1. Introduction
Ankle and subtalar joint fusions include isolated tibiotalar or talocalcaneal joint arthrodesis, tibiotalocalcaneal joint arthrodesis, or astragalectomy with tibiocalcaneal arthrodesis, which is performed when the talus is destroyed or dislocated. Even in healthy individuals, these procedures have a number of complications and risk of nonunions [
1,
2,
3]. The incidence of complications increases in patients with diabetes mellitus, Charcot arthropathy, or osteomyelitis [
4,
5]. Further increases in complications are associated with impaired vascular supply, smoking, and alcoholism [
6,
7,
8].
Surgical treatment of advanced deformities of the ankle and subtalar joint accompanied by bone destruction, osteomyelitis, or skin defect is still an unsolved medical issue. A number of factors must be considered before surgical intervention, in particular the aetiology and severity of the bone defect, the condition of the soft tissues, comorbidities and patient compliance [
9]. The goal of conservative surgery is not to preserve functional mobility of the leg, but to stabilize the vital bone and obtain a weight-bearing plantigrade leg [
10]. Reconstruction and stabilization of the ankle and subtalar improves foot stability, reduces skin calluses and defects, and improves quality of life [
11]. Therefore, some studies recommend early arthrodesis before the onset of complications [
12,
13]. On the other hand, in selected cases, amputation of the foot is a legitimate treatment method that can rid the patient of the infected lesion, is less demanding and offers a faster recovery.
2. Materials and Methods
The retrospective study included patients who underwent reconstructive surgery for ankle and subtalar joint deformity accompanied by bone destruction, infection or soft tissue defect at our department between January 2013 and December 2022.
We monitored etiology, age, gender, BMI, comorbidities, risk factors, surgery, reoperations, complications, and arthrodesis union. The union of the arthrodesis was monitored by radiographs, and a CT scan was performed when arthrodesis union was in doubt.
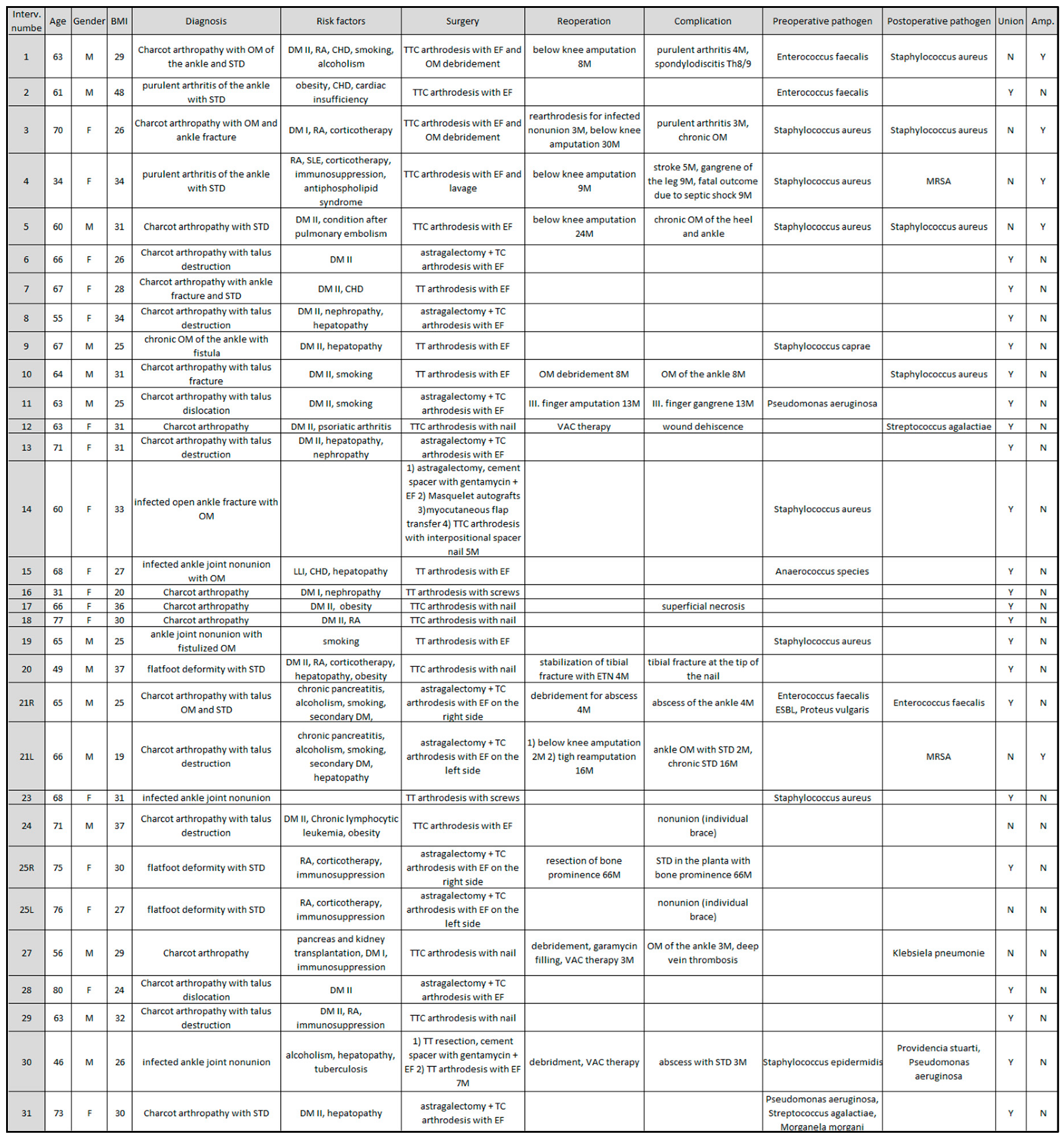
The cohort included 29 patients, 16 women and 13 men, 2 patients were operated bilaterally, so 31 interventions were followed (
Table 1).
The etiology of the deformity was Charcot arthropathy in 17 procedures (55%), osteomyelitis in 8 procedures (25%), combination of Charcot arthropathy and osteomyelitis in 3 procedures (10%) and rheumatic foot deformity with skin defect in 3 procedures (10%). The most common comorbidities were diabetes mellitus in 22 patients (71%), hepatopathy in 9 patients (29%), rheumatoid arthritis in 8 patients (26%), and ischemic heart disease in 4 patients (13%). The most common risk factors were active smoking in 6 patients (19%), corticosteroid treatment in 5 patients (16%), immunosuppression in 5 patients (16%) and active alcohol abuse in 4 patients (13%). The mean BMI was 29.6, ranging from 19 to 48.
Before or during surgery, infectious agents were cultured in 14 cases (45%). Staphylococcus aureus was the most common pathogen (6 cases), followed by Enterococcus faecalis and Pseudomonas aeruginosa (2 cases). Postoperatively, the infectious agents were cultured in 10 cases (32%). The most common postoperative pathogens was Staphylococcus aureus (4 cases) and methicillin-resistant Staphylococcus aureus (2 cases).
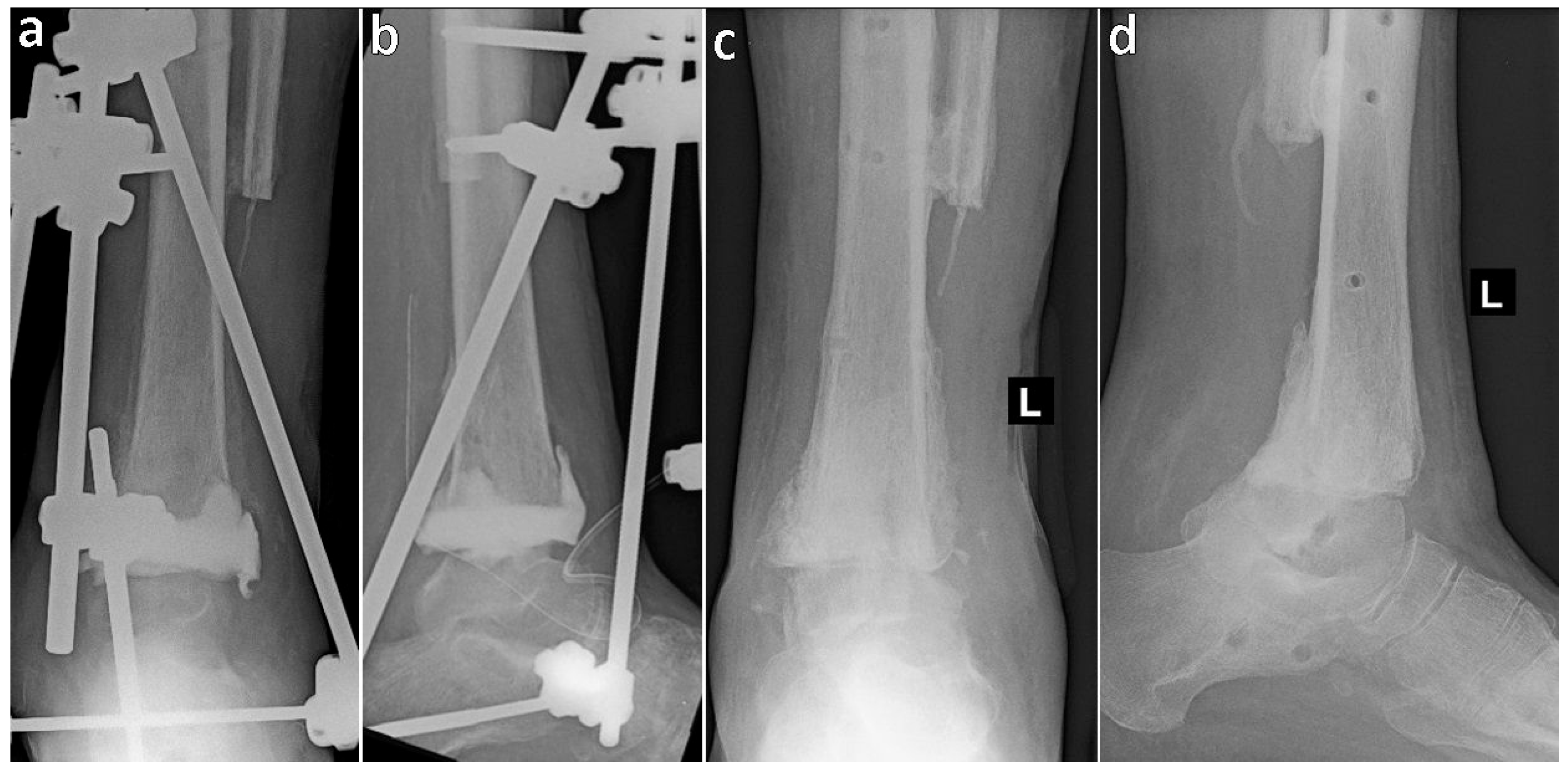
The level of arthrodesis was chosen based on the location of bone destruction, the location of osteomyelitis, and the condition of the soft tissues. The most common procedure was tibiotalocalcaneal arthrodesis in 12 operated legs (39%), of which 6 procedures used an external fixator for stabilization and 6 procedures used an intramedullary nail, astragalectomy with tibiocalcaneal arthrodesis using an external fixator was performed in 10 operated legs (32%) and tibiotalar arthrodesis was performed in 7 operated legs (23%). In 2 cases, a multistage procedure was preferred. The first multistage procedure was a patient with osteomyelitis of the ankle joint. In the first stage, resection of the articular parts of the tibia and talus was performed with implantation of a cement spacer with antibiotics and stabilization with an external fixator. After 7 months, the cement spacer was replaced with an autograft spongioplasty (
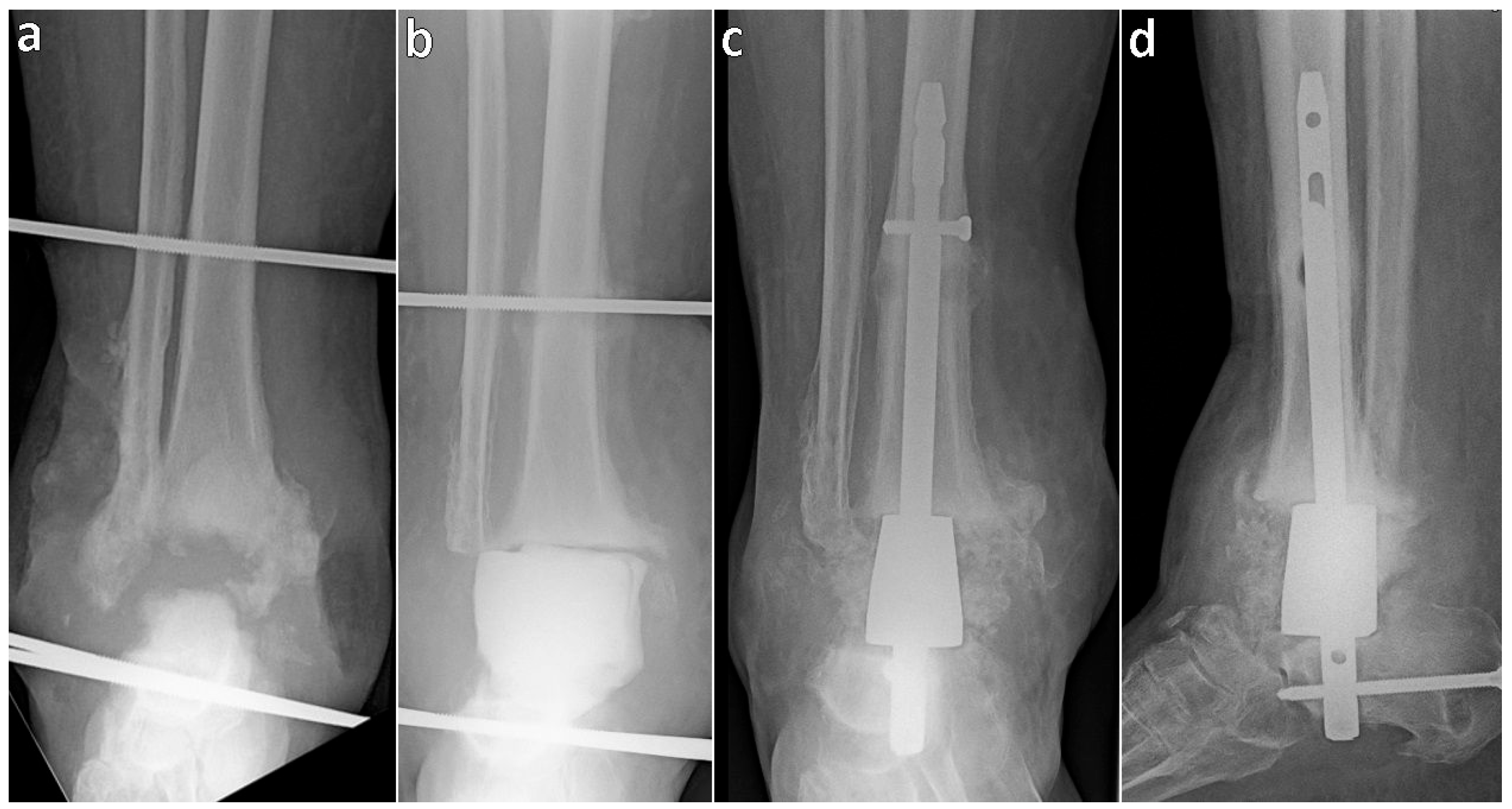
Figure 1). The second multistage procedure was performed on a patient with an infected nonunion of the ankle. Initially, resection of the destroyed talus and articular portion of the tibia was performed, and the defect was filled with a cement spacer with antibiotics and bridged using an external fixator. 2 months later the cement spacer was replaced with autologous bone grafts according to the Masquelet technique. This was followed by covering the soft tissue defect with a rotational flap. Five months after the first operation, tibiocalcaneal arthrodesis with a trabecular metal spacer nail was performed (
Figure 2).
Statistical Evaluation
Fisher’s exact test in contingency table was used for statistical evaluation. We tested arthrodesis union rate in relation to the etiology and arthrodesis union rate in relation to the level and type of fusion.
3. Results
Arthrodesis fusion occurred in 23 of 31 interventions (74%). In relation to the etiology (
Table 2), the arthrodesis healed in 13 of 17 interventions (76%) in patients with Charcot arthropathy, in 7 of 8 interventions (88%) in patients with osteomyelitis or septic arthritis, in 1 of 3 interventions (33%) in patients with a combination of Charcot arthropathy and osteomyelitis, and in 2 of 3 interventions (66%) in patients with rheumatic foot deformity and skin defect. The hypothesis of the independence of fusion healing on the etiology of the disease was not rejected in the statistical evaluation (p=0.377). The statistical evaluation did not find an effect of the etiology on the union rate.
In relation to the level and type of fusion (
Table 3), tibiotalocalcaneal arthrodesis stabilized with an external fixator healed in 1 of 6 interventions (17%), tibiotalocalcaneal arthrodesis stabilized with a nail in 5 of 6 interventions (83%), tibiocalcaneal arthrodesis stabilized with an external fixator in 8 of 10 interventions (80%), tibiotalar arthrodesis healed in all 7 interventions and both multi-stage operations also healed. The hypothesis that the union rate of arthrodesis was independent of the level and type of fusion was rejected on statistical evaluation (p=0.0199). The dependence was due to the higher number of nonunions in cases of tibiotalocalcaneal fusions using an external fixator.
The arthrodesis failed to heal in 8 interventions (26%), of which in 3 interventions the nonunion was stable and the patients were able to load the limb with an ankle-foot brace. In 5 patients the limb had to be amputated (16%). In the first case, the limb was amputated below the knee 8 months after the primary operation due to progression of osteomyelitis of the feet. In the second case, the infected nonunion in the subtalar joint did not heal and the limb was amputated below the knee 30 months after the primary operation. In the third case, a patient with Charcot’s arthropathy with soft tissue defect developed osteomyelitis of the calcaneus and 24 months after the primary surgery, the limb was amputated below the knee. In the fourth case of a patient with an overlap syndrome of rheumatoid arthritis and systemic lupus erythematosus with corticotherapy, immunosuppression and ankle arthritis, gangrene of the foot occurred. Despite below knee amputation 9 months after primary surgery, the patient died of generalized sepsis. In the fifth case, the patient was an alcoholic, smoker, with chronic pancreatitis, liver cirrhosis and diabetes, with bilateral Charcot arthropathy. He developed osteomyelitis of the ankle with skin defects on the left side. A below knee amputation performed 2 months after the primary surgery failed to heal, and a reamputation in the thigh was performed 16 months after the primary surgery.
Complicated healing of surgical wounds, phlegmon or abscess occurred in 13 interventions (42%). This was influenced by a high frequency of infection before primary surgery. In 3 cases the defect was successfully healed with Vacuum Assisted Closure (VAC) therapy, but in 10 other cases reoperation was necessary. In one intervention, an occult tibial fracture occurred during tibiotalocalcaneal nail insertion. After attempting conservative treatment, the fracture was stabilized with an intramedullary nail. In total, reoperation was necessary in 11 interventions (35%). The mean time from primary surgery to extraction of the external fixator was 117 days, ranging from 87 to 363 days.
4. Discussion
Recently, there have been only a few studies focusing on ankle and subtalar arthrodesis as an alternative to amputation in high-risk patients. One study presented nonunion of arthrodesis in 8 cases and inflammatory complications in 4 of 18 patients [
14]. In another study, arthrodesis nonunion was reported in 38% of patients with diabetes and 27% without diabetes [
15]. The literature also reports a high rate of reoperations in cases where the patient met at least two of the risk criteria including immunosuppression, diabetes and obesity [
3,
16]. In our cohort, we observed infectious complications in 42% and arthrodesis nonunion in 26% of interventions. In 5 patients, the limb had to be amputated. Since these are interventions with a high risk of complications, it is necessary to consider a number of factors such as etiology, infectious focus and comorbidity in preoperative planning [
17]. The patient must be able to follow the recommended regimen, keep the surgical wound and external fixator sterile. Compliance can be very demanding for patients with neuropathy. Although amputation offers the prospect of a quick solution, it greatly affects the patient’s self-sufficiency. The ability to maintain balance is already limited due to polyneuropathy and in some cases amputation leads to the loss of the ability to walk independently. Therefore, the patient should be informed that the surgical procedure is fraught with numerous complications, including the risk of limb amputation [
11].
Charcot arthropathy of the foot leads to progressive instability, which leads to foot deformity, skeletal protrusion, soft tissue defects, and osteomyelitis [
18]. The goal of treatment is to reduce inflammation and maintain the foot in a physiological plantigrade position. In the initial inflammatory phase, the patient is monitored, including repeated X-ray examinations, and the affected foot is protected from weight-bearing. Surgical treatment is carried out after the end of the inflammatory phase in cases where the foot is not in a plantigrade position.
If the etiology of deformity is osteomyelitis, the goal is to control the infection and achieve a plantigrade position of the leg [
19]. Initially, broad-spectrum intravenous antibiotics are administered, the abscess is drained, and the necrotic bone is removed. After isolation of the infectious agent, targeted antibiotics are administered. Definitive treatment is performed when the infection is stabilized.
In our cohort, tibiotalar arthrodesis was indicated for isolated tibiotalar joint damage. Tibiotalocalcaneal arthrodesis was chosen when both the tibiotalar and talocalcaneal joints were affected. In severe osteoporosis, tibiotalocalcaneal arthrodesis with an intramedullary nail was also selected in cases of isolated tibiotalar joint destruction, thus favouring better mechanical stability over preserving mobility of the unaffected talocalcaneal joint. Astragalectomy with tibiocalcaneal arthrodesis was chosen in cases of talus destruction or dislocation [
20,
21,
22]. Astragalectomy can correct severe leg deformities, but resection of the talus leads to shortening of the limb [
23]. In one relatively healthy patient in our cohort, the talus was replaced with a nail with a trabecular metal spacer and and the limb length was preserved.
In 21 interventions, an external fixator was used to stabilize the arthrodesis. The advantage is that an external fixator inserted into the vital bone can achieve reduction, mechanical stability, and compression at the level of the infected or altered bone [
24,
25,
26]. Skin defects can be dressed more easily and VAC therapy can be applied [
27,
28]. The disadvantage is the need for local care of the external fixator and the frequent occurrence of pin track infections [
18,
29]. However, in the group of tibiotalocalcaneal arthrodeses stabilized with an external fixator, we observed the lowest fusion rate, namely in 1 out of 6 procedures. Focusing on this group, the indications for surgery were Charcot arthropathy, septic arthritis, a combination of both and soft tissue coverage was defective. The combination of soft tissue coverage defect with bone destruction may represent a borderline indication for reconstructive surgery. In our cohort, the mean time to removal of the external fixator was 117 days (16.7 weeks), and after removal, the ankle was further fixed with a custom-made plastic brace for 6 to 12 weeks. In other studies, the time to removal of the external fixator ranged from 18 to 27.7 weeks [
2,
14,
30], but there was no further fixation with a brace.
5. Conclusions
Reconstructive surgery for advanced deformities of the ankle and subtalar joint due to Charcot arthropathy, osteomyelitis, or rheumatoid arthritis is associated with many complications. The goal of treatment is to eliminate the infection and to achieve a limb capable of bearing weight in the plantigrade position. Although amputation offers the prospect of a quick solution, in neuropathic patients it can lead to the loss of the ability to walk independently. In our high-risk patient cohort, we preferred reconstructive surgery over amputation and in 26 of 31 interventions, the limb was preserved and weight-bearing capacity was restored.
Funding
This work was supported by the Cooperatio Program (research area SURG) and MHCZ-DRO (UHHK, no. 00179906).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
interv. (intervention), amp. (amputation), STD (soft tissue defect), M (male), F (female), N (no), Y (yes), R (right), L (left), M (months since surgery), TTC (tibiotalocalcaneal), TT (tibiotalar), TC (tibiocalcaneal), EF (external fixator), OM (osteomyelitis), DM (diabetes mellitus), RA (rheumatoid arthritis), CHD (coronary heart disease), SLE (systemic lupus erythematosus), VAC (Vaccum Assisted Closure), LLI (lower limb ischemia), ETN (Expert Tibial Nail), MRSA (methicillin-resistant Staphylococcus aureus), ESBL (extended-spectrum b-lactamases)
References
- Johnson EE, Weltmer J, Lian GJ, Cracchiolo A 3rd. Ilizarov ankle arthrodesis. Clin Orthop Relat Res. 1992 Jul;(280):160-9.
- Salem KH, Kinzl L, Schmelz A. Ankle arthrodesis using Ilizarov ring fixators: a review of 22 cases. Foot Ankle Int. 2006 Oct;27(10):764-70. [CrossRef]
- Rabinovich RV, Haleem AM, Rozbruch SR. Complex ankle arthrodesis: Review of the literature. World J Orthop. 2015 Sep 18;6(8):602-13. [CrossRef]
- Thevendran G, Younger A, Pinney S. Current concepts review: risk factors for nonunions in foot and ankle arthrodeses. Foot Ankle Int. 2012 Nov;33(11):1031-40. [CrossRef]
- Ahmad J, Raikin SM. Ankle arthrodesis: the simple and the complex. Foot Ankle Clin. 2008 Sep;13(3):381-400. [CrossRef]
- Rogers LC, Bevilacqua NJ, Frykberg RG, Armstrong DG. Predictors of postoperative complications of Ilizarov external ring fixators in the foot and ankle. J Foot Ankle Surg. 2007 Sep-Oct;46(5):372-5. [CrossRef]
- Wukich DK, Belczyk RJ, Burns PR, Frykberg RG. Complications encountered with circular ring fixation in persons with diabetes mellitus. Foot Ankle Int. 2008 Oct;29(10):994-1000. [CrossRef]
- Cobb TK, Gabrielsen TA, Campbell DC 2nd, Wallrichs SL, Ilstrup DM (1994) Cigarette smoking and nonunion after ankle arthrodesis. Foot Ankle Int 15(2):64–67. [CrossRef]
- 9 Schneekloth BJ, Lowery NJ, Wukich DK. Charcot Neuroarthropathy in Patients With Diabetes: An Updated Systematic Review of Surgical Management. J Foot Ankle Surg. 2016 May-Jun;55(3):586-90. [CrossRef]
- Morris HD, Hand WL, Dunn AW. The modified Blair fusion for fractures of the talus. J Bone Joint Surg Am. 1971 Oct;53(7):1289-97. [CrossRef] [PubMed]
- Adigweme U, Oki JA, Johnson K, Baddaloo T, Cala M, Merrill T. Tibiocalcaneal Arthrodesis as a Limb Salvage Solution for a Patient With Rearfoot Charcot Neuroarthropathy and Avascular Necrosis of the Talus. www.podiatryinstitute.com.
- Caravaggi C, Cimmino M, Caruso S, Dalla Noce S. Intramedullary compressive nail fixation for the treatment of severe Charcot deformity of the ankle and rear foot. J Foot Ankle Surg. 2006 Jan-Feb;45(1):20-4. [CrossRef]
- Frey C, Halikus NM, Vu-Rose T, Ebramzadeh E. A review of ankle arthrodesis: predisposing factors to nonunion. Foot Ankle Int. 1994 Nov;15(11):581-4. [CrossRef]
- Love B, Alexander B, Ray J, Halstrom J, Barranco H, Solar S, Singh M, Shah A. Outcomes of Tibiocalcaneal Arthrodesis in High-Risk Patients: An Institutional Cohort of 18 Patients. Indian J Orthop. 2020 Feb 4;54(1):14-21. [CrossRef]
- Perlman MH, Thordarson DB. Ankle fusion in a high risk population: an assessment of nonunion risk factors. Foot Ankle Int. 1999 Aug;20(8):491-6. [CrossRef]
- Saxena A, DiDomenico LA, Widtfeldt A, Adams T, Kim W. Implantable electrical bone stimulation for arthrodeses of the foot and ankle in high-risk patients: a multicenter study. J Foot Ankle Surg. 2005;44:450–454. [CrossRef]
- Lee DJ, Schaffer J, Chen T, Oh I. Internal Versus External Fixation of Charcot Midfoot Deformity Realignment. Orthopedics. 2016 Jul 1;39(4):e595-601. [CrossRef]
- Aikawa T, Watanabe K, Matsubara H, Nomura I, Tsuchiya H. Tibiocalcaneal Fusion for Charcot Ankle With Severe Talar Body Loss: Case Report and a Review of the Surgical Literature. J Foot Ankle Surg. 2016 Mar-Apr;55(2):247-51. [CrossRef]
- Cibura C, Lotzien S, Yilmaz E, Baecker H, Schildhauer TA, Gessmann J. Simultaneous septic arthrodesis of the tibiotalar and subtalar joints with the Ilizarov external fixator-an analysis of 13 patients. Eur J Orthop Surg Traumatol. 2022 Aug;32(6):1063-1070. [CrossRef]
- Reinke C, Lotzien S, Yilmaz E, Hanusrichter Y, Ull C, Baecker H, Schildhauer TA, Geßmann J. Tibiocalcaneal arthrodesis using the Ilizarov fixator in compromised hosts: an analysis of 19 patients. Arch Orthop Trauma Surg. 2022 Jul;142(7):1359-1366. [CrossRef]
- Ettinger S, Stukenborg-Colsman C, Plaass C, Yao D, Claassen L, Berger S, Waizy H, Becher CM, Daniijidis K. Tibiocalcaneal arthrodesis as a limb salvage procedure for complex hindfoot deformities. Arch Orthop Trauma Surg. 2016;136:457–462. [CrossRef]
- LaPorta GA, Nasser EM, Mulhern JL. Tibiocalcaneal arthrodesis in the high-risk foot. J Foot Ankle Surg. 2014 Nov-Dec;53(6):774-86. [CrossRef]
- Kolker D, Wilson MG. Tibiocalcaneal Arthrodesis After Total Talectomy for Treatment of Osteomyelits of the Talus. Foot & Ankle International. 2004;25(12):861-865. [CrossRef]
- Yanuka M, Krasin E, Goldwirth M, Cohen Z, Otremski I. Ankle arthrodesis using the Ilizarov apparatus: good results in 6 patients. Acta Orthop Scand. 2000 Jun;71(3):297-300. [CrossRef]
- Rochman R, Jackson Hutson J, Alade O. Tibiocalcaneal arthrodesis using the Ilizarov technique in the presence of bone loss and infection of the talus. Foot Ankle Int. 2008 Oct;29(10):1001-8. [CrossRef]
- Wang S, Li B, Yu X, Wu H, Liu L (2023) Is ankle arthrodesis with an Ilizarov External Fixator an effective treatment for septic ankle arthritis? A study with a Minimum of 6 years of follow-up. Clin Orthop Relat Res 481(4):717–725. [CrossRef]
- Katsenis D, Bhave A, Paley D, Herzenberg JE (2005) Treatment of malunion and nonunion at the site of an ankle fusion with the Ilizarov apparatus. J Bone Joint Surg Am 87(2):302–309. [CrossRef]
- Brinkemper A, Lülsdorff RH, Lotzien S, Kruppa C, Schildhauer TA, Cibura C. Ilizarov fixator as salvage procedure after frustrating arthrodesis using intramedullary nailing - is there a chance of consolidation? Arch Orthop Trauma Surg. 2024 Nov;144(11):5031-5038. [CrossRef]
- Yammine K, Assi C. Intramedullary nail versus external fixator for ankle arthrodesis in Charcot neuroarthropathy: A meta-analysis of comparative studies. J Orthop Surg (Hong Kong). 2019 May-Aug;27(2):2309499019836012. [CrossRef]
- Fragomen AT, Borst E, Schachter L, Lyman S, Rozbruch SR. Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion. Clin Orthop Relat Res. 2012 Oct;470(10):2864-73. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).