Submitted:
25 August 2025
Posted:
25 August 2025
You are already at the latest version
Abstract
Keywords:
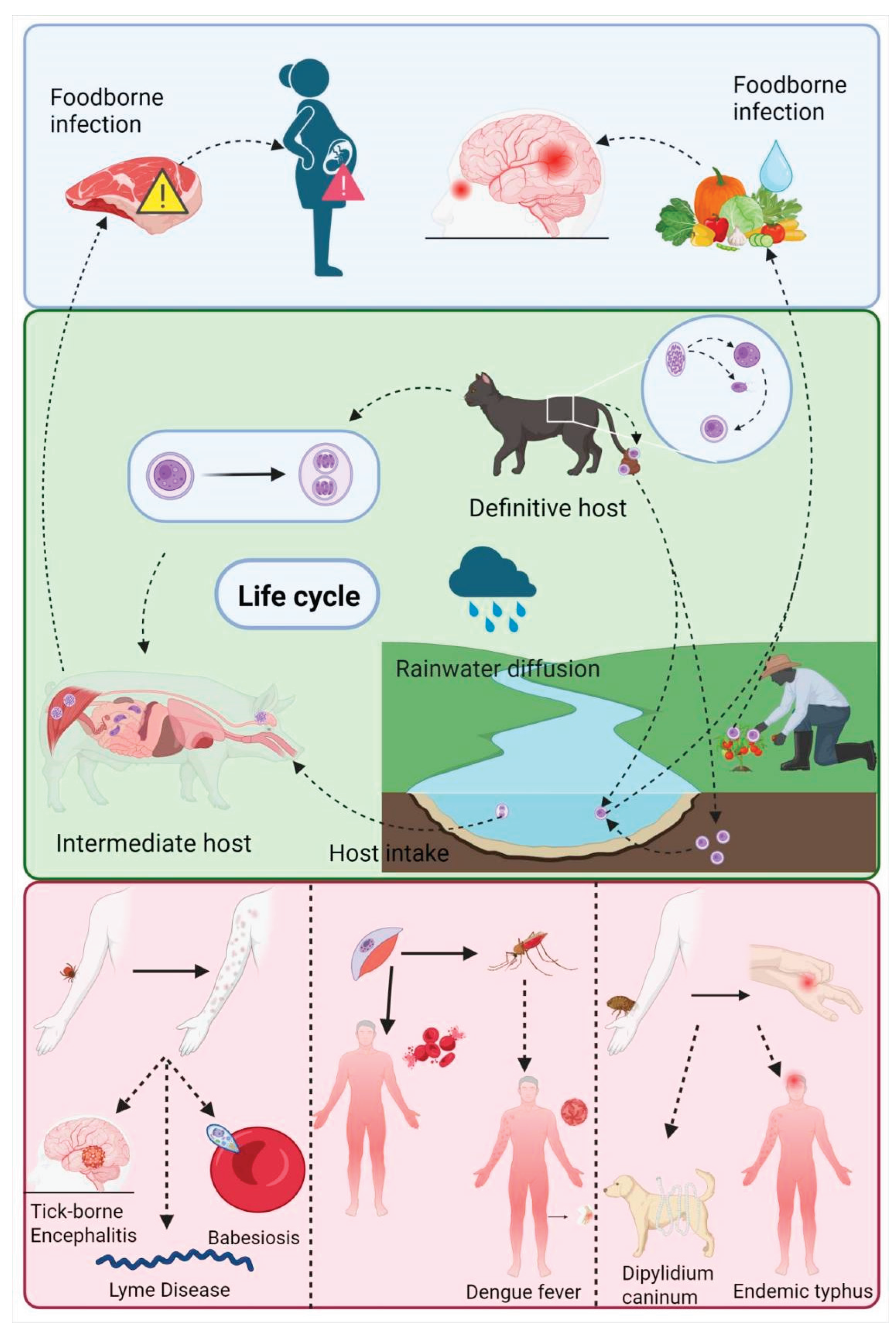
1. Introduction
2. Advantages of Nano Transdermal Delivery System
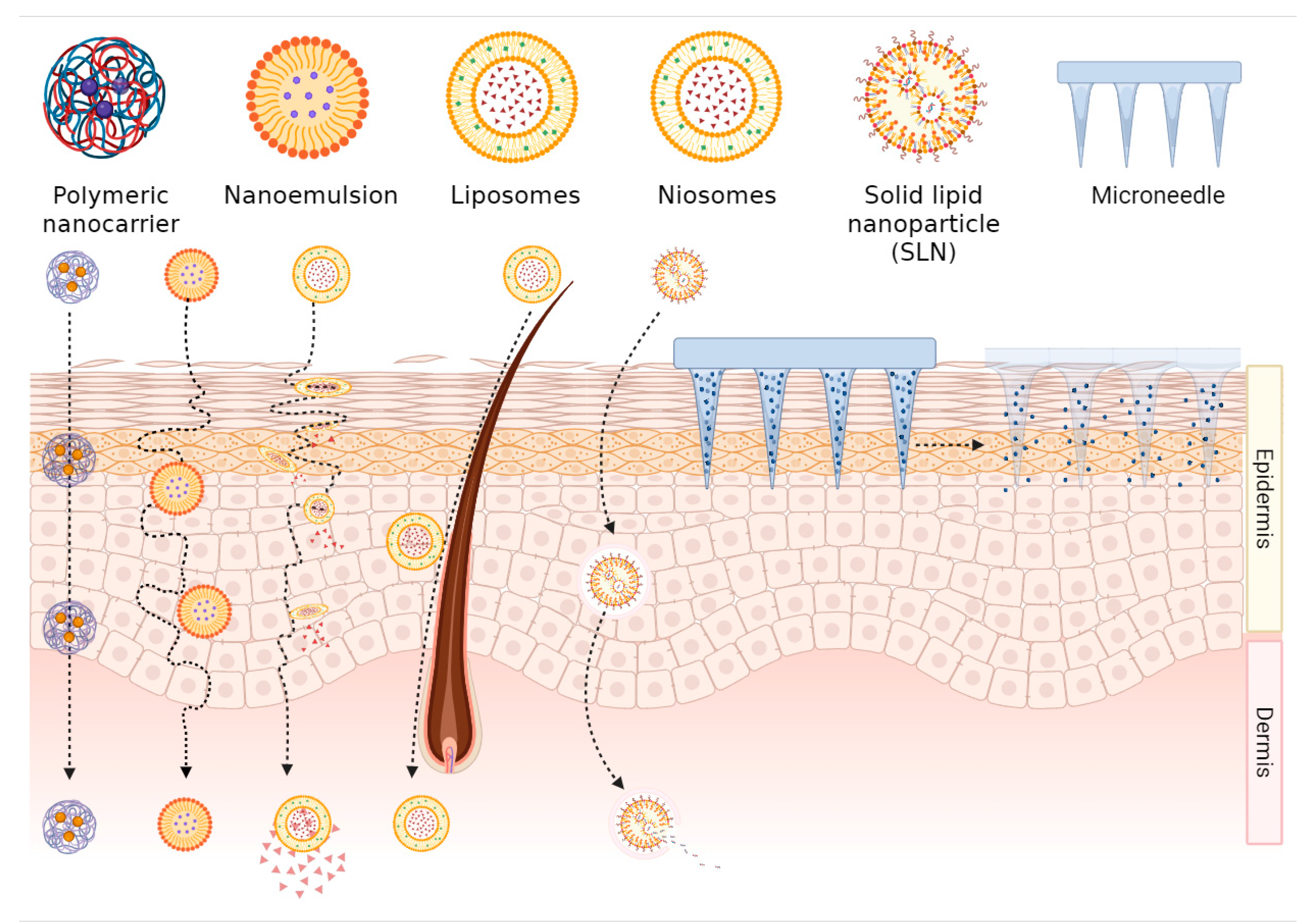
2.1. Transdermal Mechanism of Nanoformulations
2.2. Controlled Release and Targeted Delivery of Nanoformulations
3. Application of Nanoformulations in the Treatment of Parasitic Diseases
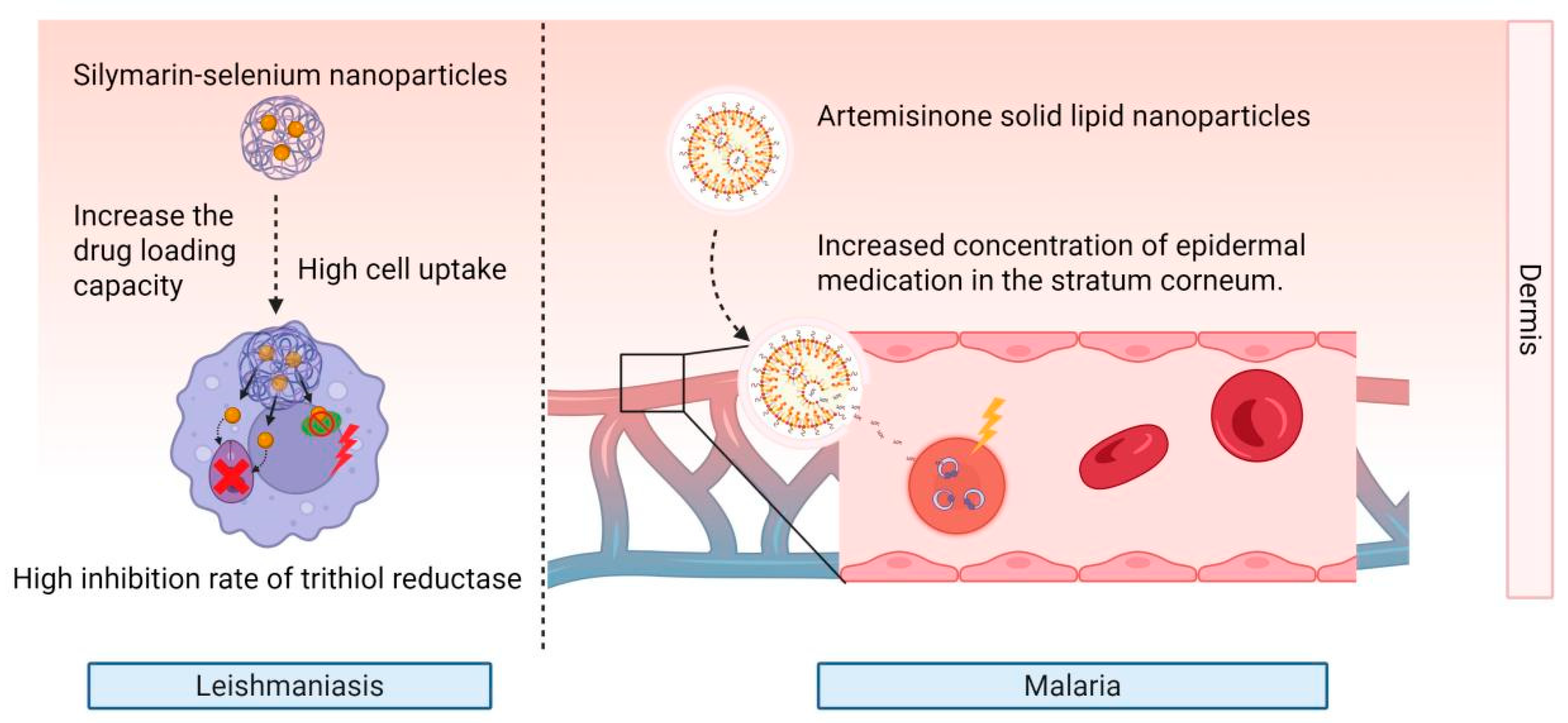
3.1. Leishmaniasis
3.2. Malaria
4. Nanoformulations in Broad-Spectrum Antiparasitic Drugs
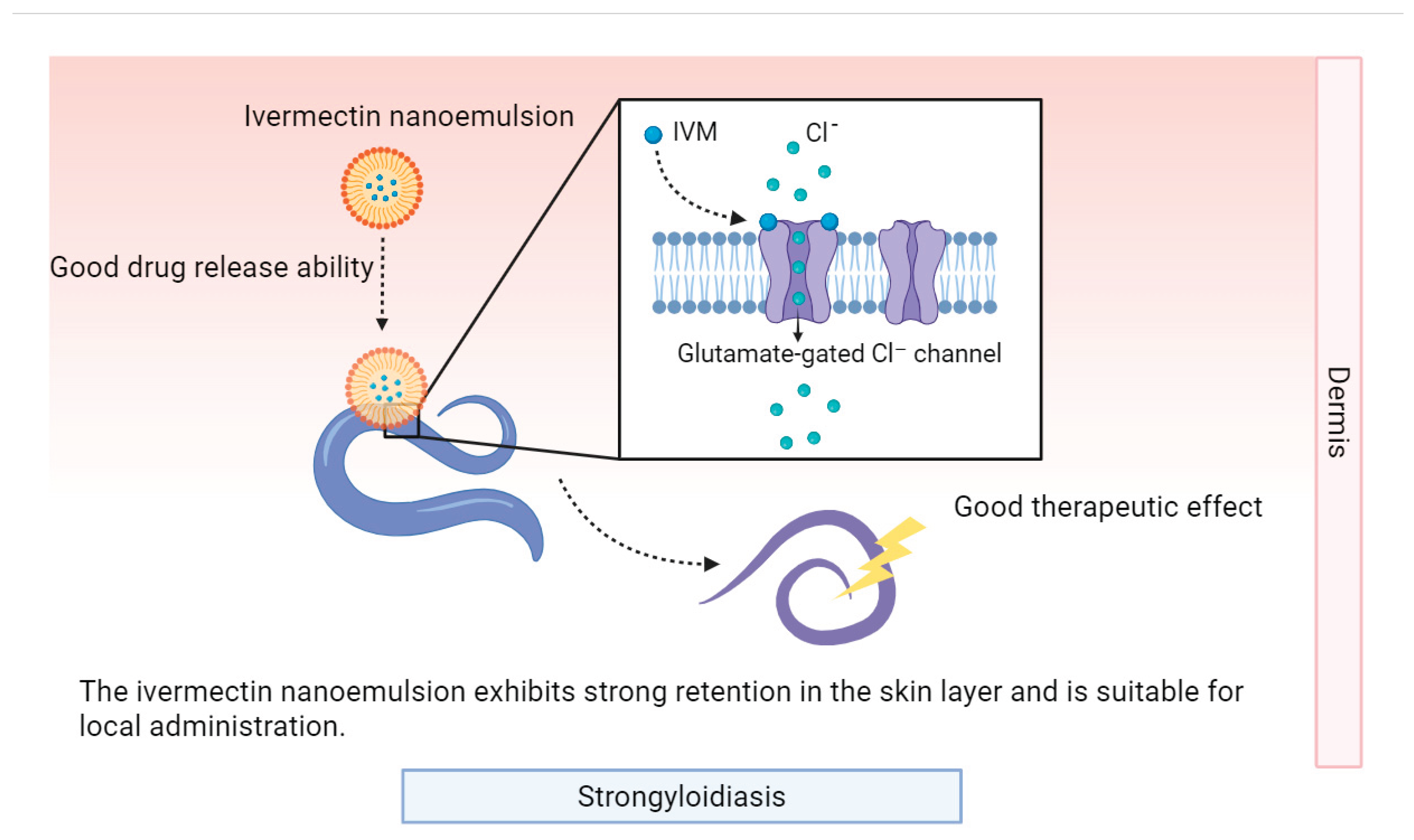
4.1. Avermectin-Class Drugs
4.2. Benzimidazole-Class Drugs
5. Summary and Perspectives
Author Contributions
Acknowledgments
Conflict of Interest
References
- Global Report on Neglected Tropical Diseases 2024.
- Otranto, D.; Strube, C.; Xiao, L. Zoonotic Parasites: The One Health Challenge. Parasitol Res 2021, 120, 4073–4074. [Google Scholar] [CrossRef]
- Alkilani, A.Z.; McCrudden, M.T.C.; Donnelly, R.F. Transdermal Drug Delivery: Innovative Pharmaceutical Developments Based on Disruption of the Barrier Properties of the Stratum Corneum. Pharmaceutics 2015, 7, 438–470. [Google Scholar] [CrossRef] [PubMed]
- Bruno, B.J.; Miller, G.D.; Lim, C.S. Basics and Recent Advances in Peptide and Protein Drug Delivery. Ther Deliv 2013, 4, 1443–1467. [Google Scholar] [CrossRef] [PubMed]
- Patlolla, R.R.; Desai, P.R.; Belay, K.; Singh, M.S. Trans Location of Cell Penetrating Peptide Engrafted Nanoparticles across Skin Layers. Biomaterials 2010, 31, 5598–5607. [Google Scholar] [CrossRef]
- Ashtikar, M.; Langelüddecke, L.; Fahr, A.; Deckert, V. Tip-Enhanced Raman Scattering for Tracking of Invasomes in the Stratum Corneum. Biochimica et Biophysica Acta (BBA) - General Subjects 2017, 1861, 2630–2639. [Google Scholar] [CrossRef] [PubMed]
- Schoellhammer, C.M.; Blankschtein, D.; Langer, R. Skin Permeabilization for Transdermal Drug Delivery: Recent Advances and Future Prospects. Expert Opin. Drug Deliv. 2014, 11, 393–407. [Google Scholar] [CrossRef]
- Zhou, X.; Hao, Y.; Yuan, L.; Pradhan, S.; Shrestha, K.; Pradhan, O.; Liu, H.; Li, W. Nano-Formulations for Transdermal Drug Delivery: A Review. Chinese Chemical Letters 2018, 29, 1713–1724. [Google Scholar] [CrossRef]
- Weng, Y.; Liu, J.; Jin, S.; Guo, W.; Liang, X.; Hu, Z. Nanotechnology-Based Strategies for Treatment of Ocular Disease. Acta Pharmaceutica Sinica B 2017, 7, 281–291. [Google Scholar] [CrossRef]
- Kayser, O.; Kiderlen, A.F. Delivery Strategies for Antiparasitics. Expert Opin. Investig. Drugs 2003. [Google Scholar] [CrossRef]
- Laouini, A.; Charcosset, C.; Fessi, H.; Holdich, R.G.; Vladisavljević, G.T. Preparation of Liposomes: A Novel Application of Microengineered Membranes–From Laboratory Scale to Large Scale. Colloids and Surfaces B: Biointerfaces 2013, 112, 272–278. [Google Scholar] [CrossRef]
- Kato, A.; Ishibashi, Y.; Miyake, Y. Effect of Egg Yolk Lecithin on Transdermal Delivery of Bunazosin Hydrochloride. Journal of Pharmacy and Pharmacology 1987, 39, 399–400. [Google Scholar] [CrossRef]
- Kirjavainen, M.; Urtti, A.; Jääskeläinen, I.; Marjukka Suhonen, T.; Paronen, P.; Valjakka-Koskela, R.; Kiesvaara, J.; Mönkkönen, J. Interaction of Liposomes with Human Skin in Vitro — The Influence of Lipid Composition and Structure. Biochimica et Biophysica Acta (BBA) - Lipids and Lipid Metabolism 1996, 1304, 179–189. [Google Scholar] [CrossRef]
- Kirjavainen, M.; Mönkkönen, J.; Saukkosaari, M.; Valjakka-Koskela, R.; Kiesvaara, J.; Urtti, A. Phospholipids Affect Stratum Corneum Lipid Bilayer Fluidity and Drug Partitioning into the Bilayers. Journal of Controlled Release 1999, 58, 207–214. [Google Scholar] [CrossRef] [PubMed]
- El Maghraby, G.M.M.; Williams, A.C.; Barry, B.W. Can Drug-Bearing Liposomes Penetrate Intact Skin? Journal of Pharmacy and Pharmacology 2006, 58, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Akram, M.W.; Jamshaid, H.; Rehman, F.U.; Zaeem, M.; Khan, J.Z.; Zeb, A. Transfersomes: A Revolutionary Nanosystem for Efficient Transdermal Drug Delivery. AAPS PharmSciTech 2021, 23, 7. [Google Scholar] [CrossRef] [PubMed]
- Sala, M.; Diab, R.; Elaissari, A.; Fessi, H. Lipid Nanocarriers as Skin Drug Delivery Systems: Properties, Mechanisms of Skin Interactions and Medical Applications. International Journal of Pharmaceutics 2018, 535, 1–17. [Google Scholar] [CrossRef]
- Raj, A.; C. , S.C.; V., A.N.; Ivon, A.; M., N.F.N.; P., N.N.P. Lipid-Based Vesicles: A Non-Invasive Tool for Transdermal Drug Delivery. J Pharm Innov 2022, 17, 1039–1052. [Google Scholar] [CrossRef]
- Zhou, X.; Hao, Y.; Yuan, L.; Pradhan, S.; Shrestha, K.; Pradhan, O.; Liu, H.; Li, W. Nano-Formulations for Transdermal Drug Delivery: A Review. Chinese Chemical Letters 2018, 29, 1713–1724. [Google Scholar] [CrossRef]
- Khan, A.U.; Jamshaid, H.; Din, F. ud; Zeb, A.; Khan, G.M. Designing, Optimization and Characterization of Trifluralin Transfersomal Gel to Passively Target Cutaneous Leishmaniasis. J. Pharm. Sci. 2022, 111, 1798–1811. [Google Scholar] [CrossRef]
- Bashir, S.; Shabbir, K.; Din, F.U.; Khan, S.U.; Ali, Z.; Khan, B.A.; Kim, D.W.; Khan, G.M. Nitazoxanide and Quercetin Co-Loaded Nanotransfersomal Gel for Topical Treatment of Cutaneous Leishmaniasis with Macrophage Targeting and Enhanced Anti-Leishmanial Effect. Heliyon 2023, 9, e21939. [Google Scholar] [CrossRef]
- Shen, S.; Liu, S.-Z.; Zhang, Y.-S.; Du, M.-B.; Liang, A.-H.; Song, L.-H.; Ye, Z.-G. Compound Antimalarial Ethosomal Cataplasm: Preparation, Evaluation, and Mechanism of Penetration Enhancement. Int. J. Nanomed. 2015, 10, 4239–4253. [Google Scholar] [CrossRef]
- A. , N.; Kovooru, L.; Behera, A.K.; Kumar, K.P.P.; Srivastava, P. A Critical Review of Synthesis Procedures, Applications and Future Potential of Nanoemulsions. Advances in Colloid and Interface Science 2021, 287, 102318. [Google Scholar] [CrossRef]
- Sghier, K.; Mur, M.; Veiga, F.; Paiva-Santos, A.C.; Pires, P.C. Novel Therapeutic Hybrid Systems Using Hydrogels and Nanotechnology: A Focus on Nanoemulgels for the Treatment of Skin Diseases. Gels 2024, 10, 45. [Google Scholar] [CrossRef]
- Coelho, D.; Veleirinho, B.; Mazzarino, L.; Alberti, T.; Buzanello, E.; Oliveira, R.E.; Yunes, R.A.; Moraes, M.; Steindel, M.; Maraschin, M. Polyvinyl Alcohol-Based Electrospun Matrix as a Delivery System for Nanoemulsion Containing Chalcone against Leishmania (Leishmania) Amazonensis. Colloids and Surfaces B: Biointerfaces 2021, 198, 111390. [Google Scholar] [CrossRef] [PubMed]
- Garcia, D.J.; Fernandez-Culma, M.; Upegui, Y.A.; Rios-Vasquez, L.A.; Quinones, W.; Ocampo-Cardona, R.; Echeverri, F.; Velez, I.D.; Robledo, S.M. Nanoemulsions for Increased Penetrability and Sustained Release of Leishmanicidal Compounds. Arch. Pharm. 2023, 356, e202300108. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Han, M.-R.; Park, J.-H. Polymer Microneedles for Transdermal Drug Delivery. Journal of Drug Targeting 2013, 21, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Zhang, L.; Jiang, X.; Li, L.; Wu, S.; Yuan, X.; Cheng, H.; Jiang, X.; Gou, M. 3D-Printed Microneedle Arrays for Drug Delivery. Journal of Controlled Release 2022, 350, 933–948. [Google Scholar] [CrossRef]
- Gunawan, M.; Bestari, A.N.; Ramadon, D.; Efendi, A.; Boonkanokwong, V. Combination of Lipid-Based Nanoparticles with Microneedles as a Promising Strategy for Enhanced Transdermal Delivery Systems: A Comprehensive Review. Journal of Drug Delivery Science and Technology 2025, 107, 106807. [Google Scholar] [CrossRef]
- Dumitriu Buzia, O.; Păduraru, A.M.; Stefan, C.S.; Dinu, M.; Cocoș, D.I.; Nwabudike, L.C.; Tatu, A.L. Strategies for Improving Transdermal Administration: New Approaches to Controlled Drug Release. Pharmaceutics 2023, 15, 1183. [Google Scholar] [CrossRef]
- Zare, M.R.; Khorram, M.; Barzegar, S.; Sarkari, B.; Asgari, Q.; Ahadian, S.; Zomorodian, K. Dissolvable Carboxymethyl Cellulose/Polyvinylpyrrolidone Microneedle Arrays for Transdermal Delivery of Amphotericin B to Treat Cutaneous Leishmaniasis. International Journal of Biological Macromolecules 2021, 182, 1310–1321. [Google Scholar] [CrossRef]
- Mahfufah, U.; Fitri Sultan, N.A.; Nurul Fitri, A.M.; Elim, D.; Sya’ban Mahfud, M.A.; Wafiah, N.; Ardita Friandini, R.; Chabib, L.; Aliyah; Permana, A. D. Application of Multipolymers System in the Development of Hydrogel-Forming Microneedle Integrated with Polyethylene Glycol Reservoir for Transdermal Delivery of Albendazole. European Polymer Journal 2023, 183, 111762. [Google Scholar] [CrossRef]
- Sharma, S.; Rawat, K.; Bohidar, H.B. Role of Nanomedicines in Controlling Malaria: A Review. Curr. Top. Med. Chem. 2023, 23, 1477–1488. [Google Scholar] [CrossRef]
- Nahanji, M.K.; Mahboobian, M.M.; Harchegani, A.L.; Mohebali, M.; Fallah, M.; Nourian, A.; Motavallihaghi, S.; Maghsood, A.H. Enhancing the Efficacy of Fluconazole against Leishmania Major: Formulation and Evaluation of FLZ-Nanoemulsions for Topical Delivery. Biomedicine & Pharmacotherapy 2024, 178, 117109. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, R. Exploring the Potential of Antimalarial Nanocarriers as a Novel Therapeutic Approach. Journal of Molecular Graphics and Modelling 2023. [Google Scholar] [CrossRef]
- Nemati, S.; Mottaghi, M.; Karami, P.; Mirjalali, H. Development of Solid Lipid Nanoparticles-Loaded Drugs in Parasitic Diseases. Discov. Nano. 2024, 19, 7. [Google Scholar] [CrossRef]
- Azim, M.; Khan, S.A.; Osman, N.; Sadozai, S.K.; Khan, I. Ameliorated Delivery of Amphotericin B to Macrophages Using Chondroitin Sulfate Surface-Modified Liposome Nanoparticles. Drug Development and Industrial Pharmacy 2025, 51, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Aderibigbe, B.; Sadiku, E.; Jayaramudu, J.; Sinha Ray, S. Controlled Dual Release Study of Curcumin and a 4-aminoquinoline Analog from Gum Acacia Containing Hydrogels. J of Applied Polymer Sci 2015, 132, app.41613. [Google Scholar] [CrossRef]
- Aderibigbe, B.A.; Mhlwatika, Z. Dual Release Kinetics of Antimalarials from Soy Protein Isolate-Carbopol-Polyacrylamide Based Hydrogels. Journal of Applied Polymer Science 2016, 133. [Google Scholar] [CrossRef]
- Guo, D.; Dou, D.; Li, X.; Zhang, Q.; Bhutto, Z.A.; Wang, L. Ivermection-Loaded Solid Lipid Nanoparticles: Preparation, Characterisation, Stability and Transdermal Behaviour. Artificial Cells, Nanomedicine, and Biotechnology 2018, 46, 255–262. [Google Scholar] [CrossRef]
- Rahimi, M.; Seyyed Tabaei, S.J.; Ziai, S.A.; Sadri, M. Anti-Leishmanial Effects of Chitosan-Polyethylene Oxide Nanofibers Containing Berberine: An Applied Model for Leishmania Wound Dressing. Iran J Med Sci 2020, 45, 286–297. [Google Scholar] [CrossRef]
- Seyyed Tabaei, S.J.; Rahimi, M.; Akbaribazm, M.; Ziai, S.A.; Sadri, M.; Shahrokhi, S.R.; Rezaei, M.S. Chitosan-Based Nano-Scaffolds as Antileishmanial Wound Dressing in BALB/c Mice Treatment: Characterization and Design of Tissue Regeneration. Iranian Journal of Basic Medical Sciences 2020, 23, 788–799. [Google Scholar] [CrossRef] [PubMed]
- Golshirazi, A.; Mohammadzadeh, M.; Labbaf, S. The Synergistic Potential of Hydrogel Microneedles and Nanomaterials: Breaking Barriers in Transdermal Therapy. Macromolecular Bioscience 2025, 25, 2400228. [Google Scholar] [CrossRef]
- Alex, M.; Alsawaftah, N.M.; Husseini, G.A. State-of-All-the-Art and Prospective Hydrogel-Based Transdermal Drug Delivery Systems. Applied Sciences 2024, 14, 2926. [Google Scholar] [CrossRef]
- Dehghani, F.; Farhadian, N.; Goyonlo, V.M.; Ahmadi, O. A Novel Topical Formulation of the Leishmaniasis Drug Glucantime as a Nanostructured Lipid Carrier-Based Hydrogel. Am. J. Trop. Med. Hyg. 2023, 109, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Rabia, S.; Khaleeq, N.; Batool, S.; Dar, M.J.; Kim, D.W.; Din, F.-U.; Khan, G.M. Rifampicin-Loaded Nanotransferosomal Gel for Treatment of Cutaneous Leishmaniasis: Passive Targeting Via Topical Route. Nanomedicine (Lond.) 2020, 15, 183–203. [Google Scholar] [CrossRef]
- Tyagi, R.K.; Garg, N.K.; Jadon, R.; Sahu, T.; Katare, O.P.; Dalai, S.K.; Awasthi, A.; Marepally, S.K. Elastic Liposome-Mediated Transdermal Immunization Enhanced the Immunogenicity of P. Falciparum Surface Antigen, MSP-119. Vaccine 2015, 33, 4630–4638. [Google Scholar] [CrossRef]
- Tyagi, R.K.; Garg, N.K.; Dalai, S.K.; Awasthi, A. Transdermal Immunization of P-Falciparum Surface Antigen (MSP-119) via Elastic Liposomes Confers Robust Immunogenicity. Human Vaccines Immunother. 2016, 12, 990–992. [Google Scholar] [CrossRef]
- Puttappa, N.; Kumar, R.S.; Yamjala, K. Artesunate-Quercetin/Luteolin Dual Drug Nanofacilitated Synergistic Treatment for Malaria: A Plausible Approach to Overcome Artemisinin Combination Therapy Resistance. Medical Hypotheses 2017, 109, 176–180. [Google Scholar] [CrossRef]
- Courtenay, O.; Peters, N.C.; Rogers, M.E.; Bern, C. Combining Epidemiology with Basic Biology of Sand Flies, Parasites, and Hosts to Inform Leishmaniasis Transmission Dynamics and Control. PLOS Pathogens 2017, 13, e1006571. [Google Scholar] [CrossRef]
- Burza, S.; Croft, S.L.; Boelaert, M. Leishmaniasis. The Lancet 2018, 392, 951–970. [Google Scholar] [CrossRef]
- Van Assche, T.; Deschacht, M.; da Luz, R.A.I.; Maes, L.; Cos, P. Leishmania–Macrophage Interactions: Insights into the Redox Biology. Free Radical Biology and Medicine 2011, 51, 337–351. [Google Scholar] [CrossRef]
- Hussain, H.; Al-Harrasi, A.; Al-Rawahi, A.; Green, I.R.; Gibbons, S. Fruitful Decade for Antileishmanial Compounds from 2002 to Late 2011. Chem. Rev. 2014, 114, 10369–10428. [Google Scholar] [CrossRef] [PubMed]
- Reithinger, R.; Dujardin, J.-C.; Louzir, H.; Pirmez, C.; Alexander, B.; Brooker, S. Cutaneous Leishmaniasis. The Lancet Infectious Diseases 2007, 7, 581–596. [Google Scholar] [CrossRef] [PubMed]
- Olliaro, P.L.; Guerin, P.J.; Gerstl, S.; Haaskjold, A.A.; Rottingen, J.-A.; Sundar, S. Treatment Options for Visceral Leishmaniasis: A Systematic Review of Clinical Studies Done in India, 1980–2004. The Lancet Infectious Diseases 2005, 5, 763–774. [Google Scholar] [CrossRef] [PubMed]
- Sundar, S.; Chakravarty, J. An Update on Pharmacotherapy for Leishmaniasis. Expert Opinion on Pharmacotherapy 2015, 16, 237–252. [Google Scholar] [CrossRef]
- De Souza, A.; Marins, D.S.S.; Mathias, S.L.; Monteiro, L.M.; Yukuyama, M.N.; Scarim, C.B.; Löbenberg, R.; Bou-Chacra, N.A. Promising Nanotherapy in Treating Leishmaniasis. International Journal of Pharmaceutics 2018, 547, 421–431. [Google Scholar] [CrossRef]
- Santos, S.S.; de Araújo, R.V.; Giarolla, J.; Seoud, O.E.; Ferreira, E.I. Searching for Drugs for Chagas Disease, Leishmaniasis and Schistosomiasis: A Review. International Journal of Antimicrobial Agents 2020, 55, 105906. [Google Scholar] [CrossRef]
- Alishahi, M.; Khorram, M.; Asgari, Q.; Davani, F.; Goudarzi, F.; Emami, A.; Arastehfar, A.; Zomorodian, K. Glucantime-Loaded Electrospun Core-Shell Nanofibers Composed of Poly(Ethylene Oxide)/Gelatin-Poly(Vinyl Alcohol)/Chitosan as Dressing for Cutaneous Leishmaniasis. International Journal of Biological Macromolecules 2020, 163, 288–297. [Google Scholar] [CrossRef]
- Mahmoud Abd-Alaziz, D.; Mansour, M.; Nasr, M.; Sammour, O. Tailored Green Synthesized Silymarin-Selenium Nanoparticles: Topical Nanocarrier of Promising Antileishmanial Activity. International Journal of Pharmaceutics 2024, 660, 124275. [Google Scholar] [CrossRef]
- Lanza, J.S.; Vucen, S.; Flynn, O.; Donadei, A.; Cojean, S.; Loiseau, P.M.; Fernandes, A.P.S.M.; Frézard, F.; Moore, A.C. A TLR9-Adjuvanted Vaccine Formulated into Dissolvable Microneedle Patches or Cationic Liposomes Protects against Leishmaniasis after Skin or Subcutaneous Immunization. International Journal of Pharmaceutics 2020, 586, 119390. [Google Scholar] [CrossRef]
- Maria Jose Alves De, O.; Regina, M.; Lucia Almeida, B.; Ademar Benevolo, L.; Valdir Sabbaga, A.; Duclerc Fernandes, P. Topical Treatment of Cutaneous Leishmaniasis: Wound Reduction in Mice Using N-Methyl Glucamine from PVP and Nano Clay Membranes. J Dermatol Res Ther 2016, 2. [Google Scholar] [CrossRef]
- Oliveira, M.J.A.D.; Villegas, G.M.E.; Motta, F.D.; Fabela-Sánchez, O.; Espinosa-Roa, A.; Fotoran, W.L.; Peixoto, J.C.; Tano, F.T.; Lugão, A.B.; Vásquez, P.A.S. Influence of Gamma Radiation on Amphotericin B Incorporated in PVP Hydrogel as an Alternative Treatment for Cutaneous Leishmaniosis. Acta Tropica 2021, 215, 105805. [Google Scholar] [CrossRef]
- Puttappa, N.; Kumar, R.S.; Kuppusamy, G.; Radhakrishnan, A. Nano-Facilitated Drug Delivery Strategies in the Treatment of Plasmodium Infection. Acta Tropica 2019, 195, 103–114. [Google Scholar] [CrossRef]
- Mishra, A.; Qamar, F.; Ashrafi, K.; Fatima, S.; Samim, M.; Mohmmed, A.; Abdin, M.Z. Emerging Nanotechnology-Driven Drug Delivery Solutions for Malaria: Addressing Drug Resistance and Improving Therapeutic Success. International Journal of Pharmaceutics 2025, 670, 125163. [Google Scholar] [CrossRef]
- Baruah, U.K.; Gowthamarajan, K.; Ravisankar, V.; Karri, V.V.S.R.; Simhadri, P.K.; Singh, V. Optimisation of Chloroquine Phosphate Loaded Nanostructured Lipid Carriers Using Box-Behnken Design and Its Antimalarial Efficacy. J. Drug Target. 2018, 26, 576–591. [Google Scholar] [CrossRef]
- Kuntworbe, N.; Martini, N.; Shaw, J.; Al-Kassas, R. Malaria Intervention Policies and Pharmaceutical Nanotechnology as a Potential Tool for Malaria Management. Drug Development Research 2012, 73, 167–184. [Google Scholar] [CrossRef]
- Santos-Magalhães, N.S.; Mosqueira, V.C.F. Nanotechnology Applied to the Treatment of Malaria. Advanced Drug Delivery Reviews 2010, 62, 560–575. [Google Scholar] [CrossRef] [PubMed]
- Eastman, R.T.; Fidock, D.A. Artemisinin-Based Combination Therapies: A Vital Tool in Efforts to Eliminate Malaria. Nat Rev Microbiol 2009, 7, 864–874. [Google Scholar] [CrossRef]
- Zech, J.; Dzikowski, R.; Simantov, K.; Golenser, J.; Maeder, K. Transdermal Delivery of Artemisinins for Treatment of Pre-Clinical Cerebral Malaria. Int. J. Parasitol.-Drugs Drug Resist. 2021, 16, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, A.; Mazumder, A.; Fox, L.T.; Brümmer, A.; Gerber, M.; Du Preez, J.L.; Haynes, R.K.; Du Plessis, J. In Vitro Skin Permeation of Artemisone and Its Nano-Vesicular Formulations. International Journal of Pharmaceutics 2016, 503, 1–7. [Google Scholar] [CrossRef]
- Aderibigbe, B.A.; Mhlwatika, Z. Dual Release Kinetics of Antimalarials from Soy Protein Isolate-carbopol-polyacrylamide Based Hydrogels. J of Applied Polymer Sci 2016, 133, app.43918. [Google Scholar] [CrossRef]
- Dandekar, P.P.; Jain, R.; Patil, S.; Dhumal, R.; Tiwari, D.; Sharma, S.; Vanage, G.; Patravale, V. Curcumin-Loaded Hydrogel Nanoparticles: Application in Anti-Malarial Therapy and Toxicological Evaluation. Journal of Pharmaceutical Sciences 2010, 99, 4992–5010. [Google Scholar] [CrossRef]
- Alfrd Mavondo, G.A.; Tagumirwa, M.C. Asiatic Acid-Pectin Hydrogel Matrix Patch Transdermal Delivery System Influences Parasitaemia Suppression and Inflammation Reduction in P. Berghei Murine Malaria Infected Sprague–Dawley Rats. Asian Pacific Journal of Tropical Medicine 2016, 9, 1172–1180. [Google Scholar] [CrossRef]
- Nnamani, P.O.; Hansen, S.; Windbergs, M.; Lehr, C.-M. Development of Artemether-Loaded Nanostructured Lipid Carrier (NLC) Formulation for Topical Application. International Journal of Pharmaceutics 2014, 477, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Ananda, P.W.R.; Elim, D.; Zaman, H.S.; Muslimin, W.; Tunggeng, M.G.R.; Permana, A.D. Combination of Transdermal Patches and Solid Microneedles for Improved Transdermal Delivery of Primaquine. International Journal of Pharmaceutics 2021, 609, 121204. [Google Scholar] [CrossRef] [PubMed]
- Permana, A.D.; Paredes, A.J.; Zanutto, F.V.; Amir, Muh. N.; Ismail, I.; Bahar, Muh.A.; Sumarheni; Palma, S.D.; Donnelly, R.F. Albendazole Nanocrystal-Based Dissolving Microneedles with Improved Pharmacokinetic Performance for Enhanced Treatment of Cystic Echinococcosis. ACS Appl. Mater. Interfaces 2021, 13, 38745–38760. [Google Scholar] [CrossRef] [PubMed]
- Devineni, J.; Pravallika, Ch.D.; Sudha Rani, B.; Nalluri, B.N. IJPER 2020, 54, s492–s504. 54. [CrossRef]
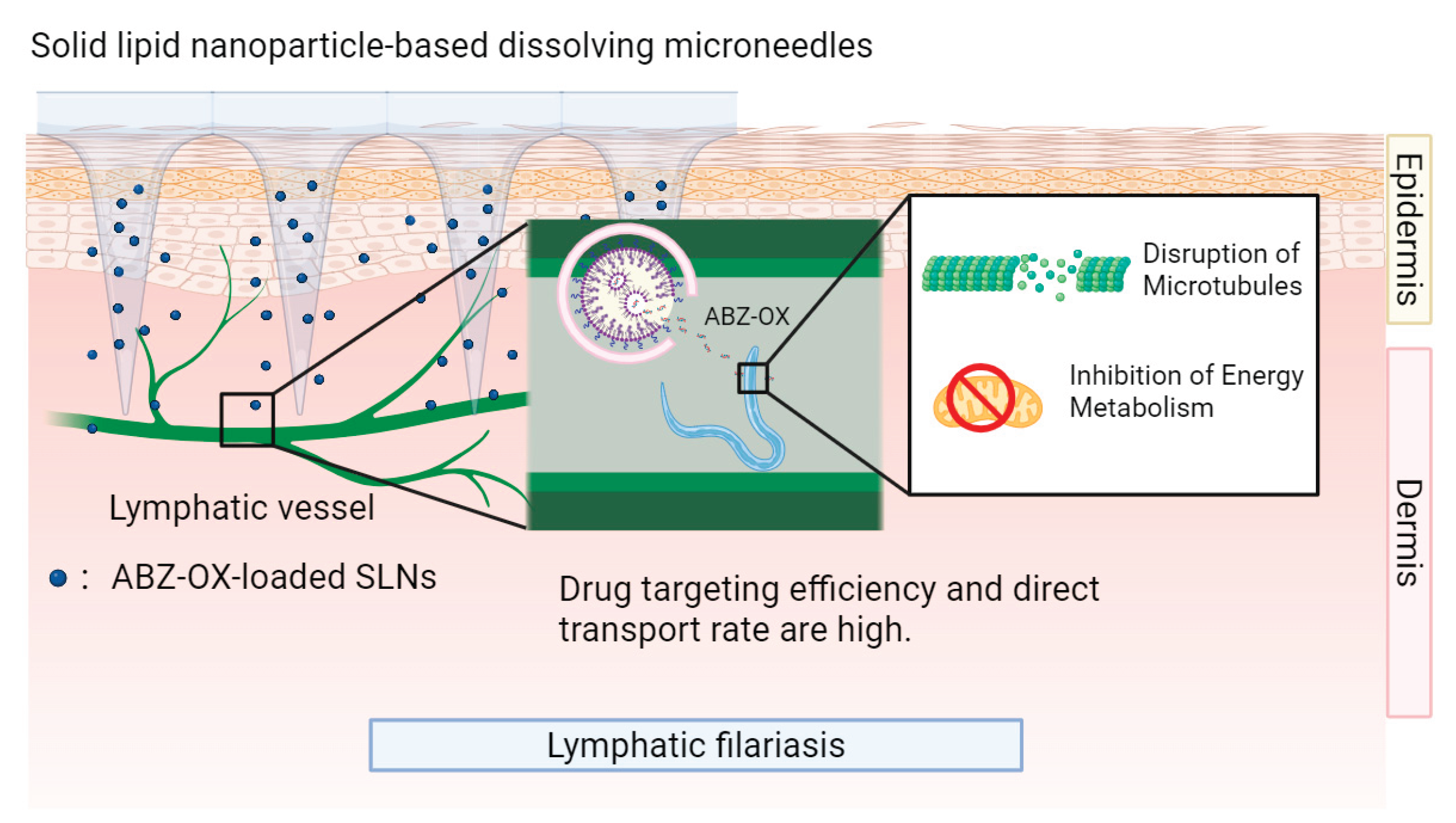
- Permana, A.D.; Tekko, I.A.; McCrudden, M.T.C.; Anjani, Q.K.; Ramadon, D.; McCarthy, H.O.; Donnelly, R.F. Solid Lipid Nanoparticle-Based Dissolving Microneedles: A Promising Intradermal Lymph Targeting Drug Delivery System with Potential for Enhanced Treatment of Lymphatic Filariasis. J. Control. Release 2019, 316, 34–52. [Google Scholar] [CrossRef]
- Manna, O.; Nditanchou, R.; Siewe Fodjo, J.; Colebunders, R. Utilization of Health Facilities and Schools in Onchocerciasis Elimination Efforts. IJID Regions 2025, 16, 100677. [Google Scholar] [CrossRef]
- Okumura, N.; Torii, A.; Suzuki, D.; Ito, K.; Iwade, K.; Takahashi, K. A Case Report of Disseminated Strongyloidiasis Following Chemoradiotherapy for Lung Cancer in a Patient Living in a Non-Endemic Area in Japan. Intern. Med. 2025. [Google Scholar] [CrossRef]
- Berger, S.N.; Rustum, A.M. A Comprehensive Study to Identify Major Degradation Products of Avermectin Active Ingredient Using High Resolution LCMS and NMR. J. Liq. Chromatogr. Relat. Technol. 2025. [Google Scholar] [CrossRef]
- de Souza, D.K.; Bockarie, M.J. Current Perspectives in the Epidemiology and Control of Lymphatic Filariasis. Clin. Microbiol. Rev. 2025, 38. [Google Scholar] [CrossRef]
- Karakoyun, Ö.; Ayhan, E.; Yıldız, İ. Effect of Ivermectin on Scabies: A Retrospective Evaluation. BMC Infect Dis 2025, 25, 937. [Google Scholar] [CrossRef] [PubMed]
- Steenekamp, E.M.; Liebenberg, W.; Lemmer, H.J.R.; Gerber, M. Formulation and Ex Vivo Evaluation of Ivermectin Within Different Nano-Drug Delivery Vehicles for Transdermal Drug Delivery. Pharmaceutics 2024, 16, 1466. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Lee, S.H.; Chia, V.D.; Chow, P.S.; Macbeath, C.; Liu, Y.; Shlieout, G. Development of Microemulsion Based Topical Ivermectin Formulations: Pre-Formulation and Formulation Studies. Colloids and Surfaces B: Biointerfaces 2020, 189, 110823. [Google Scholar] [CrossRef] [PubMed]
- Awad, H.; Rawas-Qalaji, M.; El Hosary, R.; Jagal, J.; Ahmed, I.S. Formulation and Optimization of Ivermectin Nanocrystals for Enhanced Topical Delivery. Int. J. Pharm. X 2023, 6, 100210. [Google Scholar] [CrossRef]
- Mao, Y.; Hao, T.; Zhang, H.; Gu, X.; Wang, J.; Shi, F.; Chen, X.; Guo, L.; Gao, J.; Shen, Y.; et al. Penetration Enhancer-Free Mixed Micelles for Improving Eprinomectin Transdermal c Efficiency in Animal Parasitic Infections Therapy. Int. J. Nanomed. 2024, 19, 11071–11085. [Google Scholar] [CrossRef]
- Velho, M.C.; Funk, N.L.; Deon, M.; Benvenutti, E.V.; Buchner, S.; Hinrichs, R.; Pilger, D.A.; Beck, R.C.R. Ivermectin-Loaded Mesoporous Silica and Polymeric Nanocapsules: Impact on Drug Loading, In Vitro Solubility Enhancement, and Release Performance. Pharmaceutics 2024, 16, 325. [Google Scholar] [CrossRef]
- Karpstein, T.; Kalamatianou, A.; Keller, S.; Spane, P.; Haberli, C.; Odermatt, A.; Blacque, O.; Cariou, K.; Gasser, G.; Keiser, J. Synthesis and Multidisciplinary Preclinical Investigations of Ferrocenyl, Ruthenocenyl, and Benzyl Derivatives of Thiabendazole as New Drug Candidates against Soil-Transmitted Helminth Infections. ACS Infect. Dis. 2025, 11, 2037–2047. [Google Scholar] [CrossRef]
- Bai, S.; Zhang, M.; Tang, S.; Li, M.; Wu, R.; Wan, S.; Chen, L.; Wei, X.; Li, F. Research Progress on Benzimidazole Fungicides: A Review. Molecules 2024, 29, 1218. [Google Scholar] [CrossRef]
| Indication | Nanoformulation | Compounds | Advantages | References |
|---|---|---|---|---|
| Leishmaniasis | Transfersomes | Trifluralin | High transdermal efficiency, high encapsulation efficiency, sustained release, reduced IC50 for Leishmania pathogens, high inhibition rate of amastigotes | [20] |
| Transfersomes | Nitazoxanide-quercetin | Enhanced skin permeation, increased macrophage uptake, higher CC50, smaller lesion size, low systemic toxicity | [21] | |
| Nanoemulsions | 3’-(Trifluoromethyl)-chalcone | High dermal permeation amount, high skin retention | [25] | |
| Nanoemulsions | C6I/TC1/TC2 | Enhanced skin permeation, Sustained release, high parasiticidal activity, low macrophage cytotoxicity | [26] | |
| Electrospun core-shell nanofibers | Glucantime | Stable drug release, maintenance of effective drug concentration for a long time, sustained therapeutic effect | [59] | |
| Nanoparticles | Silymarin-selenium | High drug loading capacity, high skin deposition rate, significant reduction of local treatment toxicity | [60] | |
| Transfersomes | Rifampicin | High skin permeability, targeted reduction of IC50 value | [46] | |
| Nanostructured lipid carrier | Glucantime | Controlled drug release, enhanced skin retention, reduced systemic toxicity | [45] | |
| Nanofibers | Berberine | Gradient release, excellent biocompatibility, stable release rate | [33,34] | |
| Microneedle | Aphotericin B | Improved skin permeability, minimal cellular damage | [31] | |
| Malaria | Ethosomes | Artesunate and Febrifugine | High cumulative permeation, high efficiency | [22] |
| Solid lipid nanoparticles | Artemisone | High skin delivery concentration | [71] | |
| Elastic liposomes | PfMSP-119 | Efficient targeting, long-lasting immune response | ||
| Nanoparticles | Curcumin | High antimalarial activity, prolonged drug circulation time, high bioavailability, enhanced therapeutic efficacy | [47,48,73] | |
| Nanostructured lipid carrier | Artemether | High cumulative permeation rate, high drug stability, high release controllability | [75] | |
| Microneedles | Primaquine | Optimal performance, safe for long-term medication | [76] | |
| Cystic Echinococcosis | Microneedle | Albendazole | High transdermal permeation amount, safe | [32] |
| Microneedles-Nanocrystals system | Albendazole | High transdermal depth, high peak drug concentration, long half-life | [77] | |
| Lymphatic filariasis | Solid lipid nanoparticle - microneedle system | Albendazole | High drug targeting efficiency, high direct transport rate, Sustained release, reduced metabolite generation, low drug distribution in liver and kidney | [79] |
|
Scabies, Rosacea, Head lice, Trichuriasis, Onchocerciasis, Lymphatic filariasis, Strongyloidiasis |
Microemulsion | Ivermectin | Improved membrane permeability, high solubility | [86] |
| Nanocrystals | Ivermectin | High equilibrium solubility, fast dissolution rate, high dermal deposition, low side effects | [87] | |
| Nanoemulsion (NE) | Ivermectin | Highest drug concentration in stratum corneum and epidermis/dermis junction | [85] | |
| Nanoemulsion gel (NEG) | Ivermectin | Fastest delivery rate | ||
| Colloidal system (CS) | Ivermectin | Highest drug diffusion percentage, efficient delivery | ||
| Solid lipid nanoparticles | Ivermectin | Sustained-release efficacy, targeting, low systemic toxicity, few side effects | [40] | |
| Nanoparticles | Ivermectin | suitable for acute infection management | [89] | |
| Nanocapsules | Ivermectin | suitable for chronic prevention | ||
| Hybrid micelles | Eprinomectin | High permeability, low toxicity | [88] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





