1. Introduction
Emerging evidence suggests the critical role of diet in shaping mental health outcomes, particularly anxiety and depression [
1,
2] which are increasingly prevalent among children and adolescents worldwide [
3]. Depression and anxiety arise from a combination of various complex interconnected environmental and genetic factors, and their precise aetiology remains unclear. Studying the role of modifiable risk factors such as diet is important for intervention [
2,
4].
Childhood and adolescence are pivotal periods for brain development and emotional regulation, during which nutritional intake can exert profound influences on cognitive functions, learning capacity, and emotional stability. Much of the existing literature has focused on the detrimental effects of ultra-processed foods on paediatric mental health, but little evidence is available on the impact of specific food categories on anxiety and depression [
2].
Findings from observational studies and meta-analyses suggest that healthy dietary patterns, characterized by high consumption of fruit, vegetables, whole grains and fibre and low intake of saturated fats, during the prenatal, childhood, and adolescent stages, are associated with reduced risk of internalizing (e.g., anxiety, depression) and externalizing (e.g., attention-deficit/hyperactivity disorder, conduct disorder) disorders [
4]. In contrast, diets rich in sugars, saturated animal fats and ultra-processed foods, combined with low intakes of nutrient-dense foods, are linked to increased risk of anxiety and depressive symptoms [
4].
Moreover, quantitative dietary indices, such as the Mediterranean Diet Score, have revealed significant associations between low adherence to Mediterranean diet and both clinical diagnoses and symptom severity of depression and anxiety. Specifically, analyses focusing on individual food groups indicate that higher intake of vegetables is inversely correlated with symptom severity for depression, anxiety, and fear [
5]. Similarly, increased consumption of non-refined grains is associated with reduced severity of depression and anxiety symptoms and lower odds of clinical diagnosis, even after controlling for other dietary factors [
5].
The association between diet and depressive symptoms in early childhood has not yet been adequately addressed in the literature. This relationship is complex and influenced by multiple behavioural, psychosocial, and socioeconomic factors that include maternal diet and parental mental health, child physical activity levels, screen time, and broader social determinants. The quality of maternal diet during pregnancy has been associated with a range of developmental outcomes across cognitive, behavioural and emotional domains in the offspring [
6,
7,
8]. Maternal depressive symptoms have been associated with less healthy parenting behaviours, which can negatively impact children’s dietary habits and mental health outcomes [
9,
10]. Parental anxiety and depression have been linked to increased food fussiness in children, which may act as an intermediary risk factor for internalizing disorders [
11]. Regarding physical activity and depressive symptoms in children, there is evidence that children with internalizing disorders tend to engage in significantly lower levels of physical activity [
12]. Moreover, excessive screen time has been linked to higher risks of anxiety and depression in children, particularly during periods of restricted movement, such as during the COVID-19 pandemic [
13,
14]. Socioeconomic status remains a significant determinant of both diet quality and mental health. Lower socioeconomic status is frequently associated with suboptimal dietary patterns and higher prevalence of depressive symptoms among children and adolescents [
15].
This study aims to investigate whether the dietary habits of children in the Italian Piccolipiù birth cohort at four years of age are associated with early emotional outcomes, specifically focusing on symptoms of anxiety and depression. This analysis was conducted within the framework of the Global Burden of Disease Lifestyle and Mental Disorders (GLAD) Project, whose objective is to gather evidence on the association between lifestyles and Common Mental Disorders (CMDs) to support the informed inclusion of risk factors attributable to CMDs in the Global Burden of Disease (GBD) Study framework [
16].
2. Materials and Methods
This study utilizes data from the Italian multicentre Piccolipiù birth cohort, designed to evaluate the effects of prenatal and early postnatal environmental, parental, and social exposures on child health and development. Piccolipiù recruited 3358 mother-child pairs from six maternity units across five Italian cities (i.e., Florence, Rome, Trieste, Turin, and Viareggio) between October 2011 and March 2015. All singleton pregnant women giving birth in one of the selected maternity units were considered eligible for recruitment if they met the following criteria: they were at least 18 years old; resided within the catchment area of the participating maternity centres; had sufficient knowledge of the Italian language to understand the informed consent process and complete the study questionnaires; and could be contacted via at least one telephone number. Follow-up assessments were conducted at 6, 12, 24, 48, and 84 months postpartum. Further details on the Piccolipiù study protocol are available elsewhere [
17].
The 4-year follow-up assessment was carried out in the framework of the Piccolipiù in Forma project, and had a special focus on obesity, nutrition, and physical activity [
https://piccolipiuinforma.it/]. During this follow-up visit, children were also assessed for their psychomotor and cognitive development, and for emotional and behavioural problems appraised using a validated caregiver-report, the Child Behavior Checklist (CBCL) 1.5-5 years [
18]. Overall, the response rate was 64.9% for the dietary questionnaire and 61.4% for the CBCL.
Specifically, the CBCL provides total scores and standardized scores (i.e., T-scores, with mean = 50 and standard deviation = 10) for a wide range of behavioural and emotional problems in children. Total scores are calculated as the sum of item scores for each sub-scale. Each item is rated by a parent or caregiver as follows: 0=not true; 1=somewhat or sometimes true; 2=very true or often true. T-scores are obtained by converting raw scores using normative tables based on large-scale population samples of children matched by age and sex.
The present study was specifically focused on anxiety and depression, based on: i) clinical classification, where children were classified as having clinically significant anxiety or depression if their standardized T-scores exceeded 70, following established CBCL guidelines; ii) raw total scores, expressed as continue measures, to capture the full spectrum of symptom severity, including subclinical levels. As the anxiety and depression subscales include ten items each, total scores can range from 0 to 20.
Dietary intake evaluated at the 4-year follow-up used a food frequency questionnaire (FFQ), compiled by the parents based on the child’s habitual diet during the previous two months. The FFQ collected information on frequency of consumption and portion size of 46 different food items using the Scotti-Bassani pediatric food portions atlas [
19]. For each child, the frequency of consumption in grams/day of each item was calculated, combining food portions and frequencies as follows: Portion in g/day = Portion size(g)*times per month/30⋅4 OR portion size(g)*times per week/7 OR daily size(g)*times/day. The average daily intake expressed in grams per day was calculated, for the purpose of this study, for each of the following food groups: vegetables, fruit, legumes, grains, milk, red meat, processed meat, fish, and sugar-sweetened beverages.
Moreover, sociodemographic data were collected, and family income was used as a proxy for socioeconomic status. Monthly family income was originally recorded using predefined categories: less than €1000; €1000–1499; €1500–1999; €2000–2499; €2500–2999; €3000–3999; €4000–4999; €5000–5999; and €6000 or more. An additional category indicated inability to quantify the income was also included. Following the GLAD protocol, the categorical income variable was transformed into a continuous one by assigning the median value of each bracket [
16]. For the open-ended lowest and highest categories, the respective threshold value was assigned. Cases with unquantifiable income were excluded from analyses. To obtain a more individualized measure of economic capacity and allow fairer comparisons across households of different sizes, monthly family income was divided by the number of household components to compute per capita income, expressed in euros.
Therefore, the present analysis included all children with available data for the FFQ, the CBCL, and family income at the 4-year follow-up.
2.1. Statistical Analyses
Categorical variables were summarized as absolute frequencies and percentages, while continuous variables were presented as median and interquartile range (IQR), given the non-normal distribution confirmed by the previously performed Shapiro-Wilk normality test.
Food group consumption was compared between children with and without clinical anxiety, and between those with and without clinical depression, using the Wilcoxon-Mann-Whitney test.
Univariate logistic analyses were conducted to identify potential dietary risk factors for both clinical anxiety and clinical depression, with odds ratios (ORs) reported alongside 95% confidence intervals (CIs).
Furthermore, multivariable analyses were carried out to explore the associations between food group consumption and mental health outcomes, adjusting for potential confounders (i.e., sex and per capita income). Specifically, logistic regression models were applied to binary clinical outcomes, while robust linear regression models based on MM-estimators were used for raw scores. This approach was adopted to address the skewness of the dependent variables, which can result in non-normal residuals and violate key assumptions of ordinary least squares regression. By relaxing the requirement for normally distributed residuals and reducing sensitivity to outliers and heteroscedasticity, robust regression offers more stable and reliable estimates under these conditions. All estimates (i.e., OR and regression coefficients) were reported with 95% CI. ORs and regression coefficients were presented per gram-per-day increase in the consumption of each food group. All statistical analyses were performed using R, with statistical significance set at p < 0.05 [R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL
https://www.R-project.org/].
3. Results
A total of 2166 dietary questionnaires and 2062 CBCL questionnaires were completed, with 2004 children providing data for both. Of these, 1886 were retained for analysis as they were 4 years old at the time of assessment, while children who completed the follow-up at age 5 were excluded. Among the 1886 participants, 1855 had available data on family income, although only 1726 provided quantifiable information (excluding those who reported being unable to estimate their income). Therefore, the final sample included 1726 children (median age: 4.4 years, IQR: 4.2–4.5), 50% of whom were female. The median per capita monthly income was € 687.4 (IQR: € 562.4–916.5) (
Table 1).
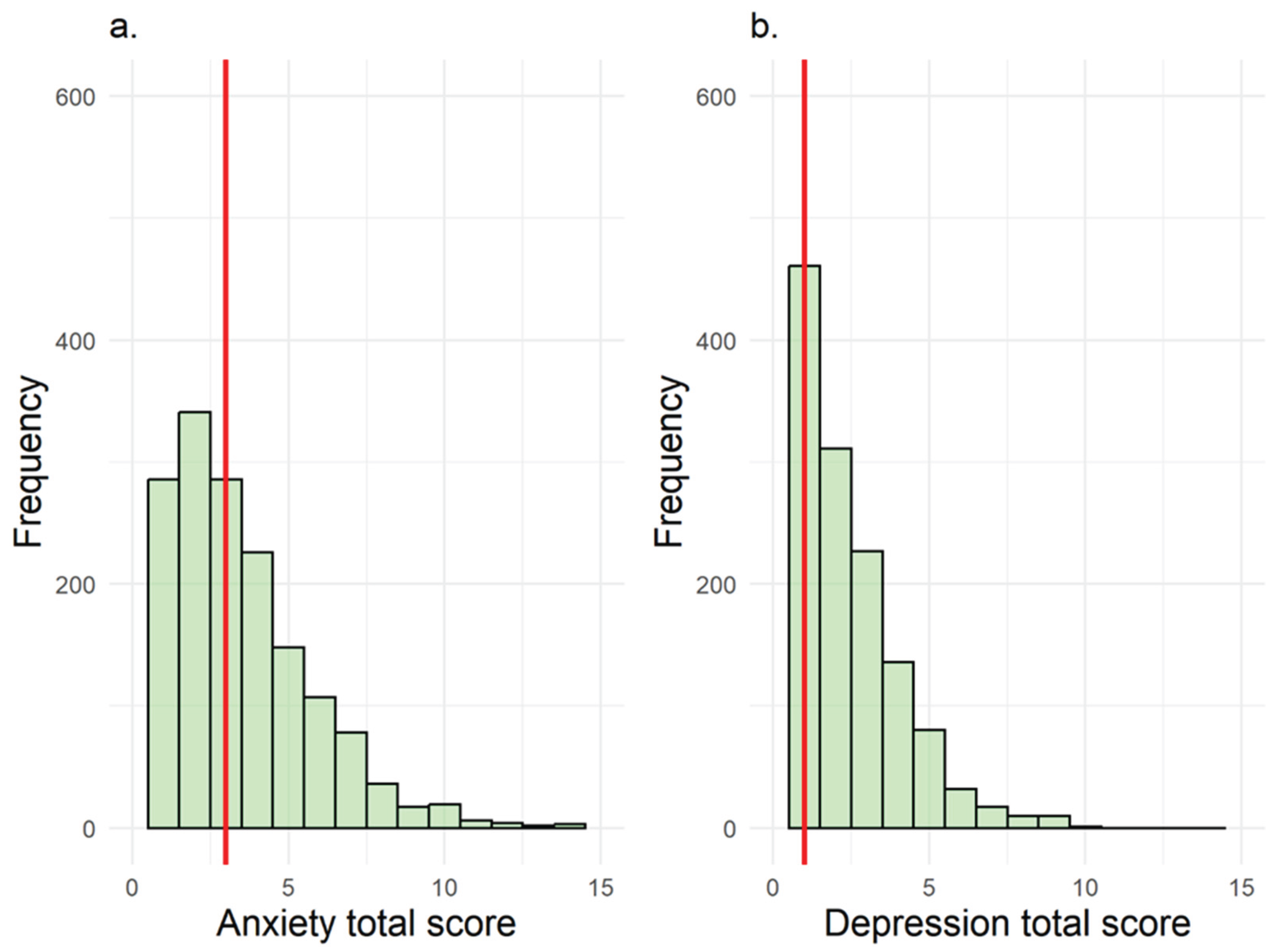
Overall, 3% of children exhibited clinically significant anxiety symptoms, and 2% showed clinically significant depressive symptoms. Median CBCL raw scores were 3 (IQR: 1–4) for anxiety and 1 (IQR: 0–3) for depression (
Figure 1).
Daily intake of each food group, stratified by clinical anxiety and depression status, is reported in
Table S1. At univariable analysis, grain intake was associated with an increased odds of clinical anxiety (OR=1.004; 95% CI: 1.001-1.007), while for clinical depression, however, higher fish consumption was associated with reduced odds of symptoms (OR = 0.946; 95% CI: 0.903–0.992), while no associations were observed for other food groups.
When analysing total scores, only vegetable intake was associated with lower anxiety (β = –0.004; 95% CI: –0.007 to –0.001) and depression scores (β = –0.003; 95% CI: –0.006 to –0.001) (
Table S2). No other food groups were associated with anxiety or depression total scores.
Multivariable analyses for anxiety, adjusted for sex and per capita income, are presented in Tables 2a and 2b. Greater grain consumption was associated with anxiety, with more evident association when considered as clinical anxiety (OR = 1.004; 95% CI: 1.001–1.007).
Table 2.
Robust linear regression coefficients with 95% CI for anxiety raw scores (a) and Odds Ratios (OR) with 95% Confidence Intervals (CI) for anxiety (b)a.
Table 2.
Robust linear regression coefficients with 95% CI for anxiety raw scores (a) and Odds Ratios (OR) with 95% Confidence Intervals (CI) for anxiety (b)a.
| |
Raw total scores for anxiety (a) |
Clinical anxiety (b) |
| Variables (g/day) |
Coeff. |
95% CI |
p-value |
OR |
95% CI |
p-value |
| Fruit |
-0.001 |
-0.003; 0.001 |
0.340 |
0.997 |
[0.991-1.003] |
0.326 |
| Vegetables |
-0.003 |
-0.001; 0.0001 |
0.073 |
1.003 |
[0.996-1.010] |
0.310 |
| Legumes |
0.008 |
-0.007; 0.022 |
0.489 |
1.016 |
[0.984-1.047] |
0.296 |
| Grains |
0.002 |
-0.0001; 0.003 |
0.063 |
1.004 |
[1.001 -1.007] |
0.039 |
| Milk |
-0.0003 |
-0.001; 0.0003 |
0.424 |
1.000 |
[0.998-1.001] |
0.957 |
| Red meat |
0.007 |
-0.002; 0.016 |
0.127 |
1.003 |
[0.981-1.025] |
0.810 |
| Cured meat |
0.010 |
-0.011; 0.030 |
0.351 |
1.015 |
[0.965-1.069] |
0.561 |
| Fish |
0.010 |
-0.0001; 0.020 |
0.052 |
1.008 |
[0.984-1.034] |
0.507 |
| Sweetened drinks |
0.000 |
-0.0003; 0.001 |
0.492 |
1.000 |
[0.998-1.001] |
0.839 |
Regarding depression total scores, higher intake of both fruit and vegetables corresponded to lower depressive symptomatology (β = –0.002; 95% CI: –0.003 to –0.0001; and β = –0.003; 95% CI: –0.005 to –0.001, respectively) (
Table 3a). No other food groups showed associations with depression total scores. For clinical depression, fish consumption was associated with reduced odds of symptoms (OR = 0.951; 95% CI: 0.907–0.997). No other dietary factors were associated with clinical depression (
Table 3b).
4. Discussion
This study examined the associations between food groups and internalizing mental health outcomes in a large multicenter cohort of Italian preschool-aged children, using both clinical cutoffs and continuous measures from the CBCL. Overall, a nuanced association was found between certain dietary intakes and symptoms of anxiety and depression. As expected, the prevalence of clinically meaningful symptoms was relatively low, with 3% of children meeting criteria for anxiety and 2% for depression. These rates are consistent with international epidemiological data that suggest that clinical manifestations of internalizing disorders are less common in early childhood compared to later developmental stages [
2].
The multivariable analyses, adjusted for sex and per capita income, revealed several noteworthy findings.
Grain consumption was consistently and positively associated with clinical anxiety, but no association was found with raw anxiety scores. This pattern may suggest a non-linear relationship or a threshold effect, whereby higher levels of grain intake are associated with clinically significant symptoms but not with subclinical variations. The consumption of refined grains, which are often characterized by high glycemic load and limited nutritional value compared with the whole grains, has been linked to systemic inflammation, oxidative stress, and increased risk of depression and anxiety in the adult population [
5,20]. In the current study we only had data on total grain consumption. It would have been interesting to have data distinguishing between whole and refined grain intake to clarify their respective impacts on child mental health.
Regarding depression, the multivariable analyses revealed that fruit and vegetable consumption was associated only with depressive symptoms as reflected by total scores, suggesting that regular intake of these foods may offer subtle but consistent emotional benefits. Since fruits and vegetables are rich in fibers, vitamins (e.g., folate, vitamin C), antioxidants, and anti-inflammatory compounds, they can reduce oxidative stress factors, which are increasingly recognized in the pathophysiology of depression, and may contribute to improved mood regulation, as observed in the adult population. Importantly, the association we observed concerned only subclinical depressive symptoms, and not clinical depression, possibly indicating a preventive or buffering effect of fruit and vegetable intake during early emotional development [21,22]. However, the lack of association with clinically significant depression could also reflect the low prevalence of this outcome in our sample, which may have limited the statistical power to detect associations of moderate magnitude.
Although no clear association was observed between fish consumption and total depression scores, higher daily intake of fish was linked to lower odds of clinical depression. This finding may reflect the well-established neurobiological effects of long-chain omega-3 fatty acids found in fish, such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which are known to influence brain structure, neurotransmitter activity, synaptic plasticity, and inflammatory processes. [23,24]. This could be explained by the fact that the relationship between fish consumption and total depression scores is not linear, and therefore the effect of fish consumption becomes significant only when the data are dichotomized based on the clinical threshold.
While evidence on children has only recently started to emerge, general population studies suggest that diets rich in anti-inflammatory and neuroprotective nutrients, found in fish, fruit, vegetables, and nuts, are associated with lower depression risk [25]. A systematic review also found that increased fruit and vegetable consumption is linked to reduced risk of depression among youth and young adults aged 15–45 years [26], supporting the potential value of early-life interventions.
Overall, the lack of associations between most other food groups and emotional outcomes suggests that, during early childhood, the relationship between diet and internalizing mental health outcomes may be more nuanced, potentially moderated by other behavioural and environmental factors.
4.1. Strenghts and Limitations
The main strengths of the present study are the use of a large birth cohort, the standardized assessments of emotional outcomes using the CBCL, and detailed dietary data derived from FFQ. The dual analysis of clinical classifications and continuous symptom scores allowed us to capture both overt and subthreshold manifestations of emotional distress, which is particularly relevant for identifying early risk factors and intervention targets.
However, several limitations warrant consideration. First and foremost, the cross-sectional design of the dietary and mental health assessments prevents any conclusions about the directionality or causality of the observed associations. Specifically, it is not possible to determine whether dietary patterns contributed to the emergence of emotional symptoms, or whether pre-existing emotional states influenced dietary behaviors (e.g., emotional eating, appetite changes). Moreover, unmeasured confounding and bidirectional effects are likely in the context of complex behavioral and psychosocial processes, further limiting causal inference. Secondly, the food frequency questionnaire relied on parental recall and did not capture dietary diversity or food processing level (e.g., ultra-processed foods), which are important dimensions of diet quality. Thirdly, the study did not include biomarkers of nutrient status or inflammation, which could have strengthened biological plausibility. Fourthly, although our data was adjusted for sex and per capita income, several other factors such as parental mental health, screen time, and broader socioeconomic conditions can significantly influence both diet quality and psychological development [
9,
13,
15]; the complexity of these interrelated influences may have reduced our ability to detect diet-specific effects, especially in a relatively healthy population with a narrow range of dietary habits. Finally, the sample’s generally low symptom burden may have limited our ability to detect associations of smaller magnitude.
5. Conclusions
Our findings support the hypothesis that higher intake of specific food groups, particularly vegetables, fruits and fish, is associated with better emotional health in preschool-aged children. While modest in effect size, these findings underscore the importance of promoting healthy dietary patterns from early childhood as part of a broader strategy for mental health prevention.
Further longitudinal research is needed to confirm these associations over time and to explore the underlying biological mechanisms. Interventions targeting early dietary habits may represent a feasible and modifiable pathway to improve long-term mental health outcomes in children.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table S1: Food group consumption (g/day) by clinical anxiety and clinical depression; Table S2: Univariate robust linear regression coefficients with 95% CI for anxiety and depression raw scores.
Author Contributions
Conceptualization, G.Z., F.C., P.P. and L.M.; methodology, G.Z., F.C., P.P., C.C., E.M., A.K., L.M. software, G.Z..; validation, G.Z. and L.M.; formal analysis, G.Z.; investigation, G.Z., F.C., P.P., C.C., E.M., A.K., L.M.; writing—original draft preparation, G.Z., F.C., P.P.; writing—review and editing, G.Z., F.C., P.P., C.C., E.M., A.K., L.M., L.R., M.C., F.R., M.P.; supervision, P.P., L.R and L.M.. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Italian Ministry of Health, through the contribution given to the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste—Italy.
Institutional Review Board Statement
The Piccolipiù study was approved by the Ethics Committee of the Local Health Unit Roma E, the national coordinator of the project (Prot. CE/82 09/06/2011), and of each local center.
Informed Consent Statement
Informed consent was obtained from parents involved in the study
Data Availability Statement
Due to the sensitive nature of the questions asked in this study, Piccolipiù survey respondents were assured raw data would remain confidential and would not be shared. For this reason, the authors do not have permission to share data.
Acknowledgments
The authors thank all the families who took part in the study, and the Piccolipiù research group.
Conflicts of Interest
The authors declare no conflicts of interest
Abbreviations
The following abbreviations are used in this manuscript:
| GLAD |
Global Burden of Disease Lifestyle and Mental Disorders |
| CMD |
Common Mental Disorders |
| GBD |
Global Burden of Disease |
| CBCL |
Child Behavior Checklist |
| FFQ |
Food Frequency Questionnaire |
| IQR |
InterQuartile Range |
| OR |
Odds Ratio |
| CI |
Confidence Interval |
| EPA |
EicosaPentaenoic Acid |
| DHA |
DocosaHexaenoic Acid |
References
- Zhang, Q.; Li, Y.; Zhang, J.; Wu, D.; Chen, Z.; Feng, X.; Liu, Q. Association between Long-Term Consumption Trajectories of Various Foods and the Risk of Anxiety and Depression in Chinese Children. Crit Public Health 2025, 35. [Google Scholar] [CrossRef]
- Malmir, H.; Mahdavi, F.S.; Ejtahed, H.S.; Kazemian, E.; Chaharrahi, A.; Mohammadian Khonsari, N.; Mahdavi-Gorabi, A.; Qorbani, M. Junk Food Consumption and Psychological Distress in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutr Neurosci 2023, 26, 807–827. [Google Scholar] [CrossRef] [PubMed]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents during COVID-19: A Meta-Analysis. JAMA Pediatr 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Talib, M.; Rachdi, M.; Papazova, A.; Nicolis, H. The Role of Dietary Patterns and Nutritional Supplements in the Management of Mental Disorders in Children and Adolescents: An Umbrella Review of Meta-Analyses: Le Rôle Des Habitudes Alimentaires et Des Suppléments Nutritionnels Dans La Prise En Charge Des Troubles Mentaux Chez Les Enfants et Les Adolescents : Une Méta-Revue de Méta-Analyses. Canadian Journal of Psychiatry 2024, 69, 567–589. [Google Scholar] [PubMed]
- Gibson-Smith, D.; Bot, M.; Brouwer, I.A.; Visser, M.; Giltay, E.J.; Penninx, B.W.J.H. Association of Food Groups with Depression and Anxiety Disorders. Eur J Nutr 2020, 59, 767–778. [Google Scholar] [CrossRef] [PubMed]
- Steenweg-de Graaff, J.; Tiemeier, H.; Steegers-Theunissen, R.P.M.; Hofman, A.; Jaddoe, V.W.V.; Verhulst, F.C.; Roza, S.J. Maternal Dietary Patterns during Pregnancy and Child Internalising and Externalising Problems. The Generation R Study. Clinical Nutrition 2014, 33, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Cendra-Duarte, E.; Canals, J.; Becerra-Tomás, N.; Jardí, C.; Martín-Luján, F.; Arija, V. Maternal Dietary Patterns and Offspring Behavioral Problems. Pediatr Res 2024. [CrossRef] [PubMed]
- Collet, O.A.; Heude, B.; Forhan, A.; Delcourt, C.; Orri, M.; Van Der Waerden, J.; Melchior, M.; Côté, S.; Lioret, S.; De Lauzon-Guillain, B.; et al. Prenatal Diet and Children’s Trajectories of Anxiety and Depression Symptoms from 3 to 8 Years: The EDEN Mother-Child Cohort. Journal of Nutrition 2021, 151, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, T.W. Maternal Depressive Symptoms and Weight-Related Parenting Behaviors. Matern Child Health J 2014, 18, 1328–1335. [Google Scholar] [CrossRef] [PubMed]
- Bechtiger, L.; Steinhoff, A.; Dollar, J.M.; Calkins, S.D.; Keane, S.P.; Shriver, L.; Wideman, L.; Shanahan, L. Maternal Depressive Symptoms and Adolescents’ Unhealthy Behavior: A 15-Year Longitudinal Study. Pediatrics 2022, 150. [Google Scholar] [CrossRef] [PubMed]
- De Barse, L.M.; Cano, S.C.; Jansen, P.W.; Jaddoe, V.V.W.; Verhulst, F.C.; Franco, O.H.; Tiemeier, H.; Tharner, A. Are Parents’ Anxiety and Depression Related to Child Fussy Eating? Arch Dis Child 2016, 101, 533–538. [Google Scholar] [CrossRef] [PubMed]
- Bedard, C.; Timmons, B.W.; Ferro, M.A. Exploratory Examination of the Association between Physical-Mental Multimorbidity and Physical Activity in Children. Front Pediatr 2023, 11. [Google Scholar] [CrossRef] [PubMed]
- Lissak, G. Adverse Physiological and Psychological Effects of Screen Time on Children and Adolescents: Literature Review and Case Study. Environ Res 2018, 164, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Xiang, M.; Liu, Y.; Yamamoto, S.; Mizoue, T.; Kuwahara, K. Association of Changes of Lifestyle Behaviors before and during the COVID-19 Pandemic with Mental Health: A Longitudinal Study in Children and Adolescents. International Journal of Behavioral Nutrition and Physical Activity 2022, 19. [Google Scholar] [CrossRef] [PubMed]
- Nowicki, G.J.; Polak, M.; Ślusarska, B.; Czernecki, K. The Relationship between Diet and the Occurrence of Depressive Symptoms in a Community Example with High Rates of Social Deprivation: A Cross-Sectional Study. Nutrients 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Ashtree, D.N.; Orr, R.; Lane, M.M.; Akbaraly, T.N.; Bonaccio, M.; Costanzo, S.; Gialluisi, A.; Grosso, G.; Lassale, C.; Martini, D.; et al. Estimating the Burden of Common Mental Disorders Attributable to Lifestyle Factors: Protocol for the Global Burden of Disease Lifestyle and Mental Disorder (GLAD) Project. JMIR Res Protoc 2025, 14. [Google Scholar] [CrossRef] [PubMed]
- Farchi, S.; Forastiere, F.; Vecchi Brumatti, L.; Alviti, S.; Arnofi, A.; Bernardini, T.; Bin, M.; Brescianini, S.; Colelli, V.; Cotichini, R.; et al. Piccolipiù, a Multicenter Birth Cohort in Italy: Protocol of the Study. BMC Pediatr 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Ruffle, T.M. The Child Behavior Checklist and Related Forms for Assessing Behavioral/Emotional Problems and Competencies. Pediatr Rev 2000, 21, 265–271. [Google Scholar] [CrossRef] [PubMed]
-
Atlante Pediatrico Delle Porzioni Degli Alimenti.; Istituto Scotti Bassani, Ed.; https://www.scottibassani.it/atlante-pediatrico/. First edition 1984 last edition 2021, 2021;
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).