of surgical complications, there were no neurovascular complications in both groups. The occurrence of proximal junctional kyphosis was 13% and 6% in 51TLIF and OLIF51 groups, however, there were no statistical differences between two groups. The instrumentation failures included the set screw dislodge or rod fracture, with or without the revision surgeries. The occurrence of instrumentation failure was 5% and 8% in 51TLIF and OLIF51 groups respectively, which was statistically equivalent (NS). In OLIF51 group, we experienced a major intraoperative complication of pulmonary fat embolism requiring emergency ECMO treatment in the intensive care unit. The patient successfully recovered and completed a two-stage surgery.
Case Presentations
Case 1: 78 years old, female, Degenerative lumbar scoliosis
The patient complained of severe low back pain, difficulty of standing, and pain and numbness in lower extremities preoperatively. She received cMIS employing OLIF51 with an intraoperative estimated blood loss of 294ml and operation time of 418 mins totally. The lumbar lordosis increased four to 54 degrees postoperatively and PI-LL mismatch became zero degree postoperatively (
Figure 5).
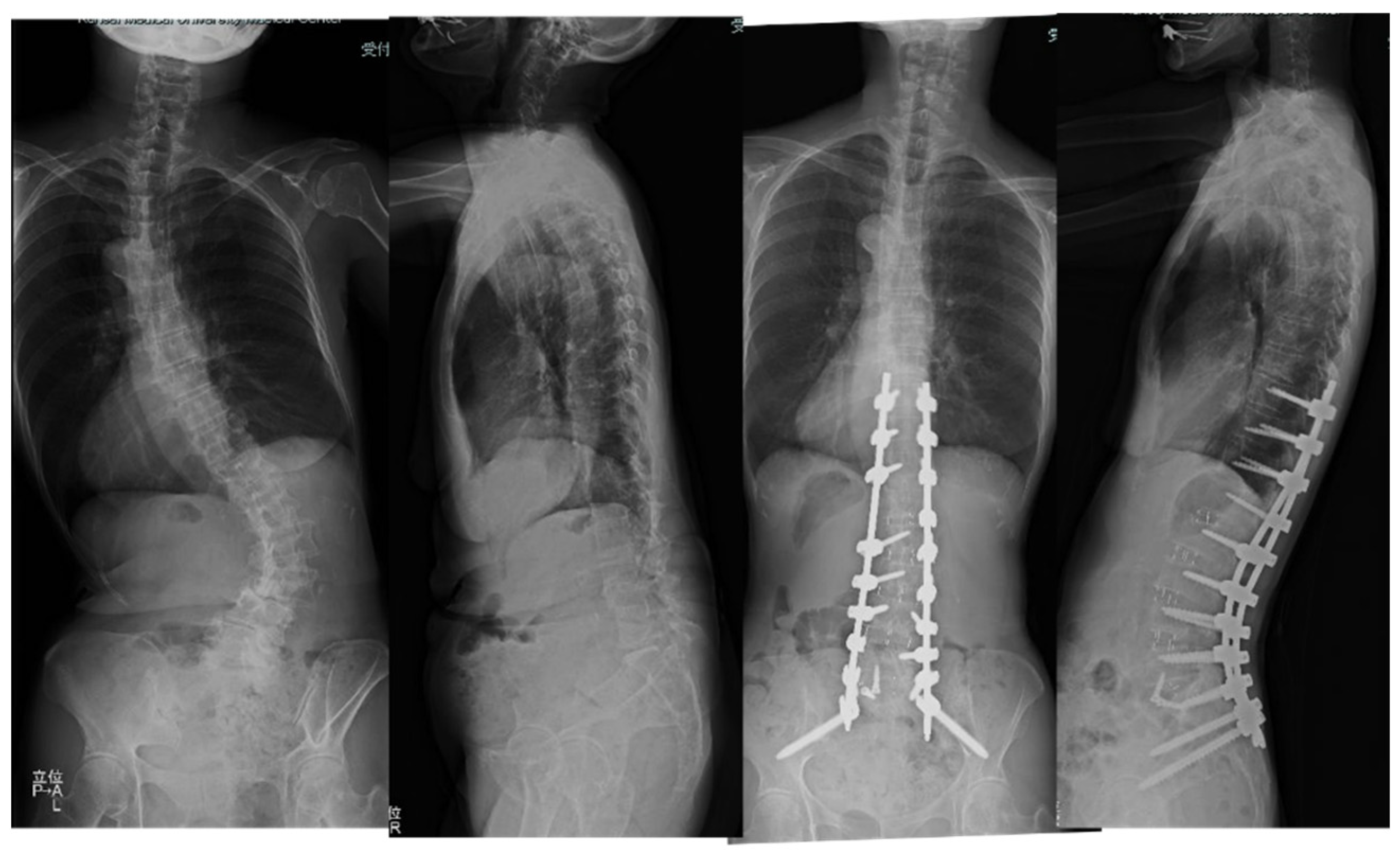
Case 2: 68 years old, female, adult scoliosis
The patient has been suffering from severe low back pain and deformity for several years.
She received cMIS employing OLIF51 with an intraoperative estimated blood loss of 594 ml and operation time of 374 mins totally. The preoperative Cobb angle of 63 degree was corrected to 7 degrees at follow-up. The preoperative PI-LL of 54 degrees was corrected to two degrees at follow-up (
Figure 6).
Table 2.
Summarized radiologic results in two groups.
Table 2.
Summarized radiologic results in two groups.
| |
OLIF51 |
TLIF |
Significance |
| Preop Cobb angle (deg) |
29.0 (0-72) |
25.1 (3.8-45.2) |
NS |
| Follow-up Cobb angle (deg) |
10.0 (0-28) |
9.5 (1.4-23.3) |
NS |
| Preop thoracic kyphosis (deg) |
23.8 (2.1-73.0) |
20.9 (1.1-77.7) |
NS |
| Follow-up thoracic kyphosis (deg) |
38.3 (18.1-59.0) |
36.0 (13.6-57.9) |
NS |
| Preop CVA (mm) |
33.9 (0-112.7) |
51.2 (19.7-123.5) |
NS |
| Follow-up CVA (mm) |
17.0 (0-58) |
29.2 (0-53.1) |
NS |
| Preop SVA (mm) |
149.0 (0-691) |
148.0(10.5349.2) |
NS |
| Follow-up SVA (mm) |
26.9 (-35.0-99.0) |
33.7 (-33.1-112) |
NS |
| Preop SS (deg) |
17.0 (-28-44) |
21.4 (11.6-33.4) |
NS |
| Follow-up SS (deg) |
30.0 (11-50.5) |
28.3 (15-35.4) |
NS |
| Preop PT (deg) |
31.2 (14-54.0) |
30.9 (18.3-48.1) |
NS |
| Follow-up PT (deg) |
19.0 (-3.0-35.0) |
16.7 (4.9-36.0) |
NS |
| Preop LL (deg) |
9.5 (-38.0-50.1) |
7.6 (-29.3-37.0) |
NS |
| Follow-up LL (deg) |
46.9 (22.0-65.0) |
45.4 (33.2-58.9) |
NS |
| Preop LLL (deg) |
20.2 (-26.7-47.2) |
18.1 (-10.4-34.8) |
NS |
| Follow-up LLL (deg) |
34.9 (13.0-51.7) |
28.8 (21.0-34.0) |
P<0.01 |
| Preop PI-LL (deg) |
39.4 (0-77.6) |
44.6 (4.3-91.5) |
NS |
| Follow-up PI-LL (deg) |
2.5 (-23.7-24.0) |
6.9 (-9.6-33.6) |
P<0.05 |
| Preop L5/S1 segmental lordosis (deg) |
11.3 (-3.0-29.7) |
10.5 (-1.1-22.2) |
NS |
| Follow-up L5/S1 segmental angle |
19.8 (5.6-44.1) |
16.0 (4.5-21.0) |
P<0.01 |
| Preop L5 coronal tilt (deg) |
6.0 (0-230) |
5.4 (0.6-14.5) |
NS |
| Follow-up L5 coronal tilt (deg) |
2.5 (0-8.0) |
4.3 (0-10.5) |
P<0.01 |
Table 3.
Visual analogue scale in two groups.
Table 3.
Visual analogue scale in two groups.
| |
OLIF51 |
TLIF |
Significance |
| Preop LBP |
58 (0-100) |
63.6 (30-80) |
NS |
| Follow-up LBP |
16.4 (0-50) |
21.0 (0-70) |
NS |
| Preop LE pain |
58.3 (0-100) |
52.7 (20-70) |
NS |
| Follow-up LE pain |
17.3 (0-80) |
26.0 (0-90) |
NS |
| Preop LE numbness |
43.4 (0-100) |
51.8 (20-70) |
NS |
| Follow-up LE numbness |
17.3 (0-60) |
11.0 (0-30) |
NS |
Figure 3.
Operation time and Estimated blood loss (EBL) in two groups. The asterisk depicts a statistical significance at P<0.05 level.
Figure 3.
Operation time and Estimated blood loss (EBL) in two groups. The asterisk depicts a statistical significance at P<0.05 level.
Figure 4.
JOABPEQ effectiveness rate (%) in two groups. The asterisk depicts a statistical significance at P<0.05 level.
Figure 4.
JOABPEQ effectiveness rate (%) in two groups. The asterisk depicts a statistical significance at P<0.05 level.
Figure 5.
78 years old female, degenerative lumbar scoliosis. The successful cMIS with OLIF51 was performed with a total blood loss of 294ml.
Figure 5.
78 years old female, degenerative lumbar scoliosis. The successful cMIS with OLIF51 was performed with a total blood loss of 294ml.
LL was corrected to 54 degrees from four degrees and PI-LL mismatch became zero at follow-up.
Figure 6.
68 years old female, adult scoliosis The successful cMIS with OLIF51 was performed with a total operation time of 374 mins and estimated blood loss of 594ml. The preoperative Cobb angle of 63 degree was corrected to 7 degrees at follow-up. The preoperative PI-LL of 54 degrees was corrected to two degrees at follow-up.
Figure 6.
68 years old female, adult scoliosis The successful cMIS with OLIF51 was performed with a total operation time of 374 mins and estimated blood loss of 594ml. The preoperative Cobb angle of 63 degree was corrected to 7 degrees at follow-up. The preoperative PI-LL of 54 degrees was corrected to two degrees at follow-up.
4. Discussion
Historically, the management of adult spinal deformities has been a challenging one for spine surgeons [
15]. The adult deformity surgery has been at greater risk for several complications. The exclusive posterior or combined anterior-posterior surgery has been advocated in conjunction with posterior column or three-column osteotomy for the effective release for rigid spines [
1,
15]. However, these surgical modalities involve the excessive estimated blood loss, longer operation time and higher postoperative complications [
1,
7].
In recent years, the multiple lateral interbody fusions (LIF) have been widely used with posterior open instrumentation (hybrid) or cMIS (all PPS) procedure for ASD [
1,
16,
17]. Bae et al. compared three surgical strategies of exclusive posterior approach, hybrid, and anterior fusion with posterior approach for ASD [
16]. Although satisfactory radiologic outcomes were achieved in three groups, however, the hybrid group demonstrated lower PJK and mechanical complications, lower ODI scores and higher SRS-22 scores [
16]. Haque et al. examined 234 ASD patients and compared three surgical modalities of open, hybrid and cMIS. The cMIS group demonstrated a significantly smaller blood loss, while larger PI-LL correction was achieved in hybrid group. The lower complication rate was found in cMIS and hybrid group, when compared to open group [
18]. Park et al. compared two surgical strategies of hybrid and cMIS in 105 patients of ASD [
19]. Although there was no difference in terms of radiologic parameters, ODI, and VAS scores, however, the complication rate was significantly lower in cMIS than hybrid group [
19].
The OLIF51 procedure is a minimally invasive ALIF performed in lateral decubitus position [
8]. Using a small oblique incision medial to ASIS, L5/S1 intervertebral disc is exposed through retroperitoneal approach following the release and retraction of bilateral common iliac vessels. After an extensive disc excision, a bone graft and cage insertion with high lordotic cage up to eighteen-degree can be placed with integrated screw fixation. The several papers advocated the advantage of OLIF51 over L5/S1 TLIF in single-level to multilevel reconstruction surgeries [
11,
12,
20,
21]. Mun et al. compared OLIF51 and L5/S1 TLIF in 148 patients for single-level fusion surgery [
20]. They demonstrated that OLIF51 achieved significantly higher disc angle than that of L5/S1 TLIF (22.6 vs 12.3 degree) as well as smaller cage subsidence rate of 16.2% (vs 25.3%). Our previous study comparing single-level OLIF51 versus TLIF demonstrated that OLIF51 showed higher fusion rate of 97% (vs 92%), better low back function in JOABPEQ effectiveness rate, and larger segmental lordosis of 17 degree (vs 12 degree) [
11]. From these reason, OLIF51 procedure has been applied to ASD surgery by several surgeons in the world [
21,
22,
23].
We have started the use of OLIF25 from 2012 for ASD and applied it to L1-5 levels in conjunction with L5/S1 TLIF. Our posterior approaches have been various with the deformity severity for hybrid, cMIS and posterior approach with osteotomy. Although the deformity correction and less invasiveness of surgery were achieved successfully according to this surgical strategy, mechanical complications including rod fracture, pseudarthrosis, and PJK were still observed [
24,
25,
26]. Since 2015, we started to employ OLIF51 combined with cMIS instead of 51 TLIF. This study was to clarify the clinical and radiologic effects of OLIF51 procedure with cMIS when compared to 51TLIF with cMIS.
In the ASD surgery, there have been several studies comparing ALIF versus TLIF at L5/S1 [
27,
28,
29]. Dorward et al. conducted a matched cohort analysis of 42 patients in each group of ALIF and TLIF, demonstrating that ALIF provided a significantly better segmental lordosis and less intraoperative blood loss over TLIF [
27]. Singh et al. retrospectively investigated pseudarthrosis rates of 49 patients of TLIF versus 51 patients of ALIF with a two-year follow-up [
28]. The results demonstrated that clinical pseudarthrosis rate was higher in TLIF (12/49) than that in ALIF (1/51) significantly. The multivariate analysis revealed the pseudarthrosis risk was 4.86 times higher in TLIF [
28]. Adogwa et al. examined rod fracture rates between TLIF and ALIF in long segment adult deformity surgery [
29]. The result demonstrated that the incidence of bilateral rod fracture was significantly higher in TLIF when compared to ALIF (2.2% vs 0.70%).
In terms of the comparison between OLIF51 and TLIF, there have been a few studies reported in ASD surgeries [
21,
22,
23]. Park SW et al. reported a series of 23 patients comprising 13 patients of OLIF51 and 10 patients of TLIF [
23]. Although the operation time was statistically equivalent, the estimated total blood loss was significantly smaller in OLIF51 group (260 vs 423ml). Radiographically, the larger segmental angle (18.4 vs 6.9 deg.), smaller PI-LL mismatch (3.6 vs 7.5 deg.), larger LL (55.5 vs 46.9 deg.) and LLL (31.1 vs 22.3 deg.) were demonstrated in OLIF51 when compared to TLIF group [
23]. Tanaka M, et al. compared 54 ASD patients comprising 13 patients of OLIF51 and 41 patients of TLIF clinically and radiographically [
21]. They demonstrated shorter operation time (356 vs 492 min.) in OLIF51, however, no significant reduction of total estimated blood loss was identified (1016 vs 1252 ml). Radiographically, larger segmental angle (21.4 vs 12.1) and disc height (11.3 vs 9.4mm) were statistically demonstrated in OLIF51, however, OLIF51 group inversely showed larger SVA and PI-LL mismatch than TLIF group [
21]. The superiority of LL and LLL creation in OLIF51 was not demonstrated in this study. In both studies, no statistical difference in PJK and rod breakage rate, and clinical outcome of ODI and VAS were demonstrated between OLIF51 and TLIF [
21,
23].
The present study demonstrated that OLIF51 provided significantly shorter operation time, and less estimated blood loss compared to TLIF. We speculated two reasons that first, TLIF required facet resections and secondary, OLIF51 procedure led to better lordotic correction, enabling an easier and faster posterior correction procedure contributing less invasiveness of surgery. Radiographically, OLIF51 provided larger segmental lordosis at L5/S1, thereby leading to better spinopelvic alignment and LLL over 70% of lumbar lordosis. We found a significant difference in L5 coronal tilt between OLIF51 and TLIF group. This meant that OLIF51 procedure achieved the three-dimensional correction at the L5/S1 segment in both coronal and sagittal planes. In previous reports, the fractional curve correction in ASD was studied in terms of the use of ALIF [
30,
31]. Geddes et al. compared the fractional curve correction of ASD between 31 cases of L5/S1 ALIF and posterior spinal fusion (PSF) versus 28 cases of PSF alone. The results demonstrated a significantly greater coronal correction was achieved in ALIF and PSF group when compared to PSF alone. Buell et al. conducted a multicenter study comparing fractional curve correction between L5/S1 ALIF versus TLIF in 106 patients of long segment fusion for ASD [
31]. The results demonstrated comparable fractional curve correction between ALIF (66.7%) versus TLIF (64.8%). In reviewing the previous studies employing OLIF51, this study was first to demonstrate the superiority of OLIF51 in coronal plane correction of ASD in addition to the sagittal plane.
There were several limitations in this study. First, the follow-up periods differed between 16-84 months in 51TLIF and 13-42 months in OLIF51 group. Although bony fusion at the segments can be evaluated mostly at 12 months periods, this difference may influence the occurrence of rod fracture and other instrumentation failures. Also, the quality-of-life parameters and VAS scores may be influenced as well. Secondary, we utilized an 18-degree cage (Capstone, Medtronics, Memphis TN) combined with autograft bone for L5/S1 TLIF. Although sixteen degrees of segmental lordosis was obtained at the L5/S1 segment, the use of recently developed hyperlordotic cage or expandable cage may change the lordotic creation as well as coronal plane correction even in the TLIF procedure. Thirdly, there were still small cases of 35 patients in the OLIF51 group evaluated. The future research will be employing larger size of cases as well as the use of propensity score matching design to precisely compare the difference of two surgical procedures.