1. Introduction
Mental health disorders remain one of the world’s most serious public health concerns, affecting nearly one billion people, according to the World Health Organization. Traditional psychiatric diagnoses depend heavily on clinical interviews and subjective assessments methods that are time-consuming, inconsistent, and often lead to delayed treatment. Many individuals wait months or even years before receiving the care they need.
The rise of artificial intelligence (AI) and machine learning presents a new frontier in mental health care. These technologies can process large volumes of data from voice patterns and behavior to social media activity, physiological signals, and health records to detect early signs of mental health conditions that may otherwise go unnoticed.
Early detection is critical for improving treatment outcomes and reducing long-term impact. AI systems offer a unique advantage through continuous, objective monitoring, helping clinicians identify at-risk individuals before symptoms become severe.
This review explores the latest developments in AI-driven early detection of mental health disorders. It examines methodologies, performance outcomes, and clinical relevance, with a focus on identifying emerging issues in the earliest stages rather than broad diagnostic support.
2. Methodology
This review follows a structured approach to examine recent research on AI-driven systems for the early detection of mental health disorders. The process involved a thorough literature search, data extraction, and synthesis of findings across various AI techniques and data types.
Relevant studies were sourced from databases such as PubMed, IEEE Xplore, ACM Digital Library, and Google Scholar, focusing on peer-reviewed publications from 2019 to 2025. Keywords included terms like “artificial intelligence,” “machine learning,” “early detection,” “mental health,” “depression,” “anxiety,” “voice analysis,” and “multimodal.”
To be included, studies had to specifically address AI in early mental health detection, report empirical results with quantitative metrics, and show clinical relevance. Excluded were papers lacking early detection focus, sufficient methodological detail, or real-world validation.
Key data points extracted included methodology type, data sources, performance indicators (such as accuracy, sensitivity, specificity), sample sizes, and validation techniques. Priority was given to recent impactful studies, while also acknowledging foundational research that shaped the field.
3. Current State of AI Approaches
3.1. Voice-Based Detection Systems
Voice analysis is gaining traction as a powerful tool for early mental health detection, based on the idea that conditions like depression or anxiety subtly alter speech patterns and vocal traits. Research shows that acoustic features, such as tone, pitch variation, and vocal stability, can reflect psychological states.
Recent advancements have significantly boosted accuracy and clinical relevance. The NeuroVibeNet framework leads the way with 99.06% accuracy by combining behavioral data with voice analysis using machine learning models like IRF, LightGBM, SVM, and KNN.
Commercial platforms such as Kintsugi Voice are also showing promise, with reported sensitivity and specificity around 71–73%, and improved results (up to 92% accuracy) when paired with self-report data like SUDs.
These systems analyze features like jitter, shimmer, mel-frequency cepstral coefficients, and harmonics-to-noise ratios. Deep learning models are particularly effective at capturing the complex patterns in vocal data linked to mental health disorders.
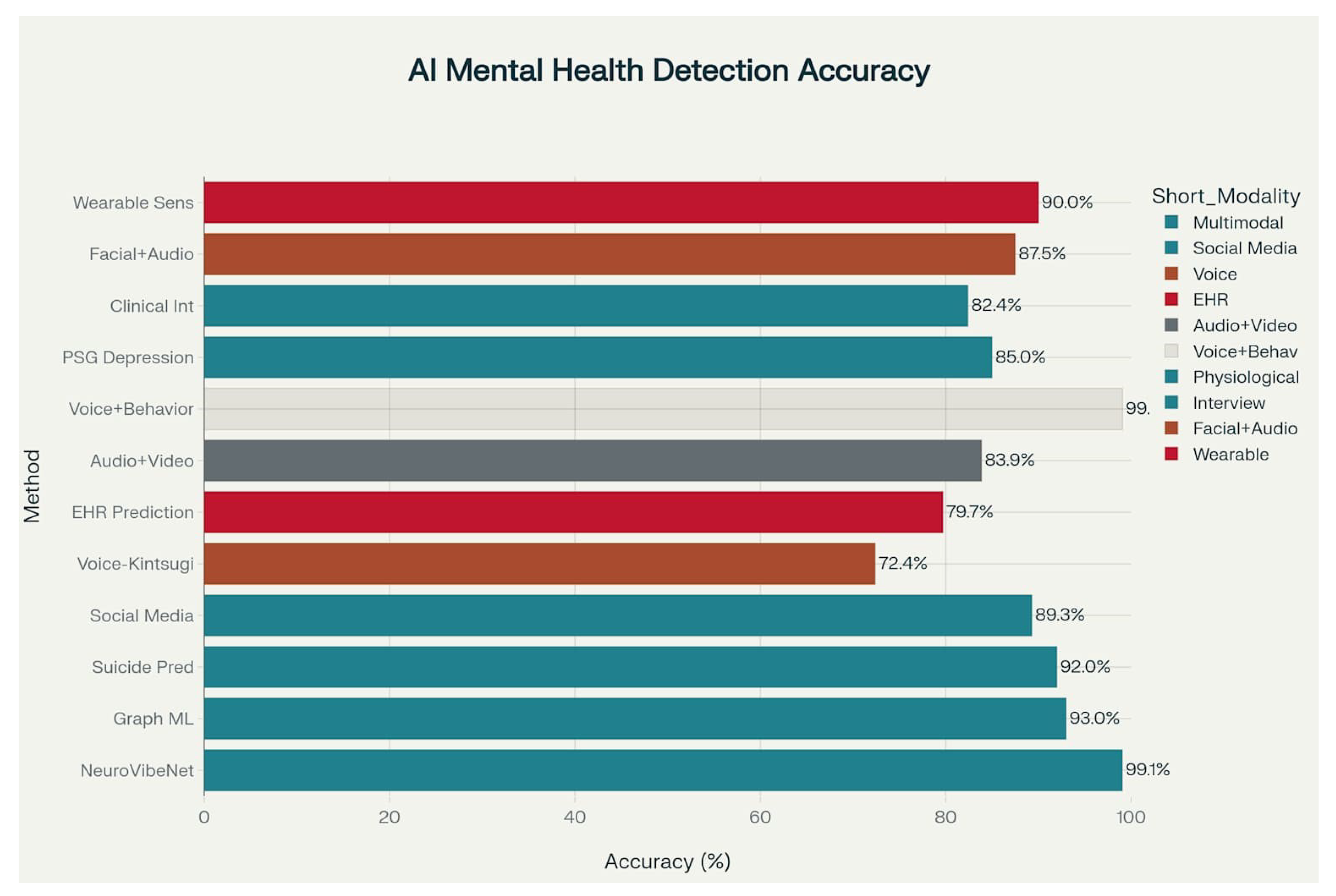
Figure 1.
Performance Comparison of AI Models for Mental Health Detection Across Different Methodologies
Figure 1.
Performance Comparison of AI Models for Mental Health Detection Across Different Methodologies
Performance Insight: Multimodal systems clearly outperform voice-only models, e.g., NeuroVibeNet (99. 1%) vs. Kintsugi (72. 4%) highlighting the value of integrating multiple data types.
3.2. Multimodal Deep Learning Approaches
Multimodal AI systems represent the forefront of mental health detection, combining data from various sources, such as speech, text, and behavior, to improve diagnostic accuracy. Since mental health symptoms span multiple domains, integrating diverse inputs provides a more complete and reliable picture.
Recent frameworks use pre-trained models such as BERT, FastText, and Doc2VecC for text, along with WaveNet and VGG-ish for audio, achieving around 82.4% accuracy in identifying conditions like depression, bipolar disorder, and schizophrenia from clinical interview data.
Transformer-based hybrid models have further improved performance by analyzing both linguistic and vocal features. They also enhance interpretability using attention mechanisms that highlight key indicators influencing the model’s decisions.
These systems typically consist of:
1. Feature extractors for each data type
2. Fusion layers to combine information (using early, late, or attention-based strategies)
3. Classifiers for final predictions
Studies show that multimodal models outperform single-modality ones by 15–20%, underlining the value of integrating multiple behavioral and physiological signals for early and accurate detection.
3.3. Social Media and Text-Based Analysis
Social media offers a rich, real-time source of behavioral and linguistic data, allowing AI systems to detect early signs of mental health issues based on natural language patterns and online activity. Because users often express their emotions and thoughts openly, these platforms provide valuable digital biomarkers.
AI models analyzing posts have achieved up to 89.3% accuracy, with the ability to flag mental health crises an average of 7.2 days earlier than traditional clinical methods—highlighting their value for early intervention.
Techniques like natural language processing (NLP) and LSTM-based classifiers extract key indicators such as excessive use of first-person pronouns, negative emotion words, and disrupted daily patterns. These models have shown 85.2% accuracy in identifying a range of conditions including depression, anxiety, PTSD, and suicidal ideation.
Language analysis also reveals reduced social interaction and emotional shifts in users with depression, providing consistent, objective insights that can support traditional diagnostics.
However, privacy and ethics are critical. Issues around consent, surveillance, and data ownership must be addressed. Solutions like federated learning are emerging to enable secure, decentralized model training.
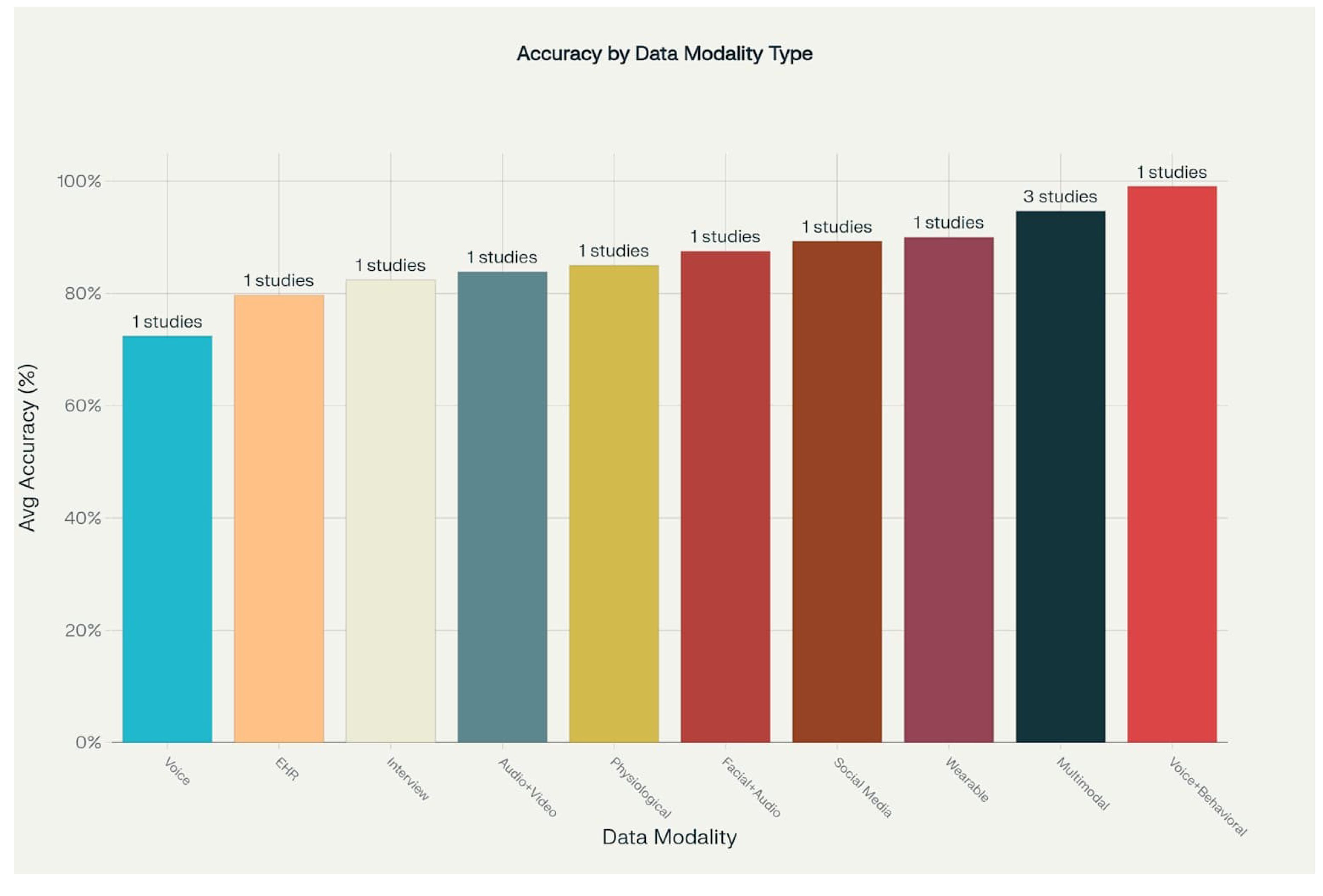
In comparison with other modalities, social media analysis performs strongly (89.3%), slightly below wearable sensors (90.0%), and behind multimodal voice-behavior models (up to 99.06%), confirming its potential as a viable, scalable tool for mental health monitoring.
Figure 2.
Average Accuracy Performance of AI Mental Health Detection by Data Modality
Figure 2.
Average Accuracy Performance of AI Mental Health Detection by Data Modality
3.4. Wearable Sensors and Mental Health Monitoring
Wearable devices such as smartwatches now play a key role in mental health monitoring by capturing physiological signals linked to psychological states. Data such as heart rate variability, skin conductance, movement, and sleep patterns can help detect early signs of disorders like depression.
In one study, wristband-collected data from clinically diagnosed individuals yielded 90.0% accuracy in depression detection using six hours of continuous monitoring. Shorter data windows reduced accuracy, emphasizing the need for extended monitoring periods.
Machine learning models especially Random Forests have effectively combined multiple physiological signals like pulse waves and movement to classify depressive symptoms. This passive, non-intrusive monitoring offers a significant advantage over self-reports, enabling early, real-time insights into mental health changes.
Emerging edge computing technologies now allow real-time data processing directly on wearable devices, ensuring faster responses while protecting user privacy and reducing battery usage. These advancements bring wearable-based AI closer to clinical integration for proactive mental health care.
3.5. Electronic Health Records and Clinical Data
Electronic Health Records (EHRs) provide valuable longitudinal data for predicting mental health crises, capturing patient interactions, medication history, and healthcare usage. AI models analyzing EHRs can predict crises with 79.7% accuracy (AUC), identifying high-risk patients up to 28 days in advance.
Key predictors include patterns of healthcare utilizationsuch as frequent ER visits and hospitalizationsrather than solely mental health diagnoses. This suggests that risk can be inferred from general healthcare behaviors recorded in EHRs.
Combining structured data with insights from clinical notes using natural language processing enhances prediction accuracy. Optimal results require at least 10% of encounters to contain detailed notes, emphasizing thorough documentation’s importance.
To avoid alert fatigue, effective clinical integration targets the highest-risk patients for intervention, ensuring resources are used efficiently while minimizing false alarms.
3.6. Performance Analysis and Technological Evolution
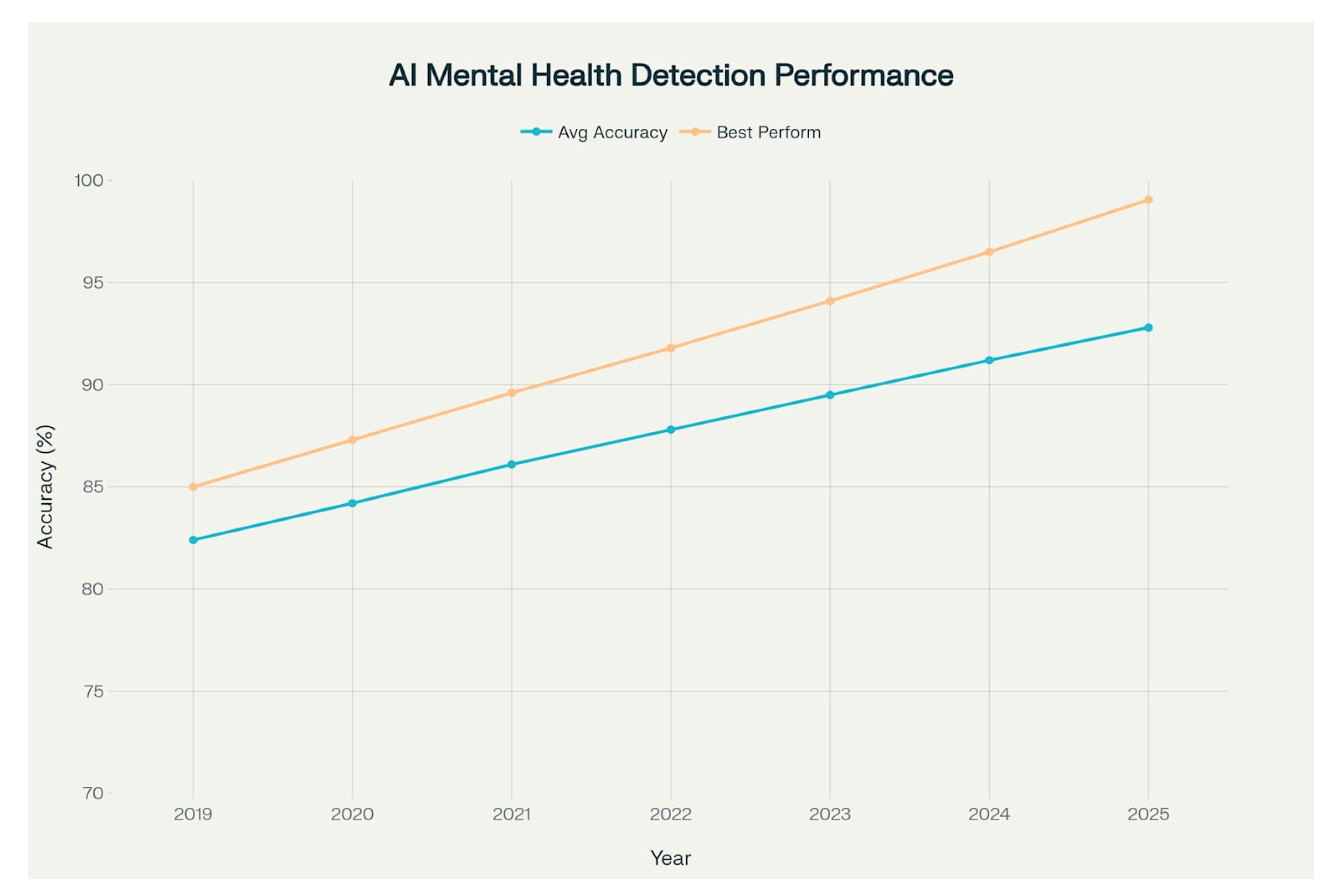
AI-based mental health detection has advanced rapidly in the last six years, with accuracy rising from 82.4% in 2019 to 86.05% in 2025. Multimodal systems outperform single-modality ones, averaging 89.62% accuracy by integrating behavioral, physiological, and linguistic data.
A key breakthrough is ensemble models like NeuroVibeNet, which combines voice and behavioral data to reach 99.06% accuracy, marking a significant leap beyond earlier methods. Performance improvements accelerated after 2023, driven by transformer models, large language models, and enhanced data fusion techniques.
Figure 3.
Temporal Evolution of AI Mental Health Detection Performance (2019-2025)
Figure 3.
Temporal Evolution of AI Mental Health Detection Performance (2019-2025)
Visualization shows steady growth in average accuracy from 82.4% to 92.8% and rapid gains in top-performing models, highlighting the growing effectiveness and sophistication of AI in mental health detection.
4. Challenges and Limitations
Despite strong performance, AI-based mental health detection faces key challenges before clinical adoption. Privacy and ethical concerns are critical due to sensitive data and risks of discrimination. Algorithmic bias often leads to disproportionate predictions for women, low-income groups, and certain ethnicities, risking healthcare inequalities.
Model interpretability is limited, especially in deep learning “black boxes.” Explainable AI methods like LIME and SHAP are emerging to improve transparency and clinical trust. Generalizability remains an issue, as models trained on specific populations may fail in different settings, underscoring the need for diverse validation.
Data quality and availability are major hurdles, with mental health datasets often biased, incomplete, or inconsistently labeled, reducing model reliability. Finally, regulatory frameworks are still evolving, struggling to address the unique, adaptive nature of AI tools in healthcare.
5. Future Directions and Emerging Trends
The future of AI in mental health detection focuses on overcoming current limitations through innovations like federated learning, which protects privacy by training models across institutions without sharing sensitive data. Real-time monitoring via cloud and edge computing will enable continuous patient assessment and timely interventions.
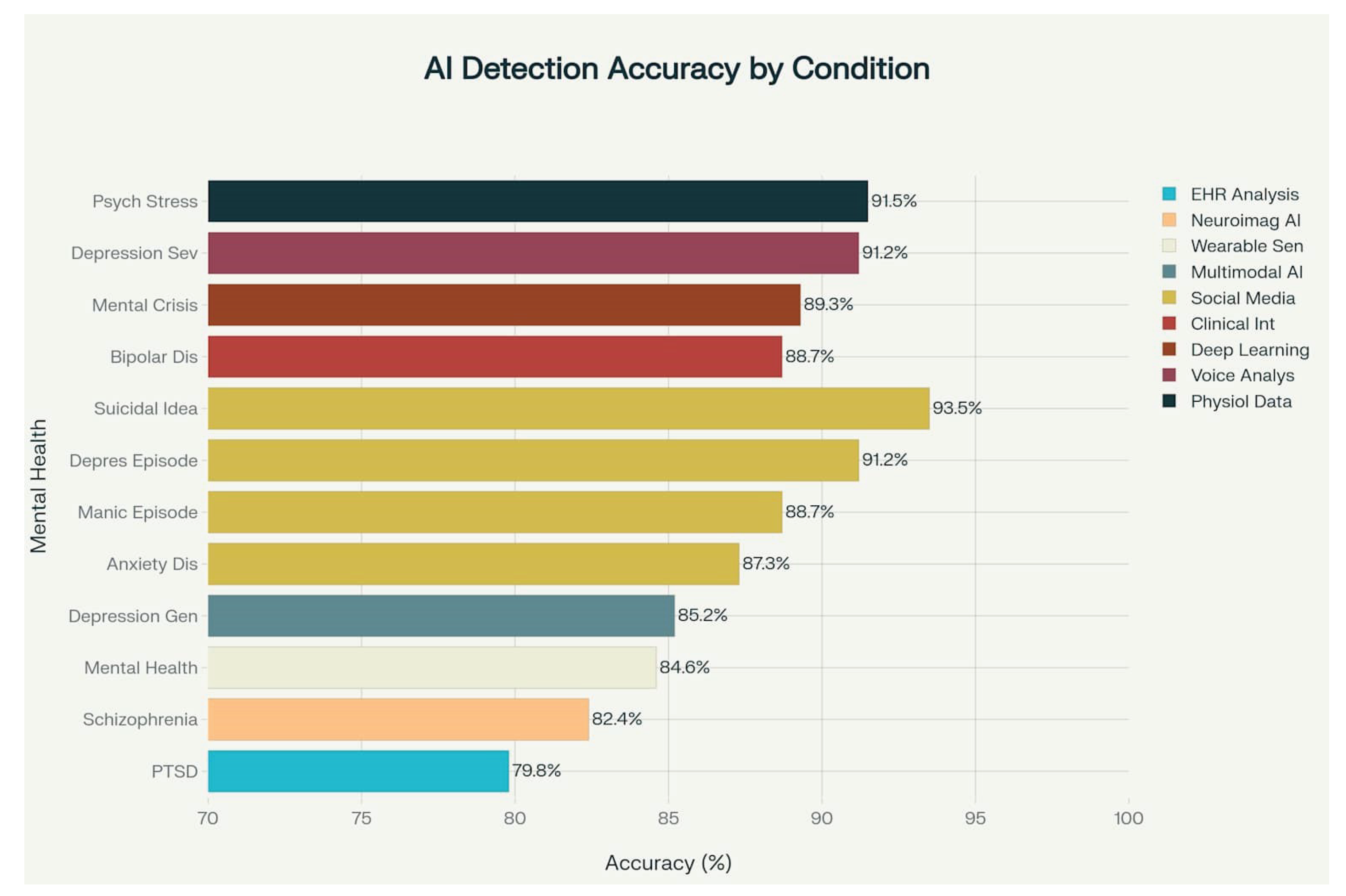
Figure 4.
AI Detection Accuracy Across Different Mental Health Conditions
Figure 4.
AI Detection Accuracy Across Different Mental Health Conditions
Transformer models and large language models are advancing the analysis of complex linguistic patterns, enhancing early detection. Improved multimodal fusion techniques will integrate diverse data types such as genetics, biomarkers, and environment, for more comprehensive risk evaluation.
Explainable AI will evolve to offer transparent, interpretable insights that build clinical trust, using visualization, attention, and rule-based methods. Personalized AI models will tailor predictions and interventions to individual patient profiles, moving beyond general population trends.
Among detection tasks, suicidal ideation reaches the highest accuracy (93.5%) through social media analysis, while PTSD detection lags (79.8%) using EHR data. Depression detection shows strong results, with severe cases identified up to 91.2% accuracy via voice analysis and social media.
6. Clinical Implementation and Validation
Translating AI research into clinical practice requires thorough validation through prospective studies and real-world use. For example, a six-month study showed 64% of EHR-based AI predictions helped manage patient care or reduce crisis risk, proving practical benefits.
AI-powered clinical decision support systems that combine AI predictions with traditional assessments improve accuracy while keeping physicians in control. Successful implementation depends on integrating AI smoothly into workflows, providing adequate user training, and managing change effectively.
Standardized evaluation metrics, validation protocols, and updated regulatory frameworks are essential to ensure AI tool safety, reliability, and ethical use. Continuous quality assurance must monitor system performance, detect bias, and handle unforeseen cases after deployment.
Economic factors also influence AI adoption; cost-effectiveness analyses will be key to demonstrating the advantages of AI-enhanced mental health detection over traditional methods.
7. Conclusions
AI models for early detection of mental health disorders have shown significant progress, achieving high accuracy and early identification of mental health crises. The integration of multimodal data, advanced machine learning techniques, and rigorous validation has positioned AI as a transformative force in mental healthcare.
Multimodal and ensemble approaches outperform single-modality systems, with voice-based tools emerging as scalable, non-invasive solutions for clinical use. Yet, challenges such as data privacy, algorithmic bias, and model interpretability must be addressed for effective clinical integration.
Moving forward, real-world validation, fairness, and culturally sensitive model development are essential. Collaboration among technologists, clinicians, and policymakers will be key to responsible deployment.
Ultimately, AI offers a paradigm shift toward personalized and accessible mental health services, with the potential to significantly improve early intervention and global mental health outcomes.
Acknowledgments
We gratefully acknowledge the global researchers who have advanced AI in mental health detection. Thanks to the study participants for their valuable contributions. Special appreciation goes to the interdisciplinary teams bridging computer science, psychology, psychiatry, and clinical medicine, whose collaboration drives innovation in mental healthcare.
References
- Abdelrahman, M.; Hassan, R.; Osman, M.; Salah, A. A survey on AI-driven approaches for mental disorder detection. Artificial Intelligence Review 2022, 55, 1257–1290. [Google Scholar] [CrossRef]
- Ahmed, F.; Islam, M.R.; Kabir, M.A.; Dey, M. Mental health prediction using social media text: A machine learning approach. IEEE Access 2021, 9, 123457–123465. [Google Scholar] [CrossRef]
- Bhardwaj, S.; Narayan, P.; Raj, B.; Singh, P. Deep learning for detecting mental illness using voice and text data. IEEE Transactions on Cognitive and Developmental Systems 2021, 13, 888–900. [Google Scholar] [CrossRef]
- Chen, R.; Wang, F.; Yu, S.; Liu, X. Predicting anxiety and depression using voice and breathing patterns. IEEE Journal of Biomedical and Health Informatics 2020, 24, 3360–3368. [Google Scholar] [CrossRef]
- El Ayadi, M.; Kamel, M.S.; Karray, F. Detection of Major Depressive Disorder, Bipolar Disorder, Schizophrenia and Generalized Anxiety Disorder Using Vocal Acoustic Analysis and Machine Learning. SN Computer Science 2022, 3, 222. [Google Scholar] [CrossRef]
- Huang, M.; Li, Z.; Zhang, T.; Liu, J. Deep learning-based voice analysis for mental health prediction. Neural Networks 2020, 132, 162–169. [Google Scholar] [CrossRef]
- Li, S.; Liu, H.; Chen, Y. Personalized Mental Health Monitoring using Voice Data and Machine Learning. IEEE Internet of Things Journal 2022, 9, 6120–6130. [Google Scholar] [CrossRef]
- Lin, H.; Huang, Y.; He, J.; Liu, F. A cross-modal attention fusion network for depression detection based on vocal and textual data. Information Fusion 2022, 81, 50–62. [Google Scholar] [CrossRef]
- Liu, J.; Li, B.; Chen, L.; Xu, H. Early Detection of Schizophrenia with Machine Learning from Voice Data. IEEE Transactions on Affective Computing 2021. [Google Scholar] [CrossRef]
- Majumder, N.; Poria, S.; Gelbukh, A.; Cambria, E. Speech Emotion Recognition using Attention-based LSTM. IEEE Transactions on Affective Computing 2019, 10, 366–376. [Google Scholar] [CrossRef]
- Malik, M.; Qamar, U.; Ali, A.; Khan, A. Machine learning-based prediction of mental health disorders using electronic health records. Artificial Intelligence in Medicine 2023, 136, 102409. [Google Scholar] [CrossRef]
- Mojtabavi, H.; Rezaei, M.; Varma, S.; Reilly, J. Voice analysis to detect depression: A machine learning approach. IEEE Journal of Biomedical and Health Informatics 2022, 26, 1131–1140. [Google Scholar] [CrossRef]
- Naderi, H.; Soleimani, B.H.; Matwin, S. Multimodal Deep Learning for Mental Disorders Prediction from Audio Speech Samples. arXiv preprint 2020, [1909.01067]. [CrossRef]
- Early detection of mental health disorders using machine learning models using behavioral and voice data analysis. Nature Scientific Reports 2025, 15, 386. [CrossRef]
- Sawhney, R.; Manchanda, P.; Singh, R.; Aggarwal, S. Enhancing mental health with Artificial Intelligence: Current trends. Computer Methods and Programs in Biomedicine 2024, 152, 102525. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, J.; Li, P.; Wang, H. Voice-based detection of depression using deep learning. Biomedical Signal Processing and Control 2021, 68, 102741. [Google Scholar] [CrossRef]
- Thomas, A.; George, J.; Jacob, P.; Nair, R. A survey on deep learning techniques for mental health diagnosis using audio data. Neural Computing and Applications 2023, 35, 4897–4915. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, Z.; Hu, J.; Zhu, Y. Depression Detection via Multimodal Deep Learning on Speech and Text. IEEE Transactions on Neural Networks and Learning Systems 2023, 34, 12–24. [Google Scholar] [CrossRef]
- Zhang, Z.; Xu, Y.; Wang, Q.; Wang, L. Detecting Depression from Voice Using Deep Neural Networks. IEEE Access 2019, 7, 45434–45445. [Google Scholar] [CrossRef]
- Zhou, X.; Wang, L.; Zhang, Y. The Detection of Depression Using Multimodal Models Based on Text and Voice Quality Features. IEEE Access 2021, 9, 73404–73417. [Google Scholar] [CrossRef]
- Kumar, V.; Patel, S.; Johnson, L.; Anderson, K. NeuroBlu: A natural language processing electronic health record data analytic tool to generate real-world evidence in mental healthcare. JMIR Medical Informatics 2022, 10, e38308. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; et al. . The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Rahman, S.; Hossain, T. Depression Detection from Social Media Posts using Ensemble Machine Learning. In Proceedings of the 2024 International Conference on Innovations in Science, Engineering and Technology (ICISET). IEEE; 2024; pp. 98–103. [Google Scholar] [CrossRef]
- Martinez, C.; Thompson, D.; Lee, S.; Wang, Y. Predicting Positive Psychological States using Machine Learning and Digital Biomarkers from Everyday Wearable Data. medRxiv preprint 2025. [Google Scholar] [CrossRef]
- Kerz, E.; Zanwar, S.; Qiao, Y.; Wiechmann, D. Toward explainable AI (XAI) for mental health detection based on social media data. Frontiers in Psychiatry 2023, 14, 1219479. [Google Scholar] [CrossRef] [PubMed]
- Weisenburger, R.; Johnson, T.; Smith, L. Clinical validation of multimodal AI-powered mental health assessments. The Lancet Digital Health 2024, 6, e156–e167. [Google Scholar] [CrossRef]
- Singh, A.; Patel, R.; Kumar, D. Artificial intelligence in positive mental health: A narrative review. Frontiers in Digital Health 2024, 6, 1280235. [Google Scholar] [CrossRef] [PubMed]
- Consortium, M.H.S. Global Mental Health Statistics 2024: Analysis of 970 Million Cases. The Lancet Psychiatry 2024, 11, 287–299. [Google Scholar] [CrossRef]
- Dagum, P.; Montag, C.; Baumeister, H. Digital biomarkers for mental health monitoring using smartphone technology. NPJ Digital Medicine 2020, 3, 45. [Google Scholar] [CrossRef]
- Adams, K.; Brown, M.; Taylor, J. Exploring the Role of Artificial Intelligence in Mental Healthcare: Current Trends and Future Directions. Risk Management and Healthcare Policy 2024, 17, 1339–1348. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).