Submitted:
12 August 2025
Posted:
14 August 2025
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Global Trends in Age and Gender Disparities
National Trends in Age and Gender Disparities
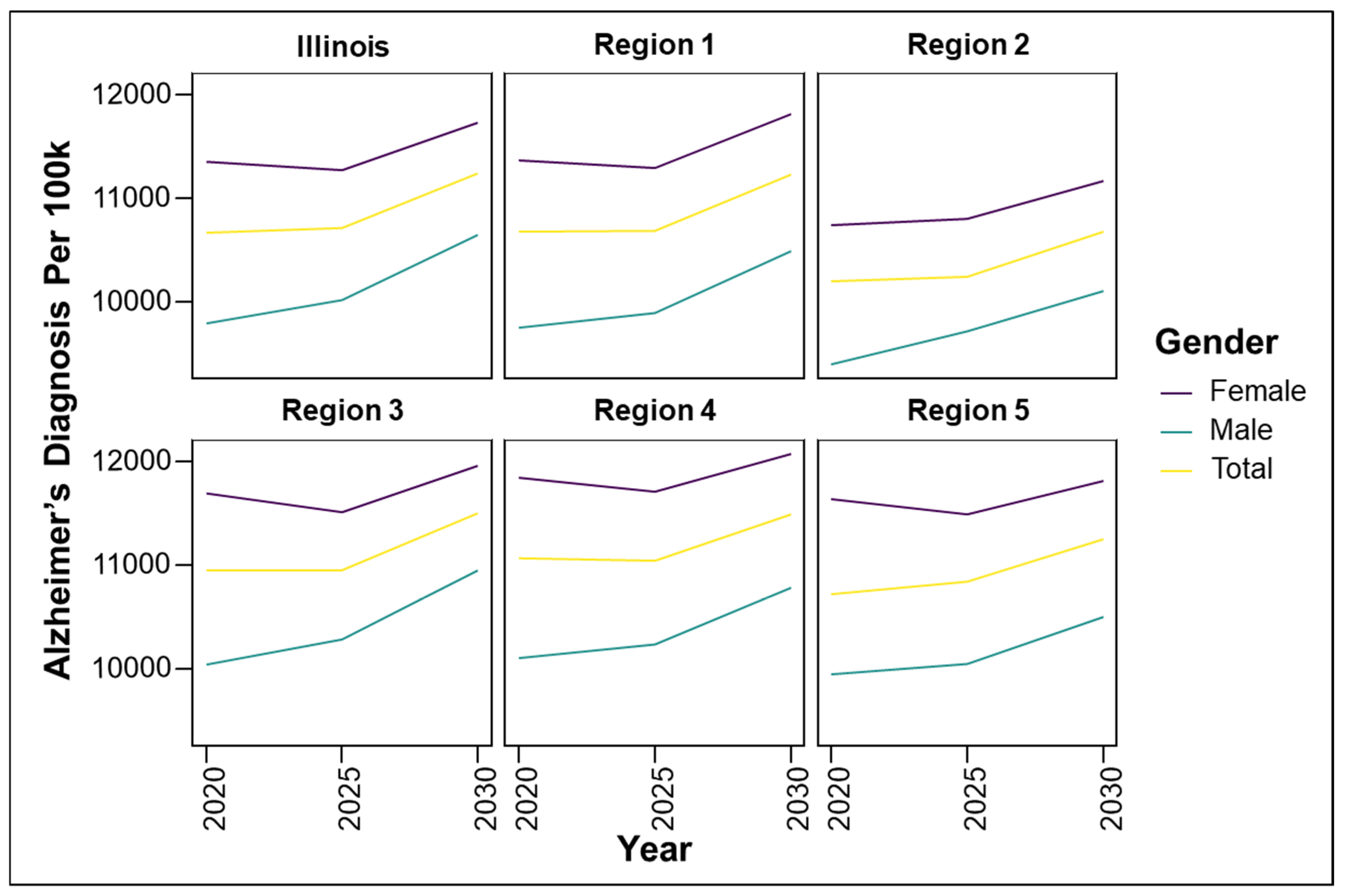
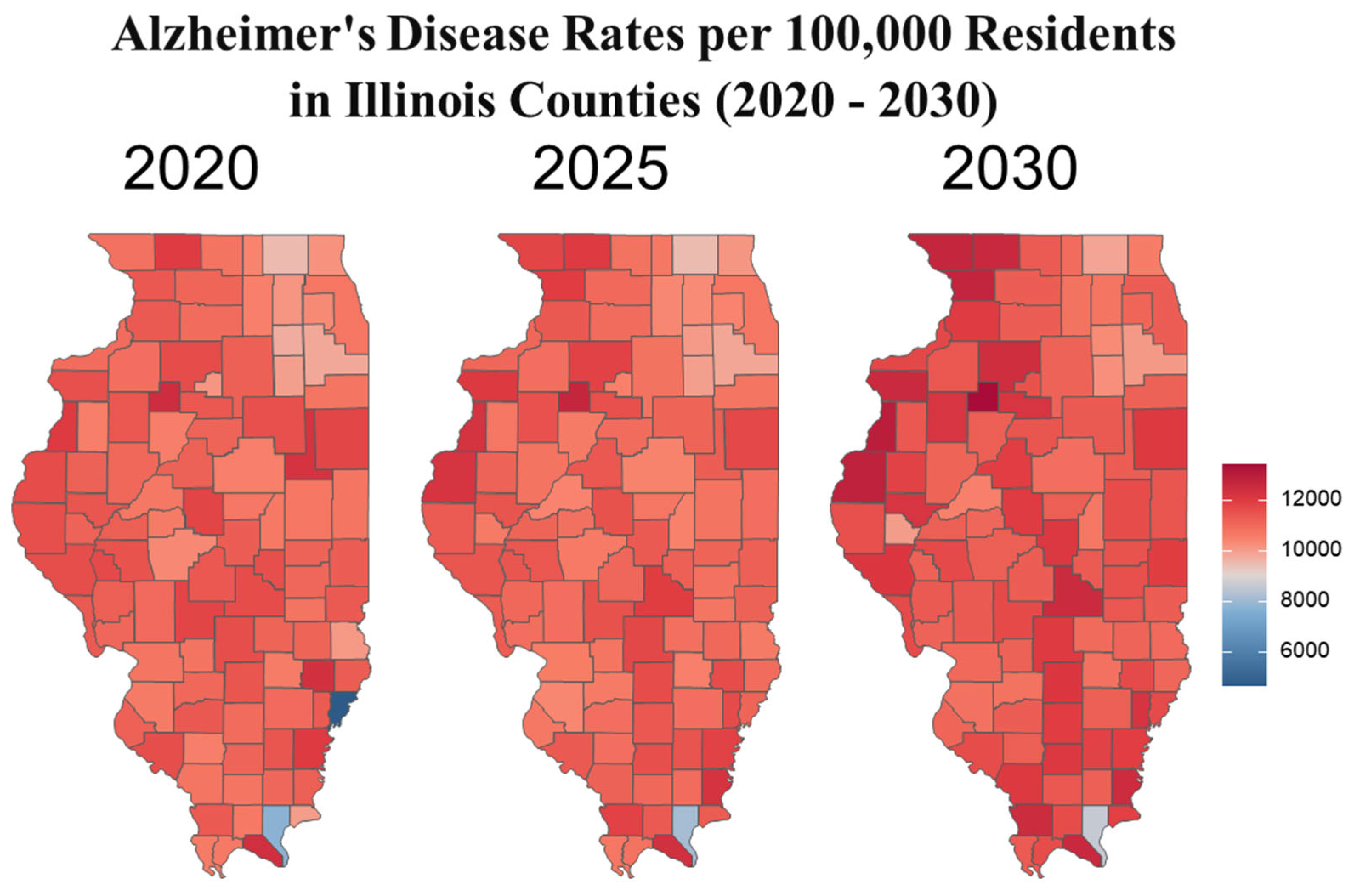
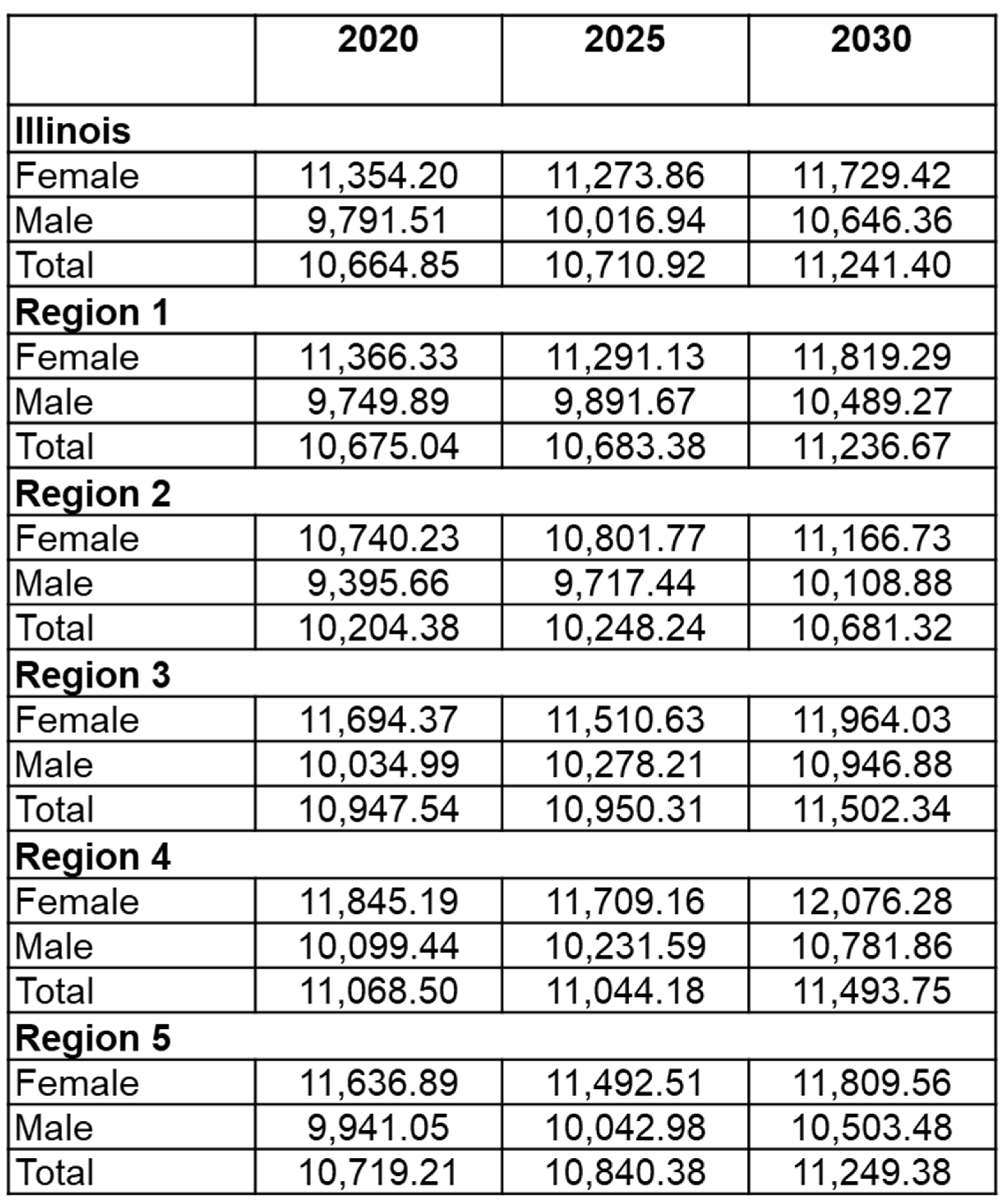
Illinois-Specific Trends in Age and Gender Disparities
Risk Factors
Non-Modifiable Risk Factors Contributing to Disparities
Age
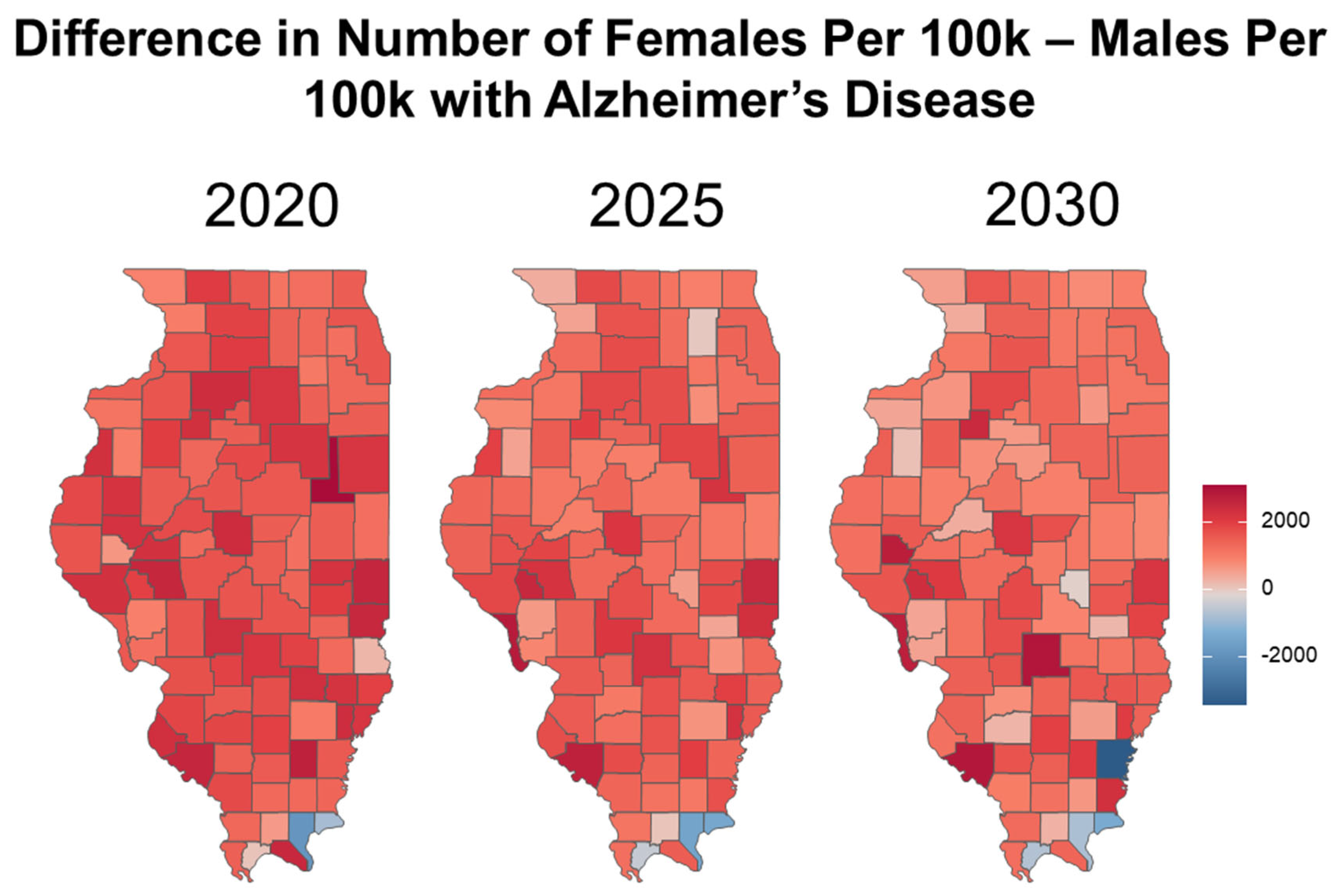
Gender
Race and Ethnicity
Modifiable Risk Factors Contributing to Disparities
Diabetes
Access to healthcare
Education
Lifestyle factors
Marital status
Economic and Caregiver Burden
Interventions and Recommendations
Conclusions
Acknowledgments
References
- Fitzpatrick AL, Kuller LH, Lopez OL, Kawas CH, Jagust W. Survival following dementia onset: Alzheimer’s disease and vascular dementia. Journal of the Neurological Sciences. 2005;229-230:43-9.
- Barclay LL, Zemcov A, Blass JP, Sansone J. Survival in Alzheimer’s disease and vascular dementias. Neurology. 1985;35(6):834-40.
- 2024 Alzheimer’s disease facts and figures. Alzheimers Dement. 2024;20(5):3708-821.
- 2023 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2023;19(4):1598-695.
- Dhana K, Beck T, Desai P, Wilson RS, Evans DA, Rajan KB. Prevalence of Alzheimer’s disease dementia in the 50 US states and 3142 counties: A population estimate using the 2020 bridged-race postcensal from the National Center for Health Statistics. Alzheimer’s & Dementia. 2023;19(10):4388-95.
- Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. The Lancet Neurology. 2011;10(9):819-28.
- Yiannopoulou KG, Papageorgiou SG. Current and Future Treatments in Alzheimer Disease: An Update. Journal of Central Nervous System Disease. 2020;12:1179573520907397.
- Adlimoghaddam A, Roy B, Albensi BC. Future Trends and the Economic Burden of Dementia in Manitoba: Comparison with the Rest of Canada and the World. Neuroepidemiology. 2018;51(1-2):71-81.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112-7.
- Matthews KA, Xu W, Gaglioti AH, Holt JB, Croft JB, Mack D, McGuire LC. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015-2060) in adults aged >/=65 years. Alzheimers Dement. 2019;15(1):17-24.
- Brookmeyer R, Evans DA, Hebert L, Langa KM, Heeringa SG, Plassman BL, Kukull WA. National estimates of the prevalence of Alzheimer’s disease in the United States. Alzheimers Dement. 2011;7(1):61-73.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. The Lancet. 2005;366(9503):2112-7.
- Bernstein Sideman A, Al-Rousan T, Tsoy E, Piña Escudero SD, Pintado-Caipa M, Kanjanapong S, et al. Facilitators and Barriers to Dementia Assessment and Diagnosis: Perspectives From Dementia Experts Within a Global Health Context. Front Neurol. 2022;13:769360.
- Gatz M, Mack WJ, Chui HC, Law EM, Barisano G, Sutherland ML, et al. Prevalence of dementia and mild cognitive impairment in indigenous Bolivian forager-horticulturalists. Alzheimer’s & Dementia. 2023;19(1):44-55.
- Canada S. Canada’s population clock (real-time model). 2024.
- The Many Faces of Dementia in Canada [Internet]. Available from: https://alzheimer.ca/en/the-many-faces-of-dementia-in-canada-landmark-study-volume-2.
- Nichols E, Szoeke CEI, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Neurology. 2019;18(1):88-106.
- Ribeiro F, Teixeira-Santos AC, Caramelli P, Leist AK. Prevalence of dementia in Latin America and Caribbean countries: Systematic review and meta-analyses exploring age, sex, rurality, and education as possible determinants. Ageing Research Reviews. 2022;81:101703.
- Llibre-Guerra JJ, Li Y, Allegri RF, Mendez PC, Surace EI, Llibre-Rodriguez JJ, et al. Dominantly inherited Alzheimer’s disease in Latin America: Genetic heterogeneity and clinical phenotypes. Alzheimer’s & Dementia. 2021;17(4):653-64.
- Shin J-H. Dementia Epidemiology Fact Sheet 2022. Ann Rehabil Med. 2022;46(2):53-9.
- Ravindranath V, Sundarakumar JS. Changing demography and the challenge of dementia in India. Nat Rev Neurol. 2021;17(12):747-58.
- Lee J, Meijer E, Langa KM, Ganguli M, Varghese M, Banerjee J, et al. Prevalence of dementia in India: National and state estimates from a nationwide study. Alzheimers Dement. 2023;19(7):2898-912.
- Kilian J, Kitazawa M. The emerging risk of exposure to air pollution on cognitive decline and Alzheimer’s disease – Evidence from epidemiological and animal studies. Biomedical Journal. 2018;41(3):141-62.
- Santos NVd, Yariwake VY, Marques KdV, Veras MM, Fajersztajn L. Air Pollution: A Neglected Risk Factor for Dementia in Latin America and the Caribbean. Frontiers in Neurology. 2021;Volume 12 - 2021.
- Ailshire JA, Walsemann KM, Fisk CE. Regional variation in U.S dementia trends from 2000-2012. SSM - Population Health. 2022;19:101164.
- Health IDoP. State of Illinois Alzheimer’s Disease Plan: 2023 –2026 Report and Recommendations. 2023.
- Air Quality Life Index [Internet]. 2023. Available from: https://aqli.epic.uchicago.edu/wp-content/uploads/2023/08/US-FactSheet-2023_Final.pdf.
- 2020 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2020;16(3):391-460.
- Prevention CfDCa. Alzheimer’s Disease Mortality by State 2022 [.
- Zacher M, Brady S, Short Susan E. Geographic Patterns of Dementia in the United States: Variation by Place of Residence, Place of Birth, and Subpopulation. The Journals of Gerontology: Series B. 2023;78(7):1192-203.
- Lamar M, Lerner AJ, James BD, Yu L, Glover CM, Wilson RS, Barnes LL. Relationship of Early-Life Residence and Educational Experience to Level and Change in Cognitive Functioning: Results of the Minority Aging Research Study. The Journals of Gerontology: Series B. 2019;75(7):e81-e92.
- Lin Z, Chen X. Place of Birth and Cognitive Function Among Older Americans: Findings From the Harmonized Cognitive Assessment Protocol. The Journals of Gerontology: Series B. 2024;79(9).
- Ho JY, Franco Y. The rising burden of Alzheimer’s disease mortality in rural America. SSM - Population Health. 2022;17:101052.
- Cross SH, Warraich HJ. Rural-Urban Disparities in Mortality from Alzheimer’s and Related Dementias in the United States, 1999–2018. Journal of the American Geriatrics Society. 2021;69(4):1095-6.
- Kulshreshtha A, Ramer S, Cato S, Hajjar I. Alzheimer’s disease mortality high in rural areas in South: 1999-2019. Alzheimer’s & Dementia. 2021;17(S10):e054933.
- Wilson RS, Yu L, Lamar M, Schneider JA, Boyle PA, Bennett DA. Education and cognitive reserve in old age. Neurology. 2019;92(10):e1041-e50.
- Sharp ES, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011;25(4):289-304.
- National Research Council Panel on Race E, Health in Later L. The National Academies Collection: Reports funded by National Institutes of Health. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington (DC): National Academies Press (US) Copyright © 2004, National Academy of Sciences.; 2004. p. 95-141.
- Pappu MSaHV. Population Projections: Illinois, Chicago and Illinois Counties by Age and Sex: July 1, 2015 to July 1, 2030. Illinois Department of Public Health; 2021.
- Rahman M, White EM, Mills C, Thomas KS, Jutkowitz E. Rural-urban differences in diagnostic incidence and prevalence of Alzheimer’s disease and related dementias. Alzheimers Dement. 2021;17(7):1213-30.
- Eren F, Ozturk S. Evaluation of the Effect of Air Pollution on Cognitive Functions, Cognitive Decline, and Dementia. Annals of Indian Academy of Neurology. 2022;25(Suppl 1).
- Chai KC, Li Q, Bao XL, Zhu J, He XX. An Empirical Study of Economic Cycle, Air Quality, and National Health Since Reform and Opening Up. Front Public Health. 2021;9:706955.
- Christensen GM, Li Z, Pearce J, Marcus M, Lah JJ, Waller LA, et al. The complex relationship of air pollution and neighborhood socioeconomic status and their association with cognitive decline. Environ Int. 2022;167:107416.
- Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413-46.
- QuickFacts: Chicago city, Illinois [Internet]. 2022. Available from: https://www.census.gov/quickfacts/chicagocityillinois.
- Hebert LE, Scherr PA, McCann JJ, Beckett LA, Evans DA. Is the Risk of Developing Alzheimer’s Disease Greater for Women than for Men? American Journal of Epidemiology. 2001;153(2):132-6.
- Valls-Pedret C, Sala-Vila A, Serra-Mir M, Corella D, de la Torre R, Martinez-Gonzalez MA, et al. Mediterranean Diet and Age-Related Cognitive Decline: A Randomized Clinical Trial. JAMA Intern Med. 2015;175(7):1094-103.
- Nebel RA, Aggarwal NT, Barnes LL, Gallagher A, Goldstein JM, Kantarci K, et al. Understanding the impact of sex and gender in Alzheimer’s disease: A call to action. Alzheimer’s & Dementia. 2018;14(9):1171-83.
- Liu H, Zhang Z, Choi SW, Langa KM. Marital Status and Dementia: Evidence from the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2020;75(8):1783-95.
- Sol K, Zaheed AB, Kraal AZ, Sharifian N, Arce Rentería M, Zahodne LB. Psychological predictors of memory decline in a racially and ethnically diverse longitudinal sample of older adults in the United States. International Journal of Geriatric Psychiatry. 2020;35(2):204-12.
- Zahodne LB, Sharifian N, Kraal AZ, Zaheed AB, Sol K, Morris EP, et al. Socioeconomic and psychosocial mechanisms underlying racial/ethnic disparities in cognition among older adults. Neuropsychology. 2021;35(3):265-75.
- Zahodne LB, Sol K, Kraal Z. Psychosocial Pathways to Racial/Ethnic Inequalities in Late-Life Memory Trajectories. The Journals of Gerontology: Series B. 2017;74(3):409-18.
- Aranda MP, Kremer IN, Hinton L, Zissimopoulos J, Whitmer RA, Hummel CH, et al. Impact of dementia: Health disparities, population trends, care interventions, and economic costs. J Am Geriatr Soc. 2021;69(7):1774-83.
- Ames BN, Grant WB, Willett WC. Does the High Prevalence of Vitamin D Deficiency in African Americans Contribute to Health Disparities? Nutrients. 2021;13(2):499.
- Lai R-H, Hsu C-C, Yu B-H, Lo Y-R, Hsu Y-Y, Chen M-H, Juang J-L. Vitamin D supplementation worsens Alzheimer’s progression: Animal model and human cohort studies. Aging Cell. 2022;21(8):e13670.
- Littlejohns TJ, Henley WE, Lang IA, Annweiler C, Beauchet O, Chaves PHM, et al. Vitamin D and the risk of dementia and Alzheimer disease. Neurology. 2014;83(10):920-8.
- Olson NL, Albensi BC. Race- and Sex-Based Disparities in Alzheimer’s Disease Clinical Trial Enrollment in the United States and Canada: An Indigenous Perspective. J Alzheimers Dis Rep. 2020;4(1):325-44.
- 2021 Alzheimer’s disease facts and figures. Alzheimers Dement. 2021;17(3):327-406.
- Luchsinger JA, Tang M-X, Stern Y, Shea S, Mayeux R. Diabetes Mellitus and Risk of Alzheimer’s Disease and Dementia with Stroke in a Multiethnic Cohort. American Journal of Epidemiology. 2001;154(7):635-41.
- Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999;53(9):1937-42.
- Cholerton B, Baker LD, Montine TJ, Craft S. Type 2 Diabetes, Cognition, and Dementia in Older Adults: Toward a Precision Health Approach. Diabetes Spectrum. 2016;29(4):210-9.
- de la Monte SM, Wands JR. Alzheimer’s Disease is Type 3 Diabetes—Evidence Reviewed. Journal of Diabetes Science and Technology. 2008;2(6):1101-13.
- Mittal K, Katare DP. Shared links between type 2 diabetes mellitus and Alzheimer’s disease: A review. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2016;10(2, Supplement 1):S144-S9.
- Sędzikowska A, Szablewski L. Insulin and Insulin Resistance in Alzheimer’s Disease. International Journal of Molecular Sciences. 2021;22(18):9987.
- McNay EC, Recknagel AK. Brain insulin signaling: A key component of cognitive processes and a potential basis for cognitive impairment in type 2 diabetes. Neurobiology of Learning and Memory. 2011;96(3):432-42.
- Roy B, Ehlert L, Mullur R, Freeby MJ, Woo MA, Kumar R, Choi S. Regional Brain Gray Matter Changes in Patients with Type 2 Diabetes Mellitus. Scientific Reports. 2020;10(1):9925.
- Koren-Iton A, Salomon-Zimri S, Smolar A, Shavit-Stein E, Dori A, Chapman J, Michaelson DM. Central and Peripheral Mechanisms in ApoE4-Driven Diabetic Pathology. International Journal of Molecular Sciences. 2020;21(4):1289.
- Ketchum FB, Monsees J, Kim AJ, Schmachtenberg T, Kind A, Shah M, et al. Pathways of care: a qualitative study of barriers and facilitators to engaging dementia care among underserved and minority populations in the US and Germany. Aging Ment Health. 2023;27(2):389-98.
- Lesley E. Williamson KES, Catherine J. Evans. Exploring access to community care and emergency department use among people with dementia: A qualitative interview study with people with dementia, and current and bereaved caregivers. International Journal of Geriatric Psychiatry. 2023;38(7).
- Ogunniyi A, Lane KA, Baiyewu O, Gao S, Gureje O, Unverzagt FW, et al. Hypertension and incident dementia in community-dwelling elderly Yoruba Nigerians. Acta Neurologica Scandinavica. 2011;124(6):396-402.
- McGinley MP, Harvey T, Lopez R, Ontaneda D, Buchalter RB. Geographic Disparities in Access to Neurologists and Multiple Sclerosis Care in the United States. Neurology. 2024;102(2):e207916.
- Sharp ES, Gatz M. Relationship Between Education and Dementia: An Updated Systematic Review. Alzheimer Disease & Associated Disorders. 2011;25(4):289-304.
- Zhong T, Li S, Liu P, Wang Y, Chen L. The impact of education and occupation on cognitive impairment: a cross-sectional study in China. Front Aging Neurosci. 2024;16:1435626.
- Gonzalez-Gomez R, Legaz A, Moguilner S, Cruzat J, Hernandez H, Baez S, et al. Educational disparities in brain health and dementia across Latin America and the United States. Alzheimers Dement. 2024;20(9):5912-25.
- Livingston G, Huntley J, Liu KY, Costafreda SG, Selbæk G, Alladi S, et al. Dementia prevention, intervention, and care: 2024 report of the <em>Lancet</em> standing Commission. The Lancet. 2024;404(10452):572-628.
- Stern Y, Arenaza-Urquijo EM, Bartrés-Faz D, Belleville S, Cantilon M, Chetelat G, et al. Whitepaper: Defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimers Dement. 2020;16(9):1305-11.
- Kim Y, Stern Y, Seo SW, Na DL, Jang J-W, Jang H, Association CRRGoKD. Factors associated with cognitive reserve according to education level. Alzheimer’s & Dementia. 2024;20(11):7686-97.
- Cha H, Farina MP, Hayward MD. Socioeconomic status across the life course and dementia-status life expectancy among older Americans. SSM - Population Health. 2021;15:100921.
- Grant WB. Using Multicountry Ecological and Observational Studies to Determine Dietary Risk Factors for Alzheimer’s Disease. J Am Coll Nutr. 2016;35(5):476-89.
- Agarwal P, Leurgans SE, Agrawal S, Aggarwal NT, Cherian LJ, James BD, et al. Association of Mediterranean-DASH Intervention for Neurodegenerative Delay and Mediterranean Diets With Alzheimer Disease Pathology. Neurology. 2023;100(22):e2259-e68.
- Wagner M, Agarwal P, Leurgans SE, Bennett DA, Schneider JA, Capuano AW, Grodstein F. The association of MIND diet with cognitive resilience to neuropathologies. Alzheimers Dement. 2023;19(8):3644-53.
- Dhana K, James BD, Agarwal P, Aggarwal NT, Cherian LJ, Leurgans SE, et al. MIND Diet, Common Brain Pathologies, and Cognition in Community-Dwelling Older Adults. Journal of Alzheimer’s Disease. 2021;83(2):683-92.
- Morris MC, Tangney CC, Wang Y, Sacks FM, Barnes LL, Bennett DA, Aggarwal NT. MIND diet slows cognitive decline with aging. Alzheimer’s & Dementia. 2015;11(9):1015-22.
- Barnes LL, Dhana K, Liu X, Carey VJ, Ventrelle J, Johnson K, et al. Trial of the MIND Diet for Prevention of Cognitive Decline in Older Persons. New England Journal of Medicine. 2023;389(7):602-11.
- Devore EE, Kang JH, Breteler MMB, Grodstein F. Dietary intakes of berries and flavonoids in relation to cognitive decline. Annals of Neurology. 2012;72(1):135-43.
- Agarwal P, Holland TM, James BD, Cherian LJ, Aggarwal NT, Leurgans SE, et al. Pelargonidin and Berry Intake Association with Alzheimer’s Disease Neuropathology: A Community-Based Study. Journal of Alzheimer’s Disease. 2022;88(2):653-61.
- Morris MC, Wang Y, Barnes LL, Bennett DA, Dawson-Hughes B, Booth SL. Nutrients and bioactives in green leafy vegetables and cognitive decline: Prospective study. Neurology. 2018;90(3):e214-e22.
- Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci U S A. 2011;108(7):3017-22.
- Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obesity Reviews. 2011;12(5):e426-e37.
- Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, Williamson A, et al. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex. 2005;15(11):1676-89.
- Erickson KI, Miller DL, Roecklein KA. The Aging Hippocampus:Interactions between Exercise, Depression, and BDNF. The Neuroscientist. 2012;18(1):82-97.
- Wennberg AMV, Wu MN, Rosenberg PB, Spira AP. Sleep Disturbance, Cognitive Decline, and Dementia: A Review. Semin Neurol. 2017;37(4):395-406.
- Ferini-Strambi L. Sleep disorders and increased risk of dementia. European Journal of Neurology. 2022;29(12):3484-5.
- Damsgaard L, Janbek J, Laursen TM, Erlangsen A, Spira AP, Waldemar G. Hospital-diagnosed sleep disorders and incident dementia: a nationwide observational cohort study. European Journal of Neurology. 2022;29(12):3528-36.
- Kitamura T, Miyazaki S, Sulaiman HB, Akaike R, Ito Y, Suzuki H. Insomnia and obstructive sleep apnea as potential triggers of dementia: is personalized prediction and prevention of the pathological cascade applicable? EPMA Journal. 2020;11(3):355-65.
- Ancoli-Israel S, Palmer BW, Cooke JR, Corey-Bloom J, Fiorentino L, Natarajan L, et al. Cognitive effects of treating obstructive sleep apnea in Alzheimer’s disease: a randomized controlled study. J Am Geriatr Soc. 2008;56(11):2076-81.
- Sommerlad A, Ruegger J, Singh-Manoux A, Lewis G, Livingston G. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Neurosurg Psychiatry. 2018;89(3):231-8.
- Agyeman-Manu K, Ghebreyesus TA, Maait M, Rafila A, Tom L, Lima NT, Wangmo D. Prioritising the health and care workforce shortage: protect, invest, together. Lancet Glob Health. 2023;11(8):e1162-e4.
- Rotenstein LS, Brown R, Sinsky C, Linzer M. The Association of Work Overload with Burnout and Intent to Leave the Job Across the Healthcare Workforce During COVID-19. Journal of General Internal Medicine. 2023;38(8):1920-7.
- Thyrian JR, Hertel J, Wucherer D, Eichler T, Michalowsky B, Dreier-Wolfgramm A, et al. Effectiveness and Safety of Dementia Care Management in Primary Care: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74(10):996-1004.
- Wong W. Economic burden of Alzheimer disease and managed care considerations. Am J Manag Care. 2020;26(8 Suppl):S177-s83.
- Pimouguet C, Lavaud T, Dartigues JF, Helmer C. Dementia case management effectiveness on health care costs and resource utilization: a systematic review of randomized controlled trials. The Journal of nutrition, health and aging. 2010;14(8):669-76.
- Skaria AP. The economic and societal burden of Alzheimer disease: managed care considerations. Am J Manag Care. 2022;28(10 Suppl):S188-s96.
- Leniz J, Evans CJ, Yi D, Bone AE, Higginson IJ, Sleeman KE. Formal and Informal Costs of Care for People With Dementia Who Experience a Transition to Hospital at the End of Life: A Secondary Data Analysis. Journal of the American Medical Directors Association. 2022;23(12):2015-22.e5.
- Lastuka A, Breshock MR, McHugh TA, Sogge WT, Swart V, Dieleman JL. U.S. dementia care spending by state: 2010–2019. Alzheimer’s & Dementia. 2024;20(4):2742-51.
- Deb A, Sambamoorthi U, Thornton JD, Schreurs B, Innes K. Direct medical expenditures associated with Alzheimer’s and related dementias (ADRD) in a nationally representative sample of older adults – an excess cost approach. Aging & Mental Health. 2018;22(5):619-24.
- Lin P-J, Zhong Y, Fillit HM, Chen E, Neumann PJ. Medicare Expenditures of Individuals with Alzheimer’s Disease and Related Dementias or Mild Cognitive Impairment Before and After Diagnosis. Journal of the American Geriatrics Society. 2016;64(8):1549-57.
- Aging NNIo. What is mild cognitive impairment? 2021 [.
- Frech FH, Li G, Juday T, Ding Y, Mattke S, Khachaturian A, et al. Economic Impact of Progression from Mild Cognitive Impairment to Alzheimer Disease in the United States. The Journal of Prevention of Alzheimer’s Disease. 2024;11(4):983-91.
- Jetsonen V, Kuvaja-Köllner V, Välimäki T, Selander T, Martikainen J, Koivisto AM. Total cost of care increases significantly from early to mild Alzheimer’s disease: 5-year ALSOVA follow-up. Age and Ageing. 2021;50(6):2116-22.
- Aging NIo. Find an Alzheimer’s Disease Research Center 2023 [Available from: https://www.nia.nih.gov/health/clinical-trials-and-studies/find-alzheimers-disease-research-center.
- Association As. Clinical Trials. nd.
- Huggins LKL, Min SH, Dennis C-A, Østbye T, Johnson KS, Xu H. Interventions to promote dementia knowledge among racial/ethnic minority groups: A systematic review. Journal of the American Geriatrics Society. 2021;70:609 - 21.
- Park J, Wiese LAK, Holt J. Online Chair Yoga and Digital Learning for Rural Underserved Older Adults at Risk for Alzheimer’s Disease and Related Dementias. Clin Gerontol. 2023:1-17.
- Park J, Hung L, Randhawa P, Surage J, Sullivan M, Levine H, Ortega M. ‘Now I can bend and meet people virtually in my home’: The experience of a remotely supervised online chair yoga intervention and visual socialisation among older adults with dementia. International Journal of Older People Nursing. 2023;18(1):e12513.
- Zahodne LB, Sharifian N, Kraal AZ, Sol K, Zaheed AB, Manly JJ, Brickman AM. Positive Psychosocial Factors and Cognitive Decline in Ethnically Diverse Older Adults. Journal of the International Neuropsychological Society. 2021;27(1):69-78.
- Alves LCS, Monteiro DQ, Bento SR, Hayashi VD, Pelegrini LNC, Vale FAC. Burnout syndrome in informal caregivers of older adults with dementia: A systematic review. Dement Neuropsychol. 2019;13(4):415-21.
- Hwang Y, Kim J. Influence of caregivers’ psychological well-being on the anxiety and depression of care recipients with dementia. Geriatric Nursing. 2024;55:44-51.
- Lauritzen J, Pedersen PU, Sørensen EE, Bjerrum MB. The meaningfulness of participating in support groups for informal caregivers of older adults with dementia: a systematic review. JBI Evidence Synthesis. 2015;13(6):373-433.
- Petriwskyj A, Parker D, O’Dwyer S, Moyle W, Nucifora N. Interventions to build resilience in family caregivers of people living with dementia: a comprehensive systematic review. JBI Evidence Synthesis. 2016;14(6):238-73.
- Parker D, Mills S, Abbey JA. Effectiveness of interventions that assist caregivers to support people with dementia living in the community: a systematic review. JBI Database of Systematic Reviews and Implementation Reports. 2008;6:484–544.
- Fillit H, Geldmacher DS, Welter RT, Maslow K, Fraser M. Optimizing Coding and Reimbursement to Improve Management of Alzheimer’s Disease and Related Dementias. Journal of the American Geriatrics Society. 2002;50(11):1871-8.
- Aging NIo. Resources for Health Care Providers: Alzheimer’s and Related Dementias 2024 [Available from: https://www.alzheimers.gov/professionals/health-care-providers.
- Yaffe MJ, Orzeck P, Barylak L. Family physicians’ perspectives on care of dementia patients and family caregivers. Canadian Family Physician. 2008;54(7):1008-15.
- Padala KP, Mendiratta P, Orr LC, Dean KT, Boozer EM, Lensing SY, et al. An Interdisciplinary Approach to Educating Medical Students About Dementia Assessment and Treatment Planning. Fed Pract. 2020;37(10):466-71.
- Organization WH. Dementia. 2023.
- Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. The Lancet Public Health. 2022;7(2):e105-e25.
- Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, et al. Prevalence of Dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology. 2007;29(1-2):125-32.
- Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimer’s & Dementia. 2021;17(12):1966-75.
| Previous count | 2023 Count | 2050 Count | |
| Global | 24 million, as of 2005 [12] | 55 million (WHO, 2023)[126] | 152.8 million [127] |
| United States | 3.4 million, as of 2002 [128] | 6.7 million [4] | 12.7 million [4] |
| Illinois | 230,000 as of 2020 [4] | 260,000 [4] |
| 2024 | 2030 | 2060 | Total Cases* | |
| Female | 4.23 M | 5.17 M | 8.22 M | 17.62 M |
| Male | 2.71 M | 3.37 M | 5.64 M | 11.72 M |
| Age | Illinois 2020 |
U.S. 2020 | Illinois 2025 |
U.S. 2025 | Illinois 2030 |
U.S. 2030 |
| 65-74 | 37,314 | 1.65 M | 42,134 | 1.88 M | 43,950 | 2.05 M |
| 75-84 | 103,270 | 2.18 M | 129,183 | 2.79 M | 157,439 | 3.46 M |
| 85+ | 85,269 | 2.24 M | 90,948 | 2.49 M | 103,908 | 3.03 M |
| Total | 225,853 | 6.07 M | 262,265 | 7.16 M | 305,297 | 8.54 M |
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




