1. Introduction
The importance of functional and aesthetic hands cannot be overstated. Among traumatic hand injuries, fingertip injury with a pulp defect is very common. When left untreated, it prognosis is unsatisfactory.1 Many treatment options for fingertip defects exist, including primary closure, skin grafting, and local, distant, and free flap transfer. However, the optimal treatment for this injury remains controversial.
Reconstruction of fingertip defects requires improvements in functional outcomes and an acceptable appearance of the hand. The choice of reconstructive options can vary depending on the need to resurface the finger and size of the defect, ranging from simple skin grafting and local flaps to complex microsurgical procedures.2,3 Flap transfer to the fingertip has shown remarkable outcomes with optimal morbidity. When considering the theory of “like with like,” the transferred tissue must provide similar texture, tenacity, and thin subcutaneous fat of the pulp.4,5 Therefore, the toe pulp is strongly suggested for resurfacing the fingertip pulp defect.2,3,4
The main theme of this study was to present cases of toe pulp-free transfer for reconstructing fingertip defects in an aesthetically pleasing manner. The sensitivity, appearance, and function of the injured fingers were assessed during follow-up examinations.
2. Materials and Methods
Between January 2022 and June 2023, we performed 13 fingertip reconstructions using second toe pulp-free flaps. A chart review including demographic and medical data was conducted. Thirteen patients (eight men and five women) with an average age of 42.5 years (range, 28–66 years) were enrolled. The modes of injury included crushing, cutting, and infection. The timing of reconstruction was dependent on the wound status assessment. Some patients immediately underwent reconstructive surgery, whereas others underwent delayed surgery. Seven patients were affected on the right hand and six on the left. The number of affected finger was four for the second finger, seven for the third finger and two for the fifth finger. After removing the injured tissue, a teardrop-shaped flap was harvested from the ipsilateral second toe. The mean size of the finger pulp defects after debridement was 2.8 × 1.6 cm (range, 1.4 × 1.8 to 3.2 × 2.5 cm). The donor site was closed primarily in all patients. Post-operative evaluations were conducted to elucidate functional and aesthetic improvements (
Table 1).
2.1. Surgical Methods
Surgery was performed under general anesthesia and aided by the application of a pneumatic tourniquet. The dissection and microsurgical procedure required loupe magnification and a surgical microscope. The procedure started with adequate debridement under a finger tourniquet, and subsequently, the recipient vessels of the digital artery and volar vein were prepared. When dissecting the digital veins, the volar side of the finger was initially explored. If an appropriate vein could not be found on the volar side, it was prepared on the dorsal side. After completion of the recipient vessel and nerve preparation, the finger tourniquet was removed. Skin marking for the toe-pulp flap was continued on the second toe according to the size and shape of the fingertip defect.
Dissection of the vein was initiated by paying attention to obtaining sufficient length. This procedure should be performed under magnification to minimize venous damage. The dissection went deep into the extensor tendon layer and was elevated from the distal to the proximal direction by releasing the septa. Dissection was continued proximally, while preserving the neurovascular bundles.
After the toe-pulp flap was completely raised, the donor site was closed. The raised toe pulp tissue was transferred to the recipient site. Microanastomosis was performed in an end-to-end fashion in both arteries and veins. The size of the digital artery and volar veins was 1–1.5 and 0.6–1.2 mm, respectively. An arterial anastomosis was created between the proper digital artery of the injured finger and the plantar digital artery of the flap. Venous anastomosis was performed between the local veins around the defect of the injured finger and the dorsal metatarsal veins of the flap. The appropriate digital nerves of the flap were anastomosed to those of the injured finger. Microanastomoses of the vessels and nerves were performed using 10–0 nylon sutures. Neurorrhaphy was performed in an end-to-side manner not to injure the original recipient nerve fiber. It was as close to the flap as possible so that the nerve was regenerated quickly. Vein insufficiency frequently occurs when the remaining soft tissue in the teardrop-shaped proximal area of the flap is pressurized. The use of skin grafting rather than suturing under tension is recommended to avoid this. Postoperative flap monitoring included capillary refill, color, temperature, and turgor. Motion and exercise may be gradually started when the flap stabilizes 2 weeks after surgery.
All patients were assessed at 12 months using the Quick Disabilities of the Arm, Shoulder, and Hand (Q-DASH) scores. In addition, the static two-point discrimination (2PD) and Semmes–Weinstein monofilament tests were applied to measure the sensitivity of the recipient sites. A visual analog scale ranging from 0 to 10 was used to estimate the degree of pain in the affected finger and donor site. Assessment for subjective aesthetic appearance was also conducted.
3. Results
All flaps survived completely, with no partial necrosis. The average flap size was 1.5 × 2 cm (range, 0.8 × 1.5 to 2.0 × 3.0 cm). None of the patients showed functional impairments. No intervention or revision surgery was required during the perioperative period. The median follow-up period was 28 months, and the median duration of surgery was 119 min (range, 100–140 min). The average static two-point discrimination score for the injured finger pulp was 3.7 mm (range, 2–5 mm), the Quick Dash score was 3.4 (range, 2.3–4.2) and the Vancouver scar scale was 1.5 (range, 0–2). Problems with gait disturbances and complaints of joint stiffness at the donor site were not addressed (
Table 1).
3.1. Case Description
3.1.1. Case 1
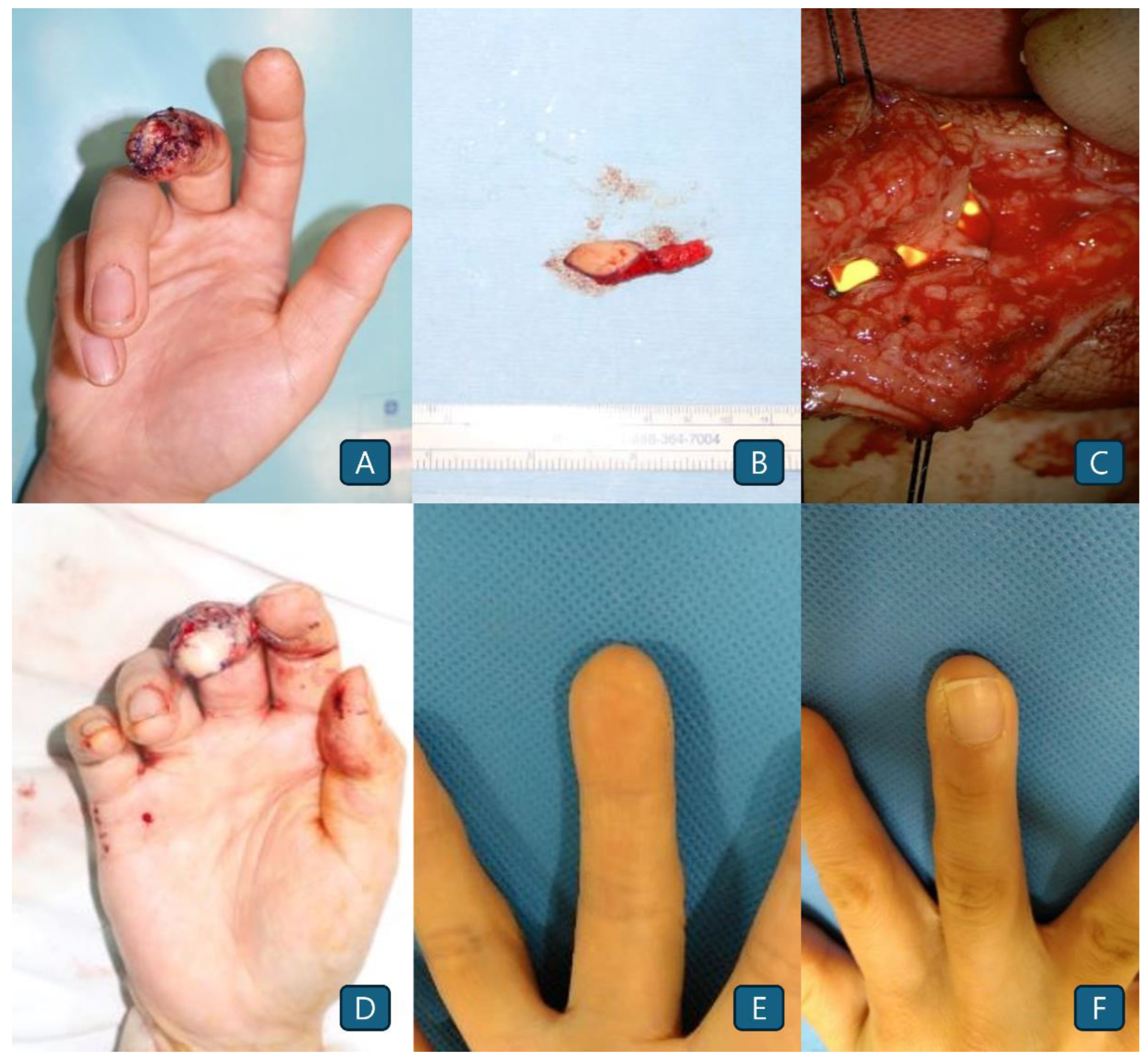
A 41-year-old female patient presented with an occupational injury to the right third finger and loss of the apical pulp (
Figure 1A). A toe pulp flap measuring approximately 1.5 × 2 cm was elevated from the ipsilateral second toe (
Figure 1B). Arterial and venous anastomoses were performed on the second toe-pulp flap pedicle in an end-to-end manner (
Figure 1C). Otherwise, the nerve anastomosis was done by end-to-side manner. The operative time was approximately 125 min. The patient recovered with no functional or cosmetic complication until the time of postoperative 60-months’ observation (
Figure 1D, 1E, and 1F).
3.1.2. Case 2
A 67-year-old female patient visited the clinic with a right third fingertip fracture and a pulp defect caused by machinery injury (
Figure 2A, 2B). The fingertip injury included a pulpal defect with a moderate-sized nail bed injury. A toe pulp flap was elevated from the second toe to the same site (
Figure 2C). Flap transfer and microanastomosis of the vessels and nerves were successfully performed (
Figure 2D). The operative time was approximately 140 min. The postoperative results showed a well-settled flap with good sensation and aesthetics (
Figure 2E and 2F).
3.1.3. Case 3
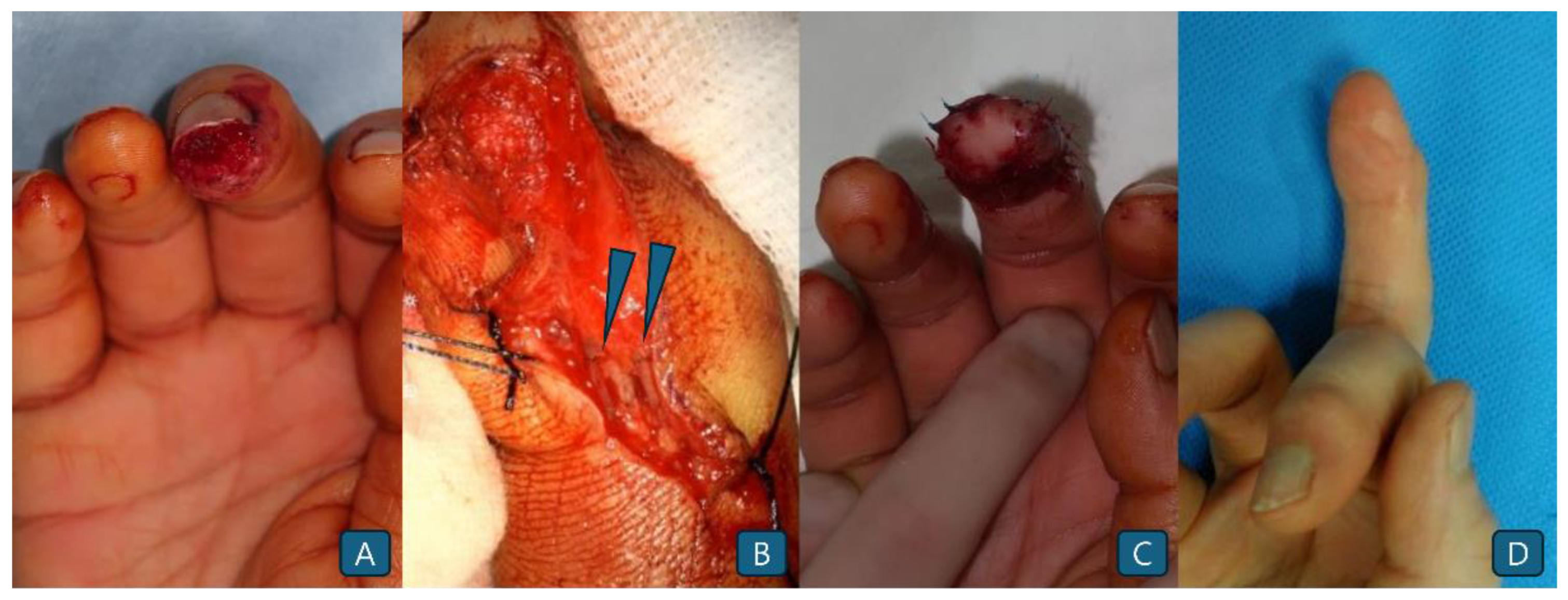
A 54-year-old man sustained an injury to right middle finger while working in an factory (
Figure 3A). The tip of the distal phalanx showed a 1.5 × 2 cm sized skin defect with no nail bed injury. Toe-pulp flap elevation and microanastomosis were successfully performed (
Figure 3B). While suturing the flap, the area of the pedicle was covered with a skin graft harvested from the hypothenar area to release tension (
Figure 3C). Functional and cosmetic outcomes were satisfactory at the postoperative 8-months’ follow-up. No limitations in finger flexion or extension were observed (
Figure 3D).
3.1.4. Case 4
A 62-year-old female patient sustained a glass injury to her left index fingertip. Loss of the skin envelope with no nail bed defects was observed on the fingertips (
Figure 4A). A 0.8 × 1.5-cm sized toe pulp flap from the ipsilateral second toe was transferred to the defect (
Figure 4B). Microanastomosis of the artery and neurorrhaphy were performed without venous anastomosis because no suitable veins were identified. The flap survived without any events, and the final outcome was satisfactory (
Figure 4C and 4D).
3.2. Figures and Table
Figure 1.
(A) The apical tip of the right third distal phalanx underwent crushing injury with no nail bed defects. (B) Toe pulp-free flap elevated from the ipsilateral second toe. (C) The digital arteries of the left second finger and volar vein were sutured with a second toe pulp flap pedicle using an end-to-end anastomosis. Nerve anastomosis was done by end-to-side manner. (D) Immediate postoperative image (E) Postoperative photograph obtained 5 years after surgery on the volar side. (F) Postoperative photograph obtained 5 years after surgery on the dorsal side.
Figure 1.
(A) The apical tip of the right third distal phalanx underwent crushing injury with no nail bed defects. (B) Toe pulp-free flap elevated from the ipsilateral second toe. (C) The digital arteries of the left second finger and volar vein were sutured with a second toe pulp flap pedicle using an end-to-end anastomosis. Nerve anastomosis was done by end-to-side manner. (D) Immediate postoperative image (E) Postoperative photograph obtained 5 years after surgery on the volar side. (F) Postoperative photograph obtained 5 years after surgery on the dorsal side.
Figure 2.
(A) The tip of the right third distal phalanx shows skin loss involving a moderately sized nail-bed defect. (B) Distal phalangeal fractures caused by same injury. (C) Elevated toe pulp flap from the second toe. (D) The pedicle is connected to the recipient’s digital artery. (E) Postoperative photograph obtained 1 year after surgery (apical view). (F) Postoperative photograph obtained 1 year after surgery (dorsal view).
Figure 2.
(A) The tip of the right third distal phalanx shows skin loss involving a moderately sized nail-bed defect. (B) Distal phalangeal fractures caused by same injury. (C) Elevated toe pulp flap from the second toe. (D) The pedicle is connected to the recipient’s digital artery. (E) Postoperative photograph obtained 1 year after surgery (apical view). (F) Postoperative photograph obtained 1 year after surgery (dorsal view).
Figure 3.
(A) The injured right third fingertip showing a skin defect invading the pulp. (B) Anastomosis between the flap pedicle and digital vessels. (Blue arrow heads) (C) Immediate postoperative photograph. (D) Postoperative photograph of the volar side 8 months after surgery.
Figure 3.
(A) The injured right third fingertip showing a skin defect invading the pulp. (B) Anastomosis between the flap pedicle and digital vessels. (Blue arrow heads) (C) Immediate postoperative photograph. (D) Postoperative photograph of the volar side 8 months after surgery.
Figure 4.
(A) Fingertip injury with apical defect. (B) A small toe pulp flap is elevated from the ipsilateral second toe. (C) Immediate postoperative photographs. (D) Postoperative photograph obtained 3 months after surgery.
Figure 4.
(A) Fingertip injury with apical defect. (B) A small toe pulp flap is elevated from the ipsilateral second toe. (C) Immediate postoperative photographs. (D) Postoperative photograph obtained 3 months after surgery.
Table 1.
Patient demographics and functional outcomes.
Table 1.
Patient demographics and functional outcomes.
| Patient No |
Sex |
Age |
Location
(Finger) |
Days after trauma |
Flap Size
(cmxcm) |
Duration of
Surgery (min) |
Anastomosis
(A; artery, V; Vein, N; Nerve) |
Skin graft
(Yes or No) |
Follow-up
(months) |
2-point D |
Q-DASH |
Vancouver
scar scale |
| 1 |
M |
58 |
Lt 3rd |
4 |
1.5x2 |
120 |
1 A, 1V, 1N |
N |
45 |
4 |
4 |
1 |
| 2 |
F |
41 |
Rt 3rd |
3 |
1.5x2 |
125 |
1 A, 1V, 1N |
N |
60 |
2 |
3 |
0 |
| 3 |
M |
46 |
Rt 5th |
6 |
2x3 |
120 |
1 A, 1V, 1N |
Y |
35 |
4 |
4.2 |
2 |
| 4 |
M |
45 |
Rt 2nd |
3 |
1.5x2 |
110 |
1 A, 1V, 1N |
N |
30 |
4 |
3.2 |
4 |
| 5 |
F |
67 |
Rt 3rd |
12 |
1.5x2 |
140 |
1 A, 1V, 1N |
N |
12 |
4 |
3 |
0 |
| 6 |
M |
45 |
Rt 3rd |
3 |
2x3 |
120 |
1 A, 1N |
Y |
25 |
5 |
4 |
2 |
| 7 |
M |
52 |
Lt 2nd |
4 |
1.5x2 |
110 |
1 A, 1V, 1N |
N |
22 |
4 |
3.4 |
1 |
| 8 |
M |
57 |
Rt 3rd |
3 |
2x3 |
120 |
1 A, 1V, 1N |
N |
14 |
4 |
4 |
2 |
| 9 |
M |
54 |
Rt 3rd |
6 |
1.5x2 |
110 |
1 A, 1V, 1N |
N |
8 |
3 |
2.4 |
0 |
| 10 |
M |
45 |
Rt 2nd |
3 |
1.5x2 |
120 |
1 A, 1V, 1N |
N |
15 |
4 |
4 |
2 |
| 11 |
F |
62 |
Lt 2nd |
2 |
0.8x1.5 |
130 |
1 A, 1N |
N |
3 |
2 |
2.3 |
1 |
| 12 |
M |
45 |
Rt 3rd |
5 |
1.5x2 |
125 |
1 A, 1V, 1N |
Y |
16 |
4 |
3 |
2 |
| 13 |
F |
35 |
Lt 5th |
3 |
1.5x2 |
100 |
1 A, 1V, 1N |
N |
24 |
4 |
4 |
2 |
4. Discussion
Reconstruction of the fingertip pulp remains challenging for surgeons because of the paucity of adjacent tissue, wherein the goal should include both restoration of function and aesthetics. The hands are one of the most important parts of the body both functionally and aesthetically. As such, addressing both of these aspects is critical in reconstruction post-injury. Several surgical methods are available today for surgeons to accomplish both acceptable functionality and favorable appearance of the hand in their patients.2,3,6
Surgical options for fingertip reconstruction vary from local flaps to free flap transfers to restore pulp and volar defects. Local flaps are ideal candidates for functionally adjacent tissues. However, the availability of local soft tissues to cover complex fingertip defects is limited.7,8 Surgeons must also consider local tissues based on the features of the fingertip wound, the patient requirements, and the surgeon’s preference for reconstructing the fingertip to minimize deformity and enhance function.9,10 Considering the primary benefit of the free flap, the donor tissue can be chosen with more freedom. However, drawbacks such as complexity of the surgical procedure, prolonged operation time, and risk of vascular crisis and failure exist. Despite these challenges, the experience in handling vessels has increased, facilitating improved outcomes with the development of microsurgery.
Diverse free tissue options exist, which are essential when considering the anatomical restoration of the fingertip with tissue similarity. In addition, the size, location, pliability, and sensation of the transferred tissue should be considered.11,12 A free thenar flap based on the superficial radial artery has the advantage of easy access during emergency surgery, a texture similar to that of the fingertip, and durable and glabrous skin. However, obtaining a sensory flap is hindered by inconsistent nerve innervation and the relative difficulty of harvesting a small area.13-15 The hypothenar flap also has the advantages of being located in the same operative field, similar to the fingertip tissue, and primary closure of the donor site, because extensive tissue in the hypothenar area can be preserved. However, these flaps exhibit anatomical variations, making it difficult to identify the perforator and cutaneous nerves in the distal ulnar area. Additionally, they are best suited for elliptical finger volar defects, not for fingertip apical defects.16,17 Considering its anatomical and textural similarities with the fingertip pulp, the toe pulp seems to be the optimal choice for defect reconstruction. The toe pulp can provide sufficient amounts of tissue with an elliptical shape, ideal for fingertip reconstruction. Furthermore, its similarity with fingertip tissue allows for “like with like” reconstruction.18,19 As a result, color and texture matching can be achieved with anatomical similarity. In terms of contour and thickness, toe pulp tissue is also excellent in terms of aesthetics and function. Moreover, reconstruction of the fingertip using a toe pulp-free flap can help restore sensation.18,19 Nerve reinnervation is so rapid that sensory recovery is promising.20 Primary closure of the donor site is also feasible since it is a partial flap that uses only half of the pulp of the second toe. This single-step procedure results in favorable sensory recovery, excellent aesthetic appearance, fingerprint restoration, and satisfactory finger function.4,19
Despite its advantages, several challenges exist in toe pulp transfer, including the risk of insufficient vessel length, vessel spasms, and tension for closure. The surgical procedure requires precise handling for exploration and preservation of the subcutaneous vein, demanding high levels of surgical experience and skill.21,22 In the present cases, when a suitable vein could not be found, an arterial anastomosis was performed. Fortunately, the flaps survived without compromise. To the best of our knowledge, this flap is relatively small, allowing for better imbibition and early marginal vessel ingrowth. Furthermore, the toe pulp is a dense tissue that is resilient to venous congestion.22 Because fingers have a very limited space inside, the anastomosed pedicle can sometimes be exposed. To address this, skin grafting on the exposed pedicle is useful under minimal tension. For this, skin can be easily accessed from the hypothenar area.4,23 Taken together, despite these challenges, the outcomes were excellent, thus highlighting the importance of performing skin grafts whenever necessary.
5. Conclusions
Fingertip injuries and defects require reconstructive procedures to restore function and aesthetics. A range of approaches exist because of the unique anatomical and tissue features of fingertips. However, toe pulp best satisfies the requirements for ideal reconstruction. Despite various potential surgical challenges, including vascular crisis and failure, patient outcomes, including motion, appearance, and sensation restoration, are reliable and satisfactory at the appropriate levels of surgical experience and skill.
Author Contributions
Conceptualization, S.J. and S.E.; methodology, S.E.; investigation, S.Y. and S.L.; resources, S.Y. and S.L.; data curation, S.Y. and S.L.; writing—original draft preparation, S.Y., S.L. and S.J.; writing—review and editing, S.E. and S.J.; supervision, S.E.; project administration, S.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Seoul National University (B-2503-960-109).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| Q-DASH |
Quick Disabilities of the Arm, Shoulder, and Hand scores |
| 2PD |
Static two-point discrimination |
References
- Yannascoli, S.M.; Thibaudeau, S.; Levin, L.S. Management of soft tissue defects of the hand. J Hand Surg. 2015, 40, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.X.; Pan, J.B.; Liu, H.J.; Zhang, N.C.; Tianm, H.; Zhang, W.Z.; Xu, T.; Feng, S.M.; Wang, J.C. Aesthetic and sensory reconstruction of finger pulp defects using free toe flaps. Aesthetic Plast Surg. 2014, 38, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.X.; Regmi, S.; Zhang, N.C.; Liu, H.J.; Zhang, W.Z.; Xu, T. Second toe microsurgical free-flap for aesthetic and sensory reconstruction of palmar soft tissue defects of fingers. J Plast Reconstr Aesthet Surg. 2015, 69, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Buncke, H.J.; Rose, E.H. Free toe-to-fingertip neurovascular flaps. Plast Reconstr Surg. 1979, 63, 607–612. [Google Scholar] [CrossRef]
- Losco, L.; Lo Torto, F.; Maruccia, M.; Di Taranto, G.; Ribuffo, D.; Cigna, E. Modified single pedicle reverse adipofascial flap for fingertip reconstruction. Microsurgery. 2019, 39, 221–227. [Google Scholar] [CrossRef]
- Hung, M.H.; Huang, K.F.; Chiu, H.Y.; Chao, W.N. Experience in reconstruction for small digital defects with free flaps. Ann Plast Surg. 2016, 76, Suppl 1:S48–54. [Google Scholar] [CrossRef]
- Sungur, N.; Kankaya, Y.; Yildiz, K.; Dolen, U.C.; Kocer, U. Bilateral V-Y rotation advancement flap for fingertip amputations. Hand (N Y). 2012, 7, 79–85. [Google Scholar] [CrossRef]
- Holm, A.; Zachariae, L. Fingertip lesions. An evaluation of conservative treatment versus free skin grafting. Acta Orthop Scand. 1974, 45, 382–392. [Google Scholar] [CrossRef]
- Koshima, I.; Urushibara, K.; Fukuda, N.; Ohkochi, M.; Nagase, T.; Gonda, K.; Asato, H.; Yoshimura, K. Digital artery perforator flaps for fingertip reconstructions. Plast Reconstr Surg. 2006, 118, 1579–1584. [Google Scholar] [CrossRef]
- Ozcanli, H.; Cavit, A. Innervated digital artery perforator flap: A versatile technique for fingertip reconstruction. J Hand Surg. 2015, 40, 2352–2357. [Google Scholar] [CrossRef]
- Miller, E.A.; Friedrich, J. Soft tissue coverage of the hand and upper extremity: The reconstructive elevator. J Hand Surg Am. 2016, 41, 782–792. [Google Scholar] [CrossRef]
- Tan, H.; Luo, X.; Yang, K.; Jiang, J.; Wei, P.; Zhao, J. Repair of minor tissue defect in hand by transfer of free tissue flap from the toe. Arch Bone Jt Surg. 2014, 2, 11–16, Kamei, K.; Ide, Y.; Kimura, T. A new free thenar flap. Plast Reconstr Surg. 1993, 92, 1380–1384. [Google Scholar] [PubMed]
- Sahu, R.K.; Kala, P.C.; Dixit, P.K.; Chakraborty, S.S.; K, S.; Katrolia, D. Finger pulp reconstruction with thenar flap: Aesthetic and functional outcome. Chin J Traumatol. 2020, 23, 307–310. [Google Scholar] [CrossRef]
- Fitoussi, F.; Ghorbani, A.; Jehanno, P.; Frajman, J.M.; Penneçot, G.F. Thenar flap for severe finger tip injuries in children. J Hand Surg Br. 2004, 29, 108–112. [Google Scholar] [CrossRef]
- Kim, K.S.; Kim, E.S.; Hwang, J.H.; Lee, S.Y. Fingertip reconstruction using the hypothenar perforator free flap. J Plast Reconstr Aesthet Surg. 2013, 66, 1263–1270. [Google Scholar] [CrossRef]
- Han, H.H.; Choi, Y.S.; Kim, I.B.; Kim, S.H.; Jun, Y.J. A perforator from the ulnar artery and cutaneous nerve of the hypothenar area: Ananatomical study for clinical application. Microsurgery. 2017, 37, 49–56. [Google Scholar] [CrossRef]
- Spyropoulou, G.A.; Shih, H.S.; Jeng, S.F. Free pulp transfer for fingertip reconstruction—The algorithm for complicated Allen fingertip defect. Plast Reconstr Surg Glob Open. 2016, 3, e584. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Fu, J.; Li, M.; Han, D.; Yang, L. Repair of hand defects by transfer of free tissue flaps from toes. Arch Orthop Trauma Surg. 2013, 133, 141–146. [Google Scholar] [CrossRef]
- Piñal, F.D.; García-Bernal, F.J.; Regalado, J.; Studer, A.; Cagigal, L.; Ayala, H. The tibial second toe vascularized neurocutaneous free flap for major digital nerve defects. J Hand Surg Am. 2007, 32, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Abele, J.; Hayakawa, T.; Buchel, E.; Brooks, D.; Buntic, R.; Safa, B.; Islur, A. Anastomosis to the common and proper digital vessels in free flap soft tissue reconstruction of the hand. Microsurgery. 2018, 38, 21–25. [Google Scholar] [CrossRef]
- Yoon, W.Y.; Lee, B.I. Fingertip reconstruction using free toe tissue transfer without venous anastomosis. Arch Plast Surg. 2012, 39, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kim, H.Y.; Rha, E.Y.; Lee, J.Y.; Han, H.H. Esthetically successful fingertip reconstruction using a second toe pulp free flap with a split thickness skin graft and tattoo. J Plast Reconstr Aesthet Surg. 2016, 69, 1574–1576. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).