Submitted:
15 July 2025
Posted:
17 July 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Population and Data
2.2. Statistical Analysis
3. Results
3.1. Patient Factors by Frailty Group and Age Group
3.2. Post-Operative Outcomes by Frailty
3.3. Post-Operative Outcomes by Age
3.4. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NSQIP | National Surgery Quality Improvement Program |
| mFI-5 | 5 factor modified frailty index |
| ACS | American College of Surgeons |
| BMI | Body mass index |
| AJCC | American Joint Committee on Cancer |
| DM | Diabetes mellitus |
| CHF | Congestive heart failure |
| COPD | Chronic obstructive pulmonary disease |
| AAPI | Asian American and Pacific Islander |
| SSI | Surgical site infection |
| C. diff | Clostridioides difficile |
| PE | Pulmonary embolism |
| UTI | Urinary tract infection |
| CVA | Cerebrovascular accident |
| CPR | Cardiopulmonary resuscitation |
| MI | Myocardial infraction |
| DVT | Deep vein thrombosis |
| aOR | Adjusted odds ratio |
| CI | Confidence interval |
| IQR | Interquartile range |
| OR | Operating room |
| ASA | American Society of Anesthesiologists |
| ICU | Intensive care unit |
References
- Itatani, Y., K. Kawada, and Y. Sakai. Treatment of Elderly Patients with Colorectal Cancer. BioMed Research International, 2018. 2018: p. 1-8.
- Agathis, A.Z.; Bangla, V.G.; Divino, C.M. Assessing the mFI-5 frailty score and functional status in geriatric patients undergoing inguinal hernia repairs. Hernia 2023, 28, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.-S.; Watts, J.N.; Peel, N.M.; Hubbard, R.E. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fedewa, S.A.; Ahnen, D.J.; Meester, R.G.S.; Barzi, A.; Jemal, A. Colorectal cancer statistics, 2017. CA: A Cancer Journal for Clinicians, 2017. 67(3): p. 177-193.
- Davey, M.G.; Joyce, W.P. Impact of frailty on oncological outcomes in patients undergoing surgery for colorectal cancer – A systematic review and meta-analysis. Surg. 2022, 21, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Niemeläinen, S.; Huhtala, H.; Ehrlich, A.; Kössi, J.; Jämsen, E.; Hyöty, M. Surgical and functional outcomes and survival following Colon Cancer surgery in the aged: a study protocol for a prospective, observational multicentre study. BMC Cancer, 2021. 21(1).
- Moreno-Carmona, M.R.; Serra-Prat, M.; Riera, S.A.; Estrada, O.; Ferro, T.; Querol, R. Effect of frailty on postoperative complications, mortality, and survival in older patients with non-metastatic colon cancer: A systematic review and meta-analysis. J. Geriatr. Oncol. 2023, 15, 101639. [Google Scholar] [CrossRef] [PubMed]
- Dressler, J.A.; Shah, N.; Lueckel, S.N.M.; Cioffi, W.G.J. Predicting Anastomotic Leak After Elective Colectomy: Utility of a Modified Frailty Index. Dis. Colon Rectum 2021, 65, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, S.; Aalberg, J.J.; Soriano, R.P.; Divino, C.M. New 5-Factor Modified Frailty Index Using American College of Surgeons NSQIP Data. J. Am. Coll. Surg. 2018, 226, 173–181e8. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.Y.; Stem, M.; Cerullo, M.; Gearhart, S.L.; Safar, B.; Fang, S.H.; Weiss, M.J.; He, J.; Efron, J.E. The Effect of Frailty Index on Early Outcomes after Combined Colorectal and Liver Resections. J. Gastrointest. Surg. 2017, 22, 640–649. [Google Scholar] [CrossRef] [PubMed]
- McGovern, J.; Grayston, A.; Coates, D.; Leadbitter, S.; Hounat, A.; Horgan, P.G.; Dolan, R.D.; McMillan, D.C. The relationship between the modified frailty index score (mFI-5), malnutrition, body composition, systemic inflammation and short-term clinical outcomes in patients undergoing surgery for colorectal cancer. BMC Geriatr. 2023, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sibia, U.S.; Badve, S.B.; Istl, A.C.; Klune, J.R.; Riker, A.I. Impact of Frailty Upon Surgical Decision-Making for Left-Sided Colon Cancer. Ochsner J. 2023, 23, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Spence, R.T.; Hirpara, D.H.; Doshi, S.; Quereshy, F.A.; Chadi, S.A. Will My Patient Survive an Anastomotic Leak? Predicting Failure to Rescue Using the Modified Frailty Index. Ann. Surg. Oncol. 2020, 28, 2779–2787. [Google Scholar] [CrossRef] [PubMed]
- Obeid, N.M.; Azuh, O.; Reddy, S.; Webb, S.; Reickert, C.; Velanovich, V.; Horst, H. M.; Rubinfeld, I. Predictors of critical care-related complications in colectomy patients using the National Surgical Quality Improvement Program: exploring frailty and aggressive laparoscopic approaches. J Trauma Acute Care Surg, 2012. 72(4): p. 878-83.
- Normann, M.; Ekerstad, N.; Angenete, E.; Prytz, M. Frailty Is an Independent Marker of Post-Operative Mortality Following Colorectal Cancer Resection Surgery in Older Adults. J. Surg. Oncol. 2025. [Google Scholar] [CrossRef] [PubMed]
- Joseph, B.; Saljuqi, A.T.; Amos, J.D.; Teichman, A.; Whitmill, M.L.; Anand, T.; Hosseinpour, H.; Burruss, S.K.; Dunn, J.A.; Najafi, K.; et al. Prospective validation and application of the Trauma-Specific Frailty Index: Results of an American Association for the Surgery of Trauma multi-institutional observational trial. J. Trauma Acute Care Surg. 2022, 94, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Neuman, H.B.; O'COnnor, E.S.; Weiss, J.; LoConte, N.K.; Greenblatt, D.Y.; Greenberg, C.C.; Smith, M.A. Surgical treatment of colon cancer in patients aged 80 years and older. Cancer 2012, 119, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Vetrano, D.L.; Palmer, K.; Marengoni, A.; Marzetti, E.; Lattanzio, F.; Roller-Wirnsberger, R.; Samaniego, L.L.; Rodríguez-Mañas, L.; Bernabei, R.; Onder, G. Frailty and Multimorbidity: A Systematic Review and Meta-analysis. Journals Gerontol. Ser. A 2018, 74, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Chok, A.Y.; Tan, I.E.-H.; Zhao, Y.; Chee, M.Y.M.; Chen, H.L.R.; Ang, K.A.; Au, M.K.H.; Tan, E.J.K.W. Clinical outcomes and cost comparison of laparoscopic versus open surgery in elderly colorectal cancer patients over 80 years. Int. J. Color. Dis. 2023, 38, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.-C.; Lu, C.-T.; Chang, K.-Y.; Chun-Li, W.; Wu, C.-Y. Robot-assisted vs. laparoscopic right hemicolectomy in octogenarians and nonagenarians: an analysis of the US nationwide inpatient sample 2005–2018. Aging Clinical and Experimental Research, 2024. 36(1).
- Saur, N.M.; Davis, B.R.; Montroni, I.M.; Shahrokni, A.M.; Rostoft, S.M.; Russell, M.M.; Mohile, S.G.M.; Suwanabol, P.A.; Lightner, A.L.; Poylin, V.; et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Perioperative Evaluation and Management of Frailty Among Older Adults Undergoing Colorectal Surgery. Dis. Colon Rectum 2022, 65, 473–488. [Google Scholar] [CrossRef] [PubMed]
|
Overall N=10,815 |
Non-frail (mFI-5=0) N=2,372 (21.9%) |
Mildly frail (mFI-5=1) N=5,540 (51.2%) |
Severely Frail (mFI-5=2 or more) N=2,903 (26.8%) |
p-value | |
| Age Group | <0.001* | ||||
| 80-89 (octogenarian) | 9,530/10,815 (88.1) | 2,088/2,372 (88.0) | 4,824/5,540 (87.1) | 2,618/2,903 (90.2) | |
| 90+ (nonagenarian) | 1,285/10,815 (11.9) | 284/2,372 (12.0) | 716/5,540 (12.9) | 285/2,903 (9.8) | |
| Sex | <0.001* | ||||
| Female | 6,027/10,815 (55.7) | 1,341/2,372 (56.5) | 3,168/5,540 (57.2) | 1,518/2,903 (52.3) | |
| Male | 4,788/10,815 (44.3) | 1,031/2,372 (43.5) | 2,372/5,540 (42.8) | 1,385/2,903 (47.7) | |
| Race | <0.001* | ||||
| AAPI | 465/8,340 (5.6) | 89/1,740 (5.1) | 217/4,340 (5.0) | 159/2,260 (7.0) | |
| Black | 545/8,340 (6.5) | 68/1,740 (3.9) | 265/4,340 (6.1) | 212/2,260 (9.4) | |
| White | 7,284/8,340 (87.3) | 1,570/1,740 (92.0) | 3,841/4,340 (88.5) | 1,873/2,260 (82.9) | |
| Other | 46/8,340 (0.6) | 13/1,740 (0.7) | 17/4,340 (0.4) | 16/2,260 (0.7) | |
| Hispanic Ethnicity | <0.001* | ||||
| Yes | 316/8,454 (3.7) | 69/1,763 (3.9) | 128/4,377 (2.9) | 119/2,314 (5.1) | |
| No | 8,138/8,454 (96.3) | 1,694/1,763 (96.1) | 4,249/4,377 (97.1) | 2,195/2,314 (94.9) | |
| BMI | <0.001* | ||||
| Normal Weight 18.5-24.9 | 4,108/10,815 (38.0) | 1,137/2,372 (47.9) | 2,102/5,540 (37.9) | 869/2,903 (29.9) | |
| Underweight <18.5 | 400/10,815 (3.7) | 148/2,372 (6.2) | 167/5,540 (3.0) | 85/2,903 (2.9) | |
| Overweight 25.0-29.9 | 3,926/10,815 (36.3) | 765/2,372 (32.3) | 2,101/5,540 (37.9) | 1,060/2,903 (36.5) | |
| Obese >29.9 | 2,381/10,815 (22.0) | 322/2,372 (13.6) | 1,170/5,540 (21.1) | 889/2,903 (30.6) | |
| Pre-operative Mechanical Bowel Prep | 0.522 | ||||
| Yes | 6,906/9,590 (72.0) | 1,509/2,124 (71.0) | 3,531/4,880 (72.4) | 1,866/2,586 (72.2) | |
| No | 2,684/9,590 (28.0) | 615/2,124 (29.0) | 1,349/4,880 (27.6) | 720/2,586 (27.8) | |
| Pre-operative Oral Antibiotic Prep | 0.385 | ||||
| Yes | 5,732/9,713 (59.0) | 1,238/2,144 (57.7) | 2,954/4,966 (59.5) | 1,540/2,603 (59.2) | |
| No | 3,981/9,713 (41.0) | 906/2,144 (42.3) | 2,012/4,966 (40.5) | 1,063/2,603 (40.8) | |
| Chemotherapy within 90 Days | 0.135 | ||||
| Yes | 407/10,700 (3.8) | 104/2,343 (4.4) | 206/5,491 (3.8) | 97/2,866 (3.4) | |
| No | 10,293/10,700 (96.2) | 2,239/2,343 (95.6) | 5,285/5,491 (96.2) | 2,769/2,866 (96.6) | |
| Clinical Stage |
0.173 |
||||
| Stage 0 | 178/10,289 (1.7) | 39/2,264 (1.7) | 91/5,253 (1.7) | 48/2,772 (1.7) | |
| Stage I | 2,298/10,289 (22.3) | 468/2,264 (20.7) | 1,207/5,253 (23.0) | 623/2,772 (22.5) | |
| Stage II | 4,467/10,289 (43.4) | 998/2,264 (44.1) | 2,302/5,253 (43.8) | 1,167/2,772 (42.1) | |
| Stage III | 3,346/10,289 (32.5) | 759/2,264 (33.5) | 1,653/5,253 (31.5) | 2934/2,772 (33.7) | |
| Operative Approach | 0.591 | ||||
| Laparoscopic | 4,401/6,564 (67.0) | 958/1,418 (67.6) | 2,314/3,462 (67.5) | 1,129/1,720 (65.5) | |
| Robotic | 736/6,564 (11.2) | 149/1,418 (10.5) | 382/3,462 (11.2) | 205/1,720 (11.9) | |
| Open | 1,472/6,564 (21.7) | 311/1,418 (21.9) | 730/3,462 (21.3) | 386/1,720 (22.4) | |
| Total Operation Time | |||||
| Median [IQR] | 150 [110,204] | 150 [112,203] | 149 [108,202] | 152 [112,207] | 0.069 |
| Unplanned re-operation | Unplanned intubation | Mortality | ||||
| aOR (95% CI) | p-value | aOR (95% CI) | p-value | aOR (95% CI) | p-value | |
| Age (years) | ||||||
| 80-89 (octogenarian) | Ref | --- | Ref | --- | Ref | --- |
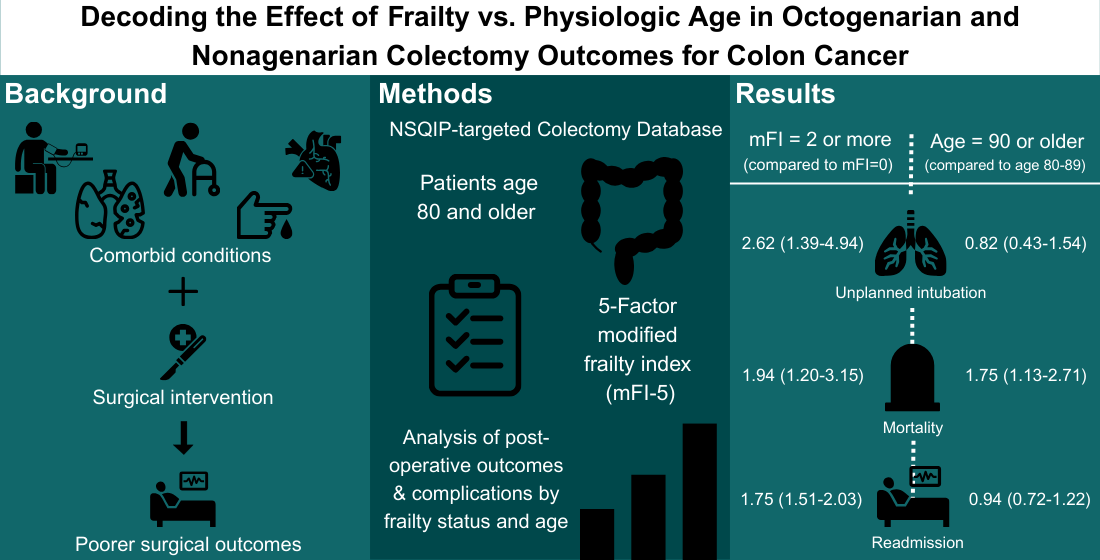
| 90+ (nonagenarian) | 0.83 (0.55-1.27) | 0.393 | 0.82 (0.43-1.54) | 0.531 | 1.75 (1.13-2.71) | 0.012 |
| Sex | ||||||
| Female | Ref | --- | Ref | --- | Ref | --- |
| Male | 1.42 (1.10-1.85) | 0.005* | 1.45 (0.99-2.13) | 0.056 | 1.88 (1.34-2.65) | <0.001* |
| Race | ||||||
| Black | 1.41 (0.68-2.93) | 0.355 | 1.77 (0.70-4.77) | 0.257 | 2.39 (0.86-6.60) | 0.093 |
| Other | 0.82 (0.10-6.55) | 0.853 | --- | --- | 6.07 (1.14-32.30) | 0.035 |
| AAPI | Ref | --- | Ref | --- | Ref | --- |
| White | 1.38 (0.78-2.43) | 0.265 | 1.33 (0.60-2.94) | 0.490 | 2.21 (0.95-5.14) | 0.066 |
| Ethnicity | ||||||
| Hispanic | 1.45 (0.75-2.81) | 0.269 | 2.04 (0.87-4.77) | 0.100 | 0.62 (0.19-2.00) | 0.426 |
| Non-Hispanic | Ref | --- | Ref | --- | Ref | --- |
| BMI | ||||||
| Normal weight 18.5-24.9 | Ref | --- | Ref | --- | Ref | --- |
| Underweight <18.5 | 0.74 (0.34-1.61) | 0.444 | 1.09 (0.38-3.08) | 0.875 | 3.74 (2.05-6.83) | <0.001* |
| Overweight 25.0-29.9 | 0.78 (0.58-1.04) | 0.090 | 0.84 (0.54-1.32) | 0.448 | 1.00 (0.68-1.48) | 0.998 |
| Obese >29.9 | 0.58 (0.40-0.85) | 0.005* | 0.90 (0.54-1.50) | 0.690 | 0.79 (0.48-1.29) | 0.345 |
| Chemotherapy within 90 days | ||||||
| Yes | 0.74 (0.36-1.54) | 0.420 | 0.62 (0.19-2.01) | 0.428 | 1.29 (0.59-2.84) | 0.530 |
| No | Ref | --- | Ref | --- | Ref | --- |
| Pre-operative mechanical bowel prep | ||||||
| Yes | 0.73 (0.52-1.02) | 0.062 | 1.22 (0.75-2.00) | 0.422 | 0.85 (0.56-1.29) | 0.440 |
| No | Ref | --- | Ref | --- | Ref | --- |
| Pre-operative oral antibiotic prep | ||||||
| Yes | 0.93 (0.68-1.28) | 0.668 | 0.49 (0.32-0.75) | 0.001* | 0.62 (0.42-0.90) | 0.013 |
| No | Ref | --- | Ref | --- | Ref | --- |
| Clinical stage | ||||||
| Stage 0 | Ref | --- | Ref | --- | Ref | --- |
| Stage I | 2.21 (0.53-9.30) | 0.278 | 0.89 (0.21-3.90) | 0.881 | 1.28 (0.30-5.53) | 0.743 |
| Stage II | 2.52 (0.61-10.43) | 0.203 | 0.97 (0.23-4.14) | 0.972 | 1.25 (0.29-5.27) | 0.766 |
| Stage III | 2.27 (0.54-9.45) | 0.261 | 0.88 (0.21-3.80) | 0.868 | 1.61 (0.38-6.82) | 0.520 |
| mFI | ||||||
| 0 | Ref | --- | Ref | --- | Ref | --- |
| 1 | 1.40 (0.98-2.00) | 0.068 | 1.78 (0.96-3.27) | 0.066 | 1.09 (0.69-1.75) | 0.706 |
| 2 or more | 1.49 (1.01-2.22) | 0.047 | 2.62 (1.39-4.94) | 0.003* | 1.94 (1.20-3.15) | 0.007* |
| Total OR time | 1.003 (1.001-1.004) | 0.001* | 1.002 (1.000-1.004) | 0.077 | 1.000 (0.998-1.003) | 0.670 |
|
Overall N=10,815 |
Non-frail (mFI-5=0) N=2,372 (21.9%) |
Mildly frail (mFI-5=1) N=5,540 (51.2%) |
Severely Frail (mFI-5=2 or more) N=2,903 (26.8%) |
p-value | |
| Anastomotic leak | 247/10,815 (2.3) | 51/2,372 (2.2) | 123/5,540 (2.2) | 73/2,903 (2.5) | 0.662 |
| Prolonged Nasogastric Tube | 1,554/10,815 (14.4) | 276/2,372 (11.6) | 812 /5,540 (14.7) | 466/2,903 (16.1) | <0.001* |
| Superficial Incisional SSI |
246/10,815 (2.3) | 58/2,372 (2.4) | 110/5,540 (2.0) | 78/2,903 (2.7) | 0.100 |
| Deep Incisional SSI | 33/10,815 (0.3) | 11/2,372 (0.5) | 10/5,540 (0.2) | 12/2,903 (0.4) | 0.052 |
| Organ/Space SSI | 304/10,815 (2.8) | 66/2,372 (2.8) | 142/5,540 (2.6) | 96/2,903 (3.3) | 0.145 |
| Wound Disruption | 49/10,815 (0.5) | 12/2,372 (0.5) | 24/5,540 (0.4) | 13/2,903 (0.4) | 0.906 |
| Pneumonia | 322/10,815 (3.0) | 54/2,372 (2.3) | 156/5,540 (2.8) | 112/2,903 (3.9) | 0.002* |
| Unplanned Intubation | 178/10,815 (1.6) | 24/2,372 (1.0) | 84/5,540 (1.5) | 70/2,903 (2.4) | <0.001* |
| Pulmonary Embolism | 87/10,815 (0.8) | 17/2,372 (0.7) | 45/5,540 (0.8) | 25/2,903 (0.9) | 0.839 |
| Mechanical Ventilation for > 48 Hours | 100/10,815 (0.9) | 15/2,372 (0.6) | 47/5,540 (0.8) | 38/2,903 (1.3) | 0.027* |
| Acute Renal Failure | 43/10,815 (0.4) | 10/2,372 (0.4) | 20/5,540 (0.4) | 13/2,903 (0.4) | 0.816 |
| Urinary Tract Infection | 274/10,815 (2.5) | 61/2,372 (2.6) | 117/5,540 (2.1) | 96/2,372 (3.3) | 0.004* |
| Stroke/CVA | 65/10,815 (0.6) | 6/2,372 (0.3) | 25/5,540 (0.5) | 34/2,903 (1.2) | <0.001* |
| Cardiac Arrest Requiring CPR | 77/10,815 (0.7) | 9/2,372 (0.4) | 40/5,540 (0.7) | 28/2,903 (1.0) | 0.042* |
| Myocardial Infarction | 173/10,815 (1.6) | 22/2,372 (0.9) | 95/5,540 (1.7) | 56/2,903 (1.9) | 0.010* |
| Transfusions intra-op/post-op | 1,343/10,815 (12.4) | 240/2,372 (10.1) | 672/5,540 (12.1) | 431/2,903 (14.8) | <0.001* |
| DVT Requiring Therapy | 98/10,815 (0.9) | 15/2,372 (0.6) | 53/5,540 (1.0) | 30/2,903 (1.0) | 0.264 |
| Sepsis | 197/10,815 (1.8) | 35/2,372 (1.5) | 94/5,540 (1.7) | 68/2,903 (2.3) | 0.039* |
| Septic Shock | 140/10,815 (1.3) | 23/2,372 (1.0) | 67/5,540 (1.2) | 50/2,903 (1.7) | 0.040* |
| C. diff | 162/10,815 (1.5) | 28/2,372 (1.2) | 74/5,540 (1.3) | 60/2,903 (2.1) | 0.040* |
| Unplanned Re-operation | 419/10,815 (3.9) | 70/2,372 (3.0) | 226/5,540 (4.1) | 123/2,903 (4.2) | 0.029* |
| Any Readmission | 1,011/10,815 (9.3) | 166/2,372 (7.0) | 535/5,540 (9.7) | 310/2,903 (10.7) | <0.001* |
| Length of hospital stay > 5 days | 4,598/10,727 (42.9) | 897/2,356 (38.1) | 2,300/5,507 (41.8) | 1,401/2,864 (48.9) | <0.001* |
| Mortality | 251/10,815 (2.3) | 38/2,372 (1.6) | 111/5,540 (2.0) | 102/2,902 (3.5) | <0.001* |
|
Overall N=10,815 |
Age 80-89 N=9,530 (88.1%) |
Age 90+ and older N=1,285 (11.9%) |
p-value | |
| Anastomotic leak | 247/10,815 (2.3) | 222/9,530 (2.3) | 25/1,285 (1.9) | 0.787 |
| Prolonged Nasogastric Tube | 1,554/10,815 (14.4) | 1,369/9,530 (14.4) | 185/1,285 (14.1) | 0.748 |
| Superficial Incisional SSI |
246/10,815 (2.3) | 213/9,530 (2.2) | 33/1,285 (2.6) | 0.452 |
| Deep Incisional SSI | 33/10,815 (0.3) | 29/9,530 (0.3) | 4/1,285 (0.3) | 0.966 |
| Organ/Space SSI | 304/10,815 (2.8) | 276/9,530 (2.9) | 28/1,285 (2.2) | 0.144 |
| Wound Disruption | 49/10,815 (0.5) | 44/9,530 (0.5) | 5/1,285 (0.4) | 0.716 |
| Pneumonia | 322/10,815 (3.0) | 272/9,530 (2.9) | 50/1,285 (3.9) | 0.040* |
| Unplanned Intubation | 178/10,815 (1.6) | 161/9,530 (1.7) | 17/1,285 (1.3) | 0.332 |
| Pulmonary Embolism | 87/10,815 (0.8) | 79/9,530 (0.8) | 8/1,285 (0.6) | 0.437 |
| Mechanical Ventilation for > 48 Hours | 100/10,815 (0.9) | 95/9,530 (1.0) | 5/1,285 (0.4) | 0.033* |
| Acute Renal Failure | 43/10,815 (0.4) | 41/9,530 (0.4) | 2/1,285 (0.2) | 0.142 |
| Urinary Tract Infection | 274/10,815 (2.5) | 238/9,530 (2.5) | 36/1,285 (2.8) | 0.515 |
| Stroke/CVA | 65/10,815 (0.6) | 55/9,530 (0.6) | 10/1,285 (0.8) | 0.381 |
| Cardiac Arrest Requiring CPR | 77/10,815 (0.7) | 71/9,530 (0.7) | 6/1,285 (0.5) | 0.266 |
| Myocardial Infarction | 173/10,815 (1.6) | 150/9,530 (1.6) | 23/1,285 (1.8) | 0.563 |
| Transfusions intra-op/post-op | 1,343/10,815 (12.4) | 1,155/9,530 (12.1) | 188/1,285 (14.6) | 0.010* |
| DVT Requiring Therapy | 98/10,815 (0.9) | 82/9,530 (0.9) | 16/1,285 (1.2) | 0.172 |
| Sepsis | 197/10,815 (1.8) | 175/9,530 (1.8) | 22/1,285 (1.7) | 0.755 |
| Septic Shock | 140/10,815 (1.3) | 119/9,530 (1.2) | 21/1,285 (1.6) | 0.251 |
| C. diff | 162/10,815 (1.5) | 137/9,530 (1.4) | 25/1,285 (1.9) | 0.370 |
| Unplanned Re-operation | 419/10,815 (3.9) | 379/9,530 (4.0) | 40/1,285 (3.1) | 0.132 |
| Any Readmission | 1,011/10,815 (9.3) | 899/9,530 (9.4) | 112/1,285 (8.7) | 0.407 |
| Length of hospital stay > 5 days | 4,598/10,727 (42.9) | 3,973/9,456 (42.0) | 625/1,271 (49.2) | <0.001* |
| Mortality | 251/10,815 (2.3) | 209/9,530 (2.2) | 42/1,285 (3.3) | 0.016* |
| Long length of stay (>5 days) | Readmission | |||
| aOR (95% CI) | p-value | aOR (95% CI) | p-value | |
| Age (years) | ||||
| 80-89 | Ref | --- | Ref | --- |
| 90+ | 1.41 (1.21-1.64) | <0.001* | 0.94 (0.72-1.22) | 0.627 |
| Sex | ||||
| Female | Ref | --- | Ref | --- |
| Male | 1.21 (1.09-1.34) | <0.001* | 1.08 (0.92-1.28) | 0.361 |
| Race | ||||
| Black | 0.85 (0.64-1.13) | 0.272 | 1.51 (0.97-2.34) | 0.067 |
| Other | 0.49 (0.23-1.03) | 0.058 | 1.05 (0.35-3.15) | 0.927 |
| AAPI | Ref | --- | Ref | --- |
| White | 0.84 (0.68-1.04) | 0.111 | 1.11 (0.78-1.58) | 0.561 |
| Ethnicity | ||||
| Hispanic | 0.90 (0.65-1.23) | 0.492 | 1.26 (0.80-2.00) | 0.317 |
| Non-Hispanic | Ref | --- | Ref | --- |
| BMI | ||||
| Normal weight 18.5-24.9 | Ref | --- | Ref | --- |
| Underweight <18.5 | 1.33 (1.01-1.75) | 0.045 | 1.31 (0.86-2.01) | 0.214 |
| Overweight 25.0-29.9 | 0.92 (0.81-1.03) | 0.137 | 1.07 (0.89-1.30) | 0.483 |
| Obese >29.9 | 0.99 (0.86-1.14) | 0.877 | 0.94 (0.75-1.18) | 0.604 |
| Chemotherapy within 90 days | ||||
| Yes | 1.02 (0.79-1.32) | 0.900 | 1.11 (0.75-1.65) | 0.609 |
| No | Ref | --- | Ref | --- |
| Pre-operative mechanical bowel prep | ||||
| Yes | 0.96 (0.84-1.10) | 0.573 | 1.06 (0.85-1.32) | 0.601 |
| No | Ref | --- | Ref | --- |
| Pre-operative oral antibiotic prep | ||||
| Yes | 0.58 (0.51-0.65) | <0.001* | 0.85 (0.70-1.03) | 0.096 |
| No | Ref | --- | Ref | --- |
| Clinical stage | ||||
| Stage 0 | Ref | --- | Ref | --- |
| Stage I | 0.95 (0.64-1.41) | 0.786 | 0.67 (0.37-1.19) | 0.169 |
| Stage II | 1.19 (0.80-1.76) | 0.391 | 0.88 (0.51-1.55) | 0.662 |
| Stage III | 1.21 (0.82-1.80) | 0.337 | 0.74 (0.42-1.32) | 0.308 |
| mFI | ||||
| 0 | Ref | --- | Ref | --- |
| 1 | 1.57 (1.24-1.99) | <0.001* | 1.24 (1.09-1.42) | 0.001* |
| 2 or more | 1.84 (1.42-2.39) | <0.001* | 1.75 (1.51-2.03) | <0.001* |
| Total OR time | 1.001 (1.000-1.002) | 0.024 | 1.001 (1.000-1.002) | 0.024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





