1. Introduction
Primary pericardial mesothelioma represents a rare malignancy, accounting for approximately 0.7% of all mesotheliomas, with merely 200 cases documented globally [
1]. This pathology is characterized by late diagnosis, limited therapeutic responsiveness, and an ominous prognosis, with median survival typically not exceeding six months [
2,
3].
Surgical intervention may constitute an efficacious therapeutic strategy when the neoplasm remains circumscribed without extensive invasion [
4,
5]. However, due to rapid disease progression and delayed diagnosis, surgical interventions often serve palliative purposes rather than curative intent. Contemporary literature regarding surgical outcomes remains limited. We present a case of a 50-year-old male presenting with cardiac tamponade secondary to primary pericardial mesothelioma who underwent successful surgical intervention.
2. Case Presentation
A previously healthy 50-year-old male with no documented asbestos exposure presented with a one-week history of left-sided chest discomfort, progressive dyspnea, fatigue, and diminished exercise tolerance. Upon admission, he exhibited significant fatigue, persistent dyspnea, chest discomfort, low-grade pyrexia (37.8°C), tachypnea (24 breaths/minute), jugular venous distention, tachycardia (110 beats/minute), and hypotension (95/60 mmHg).
Chest radiography revealed cardiomegaly with clear lung fields. Echocardiography demonstrated substantial pericardial effusion with right atrial and ventricular compression. Emergency pericardiocentesis yielded 500ml of serosanguineous fluid. Initial cytological analysis revealed chronic inflammatory characteristics without malignant cells. Serial echocardiographic monitoring demonstrated rapid fluid reaccumulation.
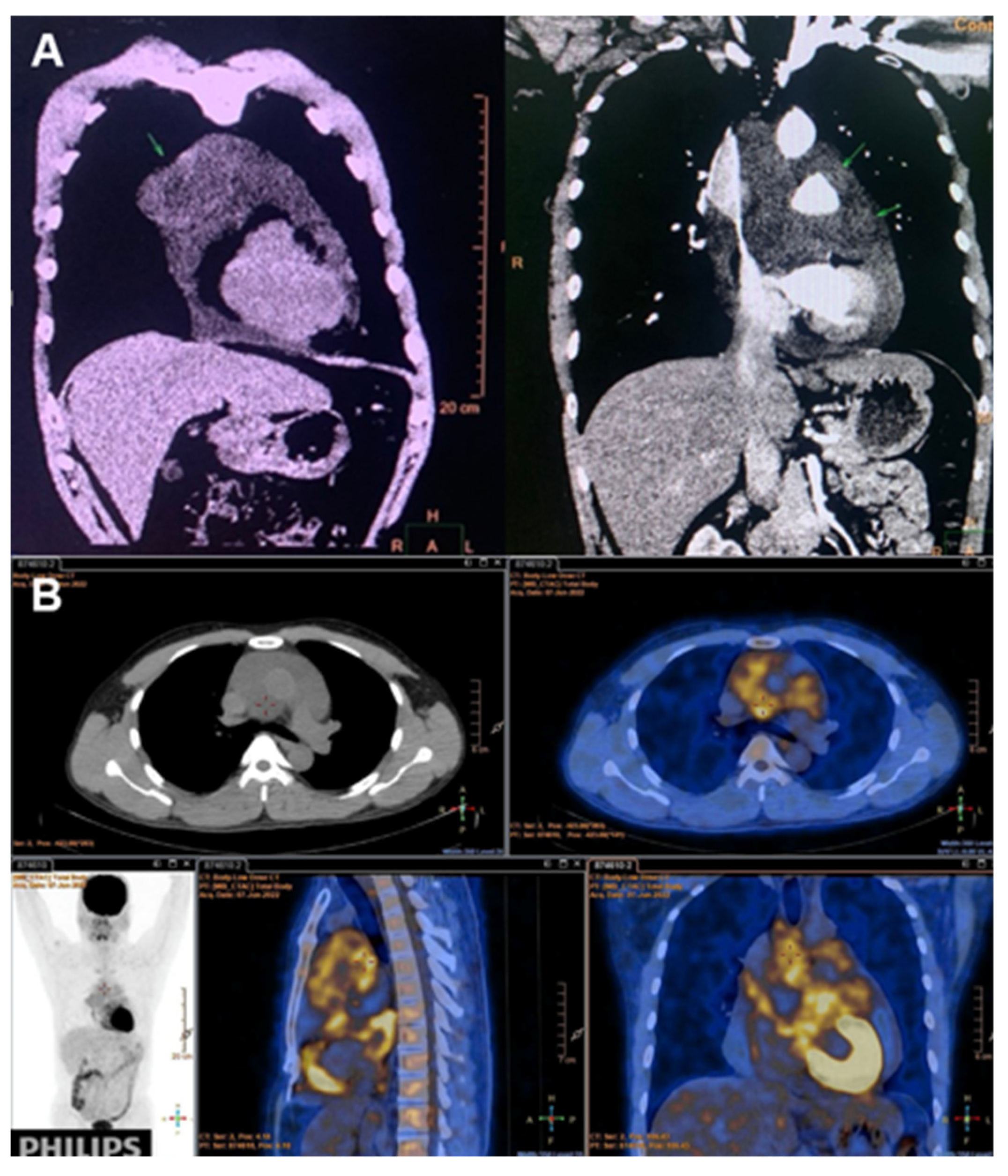
Subsequent cell-block analysis of pericardial fluid revealed epithelioid cells with nuclear atypia. Immunohistochemistry demonstrated strong positivity for CK5/6, CK7, and Calretinin; moderate positivity for WT1; and negativity for TTF-1—findings consistent with pericardial mesothelioma. PET/CT revealed pericardial thickening with multiple FDG-avid nodules without evidence of distant metastasis (
Figure 1A and 1B).
2.1. Surgical Intervention
The patient underwent surgical resection of the pericardial tumor. Intraoperatively, central venous pressure remained elevated (20-25mmHg). The pericardial cavity contained viscous, turbid fluid with multiple hemorrhagic clots. The parietal pericardium appeared inflamed and thickened with nodular infiltrations.
A substantial anterior tumor (15×15cm) was identified, extending superiorly to the aortic arch, rightward to the brachiocephalic trunk, inferiorly to the cardiac base with epicardial and myocardial invasion, and posteriorly to the left atrial roof. The neoplasm exhibited heterogeneous composition with solid and cystic components. Tumor infiltration was noted in the mediastinal pleura bilaterally, ascending aortic wall, encompassing two-thirds of the superior vena cava circumference, and invading the innominate vein, causing significant superior vena cava compression.
Complete evacuation of pericardial fluid, removal of hemorrhagic clots, and partial tumor resection were performed. Due to extensive invasion of vital structures, complete tumor resection was unattainable. The pericardial cavity was irrigated with 2% povidone solution, bilateral pleuropericardial windows were established, and bilateral pleural and pericardial drains were positioned.
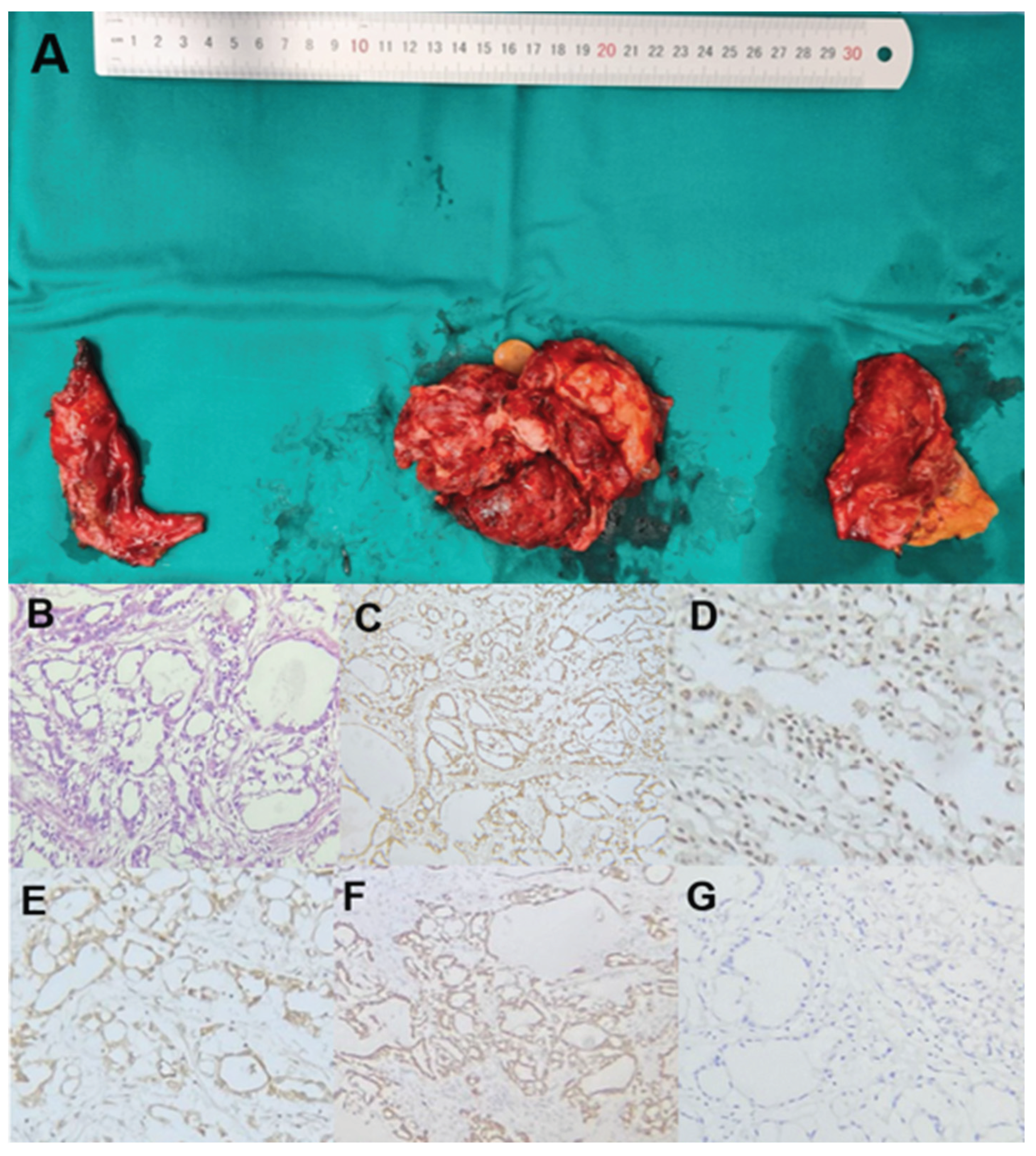
The resected tumor tissue and pericardium demonstrated irregular, thickened tissue with nodular infiltrations and areas of hemorrhage (
Figure 2A). Histopathological examination confirmed epithelioid-type primary pericardial mesothelioma, with characteristic features evident on HE staining (
Figure 2B). Immunohistochemical analysis showed strong positivity for Calretinin (
Figure 2C), positive WT1 staining (
Figure 2D), positive D2-40 staining (
Figure 2E), and CK7 positivity (
Figure 2F), while TTF-1 staining was negative (
Figure 2G), confirming the diagnosis of primary pericardial mesothelioma.
2.2. Postoperative Course
The patient’s postoperative course was favorable, with gradual clinical improvement. Symptoms of chest discomfort, dyspnea, and superior vena cava compression syndrome resolved. Stable hemodynamics were achieved. Postoperative echocardiography demonstrated minimal residual pericardial effusion with preserved cardiac contractility (ejection fraction 68%).
Maintenance chemotherapy with Pemetrexed (500 mg/m2) plus Carboplatin (AUC 6) was initiated on a 21-day cycle. At 15-month follow-up, the patient continues regular outpatient evaluations without evidence of distant metastasis.
3. Discussion
3.1. Diagnostic Challenges
Primary pericardial mesothelioma presents formidable diagnostic challenges due to its protean clinical manifestations and limitations of conventional diagnostic modalities. Patients typically present at advanced stages with manifestations of constrictive pericarditis, pericardial effusion, or cardiac tamponade
[6].
Diagnostic yield from pericardiocentesis remains suboptimal, with literature suggesting that merely 10-30% of cases are definitively diagnosed through cytological examination of pericardial fluid
[7,8]. This limitation was evident in our patient, where initial cytological analysis revealed nonspecific inflammatory cells, necessitating more sophisticated cell-block analysis for diagnosis.
Conventional imaging techniques provide variable utility. Echocardiography typically reveals nonspecific findings including pericardial effusion or thickening [
9]. PET/CT offers additional diagnostic value through identification of hypermetabolic lesions, as demonstrated in our case.
Definitive diagnosis requires histopathological examination with characteristic immunohistochemical profile, including positivity for CK5/6, Calretinin, WT1, and negativity for markers of other malignancies such as TTF-1 [10].
3.2. Surgical Management and Prognostic Implications
Contemporary literature lacks consensus regarding optimal management. Historical studies emphasize the importance of complete tumor resection for survival [
4,
5]. However, in most reported cases, surgery serves primarily palliative purposes rather than curative intent due to extensive local invasion at presentation [11].
Our surgical approach focused on symptomatic relief through partial tumor debulking, pericardial drainage, and pleuropericardial window creation. Complete resection was precluded by extensive invasion of vital mediastinal structures. Despite incomplete resection, our patient demonstrated marked symptomatic improvement and exceeded typical survival expectations, remaining clinically stable at 15-month follow-up with adjuvant chemotherapy.
This outcome contrasts with previously reported survival statistics. Brydges et al. demonstrated that pericardial mesothelioma carries significantly shorter median survival (2 versus 10 months) compared to pleural mesothelioma [12].
The dismal prognosis stems from its aggressive nature, delayed diagnosis, surgical limitations, and relative chemoradioresistance. Mortality typically results from constrictive pericarditis, cardiac tamponade, or heart failure [13].
Our case demonstrates that despite incomplete resection, surgical intervention combined with appropriate adjuvant therapy can provide significant symptomatic relief and potentially extend survival beyond the expected duration. This underscores the potential value of multimodality treatment approaches even in cases where complete resection is unattainable.
4. Conclusions
Primary pericardial mesothelioma represents an exceedingly rare malignancy with ominous prognosis. Diagnostic challenges persist due to nonspecific clinical manifestations. Surgical intervention provides valuable diagnostic information and may confer significant symptomatic relief even when complete resection is unattainable. Our case demonstrates that multimodality treatment incorporating partial surgical debulking and adjuvant chemotherapy may extend survival beyond typically reported durations. Given the extreme rarity of this condition, surgical indications, optimal operative techniques, and postoperative management strategies warrant further investigation.
Funding
This research received no external funding.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data that support the findings of this case report are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kong, L.; Li, Z.; Wang, J.; Lv, X. Echocardiographic characteristics of primary malignant pericardial mesothelioma and outcomes analysis: a retrospective study. Cardiovasc Ultrasound. 2018, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Thomason, R.; Schlegel, W.; Lucca, M.; Cummings, S.; Lee, S. Primary malignant mesothelioma of the pericardium. Case report and literature review. Tex Heart Inst J. 1994, 21, 170–174. [Google Scholar] [PubMed]
- Watanabe, A.; Sakata, J.; Kawamura, H.; Yamada, O.; Matsuyama, T. Primary pericardial mesothelioma presenting as constrictive pericarditis. Jpn Circ J. 2000, 64, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Van De Water, J.M.; Allen, W.A. Pericardial mesothelioma. Ann Thorac Surg. 1967, 3, 162–165. [Google Scholar] [CrossRef] [PubMed]
- McGehee, E.; Gerber, D.E.; Reisch, J.; Dowell, J.E. Treatment and outcomes of primary pericardial mesothelioma: a contemporary review of 103 published cases. Clin Lung Cancer. 2019, 20, e152–e157. [Google Scholar] [CrossRef] [PubMed]
- Massicotte, G.; Bernier, M.; Piché, M.-E.; Cantin, L.; Couture, C. Case report of aggressive primary pericardial mesothelioma presenting as a constrictive pericarditis. Circ Cardiovasc Imaging. 2019, 12, e008621. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, A.; Rasmuson, T. Primary pericardial mesothelioma: report of a patient and literature review. Case Rep Oncol. 2009, 2, 125–132. [Google Scholar] [CrossRef] [PubMed]
- McGehee, E.; Gerber, D.E.; Reisch, J.; Dowell, J.E. Treatment and outcomes of primary pericardial mesothelioma: a contemporary review of 103 published cases. Clin Lung Cancer. 2019, 20, e152–e157. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Li, Z.; Wang, J.; Lv, X. Echocardiographic characteristics of primary malignant pericardial mesothelioma and outcomes analysis: a retrospective study. Cardiovasc Ultrasound. 2018, 16, 7. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).