1. Introduction
The World Health Organization (WHO) defines the Rational Use of Medicines (RUM) as; patients receiving medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and their community [
1].
To measure and monitor drug use in an objective manner, the WHO in collaboration with the International Network for Rational Use of Drugs (INRUD) developed a set of drug use indicators for hospitals [
2]. These indicators serve as a tool to monitor and guide the health care services for proper documentation of medicine usage with emphasis on prescribing practices, patient care and facility specific factors [
2]. These include 12 standardized core drug use indicators, of which five are known as “prescribing indicators” designed to measure whether the health care providers prescribe drugs appropriately [
2]. Each indicator has been assigned an optimum score to allow objective assessment [
3].
In addition to monitoring drug use in general, the indicators also specifically monitor the use of antibiotics as their irrational use can lead to antimicrobial resistance (AMR). It is recommended that the antibiotic prescription should be less than 27% of all outpatient prescriptions [
4,
5,
6]. The prescribing indicator on use of antibiotics is further enriched by considering antibiotic usage per the WHO
AWaRe (Access, Watch and Reserve) categories [
7,
8]. The Access category includes antibiotics for empirical treatment of common infections which should be available in all health care settings. The Watch category antibiotics have a higher potential for resistance and their use should be limited. The Reserve category are “last resort” antibiotics and their use should be reserved for special situations with multidrug-resistant bacterial infections where alternative treatments have failed [
7,
8].
A report from WHO showed that half of medicines across the world are prescribed inappropriately, and that half of patients are unable to use their medicines correctly [
1]. The World Bank estimates that medicines account for 20 – 50% of all healthcare expenses in low-and-middle-income countries (LMICs) [
9]. Therefore, RUM is especially important in LMICs such as Ghana that are constrained in terms of resources and effective regulation of use of medications while at the same time grappling with AMR [
10]. According to the WHO Ghana 2023 annual report, AMR was linked to 25,300 deaths in the country [
11]. A situational analysis of antibiotic use and regulation in Ghana conducted in 2017 highlighted that the absence of national antimicrobial policy, weak regulatory environment and non-compliance to practice standards may have contributed to increased and unregulated access to antimicrobials in Ghana [
12].
The Ghana National Drug policy stipulates that there should be routine monitoring of RUM in healthcare facilities using the WHO core indicators [
13]. An operational research (OR) study conducted by Amponsah
et al. in the out-patient department (OPD) of the University Hospital, Kwame Nkrumah University of Science and Technology (KNUST), in 2021 found that only one of the WHO prescribing indicators assessed met WHO optimum levels. In particular, the assessment found antibiotic prescribing to be high at 36% compared to the WHO recommended threshold of <27% [
14,
15].
The findings from the OR study were a clarion call to the KNUST hospital management to improve the prescription practices of medicines, especially antibiotics in the OPD. Following the assessment, antimicrobial stewardship (AMS) program which had been instituted for in-patients was extended to include the outpatient department.
Assessing the impact that these interventions may have made on prescriber compliance to WHO standards of prescribing is imperative, so that informed decisions can be taken to improve rational use of medicines including antibiotics at the OPD of the hospital. Considering the assessment of 2021 as a baseline, this study aimed to assess if there has been any change in drug use as per the WHO prescribing indicators in the OPD of University Hospital, KNUST. The specific objectives were to compare the key WHO prescribing indicators and the pattern of antibiotic prescription according to WHO AWaRe classification among the prescriptions of all the patients who sought care at the OPD of University hospital during the calendar year of 2021 (first OR study) and 2023 (current OR study).
2. Materials and Methods
2.1. Study Design
This study was a comparison of compliance to WHO rational prescribing guidelines using routinely collected data from the Electronic Medical Records (EMR) of out-patients at the University Hospital, KNUST, measured through cross-sectional assessments conducted during 2023 (current study) and 2021 (first OR study).
2.2. General Settings
Ghana is a West African country bordered by Burkina Faso to the north, the Gulf of Guinea to the south, Togo in the east and Cote D’Ivoire in the west [
16]. Administratively, the country is divided into sixteen regions with their regional capitals. Healthcare services in the country is delivered through private and public facilities [
12]. The public facilities include Health Centers, District Hospitals, Regional and Tertiary hospitals [
17] . District hospitals form an important aspect of healthcare provision as the first point of referral [
12]. Medicines prescribed through the National Health Insurance Scheme (NHIS) are dispensed free of cost at health facilities[
18]. Clients can buy medicines including antibiotics, from pharmacies and over the counter (OTC) medicine sellers (for OTC medicines) through out-of-pocket payments.
2.3. Specific Settings
The University Hospital, KNUST, is located in the second largest city in Ghana, Kumasi, the capital of the Ashanti region [
16]. It is a 135-bed capacity quasi-government district-level hospital serving primarily the Oforikrom Municipality with approximately 303,016 inhabitants [
16] . The facility also attends to patients from the municipality’s environs, extending to Northern Ghana. The University Hospital offers primary care services to residents in the municipality and receives referrals from other health facilities. The average OPD footfall per day was 136 patients in 2021.
The point of entry for individuals seeking healthcare at the University Hospital is the OPD. The individuals are checked into the hospital by a receptionist from the Records Department. An account is activated for the individual through the EMR – a web-based electronic medical recording system which connects various departments of the hospital. The hospital attendant is subsequently triaged by a registered nurse and directed to see a prescriber in a consulting room.
A new electronic hospital data management system has been operationalized since December 2022. The current EMR system has modules including an out-patient module with different levels of access granted based on the cadre of the healthcare provider. The demographic data and clinical records including antibiotic prescriptions of patients attending the facility can be accessed using a unique patient identification number.
2.4. Process of Prescription and Issuing of Medicines to Outpatients in University Hospital, KNUST
The medical prescription following the patient encounter is directly documented into the EMR system by the consulting prescriber (medical doctor, dentist, physician assistant, ophthalmic nurse, dialysis nurse, and dental nurse). Treatment advice is immediately received at the pharmacy department via the EMR for dispensing the medicines to the patient. For medicines unavailable at the facility, a paper-based electronic prescription is generated and provided to the patient for purchase from other pharmacies.
2.5. Antimicrobial Stewardship (AMS) Activities Undertaken at University Hospital, KNUST, After the First Operational Research Study
The results of the baseline operational study were disseminated using multiple communication tools targeting decision makers and stakeholders of the University Hospital. This led to the extension of the AMS program to OPD from November 2022, which was previously operationalized only in the inpatient department. Under the AMS program, the healthcare providers were trained in capacity building on rational antibiotic use and infection prevention and control. Measures were undertaken to ensure the documentation of indications for antibiotic prescription through routine monitoring by the AMS team. Health care providers were informed and trained to conduct culture and drug susceptibility analyses before the initiation of empiric antibiotic therapy. In consultation with specialists in the hospital, certain antibiotics were placed on restricted access (requiring prior authorization before use) to reduce their inappropriate use. Dissemination details (Supplementary Table 1) and implementation status of the recommendations (Supplementary Table 2) of the first OR study are provided in the appendix.
2.6. Study Period
The first OR study was conducted utilizing the data collected between January to December 2021. The current study was conducted using data collected between January and December 2023. Data analysis and compilation of results were done between January and March 2025.
2.7. Study Population
The study population in the first OR study and the current study included the prescriptions of all patients who sought care at the OPD of the University Hospital during the calendar years 2021 and 2023.
2.8. Sample Size
Based on the previous study, we expected approximately 350,000 prescriptions between January and December 2023. A prevalence difference of 11% was assumed to be achieved as a decrease in prevalence of antibiotic prescriptions from 36% (2021) to 25% (2023) would bring the indicator to compliance. Hence, the minimum sample size required to be able to identify a prevalence difference of 11% with 95% confidence interval and 80% power was 288 prescriptions from the two assessment periods. However, we considered all the prescriptions from both years.
2.9. Data Collection and Data Variables
The data for this study were extracted from the EMR database by the University IT team. The demographic and clinical characteristics of patients who sought care during the calendar year 2023 were extracted. To compare the compliance with WHO prescribing indicators, the name and class of antibiotics, number of antibiotics prescribed in each patient encounter, route of administration of the medicines were extracted from two calendar years, 2021 and 2023.
2.10. Data Analysis
Data was retrieved in MS Excel format and analyzed using STATA® (version 16.0 Copyright 1985-2019, StataCorp LLC, College Station, TX, USA)). The demographic and clinical characteristics of patients were summarized using frequencies and percentages.
Calculation of indicators was done as shown in
Table 1. Each indicator was summarized as percentage. The indicator “Average number of medicines per patient encounter” was summarized as mean. Each indicator was compared between the first OR study and the current OR study using a test of two proportions. A p-value <0.05 was considered significant.
2.11. Operational Definitions
A consultation with a single patient on a single day in a department of the OPD was considered as a patient encounter. Each medicine prescribed during a patient encounter was considered as a separate prescription. A patient was considered to have been prescribed an antibiotic if any of the prescriptions retrieved against their unique identifier contained an antibiotic. Antibiotics prescribed were categorized according to the WHO AWaRe classification 2023 into Access, Watch, or Reserve group [
19]. The medicines in the prescription were matched with the medicines listed in the Ghana EML to identify whether they were listed in the EML or not.
3. Results
Between January and December 2023, 65,157 patients visited the OPD of KNUST Hospital and recorded 171,517 patient encounters. In comparison, during the same period in 2021, 49,660 patients accounted for 110,280 patient encounters. In 2023, 151,823 total patient encounters led to prescription of at least one medicine. In total, there were 247,313 prescriptions in 2023 compared to 350,149 prescriptions in 2021.
3.1. Demographic and Clinical Characteristics
More than half of the patients in 2023 were female (56.1%) and approximately 45% were between the age group of 15 and 24 years. The mean (SD) age of patients was 28.8 (18.2) years.
Table 2 shows the demographic and clinical characteristics of patients who attended the OPD of University Hospital, KNUST in 2021 and 2023. The general OPD services accounted for about 79% and 86% in 2021 and 2023, respectively. There was statistically significant (p<0.001) increase in the proportion of patients with a single encounter in 2023 compared to 2021 (12.3 % to 41.9%). Also, the proportion of patients with multiple encounters (three and more) decreased in 2023 as compared to 2021 (73% to 38.4%).
3.2. Comparison of Adherence to WHO Prescribing Indicators Between 2021 and 2023
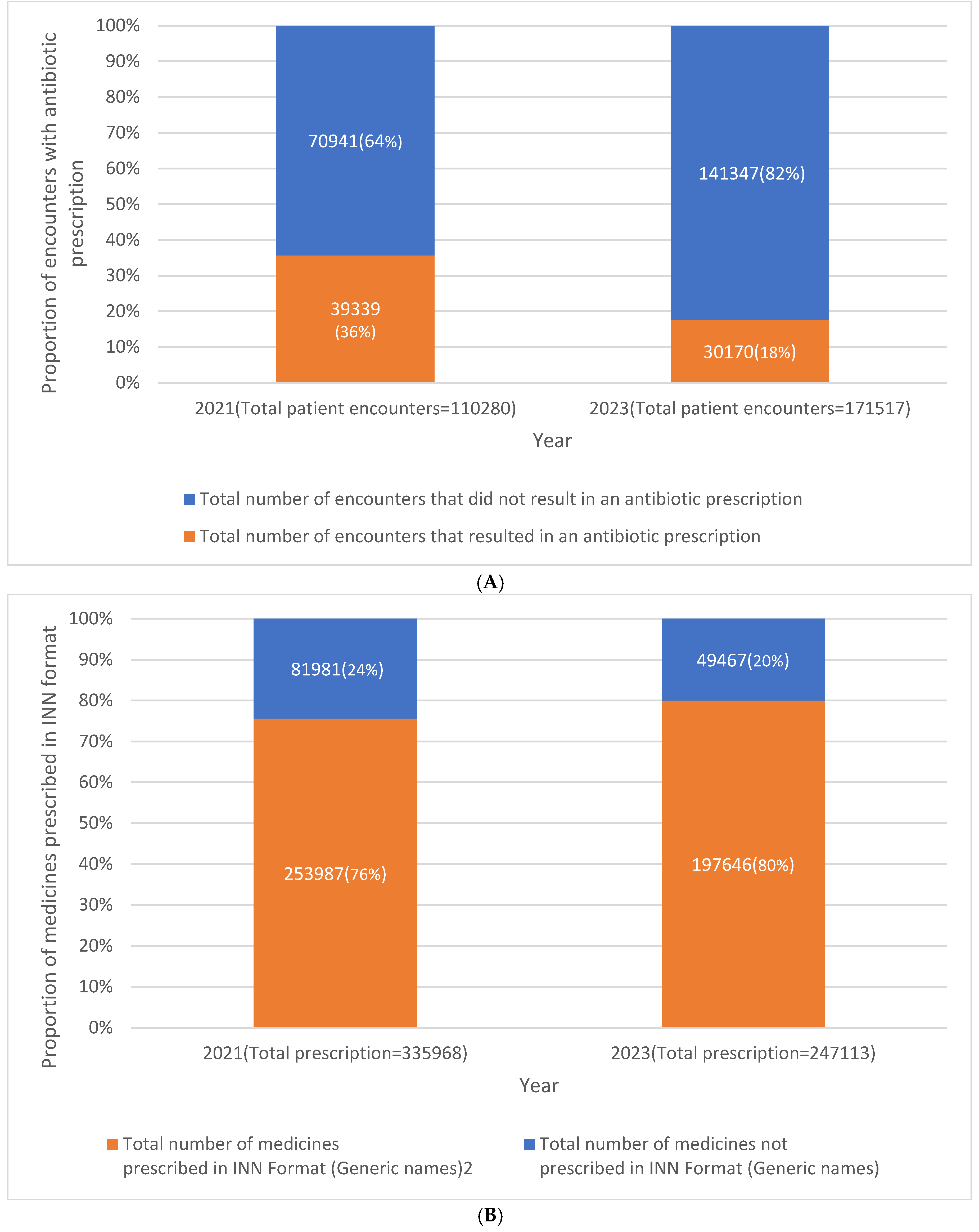
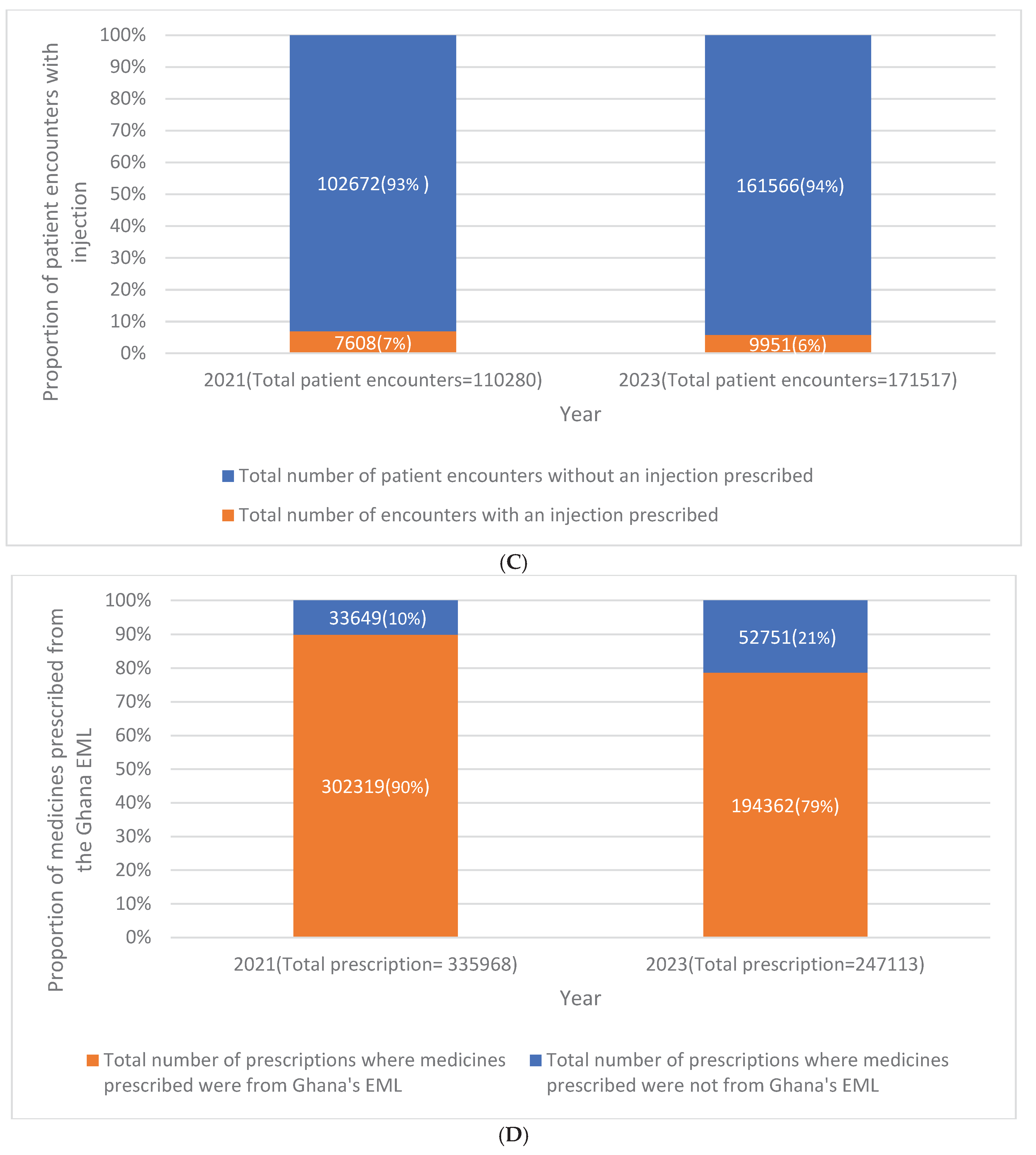
The proportion of patient encounters that resulted in antibiotic prescription decreased significantly from 36% in 2021 to 18% in 2023 (p-value<0.001) (
Figure 1A). The average number of medicines prescribed per encounter reduced to 2 (p<0.001), ranging from 1-21 as compared to 3 in 2021, with a range of 1-18. The proportion of medicines prescribed using generic names increased from 76% in 2021 to 80% in 2023, and this was statistically significant. (
Figure 1B). Compared to 2021, in 2023, the prescription of injections reduced by 1.1 % (p<0.001) (
Figure 1C).
Figure 1D shows that 79% of the medicines prescribed in 2023 were from the Ghana essential medicines list compared to 90% in 2021.
3.3. Pattern of Antibiotic Prescriptions According to the WHO AWaRe (Access, Watch, Reserve) Classification in 2021 and 2023
Table 3 shows the pattern of antibiotic prescriptions by WHO Aware, Watch, and Reserve categories in 2021 and 2023. In both years, approximately 48% of the antibiotics were prescribed from the Access group. The prescription of antibiotics from the Watch group and Reserve group has increased by 4.6% (46.5% in 2021 to 51.1 % in 2023) and 1.7% (1.8% in 2021 to 3.5 in 2023), respectively. The prescription of antibiotics that belong to the Not recommended category has reduced from 3.1% in 2021 to 2.6% in 2023. These differences were found to be statistically significant(p<0.001).
4. Discussion
The present comparative study demonstrated an improvement in the compliance with WHO indicators compared to the baseline OR study conducted in 2021 in the district-level hospital in Ghana [
14,
15]. Three prescribing indicators changed in the hospital OPD setting following the extension of the AMS intervention as a result of the baseline study. First, there was a reduction in the proportion of patient encounters that resulted in antibiotic prescriptions to 18% in 2023 from 36% in 2021. Second, the average number of antibiotics prescribed per encounter was reduced from three to two. Finally, the prescription of injections was reduced further to 6% from 7%. Hence, among the five WHO prescribing indicators, three have achieved levels within the optimum recommended by the WHO.
Our study has several strengths. First, the current study is built on a baseline OR, and the use of cross-sectional assessment before and after the intervention has enabled clear assessment of changes in key indicators. Second, the use of EMR data with very few missing data minimized reporting bias and allowed robust evaluation. Finally, we have adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting this study [
20]. The study has a few limitations. We did not have a control group or setting to compare, so it is difficult to completely rule out the effect of other external factors that might have influenced the observed changes. Hence, the changes observed cannot be completely attributed to the extension of the AMS intervention. However, with the comparison conducted in a time difference of one year in the absence of any other evident changes in the hospital setting other than the AMS intervention, the improvement observed can likely be due to the interventions. Another limitation of our study is that we conducted this study in a single district-level hospital; hence, the findings may not be generalizable to all other settings, particularly rural or private facilities in Ghana.
The study has several policy and practical implications too, for AMR stewardship in the hospital setting. The OPD is often the first point of contact for most patients in a hospital setting in LMICs. However, the AMS Program (ASP) in hospitals is often implemented in inpatient settings. The evidence on their impact in OPDs, particularly in low- and middle-income countries (LMICs), remains limited compared to high-income countries [
21,
22] and our study helps reduce this evidence gap. With the study findings, we highlight the feasibility and utility of extending ASP activities beyond inpatient settings, which is the first and foremost implication of our study.
Secondly, the improvements in the WHO prescribing indicators observed in 2023 may likely be due to the capacity-building interventions, routine audits, and feedback under the ASP, implemented and extended to the outpatient setting of the hospital [
23]. These improvements align with broader efforts seen across African countries, where hospitals are increasingly adopting ASP to improve antibiotic use [
23,
24,
25]. Evidence from antibiotic use assessment across hospitals in Ghana, Uganda, Zambia, and Tanzania also highlights the high empirical use of antibiotics, emphasizing the critical need for strengthening AMS interventions in hospital settings [
26,
27,
28]. Our study thus aligns with the growing momentum for AMS across the continent.
Third, our study has utilized the WHO key prescribing indicators. This has offered insights into their relevance to local practice and to understand whether the international benchmarks are valid in our setting. However, we recommend further research in this area to evaluate its appropriateness and contextual fit of these indicators. In addition, implementation of AMS using practical toolkits, such as those developed by WHO and the Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS), [
29,
30], in achieving measurable improvements, helps us to understand how these can be adopted in our setting.
Finally, analysis of antibiotic prescription patterns using the WHO AWaRe classification demonstrated that the proportion of antibiotics from the Access category remained unchanged in 2021 and 2023. The WHO recommends a target of 70% and above for the Access category of antibiotics [
31]. Similar patterns have been documented in several African countries, with empirical prescribing and limited microbiological support contributing to suboptimal AWaRe distribution, especially with high use of Watch antibiotics [
32]. In some LMIC outpatient hospital settings, Watch group antibiotics have been reported to constitute as high as 60% of total prescriptions [
33]. Even though the increase in Watch and Reserve group antibiotic in our study may potentially be due to clinical necessity in some cases, it is important that continued monitoring and training be conducted due to the higher potential of these categories to drive antimicrobial resistance [
7,
19].
5. Conclusion
The study has demonstrated the importance of operational research, its findings and their impact in real-world patient care settings. The AMR stewardship intervention instituted has significantly improved the rational use of antibiotics and increased compliance with WHO quality standards for prescribing at the OPD of the University Hospital. However, targeted efforts are still needed to further enhance prescribing of the Access group and minimize reliance on Watch and Reserve antibiotics unless clinically justified, as part of sustained interventions to contain antimicrobial resistance. Also, a qualitative exploration to identify enablers and barriers to rational use of antibiotics at the hospital would further guide the scale up and sustainability of the interventions.
Author Contributions
Conceptualization, N.A.A., O.K.O.A., D.N., N.K.A.B; methodology, N.A.A., O.K.O.A., D.N., N.K.A.B.; software, E.K., D.N.; validation, E.K., D.O.A., D.N.; formal analysis, D.N.; investigation, N.A.A., O.K.O.A., D.N., A.B.O., E.K.; data curation, E.K., D.O.A.; writing—original draft preparation, N.A.A., O.K.O.A., K.C.P., D.N.; writing—review and editing, ALL AUTHORS.; visualization, D.N., K.C.P.; supervision K.O.B., N.K.A.B.; project administration, N.A.A., O.K.O.A., A.B.O., N.K.A.B All authors have read and agreed to the published version of the manuscript.
Funding
This operational research was conducted in routine operational settings without any additional funds. However, the proposal and manuscript were developed during the participation of the primary (corresponding) author in a SORT IT course. This SORT IT program was funded by TDR (Grant Number TDR.HQTDR 2422924-4.1-72863). The APC was also funded by TDR. TDR is able to conduct its work thanks to the commitment and support from a variety of funders. A full list of TDR donors is available at: https://tdr.who.int/about-us/our-donors.
Institutional Review Board Statement
The first OR study received ethical approval from the Union Ethics Advisory Group (EAG Number-50/21 dated 13 December 2021) and the Committee on Human Research, Publication and Ethics (CHRPE) of KNUST (CHRPE/AP/066/22 dated 18 February 2022). The results were published in an open-access journal. The previous study was appropriately cited wherever results from that study were reported for the purpose of comparisons in the current study. For this study, permission to access EMR database was obtained from the Director, University Hospital, KNUST. Ethical approval was sought and approved from the Union Ethics Advisory Group, International Union Against Tuberculosis and Lung Disease, Paris, France, and the Committee on Human Research, Publication and Ethics (CHRPE) of KNUST (CHRPE/AP/739/24 dated 1st August 2024).
Informed Consent Statement
As this was a record review study with no patient identifiers, the issue of informed patient consent did not apply.
Data Availability Statement
Requests to access these data should be sent to the corresponding author.
Acknowledgments
This publication was developed through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by TDR, the UNICEF, UNDP, World Bank and WHO Special Program for Research and Training in Tropical Diseases, hosted at the World Health Organization (WHO). This specific SORT IT program that led to this publication included a collaboration between TDR, The Word Health Organization Ghana Country Office, and following Ghanian and International Institutions (listed in alphabetic order). International Institutions: The Centre for Operational Research of the International Union Against Tuberculosis and Lung Disease (The Union), Paris and India offices; The Institute of Tropical Medicine, Antwerp, Belgium; Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Pondicherry; The National TB Control Program of Kyrgyzstan; The Tuberculosis Research and Prevention Center NGO, Armenia. University of St Andrews Medical School, Scotland, UK. Ghana institutions; 37 Military Hospital, Ghana; Bishop Ackon Memorial Christian Eye Centre, Ghana; Council for Scientific and Industrial Research – Animal and Water Research Institutes, Ghana; Environmental Protection Authority, Ghana; Ho Teaching Hospital, Ghana; Korle-Bu Teaching Hospital, Ghana University Hospital;, Kwame Nkrumah University of Science and Technology, Ghana; Department of Pharmacy Practice, Kwame Nkrumah University of Science and Technology, Ghana, Department of Pharmacy Practice, University of Health and Allied Sciences, Ho, Ghana. We gratefully acknowledge the contributions of all participating institutions and partners.
Declaration on Use of Artificial Intelligence
We have not used any form of artificial intelligence for any aspect of drafting this manuscript
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. No conflicts of interest.
Disclaimer
There should be no suggestion that WHO endorses any specific organization, products or services. The views expressed in this article are those of the authors and do not necessarily reflect those of their affiliated institutions. The use of the WHO logo is not permitted.
Appendix A
Appendix A.1. Dissemination Details of the Baseline Operational Research Study
Table A1.
Dissemination details of the baseline operational research study at the University Hospital, KNUST in 2021.
Table A1.
Dissemination details of the baseline operational research study at the University Hospital, KNUST in 2021.
| How |
To Whom |
Where (Number) |
When |
| Stakeholder engagement and communication planning |
Officials of KNUSTAntimicrobial Stewardship Committee, University Hospital, KNUST |
University Hospital, KNUST (13) |
October 2021, June – August; October-December 2022, |
| Evidence summaries (Handouts summarizing study findings) |
Healthcare providers and students of KNUST |
Newsstand of the Dean’s office of the School of Pharmacy, KNUST (Approximately 15 staff and more than 100 students) |
October 2022 to July 2023 |
| Seminar attendees and via email |
Ghana SORT IT AMR dissemination Seminar (36) |
July 2023
|
| PowerPoint presentation and discussions |
The study findings were disseminated during various training seminars conducted for staff of the University Hospital, KNUST and the students at the faculty of Clinical Pharmacy
|
Department of Pharmacy Practice, Faculty of Pharmacy and Pharmaceutical Sciences, KNUST (10) |
December 2022-January 2023
|
| School of Graduate Studies, KNUST (approximately 35) |
July 2023 to present (May 2024) |
| Manuscript full text dissemination via emails |
Representatives of
ReAct Africa (Action on Antibiotic Resistance) AMR Technical Office, Ministry of Health, Ghana Ghana AMR Coordinating Committee
|
|
August 2022 |
| Publication in a peer-reviewed journal |
International Journal of Environmental Research and Public Health (IJERPH) |
Reference 1 [14] (2157 article views according to IJERPH; 16 citations according to Google scholar)
Reference 2 [15] (1582 article views according to IJERPH; 2 citations according to Google scholar) |
August 2022 to present
September 2022 to present |
Appendix A.2. Recommendations and Actions Taken Following the Baseline Operational Research Study
Table A2.
Recommendations and actions taken following the baseline operational research study at the University Hospital, KNUST in 2021.
Table A2.
Recommendations and actions taken following the baseline operational research study at the University Hospital, KNUST in 2021.
| Recommendation |
Action Status |
Details of Action (When and What) |
| EMR is customized to control the prescription of Watch and Reserve antibiotics only to higher ranked prescribers and medical conditions in consultation with pharmacists |
Partially implemented and on-going |
December 2022- present
EMR changed to different type of management software.
Director of Hospital in talks with software managers to incorporate custom controls on antibiotic prescriptions into new software |
| OPD services included in the antimicrobial stewardship program |
Implemented |
July 2023-present
Current iteration of antimicrobial stewardship activities including point prevalence surveys include out- patient services in purview, staff education and capacity building seminars. |
| Six-monthly audit and feedback system for OPD prescriptions have been established |
Implemented |
Nov 2023, May 2024
On-going online point prevalence surveys to audit prescriptions |
| Drafting of an antibiotic prescription policy document on antibiotic prescribing and use at the hospital |
Implemented |
September 2023
A policy document has been developed which covers outpatient and inpatient antibiotic use and the role of all the health cadres in the hospital in prescribing. Provisional approval has been given, awaiting formal adoption by Hospital Management Committee |
| Additional research is planned with the hospital management as a follow-up on outpatient and inpatient antibiotic use practices in the hospital. |
Partially implemented and ongoing |
November 2023-present
In-patient and out-patient point prevalence surveys ongoing. Routine audits of prescriptions on going.
Publication for antibiogram developed on account of activities undertaken by AMS team under review by JAC-Antimicrobial Resistance |
| Training seminars on AMR, AMS, and IPC organized for all health cadres at the hospital |
Implemented and ongoing |
July 2023-present
Since inception of the AMS committee, various training seminars have been organized for staff of the university hospital on AMR.
Newly appointed staff orientation exercise also includes AMR/AMS as important topic so that all staff are kept abreast of guidance before starting official duties at the hospital. |
| Additional funding for AMS, laboratory infrastructure and research |
Partially implemented and ongoing |
June 2023
Expansion of microbiology laboratory and acquisition of new equipment at the university hospital to conduct culture and sensitivity testing |
References
- World Health Organization Promoting Rational Use of Medicines: Core Components. Available online: https://apps.who.int/iris/bitstream/handle/10665/67438/WHO_EDM_2002.3.pdf (accessed on 5 August 2022).
- World Health Organization Action Programme on Essential Drugs and Vaccines How to Investigate Drug Use in Health Facilities : Selected Drug Use Indicators. Available online: https://apps.who.int/iris/handle/10665/60519 (accessed on 2 November 2021).
- Isah, A.; Laing, R.; Quick, J.; Mabadeje, A.F.B.; Santoso, B.; Hogerzeil, H.; Ross-Degnan, D. The Development of Reference Values for the WHO Health Facility Core Prescribing Indicators. West Afr. J. Pharmacol. Drug Res. 2001, 18, 6–11. [Google Scholar] [CrossRef]
- Ofori-Asenso, R. A Closer Look at the World Health Organization’s Prescribing Indicators. J Pharmacol Pharmacother 2016, 7, 51–54. [Google Scholar] [CrossRef]
- Ofori-Asenso, R.; Agyeman, A.A. A Review of Injection and Antibiotic Use at Primary Health Care (Public and Private) Centers in Africa. J. Pharm. Bioallied Sci. 2015, 7, 175–180. [Google Scholar] [CrossRef]
- Hypertension.
- Hsia, Y.; Lee, B.R.; Versporten, A.; Yang, Y.; Bielicki, J.; Jackson, C.; Newland, J.; Goossens, H.; Magrini, N.; Sharland, M. Use of the WHO Access, Watch, and Reserve Classification to Define Patterns of Hospital Antibiotic Use (AWaRe): An Analysis of Paediatric Survey Data from 56 Countries. Lancet Glob. Heal. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- WHO WHO Releases the 2019 AWaRe Classification Antibiotics. Who 2019.
- Govindaraj, R.; Reich, M.R.; Cohen, J.C. World Bank Pharmaceuticals. Available online: https://openknowledge.worldbank.org/handle/10986/13734 License: CC BY 3.0 IGO. (accessed on 7 August 2022).
- Haque, M. Antimicrobial Use, Prescribing, and Resistance in Selected Ten Selected Developing Countries: A Brief Overview. Asian J. Pharm. Clin. Res. 2017, 10, 37–45. [Google Scholar] [CrossRef]
- World Health Organization 2023 Annual Report: WHO Ghana | WHO | Regional Office for Africa.
- Yevutsey, S.K.; Buabeng, K.O.; Aikins, M.; Anto, B.P.; Biritwum, R.B.; Frimodt-Møller, N.; Gyansa-Lutterodt, M. Situational Analysis of Antibiotic Use and Resistance in Ghana: Policy and Regulation. BMC Public Health 2017, 17, 896–902. [Google Scholar] [CrossRef]
- Ministry of Health Ghana National Drug Policy | Source.
- Amponsah, O.K.O.; Nagaraja, S.B.; Ayisi-Boateng, N.K.; Nair, D.; Muradyan, K.; Asense, P.S.; Wusu-Ansah, O.K.; Terry, R.F.; Khogali, M.; Buabeng, K.O. High Levels of Outpatient Antibiotic Prescription at a District Hospital in Ghana: Results of a Cross Sectional Study. Int. J. Environ. Res. Public Health 2022, 19. [Google Scholar] [CrossRef]
- Amponsah, O.K.O.; Ayisi-Boateng, N.K.; Nagaraja, S.B.; Nair, D.; Muradyan, K.; Hedidor, G.K.; Labi, A.K.; Opare-Addo, M.N.A.; Sarkodie, E.; Buabeng, K.O. Adherence to Prescribing Indicators at a District Hospital in Ghana: Do We Match WHO Standards? Int. J. Environ. Res. Public Health 2022, 19. [Google Scholar] [CrossRef]
- 2021 Population and Housing Census - Ghana Statistical Service. Available online: https://census2021.statsghana.gov.gh/ (accessed on 3 November 2021).
- Ministry of Health (MoH) Overview of the Health System in Ghana. Ghana Serv. Provis. Assess. Surv. 2020 2020, 13–24.
- Ghana National Drugs Programme Essential Medicines List. Available online: https://www.moh.gov.gh/wp-content/uploads/2020/07/GHANA-EML-2017.pdf (accessed on 27 August 2022).
- The World Health Organization AWaRe Classification of Antibiotics for Evaluation and Monitoring of Use. 2023. WHO https//www. who. int/publications/i/item/WHO-MHP-HPS-EML-2023.04 2023, 11. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbrouckef, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- Sayood, S.; Durkin, M.J. The Challenge of Outpatient Antibiotic Stewardship. JAMA Netw. Open 2023, 6, e2312996–e2312996. [Google Scholar] [CrossRef] [PubMed]
- Drekonja, D.M.; Filice, G.A.; Greer, N.; Olson, A.; MacDonald, R.; Rutks, I.; Wilt, T.J. Antimicrobial Stewardship in Outpatient Settings: A Systematic Review. Infect. Control Hosp. Epidemiol. 2015, 36, 142–152. [Google Scholar] [CrossRef]
- Amponsah, O.K.O.; Courtenay, A.; Ayisi-Boateng, N.K.; Abuelhana, A.; Opoku, D.A.; Blay, L.K.; Abruquah, N.A.; Osafo, A.B.; Danquah, C.B.; Tawiah, P.; et al. Assessing the Impact of Antimicrobial Stewardship Implementation at a District Hospital in Ghana Using a Health Partnership Model. JAC-Antimicrobial Resist. 2023, 5. [Google Scholar] [CrossRef] [PubMed]
- Saleem, Z.; Godman, B.; Cook, A.; Khan, M.A.; Campbell, S.M.; Seaton, R.A.; Siachalinga, L.; Haseeb, A.; Amir, A.; Kurdi, A.; et al. Ongoing Efforts to Improve Antimicrobial Utilization in Hospitals among African Countries and Implications for the Future. Antibiotics 2022, 11, 1824. [Google Scholar] [CrossRef]
- Ghana National Action Plan for Antimicrobial Use and Resistance Republic of Ghana 2017.
- Amponsah, O.K.O.; Buabeng, K.O.; Owusu-Ofori, A.; Ayisi-Boateng, N.K.; Hämeen-Anttila, K.; Enlund, H. Point Prevalence Survey of Antibiotic Consumption across Three Hospitals in Ghana. JAC-Antimicrobial Resist. 2021, 3, 1–7. [Google Scholar] [CrossRef] [PubMed]
- D’Arcy, N.; Ashiru-Oredope, D.; Olaoye, O.; Afriyie, D.; Akello, Z.; Ankrah, D.; Asima, D.; Banda, D.C.; Barrett, S.; Brandish, C.; et al. Antibiotic Prescribing Patterns in Ghana, Uganda, Zambia and Tanzania Hospitals: Results from the Global Point Prevalence Survey (G-PPS) on Antimicrobial Use and Stewardship Interventions Implemented. Antibiot. 2021, Vol. 10, Page 1122 2021, 10, 1122. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.A.; Vlieghe, E.; Mendelson, M.; Wertheim, H.; Ndegwa, L.; Villegas, M. V.; Gould, I.; Levy Hara, G. Antibiotic Stewardship in Low- and Middle-Income Countries: The Same but Different? Clin. Microbiol. Infect. 2017, 23, 812–818. [Google Scholar] [CrossRef]
- Commonwealth Pharmacists Association Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS) Toolkit; 2020.
- World Health Organization Antimicrobial Stewardship Programmes in Health-Care Facilities in Low- and Middle-Income Countries: A WHO Practical Toolkit; 2019; Vol. 1; ISBN 9789241515481.
- Organization World Health Global Antimicrobial Resistance and Use Surveillance System (GLASS). Antibiotic Use Data for 2022; 2025.
- Wieters, I.; Johnstone, S.; Makiala-Mandanda, S.; Poda, A.; Akoua-Koffi, C.; Abu Sin, M.; Eckmanns, T.; Galeone, V.; Kaboré, F.N.; Kahwata, F.; et al. Reported Antibiotic Use among Patients in the Multicenter ANDEMIA Infectious Diseases Surveillance Study in Sub-Saharan Africa. Antimicrob. Resist. Infect. Control 2024, 13, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Nasehi, M.M.; Effatpanah, M.; Gholamnezhad, M.; Karami, H.; Ghamkhar, M.; Armand, N.; Sohi, Y.H.; Mehrizi, R.; Ghamkhar, L. Antibiotic Prescription Prevalence in Iranian Outpatients: A Focus on Defined Daily Doses and the AWaRe Classification System. Am. J. Infect. Control 2024, 52, 1359–1365. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).