1. Introduction
The impact of COVID-19 has been shown to severely compromise respiratory function in affected patients. The virus can infiltrate both the upper and lower respiratory tracts, causing significant inflammation in the alveoli of the lungs. This condition may lead to a marked decline in pulmonary function, particularly if patients do not receive timely and appropriate medical intervention [
1,
2,
3]. The respiratory system struggles to intake oxygen and expel carbon dioxide, resulting in clinical signs such as shortness of breath, persistent cough, sputum retention, and impaired daily mobility. Unresolved COVID-19 conditions, often referred to as “long COVID,” are characterized by symptoms such as persistent cough and sputum production lasting beyond six months [
3,
4].
Evidence suggests that regular exercise can help reverse symptoms and conditions associated with COVID-19. Physical activity programs can counteract muscle atrophy and fatigue observed in long COVID patients [
5,
6,
7]. Tailored exercise regimens have shown significant improvements in patients with severe long COVID symptoms, particularly in enhancing cardiorespiratory function and alleviating long COVID symptoms.
During the COVID-19 pandemic, many people stayed home and could not attend normal work or social activities. As a result, many hospitals and clinics developed telehealth services, incorporating home-based exercise regimes monitored through a telemonitoring system. These initiatives marked a new era in rehabilitation, which has continued to develop even well after the global COVID pandemic has settled. With the rapid advances in digital technology, many countries are continuing to develop these remote health monitoring services as a more cost-effective model of health care delivery [
9,
10]. The benefits of videoconferencing exercise interventions include the concurrent management of many patients and the elimination of patients travelling to the clinical centres. The downside would be the lack of direct in-person instant feedback and guidance that can be provided when patients attend therapy in the clinical setting [
11].
In response to the COVID-19 pandemic, government and non-profit organizations in Hong Kong have piloted some telehealth services aimed at reducing patients’ travel time and optimizing physical well-being [
12,
13]. These initiatives encompass three main domains: telemedicine and teleconsultation provided by medical professionals, telemonitoring of patients’ clinical data to aid in medical feedback and intervention, and tele-support through online services offering information and advice to patients and caregivers. These initiatives are integrated in the “HA Go” app, which was originally designed to enable patients to make appointments for medical consultations in public hospitals and clinics [
13]. Following the outbreak of COVID-19, the Hospital Authority in Hong Kong expanded the use of telehealth technologies, incorporating video conferencing and mobile apps to facilitate treatment follow-ups and support rehabilitation services including online exercise instructions for patients with various chronic diseases.
This study examines the effectiveness of a telehealth program designed to increase the exercise participation of young adults after COVID, and changes in cardiorespiratory function before and after exercise training is the main outcome measure.
2. Methods and Materials
2.1. Study Design
This is a quasi-experimental pre-post study design with two groups. Undergraduate students at a local college suffering from post COVID-19 complications were recruited by convenience sampling from September 2023 to December 2024. Ethics approval was obtained prior to commencing the study.
2.2. Participants
Potential participants aged between 18 to 30 years old with good past health were recruited. They were screened using the Physical Activity Readiness Questionnaire (PAR-Q) 2020 English version, and only those who answered “No” to all questions were included. For lung function assessment, apart from the standard value of spirometry, the Global Lung Function Initiative (GLI) equation [
14] was used to exclude abnormal data after obtaining the lung function test results. The American Thoracic Society (ATS) and the European Respiratory Society (ERS) recommended that the bottom 5th percentile (z-scores ≤1.645) be defined as the lower limit of normal. The z-scores of the ratios of forced expiratory volume to forced vital capacity (FEV1/FVC) and forced vital capacity (FVC) values smaller than -1.645 were considered unusually low and excluded from the analysis of this study.
Sample size estimation was conducted using G*Power 3.1.9.6. The sample size was calculated with a paired t-test with 80% (α = 0.05) and a dropout rate of 15%. Overall, 60 participants were initially included in the study. 14 participants were excluded after having abnormal baseline lung function test results. 36 cases were recruited for this telehealth exercise program, and 24 of the 65 cases were recruited as the control group to compare lung function without engaging in the telehealth exercise component.
All participants were assessed for their body composition by the InBody machine and lung function by the MIR Spiro.
Participants in the telehealth exercise group received instructions about the four-week telehealth exercise program. An exercise video was delivered to all participants through WhatsApp and uploaded to the webpage “tung-wah.odoo.com,” with a QR code provided. They were instructed to perform the exercises at least 5 times per week. The tele-exercise was essentially a 30-minute stepping exercise with a cadence of 120 bpm. It corresponded to 4.8 METs to reach the moderate intensity level for training according to ACSM standards [
15].
2.3. Exercise Intervention and Control Group
In this four-week tele-exercise initiative, participants received constant reminders via WhatsApp concerning the 10,000 steps program. Concurrently, Google or Apple pedometer applications were installed on their mobile devices to bolster their self-efficacy regarding this telehealth initiative. The gentle messages and a video link for step exercises were provided through WhatsApp. The website offered live conferences to address any difficulties in engaging with the telehealth exercise program.
The control group only received the message of the “10000 step exercise” and the benefits of step exercise in this four-week program. They did not receive any further information on the exercise program app or any soft reminder from the WhatsApp message to do the stepping exercise.
2.4. Outcome Measures
Demographic information was collected via self-reported questionnaires. Basic body measurements, including weight, height, and body mass index (BMI), were obtained using the InBody-770 device. The primary outcomes measured included the average daily step count, tracked by a pedometer application on participants’ mobile phones, and changes in lung function measures pre- and post-intervention.
Lung function tests were conducted using the Scientech Spirolab™ device. Assessments were performed both before and after a four-week intervention to evaluate improvements in lung function through spirometry, as well as participants’ reported experiences of dyspnea during daily activities.
During the assessment, four pulmonary outcomes were measured: forced expiratory volume in one second (FEV1), forced vital capacity (FVC), peak expiratory flow rate (PEFR), and the ratio of FEV1 to FVC. The FVC measurement indicates the total amount of air a person can forcibly and quickly exhale after taking a deep breath, while FEV1 reflects the amount of air exhaled in one second during the FVC test. The FVC and FEV1 ratios are commonly used in identifying specific types of lung disease.
The recorded measurements included FVC in liters, FEV1 in liters, FEV1/FVC as a percentage, and PEFR in liters per minute. The best values from three acceptable maneuvers with consistent FVC and FEV1 results were used for analysis.
To monitor compliance, participants were provided with hard copies of logbooks, where they could record whether they had completed the moderate-intensity stepping exercise each day.
2.5. Data Analysis
Data were analyzed utilizing the Statistical Package for the Social Sciences (SPSS) version 29. Descriptive statistics were computed and presented as means and standard deviations. The Chi-square test was employed to assess the homogeneity of sex across the various groups. A paired t-test was conducted to evaluate the changes before and after the 4-week telehealth exercise program, encompassing average daily step counts and values from lung function tests (FVC, FEV1, and PEFR).
3. Results
3.1. Demographic Information
Sixty undergraduate students were recruited for this pilot study. Overall, there were 36 males and 24 females. They were allocated to either the telehealth exercise (TE) group or the control group. The age and body build of the 2 groups are fairly similar (
Table 1).
3.2. Lung Function Test Results
After finishing the 4-week 10,000 step exercise program, all the participants in the TE group showed significant changes in the lung function parameters of FVC, FEV1, and FEV1/FVC. In contrast, there were no changes in these lung function test parameters in the control group. The results are summarised in
Table 2.
The significant increase in both FVC and FEV1 in the TE group after the 4 weeks’ training suggested that the participants showed improved expiratory volumes. This implies that more air can be expelled from the lungs resulting in improved lung capacity and better gaseous exchange. In the control group, there was no improvement in FVC and FEV1. This result is also consistent with the significant between-group difference for both the FVC and FEV1.
The ratios of FEV1 to FVC were within the normal range in both groups. This indicated normal pulmonary function as the participants were healthy young adults. The ratio exhibited a statistically significant change in the TE group. Conversely, the control group showed a slight decrease of about 1.4% in FEV1/FVC ratio after four weeks. The different results in the two groups contributed to a significant difference between groups (P<0.001).
With respect to PEFR, both groups demonstrated a statistically significant improvement within each group, and there was no significant between-group difference.
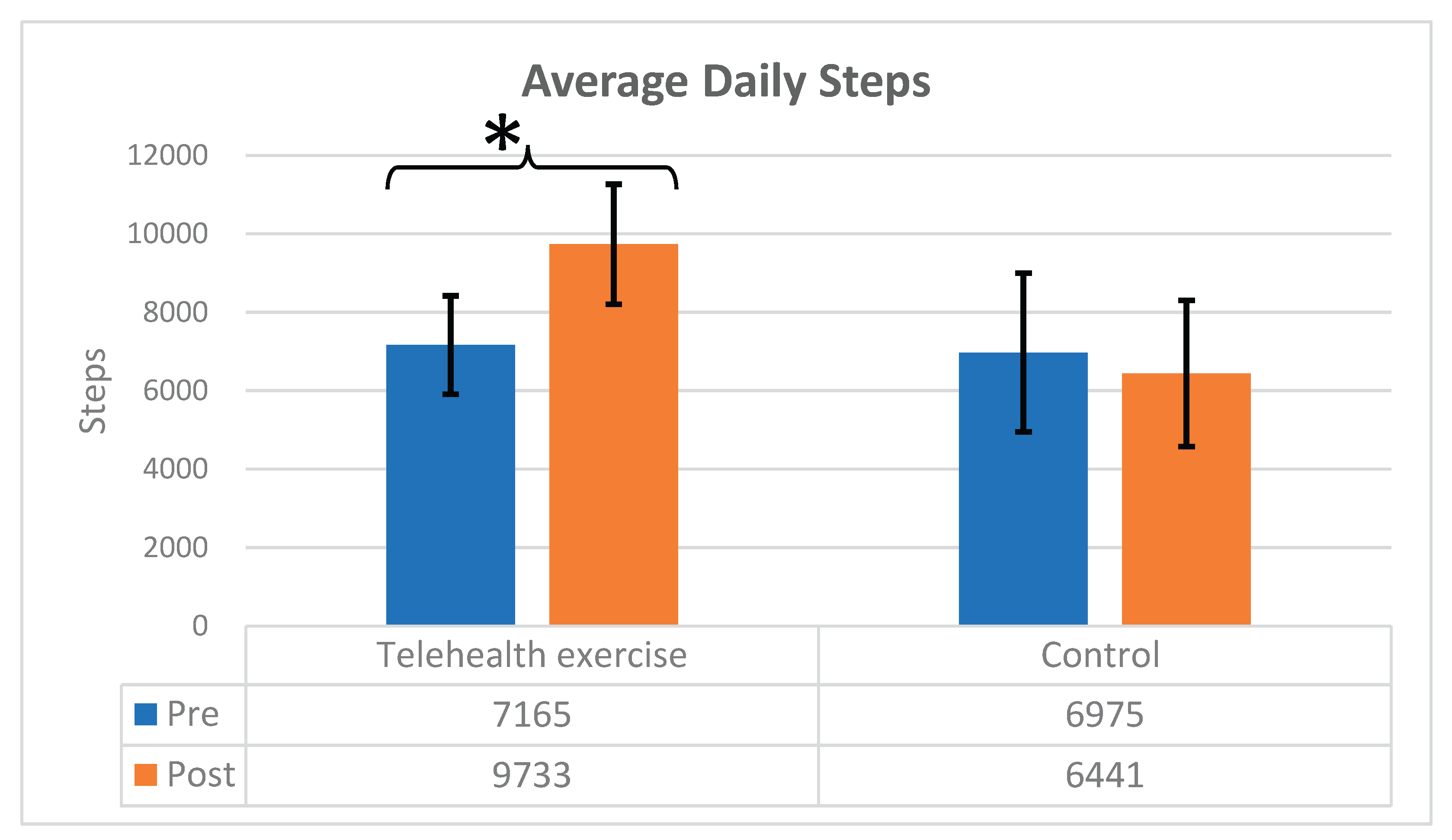
3.3. Average Daily Steps in the Telehealth Exercise and Control Groups
In the TE group, the average step count was 7,165 ± 1,255 at baseline and increased to 9,733 ± 1,531 after four weeks of training (
Figure 1). This significant increase in steps completed suggests that the participants were motivated and compliant with the exercise training. The exercise program set the target at “10,000 steps” and the average steps completed by the participants were 9733, which means that the goal was achieved by more than 50% of the participants in this group. This increase in exercise activity is the main factor contributing to the significant change in lung function parameters such as the FEV1 and FVC. Conversely, the control group exhibited an initial average of 6,975 ± 2,022, and declined to 6,442 ± 1,865. This result suggested that the control group participants were not so motivated to do the exercise stepping. The difference in the steps achieved by the two groups led to a significant between-group difference of P<0.001.
4. Discussion
Apart from manifestations such as fatigue, sleep disturbances, and cognitive impairment, young adults afflicted with COVID experience subjectively a notable decline in pulmonary function, characterized by a reduction in FVC and FEV1, alongside a compromised diffusion capacity. These alterations contribute to ineffective respiration and a diminished overall lung capacity [
16,
17]. With the COVID19 attack, the deconditioning of the diaphragm and intercostal muscles significantly impacted the efficiency of breathing which could have adverse effects on a number of different pulmonary functions [
17,
18].
The four-week telehealth exercise program produced positive outcomes in FVC and FEV1 and these are contributed by the high numbers of daily average steps performed. The exercise increased the cardiopulmonary capacity of the participants. The daily step goal enhanced exercise habits and transformed sedentary behaviors into active engagement in aerobic capacity training. These results are consistent with those reported by previous research that involved in-person physical exercise training programs. In the systematic review by Rahmati et al [
19], 10 studies reported significant improvements in FVC and FEV1 after a physical rehabilitation program in post-discharge COVID patients. The present study was able to produce significant improvement in FVC and FEV1 via a telehealth program without the direct face-to-face contact of therapists with patients, and this is providing important evidence to support the effectiveness of telehealth service model.
The rhythmic step exercises acted as a training stimulus for the diaphragm, the intercostal muscles, and accessory muscles in respiration. This can have positive effects on muscle hypertrophy and enhanced neuromuscular efficiency. The stronger the inspiration, the deeper the total volume of air that can be exhaled (FVC). The stronger the expiration, the stronger FEV1 exhaled with good expiratory muscle function [
20]. The improvement enhanced the respiratory muscles and resulted in less fatigue during aerobic exercise in training for ventilation. The stretching effect on the lung tissue and chest wall can also improve the work of breathing as the changes in FVC and FEV1 improved lung compliance.
During the stepping exercise, cardiac output and stroke volume improved. Perfusion to the pulmonary capillaries increased [
17]. The indirect effect of the change in FVC and FEV1 showed that the efficiency of the work of the lung function contributed to the matching of the ventilation and perfusion ratio in the improvement of FVC and FEV1.
The participants in the present study were mainly young healthy adults prior to suffering COVID. Hence their values in FEV1 to FVC were in the normal range, and therefore the absolute change in their values were relatively small after exercise training. If the clients had respiratory illnesses such as asthma or obstructive lung disease, their baseline FEV1 to FVC ratio would be in the clinical range and the changes would need to be a greater extent in order to restore their lung functions.
The present telehealth exercise program, with the video of rhythmic step exercises performed daily, maintained an approximate 4-5 METs cardiopulmonary exercise training [
15]. This is the appropriate exercise intensity for young adults to improve their cardiorespiratory fitness. Moderate-intensity exercises have been reported to produce cardiovascular and respiratory benefits enhancing oxygen delivery and utilization [
5]. While the present telehealth training program mainly focus on stepping exercise, eventually the participants may feel well enough to attempt other forms of exercise. This can have a long-term benefit on their fitness and well-being in general.
The telehealth exercise program demonstrated feasibility and high self-efficacy to increase their personal drive to perform the volume of physical activity. This result is consistent with other research findings supporting the benefits of adopting telehealth exercise program yield similar benefits for individuals with cancer, chronic pain syndromes and among the aging population in community settings [
9,
11,
21].
The telehealth exercise program allowed for a flexible schedule and enabled the participants to perform exercises at home daily. The positive reinforcement with the video and the soft reminder in WhatsApp conveyed the importance of the daily aerobic exercise. This reduced the common dropout in the rehabilitation process. With the use of pedometer apps, the steps can be tracked automatically. This element may have enhanced the performance of the participants and serves as a motivator to achieve the goal [
22,
23].
5. Conclusions
The telehealth exercise program has the potential to become a vital component of pulmonary rehabilitation post-COVID-19, effectively combining physical recovery with psychological support. The present study demonstrated the effectiveness of the telehealth exercise program which produced positive engagement of the participants in the training program and significant improvement in lung functions were achieved. Continued research with the use of telehealth exercise is necessary to refine program delivery and establish long-term outcomes for lung function recovery will be beneficial for the rehabilitation of patients after COVID pandemics.
Author Contributions
Conceptualization: Eyckle CH Wong, Raymond WM Lo Methodology: Eyckle CH Wong, Raymond WM Lo Software: Eyckle CH Wong, Raymond WM Lo Validation: Eyckle CH Wong, Rachel LC Kwan Formal Analysis: Eyckle CH Wong, Raymond WM Lo, Rachel LC Kwan Investigation: Eyckle CH Wong, Sara WY Lam, Natalie NM Chan, Ruby YK Ng, Suyi KC Wong Resources: Sara WY Lam, Natalie NM Chan, Ruby YK Ng, Suyi KC Wong Data Curation: Sara WY Lam, Natalie NM Chan, Ruby YK Ng, Suyi KC Wong Writing-Original Draft Preparation: Eyckle CH Wong, Raymond WM Lo, Sara WY Lam, Natalie NM Chan, Ruby YK Ng, Suyi KC Wong Writing -Review and Editing: Eyckle CH Wong, Raymond WM Lo, Rachel LC Kwan, Grace PY Szeto Visualization: Eyckle CH Wong, Raymond WM Lo, Rachel LC Kwan Supervision: Eyckle CH Wong, Raymond WM Lo, Rachel LC Kwan.
Funding
No external funding was received.
Institutional Review Board Statement
This study received ethical approval from Tung Wah College Research Ethics Committee on 8 August 2023, IRB number (MHS/PT/AY23-24/1).
Informed Consent Statement
Informed consent was obtained from all participants.
Abbreviations
The following abbreviations are used in this manuscript:
| PAR-Q |
Physical Activity Readiness Questionnaire |
| GLI |
Global Lung Function Initiative |
| ATS |
American Thoracic Society |
| ERS |
European Respiratory Society |
| FEV1/FVC |
Ratio of forced expiratory volume to forced vital capacity |
| FVC |
forced vital capacity |
| FEV1 |
forced expiratory volume in one second |
| PEFR |
peak expiratory flow rate |
| BMI |
body mass index |
| SPSS |
Statistical Package for the Social Sciences |
References
- Mogensen, I.; Ekström, S.; Hallberg, J.; Georgelis, A.; Melén, E.; Bergström, A.; Kull, I. Post COVID-19 symptoms are common, also among young adults in the general population. Sci. Rep. 2023, 13, 38315. [Google Scholar] [CrossRef]
- del Rio, C.; Collins, L.F.; Malani, P. Long-term Health Consequences of COVID-19. JAMA 2020, 324, 1723–1724. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2023, 401, e21–e33. [Google Scholar] [CrossRef]
- Salem, A.M.; Al Khathlan, N.; Alogily, M.; Alharbi, M.; Alsubaei, N.; AlOuhali, H.; AlOtaibi, A.; Al Hamam, A.; Al Ghamdi, K.; Al-Asoom, L.; Yar, T. Respiratory muscle weakness, reduced exercise capacity, and impaired lung functions in long-term post-COVID-19 patients. Electron. J. Gen. Med. 2025, 22, 16228. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Su, C.-H. Tailored Physical Activity Interventions for Long COVID: Current Approaches and Benefits—A Narrative Review. Healthcare 2024, 12, 1539. [Google Scholar] [CrossRef] [PubMed]
- Coscia, F.; Di Filippo, E.S.; Gigliotti, P.V.; Fanò-Illic, G. Effect of physical activity on long COVID fatigue: an unsolved enigma. Eur. J. Transl. Myol. 2023, 33, 11639. [Google Scholar] [CrossRef]
- Rathore, F.A.; Khalil, M.T.; Khan, O.J. Rehabilitation Perspectives in Long COVID-19. J. Pak. Med. Assoc. 2023, 73, 1553–1555. [Google Scholar] [CrossRef]
- Chiang, S.L.; Shen, C.L.; Chen, L.C.; Lo, Y.P.; Lin, C.H.; Lin, C.H. Effectiveness of a home-based telehealth exercise training program for patients with cardiometabolic multimorbidity: a randomized controlled trial. J. Cardiovasc. Nurs. 2020, 35, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.C.; Coombes, J.S.; Rodriguez, K.J.; Hickman, I.J.; Keating, S.E. Effectiveness of exercise via telehealth for chronic disease: a systematic review and meta-analysis of exercise interventions delivered via videoconferencing. Br. J. Sports Med. 2022, 56, 1042–1052. [Google Scholar] [CrossRef]
- Flynn, A.; Preston, E.; Dennis, S.; Canning, C.G.; Allen, N.E. Utilising telehealth to support exercise and physical activity in people with Parkinson disease: a program evaluation using mixed methods. BMC Health Serv. Res. 2023, 23, 224. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Development of telehealth services. Available online: https://www.legco.gov.hk/research-publications/english/essentials-2021ise14-development-of-telehealth-services.htm (accessed on 21 July 2025).
- HA Go website. Available online: https://www2.ha.org.hk/hago/en/home (accessed on 21 July 2025).
- Pauwels, R.A.; Buist, A.S.; Calverley, P.M.; Jenkins, C.R.; Hurd, S.S. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am. J. Respir. Crit. Care Med. 2001, 163, 1256–1276. [Google Scholar] [CrossRef] [PubMed]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Christopher, D.J.; Isaac, B.T.; John, F.B.; Shankar, D.; Samuel, P.; Gupta, R.; Thangakunam, B. Impact of post-COVID-19 lung damage on pulmonary function, exercise tolerance and quality of life in Indian subjects. PLOS Glob. Public Health 2024, 4, e0002884. [Google Scholar] [CrossRef]
- Crameri, G.A.G.; Bielecki, M.; Züst, R.; Buehrer, T.W.; Stanga, Z.; Deuel, J.W. Reduced maximal aerobic capacity after COVID-19 in young adult recruits, Switzerland, May 2020. Euro Surveill. 2020, 25, 2001542. [Google Scholar] [CrossRef]
- Goërtz, Y.M.; Van Herck, M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.; Houben-Wilke, S.; Burtin, C.; Posthuma, R.; Franssen, F.M.; van Loon, N.; Hajian, B.; Spies, Y.; Vijlbrief, H.; van ’t Hul, A.J.; Janssen, D.J.; Spruit, M.A. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 2020, 6, 00542–2020. [Google Scholar] [CrossRef]
- Rahmati, M.; Shamsi, M.M.; Woo, W.; Koyanagi, A.; Lee, S.W.; Yon, D.K.; Shin, J.I.; Smith, L. Effects of physical rehabilitation interventions in COVID-19 patients following discharge from hospital: A systematic review. J. Integr. Med. 2023, 21, 149–158. [Google Scholar] [CrossRef]
- Wagner, P.D. The physiological basis of pulmonary gas exchange: implications for clinical interpretation of arterial blood gases. Eur. Respir. J. 2014, 45, 227–243. [Google Scholar] [CrossRef]
- da Costa, B.O.; Andrade, L.S.; Botton, C.E.; Alberton, C.L. Effects of a telehealth stretching exercise program on pain, sleep, depression, and functionality of women with fibromyalgia during the COVID-19 pandemic: A randomized clinical trial. Sustainability 2023, 15, 1–16. [Google Scholar] [CrossRef]
- Ridgers, N.D.; McNarry, M.A.; Mackintosh, K.A. Feasibility and effectiveness of using wearable activity trackers in youth: a systematic review. JMIR Mhealth Uhealth 2016, 4, e6540. [Google Scholar] [CrossRef]
- Ingledew, D.K.; Markland, D.; Strömmer, S.T. Elucidating the roles of motives and gains in exercise participation. Sport Exerc. Perform. Psychol. 2014, 3, 116. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).