Submitted:
25 June 2025
Posted:
26 June 2025
You are already at the latest version
Abstract
Keywords:
Introduction
2. Materials and Methods
2.1. Study Population
2.2. Postoperative Analgesia
2.3. Data Collection and Analysis
2.4. Statistical Analysis
3. Results
3.1. Sudy Population
Outcome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APOP | Acute Post Operative Pain |
| ERAS | Enhanced Recovery After Surgery |
| VATS | Video-Assisted Thoracic Surgery |
| TEA | Thoracic Epidural Anaesthesia |
| PVB | ParaVertebral Block |
| OS | Opioid-Sparing |
| MHz | Mega Hertz |
| mg | Milligram |
| kg | Kilogram |
| NRS | Numeric Rating Scale |
| BMI | Body Mass Index |
| PONV | Postoperative Nausea And Vomiting |
| LOS | Length Of Hospital Stay |
| SpO2 | Blood Oxygen Saturation |
| ASA | American Society Of Anetshesiologists |
| SBP | Systolic Blood Pressure |
| DBP | Diastolic Blood Pressure |
| HR | Heart Rate |
| bpm | beat per minute |
| NMDA | Ketamine, an N-methyl-D-aspartate |
| LAST | Local Anesthetic Sytemic Toxicity |
References
- Gerner, P. Postthoracotomy Pain Management Problems. Anesthesiol. Clin. 2008, 26, 355–367. [Google Scholar] [CrossRef]
- Maxwell, C.; Nicoara, A. New developments in the treatment of acute pain after thoracic surgery. Curr. Opin. Anaesthesiol. 2014, 27, 6–11. [Google Scholar] [CrossRef]
- Elmore, B.; Nguyen, V.; Blank, R.; Yount, K.; Lau, C. Pain Management Following Thoracic Surgery. Thorac. Surg. Clin. 2015, 25, 393–409. [Google Scholar] [CrossRef] [PubMed]
- Ghanty, I.; Schraag, S. The quantification and monitoring of intraoperative nociception levels in thoracic surgery: a review. J. Thorac. Dis. 2019, 11, 4059–4071. [Google Scholar] [CrossRef] [PubMed]
- Setti, T.; Sanfilippo, F.; Leykin, Y. Transdermal buprenorphine for postoperative pain control in gynecological surgery: a prospective randomized study. Curr. Med Res. Opin. 2012, 28, 1597–1608. [Google Scholar] [CrossRef] [PubMed]
- Marshall, K.; McLaughlin, K. Pain Management in Thoracic Surgery. Thorac Surg Clin. 2020, 30, 339–346. [Google Scholar] [CrossRef]
- Baldi, C.; Bettinelli, S.; Grossi, P.; Fausto Sardanelli, A.F.; Cavalloro, F.; Allegri, M.; Brasch, A. Ultrasound guidance for locoregional anesthesia: a review. Minerva Anestesiol. 2007, 73, 587–593. [Google Scholar]
- Biuzzi, C.; Marianello, D.; Wellens, C.; Bidi, B.; DI Chiaro, A.; Remiddi, F.; Franchi, F.; Scolletta, S. Multimodal analgesic strategies in polytraumatized patients. Minerva Anestesiol. 2024, 90, 1029–1040. [Google Scholar] [CrossRef]
- Sepolvere, G.; Marianello, D.; Santonocito, C.; Messina, S.; Silvetti, S.; Franchi, F.; Paternoster, G.; Sanfilippo, F. Perspectives On The Role Of Thoracic Fascial Blocks In Cardiac Anaesthesia: Will They Represent A New Era? J Clin Med. 2025, 14, 973. [Google Scholar] [CrossRef]
- Joshi, G.P.; Bonnet, F.; Shah, R.; Wilkinson, R.C.; Camu, F.; Fischer, B.; Neugebauer, E.A.M.; Rawal, N.; Schug, S.A.; Simanski, C.; et al. A Systematic Review of Randomized Trials Evaluating Regional Techniques for Postthoracotomy Analgesia. Anesthesia Analg. 2008, 107, 1026–1040. [Google Scholar] [CrossRef]
- Davies, R.G.; Myles, P.S.; Graham, J.M. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy—a systematic review and meta-analysis of randomized trials. Br. J. Anaesth. 2006, 96, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Yeung, J.H.Y.; Gates, S.; Naidu, B.V.; Wilson, M.J.A.; Gao Smith, F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016, 2, CD009121. [Google Scholar] [CrossRef] [PubMed]
- D’Erco Hle, F.; Harendra Arora, H.; Kumar, P. Paravertebral block for Thoracic Surgery. Journal of Cardiothoracic and Vascular Anesthesia 2018, 32, 915–927. [Google Scholar] [CrossRef]
- Crumley, S.; Schraag, S. The role of local anaesthetic techniques in ERAS protocols for thoracic surgery. J. Thorac. Dis. 2018, 10, 1998–2004. [Google Scholar] [CrossRef] [PubMed]
- George, M.J. The site of action of epidurally administered opioids and its relevance to postoperative pain management. Anaesthesia 2006, 61, 659–664. [Google Scholar] [CrossRef]
- Batchelor, T.J.P.; Rasburn, N.J.; Abdelnour-Berchtold, E.; Brunelli, A.; Cerfolio, R.J.; Gonzalez, M.; Ljungqvist, O.; Petersen, R.H.; Popescu, W.M.; Slinger, P.D.; et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardio-Thoracic Surg. 2018, 55, 91–115. [Google Scholar] [CrossRef]
- Cook, T.M.; Counsell, D.; Wildsmith, J.A.W. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br. J. Anaesth. 2009, 102, 179–190. [Google Scholar] [CrossRef]
- Ding, X.; Jin, S.; Niu, X.; Ren, H.; Fu, S.; Li, Q.; Landoni, G. A Comparison of the Analgesia Efficacy and Side Effects of Paravertebral Compared with Epidural Blockade for Thoracotomy: An Updated Meta-Analysis. PLOS ONE 2014, 9, e96233. [Google Scholar] [CrossRef]
- Helms, O.; Mariano, J.; Hentz, J.-G.; Santelmo, N.; Falcoz, P.-E.; Massard, G.; Steib, A. Intra-operative paravertebral block for postoperative analgesia in thoracotomy patients: a randomized, double-blind, placebo-controlled study. Eur. J. Cardio-Thoracic Surg. 2011, 40, 902–906. [Google Scholar] [CrossRef]
- Eason, M.; Wyatt, R. Paravertebral thoracic block—a reappraisal. Anaesthesia 1979, 34, 638–642. [Google Scholar] [CrossRef]
- Luyet, C.; Herrmann, G.; Ross, S.; et al. Ultrasound-guided thoracic paravertebral puncture and placement of catheters in human cadavers: where do catheters go? Br J Anaesth. 2011, 106, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Fortier, S.; Hanna, H.A.; Bernard, A.; Girard, C. Comparison Between Systemic Analgesia, Continuous Wound Catheter Analgesia And Continuous Thoracic Paravertebral Block: A Randomised, Controlled Trial Of Post thoracotomy Pain Management. Eur J Anaesthesiol. 2012, 29, 524–530. [Google Scholar] [CrossRef]
- Radvansky, B.M.; Shah, K.; Parikh, A.; Sifonios, A.N.; Le, V.; Eloy, J.D. Role of Ketamine in Acute Postoperative Pain Management: A Narrative Review. BioMed Res. Int. 2015, 2015, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chumbley, G.M.; Thompson, L.; Swatman, J.E.; Urch, C. Ketamine infusion for 96 hr after thoracotomy: Effects on acute and persistent pain. Eur. J. Pain 2019, 23, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, C.; Alfille, P.; Mountjoy, J.; Bao, X. Regional anesthesia and acute perioperative pain management in thoracic surgery: a narrative review. J. Thorac. Dis. 2022, 14, 2276–2296. [Google Scholar] [CrossRef]
- Chen, X.; Liu, Q.; Fan, L. Effects of thoracic paravertebral block combined with s-ketamine on postoperative pain and cognitive function after thoracoscopic surgery. Heliyon 2022, 8, e12231. [Google Scholar] [CrossRef]
- Michelet, P.; Guervilly, C.; Hélaine, A.; Avaro, J.P.; Blayac, D.; Gaillat, F.; Dantin, T.; Thomas, P.; Kerbaul, F. Adding ketamine to morphine for patient-controlled analgesia after thoracic surgery: influence on morphine consumption, respiratory function, and nocturnal desaturation. Br. J. Anaesth. 2007, 99, 396–403. [Google Scholar] [CrossRef]
- Suzuki, M.; Haraguti, S.; Sugimoto, K.; Kikutani, T.; Shimada, Y.; Sakamoto, A. Low-dose Intravenous Ketamine Potentiates Epidural Analgesia after Thoracotomy. Anesthesiology 2006, 105, 111–119. [Google Scholar] [CrossRef]
- Dualé, C.; Gayraud, G.; Taheri, H.; Bastien, O.; Schoeffler, P. A French Nationwide Survey on Anesthesiologist-Perceived Barriers to the Use of Epidural and Paravertebral Block in Thoracic Surgery. J. Cardiothorac. Vasc. Anesthesia 2015, 29, 942–949. [Google Scholar] [CrossRef]
- Chumbley, G.M.; Thompson, L.; Swatman, J.E.; Urch, C. Ketamine infusion for 96 hr after thoracotomy: Effects on acute and persistent pain. Eur. J. Pain 2019, 23, 985–993. [Google Scholar] [CrossRef]
- Jouguelet-Lacoste, J.; La Colla, L.; Schilling, D.; Chelly, J.E. The Use of Intravenous Infusion or Single Dose of Low-Dose Ketamine for Postoperative Analgesia: A Review of the Current Literature. Pain Med. 2015, 16, 383–403. [Google Scholar] [CrossRef] [PubMed]
- Nesher, N.; Serovian, I.; Marouani, N.; Chazan, S.; Weinbroum, A. Ketamine spares morphine consumption after transthoracic lung and heart surgery without adverse hemodynamic effects☆. Pharmacol. Res. 2008, 58, 38–44. [Google Scholar] [CrossRef]
- Turhan, Ö.; Sivrikoz, N.; Sungur, Z.; Duman, S.; Özkan, B.; Şentürk, M. Thoracic Paravertebral Block Achieves Better Pain Control Than Erector Spinae Plane Block and Intercostal Nerve Block in Thoracoscopic Surgery: A Randomized Study. J. Cardiothorac. Vasc. Anesthesia 2021, 35, 2920–2927. [Google Scholar] [CrossRef] [PubMed]
- Feray, S.; Lemoine, A.; Aveline, C.; Quesnel, C. Pain management after thoracic surgery or chest trauma. Minerva Anestesiol. 2023, 89, 1022–1033. [Google Scholar] [CrossRef] [PubMed]
- Dualé, C.; Ouchchane, L.; Schoeffler, P.; Dubray, C.; Soule-Sonneville, S.; Decoene, C.; Baylot, D.; Lefebvre-Kuntz, D.; Reynier, P.; Sokolo, B.; et al. Neuropathic Aspects of Persistent Postsurgical Pain: A French Multicenter Survey With a 6-Month Prospective Follow-Up. J. Pain 2014, 15, 24.e1–24.e20. [Google Scholar] [CrossRef]
- Huan, Y.; Wannan, C.; Youwen, C.; Huayuan, G.; Yu, F.; Mingxiang, F.; Xiaoming, W.; Han, T.; Jiacheng, Y.; Yunjia, Q.; Ming, D.; Jing, C.; Changhong, M.; Hao, W. Opioid-Free Versus Opioid-Based Anesthesia on Postoperative Pain After Thoracoscopic Surgery: The Use of Intravenous and Epidural Esketamine. Anesthesia & Analgesia. 2023, 137, 399–408. [Google Scholar]
- Na, H.-S.; Koo, C.-H.; Koo, B.-W.; Ryu, J.-H.; Jo, H.; Shin, H.-J. Effect of the Paravertebral Block on Chronic Postsurgical Pain After Thoracic Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Cardiothorac. Vasc. Anesthesia 2022, 37, 252–260. [Google Scholar] [CrossRef]
- Bugada, D.; Ghisi, D.; Mariano, E.R. Continuous regional anesthesia: a review of perioperative outcome benefits. Minerva Anestesiol. 2017, 83, 1089–1100. [Google Scholar] [CrossRef]
| Variables | Overall Population (N =62) |
OS Group (n=41) |
Control Group (n=21) |
p Value |
|---|---|---|---|---|
| Age, years | 68 [64-73] | 71 [65-74] | 67 [61-73] | 0.16 |
| Sex (M), N (%) | 24 (39) | 18 (44) | 6 (29) | 0.25 |
| Weight, kg | 70 [58-79] | 70 [60-80] | 65 [55-70] | 0.13 |
| Height, cm | 166 [160-172] | 166 [162-180] | 165 [159-175] | 0.60 |
| ASA Score | 2 [2-2] | 2 [2-2] | [2-2] | 0.07 |
| Variables | Overall Population (n=62) | OS Group (n=41) |
Control Group (n=21) |
p |
|---|---|---|---|---|
| Morphine rescue (by 48 h) | 18 (29%) | 8 (19.5%) | 10 (47.6%) | 0.021 |
| NRS after surgery | 2 [1-3] | 1 [1-2] | 4 [3-4] | <0.001 |
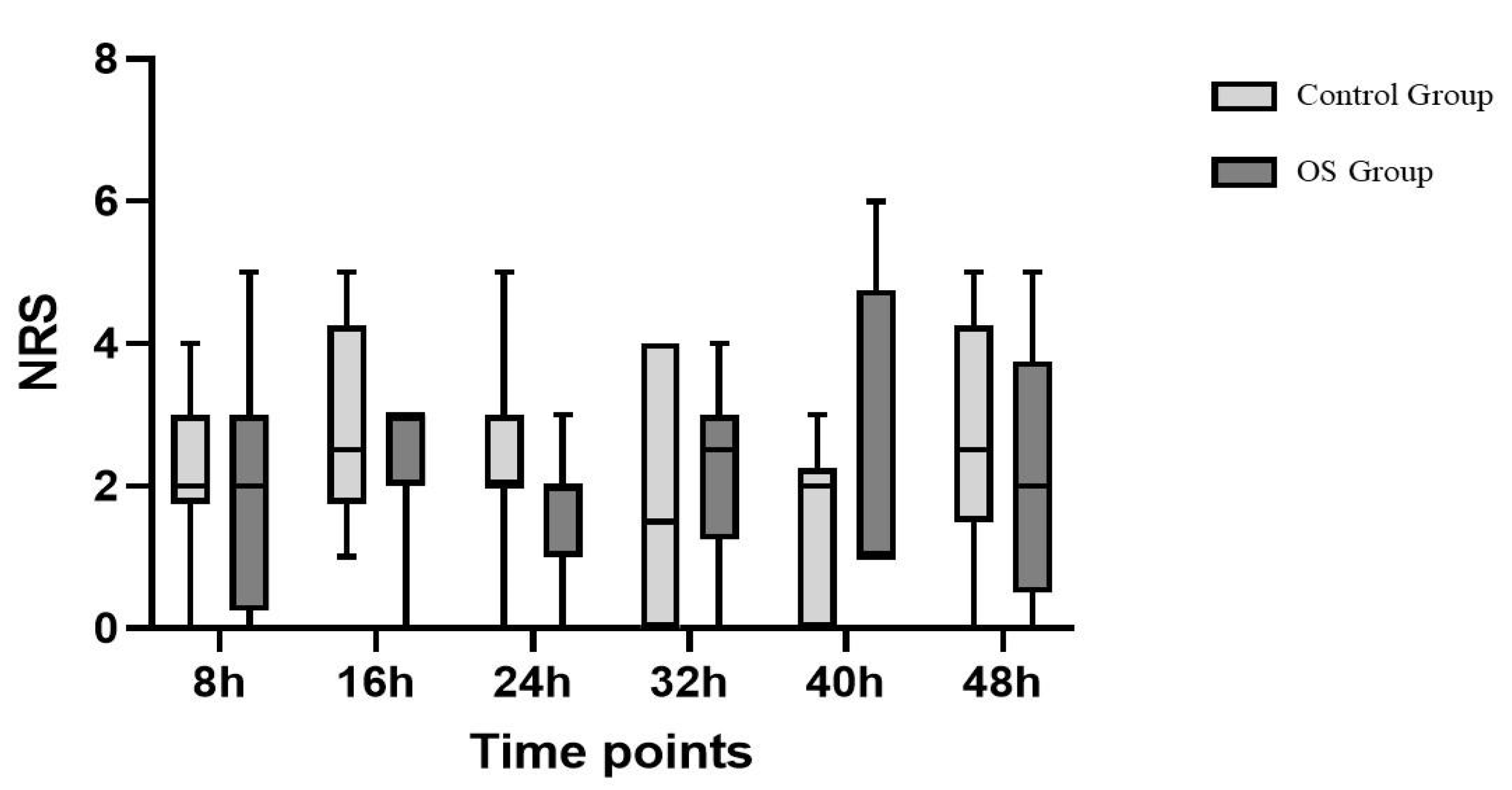
| NRS 8h | 2 [1-2] | 2 [1-2] | 2 [1-2] | 0.66 |
| NRS 16h | 2 [1-3] | 1 [1-2] | 2 [1-2] | 0.50 |
| NRS 24h | 2 [1-2] | 2 [1-2] | 2 [1-3] | 0.24 |
| NRS 32h | 1 [1-2] | 0 [0-2] | 2 [1-3] | 0.12 |
| NRS 40h | 1 [0-2] | 1 [1-2] | 1 [0-2] | 0.37 |
| NRS 48h | 1 [0-2] | 1 [0-2] | 0 [0-3] | 0.11 |
| Chronic Pain, n (%) | 21 (33,9%) | 10 (23,8%) | 11 (52,4%) | 0.028 |
| Overall Population (n=62) |
OS Group (n=41) |
Control Group (n=21) |
p | |
|---|---|---|---|---|
| SBP after surgery, mmHg | 120 [110-135] | 120 [110-135] | 120 [115-140] | 0.28 |
| SBP 8h | 130 [120-140] | 130 [120-140] | 130 [115-140] | 0.71 |
| SBP 16h | 125 [115-135] | 123 [115-135] | 125 [112-135] | 0.80 |
| SBP 24h | 125 [115-145] | 130 [115-150] | 125 [110-130] | 0.11 |
| SBP 32h | 125 [116-140] | 130 [120-140] | 120 [110-130] | 0.06 |
| SBP 40h | 125 [115-145] | 125 [115-145] | 120 [115-125] | 0.58 |
| SBP 48h | 130 [120-145] | 130 [120-150] | 133 [115-140] | 0.54 |
| DBP after surgery, mmHg | 70 [61-80] | 70 [60-80] | 70 [65-75] | 0.83 |
| DBP 8h, mmHg | 75 [70-85] | 80 [70-85] | 75 [60-80] | 0.26 |
| DBP 16h, mmHg | 75 [65-83] | 80 [65-83] | 70 [65-80] | 0.64 |
| DPB 24h, mmHg | 70 [65-80] | 75 [65-85] | 70 [60-80] | 0.07 |
| DBP 32h, mmHg | 72 [65-80] | 75 [68-87] | 70 [65-75] | 0.15 |
| DBP 40h, mmHg | 75 [65-85] | 75 [67-90] | 75 [65-80] | 0.24 |
| DBP 48h, mmHg | 80 [65-85] | 80 [65-90] | 75 [67-80] | 0.13 |
| HR after surgery, bpm | 75 [68-80] | 70 [67-75] | 85 [76-86] | <0.001 |
| HR 8h, bpm | 74 [70-78] | 75 [70-79] | 74 [67-76] | 0.32 |
| HR 16h, bpm | 75 [70-80] | 76 [68-81] | 75 [72-80] | 0.87 |
| HR 24h, bpm | 78 [70-85] | 78 [68-85] | 78 [75-84] | 0.67 |
| HR 32h, bpm | 74 [70-78] | 74 [70-80] | 75 [70-78] | 0.93 |
| HR 40h, bpm | 77 [70-80] | 77 [70-80] | 77 [70-80] | 0.64 |
| HR 48h, bpm | 78 [70-83] | 76 [70-80] | 80 [76-90] | 0.11 |
| SpO2 after surgery, % | 95 [94-97] | 95 [94-97] | 95 [94-95] | 0.02 |
| SpO2 8h, % | 96 [94-97] | 96 [94-97] | 95 [94-96] | 0.20 |
| SpO2 16h, % | 96 [94-97] | 96 [94-97] | 96 [94-97] | 0.96 |
| SpO2 24h, % | 95 [93-97] | 96 [93-98] | 95 [93-96] | 0.12 |
| SpO2 32h, % | 95 [93-97] | 95 [94-97] | 94 [92-96] | 0.14 |
| SpO2 40h, % | 95 [92-96] | 95 [93-96] | 93 [91-96] | 0.18 |
| SpO2 48h, % | 94 [93-96] | 94 [93-96] | 94 [91-96] | 0.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





