1. Introduction
Melanoma is a major public health concern, with over 330,000 new cases and more than 58,000 deaths per year worldwide by 2022 (1). It has now been established that one of the major prognostic factors for melanoma is the Breslow index, corresponding to the depth of invasion, measured in millimeters, of these lesions (2). Subungual melanomas (SUM) belong to the subcategory of acral-lentiginous melanomas, which represent ap- proximately 0.7 to 3.5% of all types of melanomas in Caucasians, but sometimes up to 50% of melanomas in Asian or African-Caribbean subjects (3, 4). SUM is most frequently found in the nail matrix, where it manifests as a dark, heterochromatic, longitudinal mela- nonychia with ill-defined contours that can sometimes invade adjacent skin folds. Historically, treatment was based on systematic amputation of the affected digit, often resulting in significant functional defect and cosmetic damage, which had a considerable impact on quality of life (5). Today, it has been established that in situ or minimally invasive melanomas (Breslow thickness < 0.5 mm) can be treated conservatively, by wide local excision (WLE) of the nail apparatus (6-8). SUM involves excision of the entire nail with margins generally between 5 and 10 mm, and immediate or delayed reconstruction (9). The choice of reconstruction technique is complex and not consensual, particularly when the excision is large, local functional requirements are important, and scarring threatens to cause cosmetic damage with social repercussions (10, 11). In order to better identify the possibility of reconstruction, we firstly, carried out a systematic review of the literature on surgical techniques used in nail reconstruction following SUM. Secondly, we evaluated the reconstructions carried out in our center, by a single operator, of soft tissue defect caused by a WLE in the context of a SUM.
2. Materials and Methods
2.1. Litterature Review
To identify the main surgical techniques used and to assess whether a consensus exists, we conducted a systematic review of the literature on methods of reconstruction after extended excision of the nail apparatus in SUM of the upper and lower limbs.
This systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (12). An exhaustive search was conducted in the MEDLINE (PubMed), Embase and Cochrane Library data-bases, from their creation to January 2025. The keywords used were: (‘Nail apparatus Melanoma’ OR ‘Nail Matrix Melanoma’ OR ‘Subungual Melano-ma’) AND (‘reconstruction’ OR “flap” OR ‘dermal matrix’ OR ‘skin graft’ OR ‘healing’). A manual search for the bibliographies of relevant articles completed the analysis. Only articles in English and French were retained. After an initial screening of titles and abstracts, duplicates, irrelevant studies, literature reviews, animal studies and cases of amputation were excluded. The full texts were then analyzed, and purely anatomical studies were excluded. This research project has been approved by the institutional ethics committee.
Studies were included according to the following criteria:
Type of study: case series, case reports, cohort studies, randomized controlled trials of nail reconstruction after melanoma removal.
Participants: adult or pediatric patients undergoing reconstruction after removal of a subungual melanoma of the upper or lower limb.
Results reported: type of melanoma and excision (margins), reconstruction technique, time frame, adjuvant treatments, complications, functional and aesthetic results, patient satisfaction, recurrences, length of follow-up. Two reviewers (L.C. and E.L.) independently examined the titles and abstracts, then the full texts of potentially eligible articles. Disagreements were resolved by discussion or arbitration by a third reviewer (O.C.).
Due to the heterogeneity of the studies (designs, populations, techniques), a meta-analysis was not envisaged. A narrative summary was produced, and the results were presented in the form of summary tables, bringing together the main characteristics and conclusions of the studies included.
Given the heterogeneity of study designs and outcome measures, a meta-analysis was not preferred. Instead, a narrative synthesis of the included studies was carried out. The data were organized and summarized in tabular form, highlighting the characteristics of the included studies, key findings and outcomes of interest.
2.2. Monocentric Retrospective Analysis
This is a single-center retrospective study carried out between July 2024 and March 2025, including all patients who have undergone reconstruction after extended excision of the nail apparatus as part of the treatment of a subungual melanoma.
This research project has been approved by the institutional ethics committee.
Adult and pediatric patients who underwent extended nail resection of the upper or lower limbs for subungual melanoma between January 2021 and October 2024 at our center were included.
Patients operated on for a non-melanoma nail tumor, those who refused to take part in the study, and cases with erratic follow-up that did not allow sufficient data to be collected were excluded.
The following variables were collected for each patient:
Demographic data: age, sex, occupation, laterality (in the case of upper limb involvement).
Complication risk factors: history of diabetes, smoking, major comorbidities.
Tumor characteristics: Breslow index, sentinel lymph node status if present.
Excision strategy: excision margins applied.
Reconstruction strategy: number of stages, reconstruction time, technique used, operating time.
Post-operative follow-up: occurrence of any major complications (infection, hematoma, failure of the reconstruction) or minor complications (early consultation, disunion, healing problems, return to the operating theatre for secondary touch-up).
Duration of post-operative follow-up.
Each patient was also asked to complete a functional evaluation questionnaire at least 6 months after the last operation:
- -
Damage to the upper limb was assessed by the Quick DASH (score from 0 to 100) and the Modified Mayo Wrist Score (score from 0 to 100).
- -
Damage to the lower limbs was assessed using the AOFAS score (American Orthopedic Foot and Ankle Score; score from 0 to 90).
3. Results
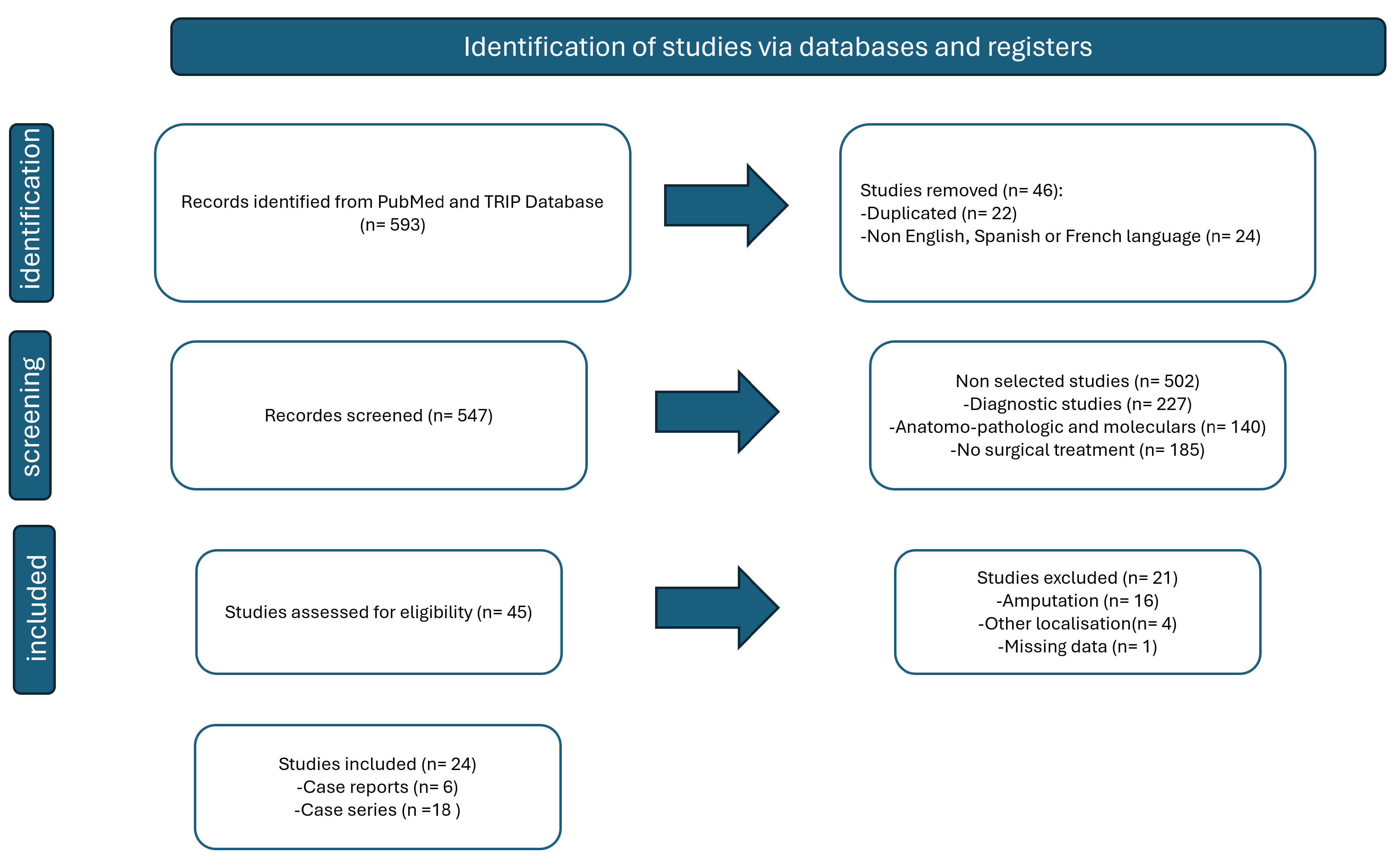
An initial search conducted in the PubMed and TRIP databases identified 593 articles. After removing duplicates and excluding articles written in languages other than French, English, or Spanish, 547 unique references were included for screening. Title and abstract review led to the selection of 45 articles for full-text assessment. Of these, 21 were excluded: 16 focused on cases managed by amputation, one provided insufficient data, and four dealt with acral lentiginous melanomas at unrelated anatomical sites. In total, 24 studies met the predefined inclusion and exclusion criteria and were included in the analysis (
Figure 1).
Of the 24 studies selected, 18 were case series (13-30), and six were single case reports (31-36). All the studies were retrospective (n = 23), except for one study which was a prospective case series (36). All the studies were published between 2003 for the oldest (17) and 2023 for the most recent (20).
Sample sizes varied from study to study, ranging from 1 to 140 (20) participants, for a total of 373 patients, with an average age of 53.4 years (4 to 81 years). Women predominated, with 252 of the 373 patients being women, representing a sex ratio of 67%.
One study did not specify the sex of the patients (26).
Of the articles included for which the location was specified, 91 patients had involvement of the lower limb - including 25 cases involving the hallux when this information was available - and 164 patients had involvement of the upper limb - including 50 cases involving the thumb. However, for 118 patients, the precise anatomical location was not reported. Four studies did not mention the location of the lesion at all (15, 17, 22, 25).
Regarding the diagnostic phase, the majority of articles (16, 20, 22-24, 26, 28, 30, 31, 33-35) reported that an initial biopsy was performed. Only one article (32) mentioned an immediate biopsy-exeresis, while two studies (18, 36) mentioned the absence of a biopsy. The presence or absence of prior biopsy was not specified in nine articles (13-15, 17, 19, 21, 25, 27, 29). When the degree of local invasion was reported, the majority of melanomas were in situ (n = 65). Among the invasive forms, five cases had a Breslow index of less than 1 mm, two cases a Breslow of between 1 and 3 mm, and two cases a Breslow of more than 3 mm. Six studies did not mention the stage of the melanoma (17, 18, 20-22).
These were not tumour resection margins in the strict sense of the term, but margins for resection of the entire nail apparatus, generally set at 5 mm in most studies (13-19, 22, 24, 34-36). However, some publications have reported wider margins of 10 mm (23, 31, 33, 35), while others have recommended narrower margins of 3 mm (20, 32). The standard Mohs micrographic surgery technique was used in two studies (25, 30), and the delayed Mohs or ‘Slow Mohs’ technique was also mentioned in two other publications (25, 30). Finally, one study reported the use of extemporaneous anatomopathological examination to check the margins of excision of the nail apparatus (28).
Full thickness skin graft (FTSG) was the preferred reconstruction technique in the majority of studies (13-19, 21, 23, 24, 27, 30-32), involving a total of 112 patients. Of these, ten studies (14-16, 19, 23, 24, 27, 30-32) reported that FTSG was performed immediately, at the same time as the extended excision, in 52 patients. In contrast, seven studies reported delayed reconstruction, involving 55 patients (14, 15, 17, 18, 24, 28-30, 32, 33, 36). The immediate or delayed nature of the reconstruction was not specified in four publications (13, 18, 21, 25).
Only the series by Crisan et al. reported the use of a negative pressure dressing in preparation for delayed FTSG (43). FTSG was used exclusively in 71 patients (13-15, 18,19, 21, 23, 24, 29-32), combined with a dermal matrix in five cases ((28, 33, 36), and combined with a perionychium flap in 43 patients (16, 17, 19). One study used a delayed thin skin graft after Mohs micrographic analysis (25).
With regard to the use of dermal matrices, three articles (28, 33, 36) were concerned, involving a total of five patients, for whom the dermal matrix was placed at the same time as the resection and a second stage with the placement of a FTSG three weeks after the first stage was carried out. Only PELNAC® matrix was used, except in one study where INTEGRA® was used (33).
Regarding flaps, only Motta et al. and Lee et al. (22, 35) who used free flaps, respectively a free toe transfer in one case, and ultra-thin perforating flaps of the superficial circumflex iliac artery (SCIP) in 41 cases, whereas eight studies mentioned local flaps, six of which in association with a FTSG (13, 16-19, 30) and two exclusive Foucher flap reconstruction (26, 34). Local flaps combined with FTSG were most often perironychium advancement or palmar advancement flaps (16, 17, 19); one case report proposed a cross-finger flap (30). Finally, two studies favoured directed healing only (18, 25) and one study did not mention the surgical technique for reconstruction (35).
The most frequently observed complication was melanoma recurrence, found in 11 studies ((15, 17-22, 24-26, 29, 30) involving a total of 67 patients. Of these, 13 required secondary amputation of the affected digit (15, 18, 19, 24-26, 29, 30). In 2 cases, recurrence was linked to histologically positive excision margins, requiring amputation (15, 29).
In a further 33 cases, the status of the margins was not specified, and the treatment options varied: 11 patients underwent amputation (18, 19, 24-26, 30), and 5 underwent revision surgery of the margins (17, 22, 25), including 3 by deferred Mohs technique (25). As regards distant recurrence, 21 cases were described (17, 19-22, 25) including:
2 transit metastases, one of which was treated surgically (17, 22)
10 lymph node involvement (17, 21)
11 visceral metastases, resulting in 2 deaths (17, 19, 20, 25).
Residual nail spicules were reported in 15 patients (13, 15, 16, 18) and epidermal cysts in 13 patients (13-15, 18). Other adverse events included:
10 cases of hypersensitivity to cold or shock;
9 cases of graft hyperpigmentation (13);
1 case of distal interphalangeal arthritis (29);
1 flexor sheath hematoma (24);
1 case of temporary functional exclusion of the finger (14).
Six studies reported no complications (23, 27, 28, 33, 34, 36) and two did not mention this criterion (31, 35)
Most studies did not mention complementary treatments (n=23).
Only one study (29) described complementary treatments, with an adjuvant course of Interferon alpha for one patient, in the context of the appearance of distant metastases. This same study also described a case of recurrence treated by radiotherapy, with an unspecified impact on the outcome of reconstruction, and a case of multiple recurrences of metastases in transit treated by iterative excision and directed healing. The sentinel node procedure was mentioned only in the study by Wollina et al, involving four patients, only one of whom had a micrometastasis (21). No study mentioned immunotherapy.
Post-operative functional and cosmetic results were assessed by the examiner in six studies (18, 29, 31-33, 35), by the patient in six other studies (14-16, 22, 28, 34), and by the patient and the examiner in one study (23); six studies did not mention who the assessor was (13,17, 24, 25, 27, 33, 36). 281
Functional recovery was judged acceptable to satisfactory in eight studies, involving a total of 80 patients (13, 14, 16-18, 23, 28, 29), whereas it was considered total, with a return to normal function in seven studies (14, 18, 24, 32-35) involving 39 patients.
Regarding the cosmetic result, it was judged to be little disturbed or good in 12 articles (13, 15-18, 23, 26, 28, 29, 31, 33, 36), involving 76 patients, whereas it was judged to be excellent or equivalent to the previous state in four studies (18, 24, 34, 35), involving 42 patients with heterogeneous surgical techniques: exclusive directed healing (18), Foucher flap in the case report of one patient (34), free onycho-cutaneous flap harvested from the hallux in the case report of one patient (35), and six cases treated by FTSG and five by exclusive directed healing in the series by Neczyporenko et al. (24). The cosmetic result was judged to be poor in only two patients in the series by Goettmann et al. (18), but although directed healing was the predominant choice, the technique used for these two patients were not specified.
Only one article classified its results using validated questionnaires, that of Lee et al (22), which found an average Quick-Disabilities of the Arm, Shoulder and Hand (DASH) score of 1.3 in the 14 patients undergoing surgery on the upper limb and an average Foot Function Index (FFI) score of 3.1 in the 12 patients undergoing surgery on the lower limb. 298
The time to return to work was specified in two studies (29, 33), and averaged four and six weeks respectively after the last operation.
Reported follow-up ranged from 3 months (34-36) to 120 months (18). The mean follow-up was 60.1 months, with a mean of 45 months.
Table 1.
summarizes the characteristics of the included studies.
Table 1.
summarizes the characteristics of the included studies.
| Ref. |
Type of arti- cle
Number of patients Distribution
Mean age (years)
(range)
|
Localisa-tion
F (Finger) T (Toe)
(n)
|
Local ex- tension |
Presence of
previous biopsy
Margins from Nail apparatus
|
Strategy of econstruction
Surgical management
|
Side effects,
Complications
|
Complemen- tary
treatment
|
Results |
Follow up mean (range) |
| Anda- Juarez et al, An Bras Derma- tol, 2016 |
Retrospective
15 patients (9F, 6M)
31 (4-66) |
Right hand: F2(2), F4(2), F5(1)
Left hand: F1 (1), F5 (3)
Right foot (5):
T1 (5)
Left foot (1): T1 |
SUM in situ |
5 mm
Supra periosteum re- section |
FTSG (14)
Banner flap (1 patient) |
No recurrence
Inclusion cysts (4)
Spicules (6)
Hypersensitivity (4) Moderate chronic pain (1)
Hyperpigmentation of
the skin graft (9) |
NA |
Functional and cos- metic outcome was good in all of them |
55
months (12-98) |
| Lazar et al, Hand- Surg Br, 2005 |
Retrospective
13 patients (8F, 5M)
10 patients with SUM (7F, 3M)
40 (NA) |
Right hand F1(3), F3(1), F5(1)
Left hand: F1 (2), F5(3) |
SUM in situ |
5 mm |
Immediate FTSG harvested from same forearm (9) Delayed FTSG harvested from same forearm (1) |
Temporary finger exclu- sion (1case)
Epidermal cyst (5 cases) |
NA |
Sensitivity: Weber 4-
6mm (7), NA (1)
Normal function (4), Slightly limited function (5), NA (1) Cosmetic outcome: Satisfied or normal (9), NA (1) |
48
months (6 – 84) |
| Puhain- dran et al, Tech Hand Up Ex- trem Surg, 2011 |
Retrospective
10 patients
(4F, 6 M)
6 patients with a SUM
MA 52 (24-80) |
NA |
SUM in situ,
<2cm diame- ter |
2 mm to nail fold |
Immediate FTSG |
Positive margin (1), treated by PID Disartic- ulation
Secondary surgery: Epidermal inclusion cyst (1)
Nail remnant (1) |
NA |
Acceptable appear- ance for all patients (assessed by 2 sur- geons)
Patients satisfied (6)
Unrestricted use of the hand (6) |
35
months (8-72) |
| Flores- Terry et al, Actas Dermo- sifiliogr, 2018 |
Retrospective 11 patients
7 patients with SUM (4F, 3M)
5 patients (3F, 2M)
treated by WLE
61 (45-81) |
Right hand: F2(1)
F3(1)
Left hand F1(1)
F2(1)
Right foot: T1 (1) |
SUM in situ (4)
or Sum with Breslow <1
mm (1) |
Previous biopsy 5 mm
Supra periosteum re- section |
Circumferential advance- ment flap
and Immediate FTSG |
No recurrency (5)
Wound infection (2)
subungual spicules (1), moderate stiffness of DIP of one finger (1) hy- persensitivity to cold (2), hypersensitivity to
mild trauma (4) |
NA |
Patients were satis- fied with the proce- dure and the results obtained (5)
Satisfaction was good and the impact on quality of life was minimal (5) |
39
months (12-96) |
| Moehrle et al, Derma- tol Surg, 2003 |
Retrospective
62 patients with SUM (25H, 37F)
31 treated by WLE (11 H, 20F)
MA 61 |
F1,2,3,4,5(20)
T1,2,3,4,5 (11) |
SUM in situ
Invasive SUM
Breslow < 1mm (6)
Breslow 1 to 2mm
(8)
Breslow 2 to 4mm
(6)
Breslow > 4mm (4)
NA: (7) |
5 mm WLE with safety
margin without bone resection (3)
WLE with safety margin with resec- tion of the distal part of the distal phalanx (28) |
FTSG with pulpal advance- ment flap
Single stage (1)
Several stages (30) Unspecified reconstruction after definitive three-dimen- sional histology |
Recurrencies (20 pa- tients)
Local recurrence (2) In transit recurrence (1)
Lymph node metastasis (7)
Distant metastasis (1) |
NA |
Function and cosme- sis of the involved finger or toe « pre- served » |
54
months (NA) |
| Goett- mann et al, J Eur Acad Derma- tol Ve- nereol, 2018 |
Retrospective
63 patients (44F, 19M)
58 treated by WLE
51 (NA) |
F1 (24)
F2,3,4,5 (23)
T1 (10)
T3(1) |
All SUM, if pulp not in- volved |
No previous biopsy WLE (12)
Partial excision of the appliance removing the lesion, and the nearby paronychium (47) |
Healing by secondary inten- tion (52)
FTSG (3 patients)
Flap (1) |
Local recurrences at 24 and 32 months treated by amputation (2)
Spicules (7)
Epidermal cysts (2) |
NA |
No functional dis- comfort (20) Moderate discom- fort (14) Aesthetic discomfort was judged to be absent
(29) Moderate aes-
thetic discomfort (8)
Severe aesthetic dis- comfort (2) |
120
months (NA) |
| Chow et al, J Plast Re- constru Surg, 2013 |
Case report
1 M with SUM in situ
41 |
Right T1 (1) |
SUM in situ |
Biopsy 10 mm
WLE with a layer of bone |
Immediate FTSG (harvested from the groin) |
NA |
NA |
Acceptable cosmetic result (assessed by surgeon) |
5
months |
| Duarte et al, Derma- tol, 2010 |
Case report
1 F with SUM in situ
61 |
Right F1 (1) |
SUM in situ |
Excisional biopsy 3 weeks later
3 mm margin WLE |
FTSG taken from the arm |
No local recurrence or metastasis |
NA |
Thumb function completely pre- served |
12
months |
| High et al, Arch Derma- tol, 2004 |
Retrospective
7 patients (5F, 2M) with SUM in situ
4 patients treated by WLE
MA 56 (NA) |
Right hand (1): F2
Left hand (2): F2(1), F5(1)
Right foot (1): T1(1) |
SUM in situ |
Previous biopsy MOHS surgery: 1
stage (3)
2 stages (1) |
FTSG taken from the arm (3) cross finger flap (1) |
Recurrence: (1) treated by revisional amputa- tion |
NA |
NA |
24
months (10-29) |
| Sinno et al, J Plast Surg Hand Surg, 2015 |
Retrospective
35 patients with melanoma of the hand (24F, 11M)
18 patients with SUM
10 patients with SUM treated by WLE |
F1 (8)
F2 (12)
F3(3)
F5(3) |
Melanomas in situ (7) Invasive Melanoma T2(1 pa-
tients) B=2.5mm
Invasive Melanoma T3 (2); B=3.00mm
and
B=3.08mm |
5 mm |
FTSG (3)
Paronychial advancement flap + FTSG (3) Paronychial advancement flap + forearm flap + FTSG (1)
Paronychial advancement flap + FTSG Volar Flap FTSG (1)
FTSG Volar and dorsal ad- vancement flaps (1)
FTSG Local advancement
flap (1) |
Revisional amputation (3)
Unknow (1)
Deceased (1) |
NA |
NA |
47
months (7–74) |
Smock et al, J Plast Re- constr Aesthet Surg,
2010 |
Case report 1 M
44 |
Right F1 (1) |
Ulcerated SUM Bres- low of 1.2 mm |
Previous Biopsy 10 mm, including the
periosteum |
Immediate reconstruction by dermal matrix (INTEGRA) STSG 3 weeks later |
None |
NA |
Fully functional thumb and a good cosmetic result Went back to job at 4 weeks |
24
months |
| Bjedov et al, Acta Dermato Venereol Croat, 2019 |
Case report (1)
F, 31 |
Left F1 (1) |
SUM in situ |
Several nail matrix biopsies
5 mm, with perios- teum
Mohs analysis |
Pedicled innervated Fascio cutaneous Foucher's flap Donor site was covered with a FTSG taken from the volar side of the elbow. |
None |
NA |
The hand was fully functional, and the patient was very sat- isfied with the ap- pearance of the thumb
Full sensory cortical
reorientation |
3
months |
| Oh et al, J Am Acad Derma- tol, 2023 |
Retrospective
140 patients with SUM
107 with con- servative treat- ment
(57 F, 50 H)
Mean age: 56 |
F1,2,3,4,5 (71)
T1,2,3,4,5 (36) |
If no bone invasion (MRI + bi-
opsy) |
Biopsy and MRI at least 3 to 4 mm, with periosteum |
NA |
Recurrency (23 pa- tients):
Local recurrence (15)
Distant recurrences (8) |
NA |
NA |
45
months (14- 76) |
| Motta et al, Arch Derma- tol, 2007 |
Case report 12 years old, F |
Right F1 (1) |
SUM in situ |
Biopsy
WLE with Mohs Mi- crographic analysis 5-10mm (lateral)
5 mm (proximal and
distal edges) |
Two stages
Second stage (1week later) microvascular composite on- ycho-cutaneous free flap
from the right first toe |
NA |
NA |
Normal nail growth and full mobility of the interphalangeal thumb joint were present |
3
months |
| Wollina et al, Derma- tol Ther, 2019 |
Retrospective Serie of 12 pa- tients with SUM)
6 patients with conservative treatment (2F, 4M)
76 (NA) |
Right foot T1(2)
T3 (1)
Left foot: T1 (3) |
SUM with Breslow be- tween 1.6
mm to 4.8 mm |
Wide excision (4) Excision with de- layed Mohs surgery (2) |
Full thickness skin trans- plantation.
One patient refused, second intention healing |
Local relapse (2) Later metastasis () Satellites only (1 pa- tient, B=2.55)
Liver, pancreas, spleen, lymph nodes, stomach, adrenal glands, greater omentum, CNS (1, with Breslow =4.8mm)
In transit, lymph node regional, pericardium (1, with Breslow=3.20) |
Sentinel Lymph node (4), with micro-invasion (1)
Polychemother- apy for later me- tastasis (1) Transit metasta- ses treated by er- bium YAG-laser as a palliative measure (1) interferon-alfa therapy for 9 years after sur- gery satellites metastasis (1) Adjuvant radio- therapy (1) |
NA |
104
months (17 -208) |
Crisan et al, Acad Derma- tol Ve- nereol,
2017 |
Retrospective
Serie of 7 pa- tients (3F, 4H)
64 (NA) |
F1 (3)
F4 (3)
T1 (1) |
SUM in situ
pT1a (1)
pT1b (1) |
WLE (7) NA |
First stage: vacuum-assisted closure
Second stage: FTSG (5) |
Second stage amputa- tion (2 patients) for:
-DIP joint arthritis (1)
-Positive margin (1) |
NA |
At 6 weeks, the 5 pa- tients grafted could resume normal ac- tivity
Good cosmetic and
functional |
12
months (NA) |
Lee et al, Plast Re- constr Surg,
2017 |
Prospective
41 patients with conservative |
Fingers: 25
Toes: 16 |
SUM with Breslow thickness of
≤ 2 mm on |
Preoperative biopsy 5-mm with perios- teum excise
(10 mm margin if in-
vasive lesion) |
Immediate reconstruction by SCIP flap with a final thick- ness ranging from 1.5 to 4 mm after defatting |
Necrosis of the flap (1) (arterial insufficiency) Venous congestion (3) with partial necrosis of
the flap |
NA |
Average healing time: 15 days Questionnaire car- ried out on 26 |
31
months (NA) |
| |
treatment (21M, 20F)
51.1 (NA) |
|
preoperative biopsy |
|
(Scouted with Doppler)
End to end anastomosis with digital artery and dorsal vein
Donor site primary closing |
Seroma of the donor site (1) Recurrences:
-local recurrence (1)
-metastasis in transit (1) Second surgical stage until degreasing (12) |
|
patients: WLE in the upper limb (14): The mean Quick- DASH score was 1.3 (range 0 to 6.8).
WLE in the lower limb (12): FFI survey for foot lesions, mean score was 3.1
(range 0 to 8.0) |
|
| Hayashi et al, Derma- tol Surg, 2012 |
Case report (1M), 52 |
Left F3 |
SUM in situ |
No biopsy
5 mm with excision of periosteum |
Immediate reconstruction with artificial dermis (PELNAC)
Second stage at 4 weeks with FTSG |
No recurrency No metastasis |
NA |
Good cosmetic re- sults |
3
months |
| Sureda et al, Br J Derma- tol, 2011 |
Retrospective
Serie of 7 patients (5F, 2M)
MA 58 y |
F1(2), F2(2), F4(1)
T1 (2) |
SUM in situ (5)
or minimally invasive SUM (2)
(Breslow 0.2
and 0.15) |
Biopsy systematically 5-10 mm
Deep margin was bone contact |
Immediate FTSG taken from the internal aspect of an arm |
No recurrence |
NA |
Interrogation of pa- tient and observer: High level of satis- faction, a good func- tional and quite good cosmetic re- sult. |
45
months (24-84) |
Nec- zyporen ko et al, J Eur Acad Derma- tol Ve- nereol,
2014 |
Retrospective
Serie of 11 pa- tients (8 F, 3 M)
48 (NA) |
Right hand: F1(3), F2(1), F5(1)
Left hand: F1(1) F2(1)
T1(3), T2(1) |
Melanoma in situ |
Biopsy systematically (tangential or punch) 6 mm |
Immediate FTSG (6)
Secondary intention and de- layed FTSG (5) |
Tendon sheath haema- toma (1)
Lymphangitis post (1) Recurrence treated by secondary amputation and sentinel node (2) (7- and 11-years post op) |
NA |
Healing by second- ary intention and grafting were fully satisfactory, cosmet- ically and function- ally |
65
months (5-167) |
| Terush- kin et al, Derma- tol Surg, 2016 |
Retrospective
Serie of 40 pa- tients (21 F,19M)
63 (NA) |
NA |
WLE in cases of ex- tensive SUM (>40%
of the bed) |
Excisional biopsy with Mohs micro- graph,
Supra Periosteum dissection |
Second intention FTSG STSG |
Recurrences (5) Second operation with com- plete excision of the ma- trix (2) Amputation (2) Death due to metastasis
(1) |
NA |
NA |
76
months (2-276) |
| Rayatt et al, Plast Reconstr Aesthet Surg, 2007 |
Retrospective
Serie of 4 pa- tients
56 (NA) |
F1 (4) |
SUM with- out deep margin clini- cally in- volved
Breslow
0.9m m to 4mm |
All had initial biop- sies to confirm the di- agnosis
10 mm including the periosteum |
Immediate:
-Foucher flap (1)
-Flag flap (2)
Delayed reconstruction (flag flap) (1) |
Recurrence at 36 months treated by am- putation (1) |
NA |
Usefully maintain function. |
72
months (-117) |
| Imakado et al, J Derma- tol, 2008 |
Retrospective
Serie of 2 pa- tients (1M, 1F)
50 |
Left F3 (1) Right F5(1) |
SUM in situ |
All the nail apparatus with nail folds |
Immediate FTSG |
No recurrence |
NA |
NA |
27
months (6 -48) |
| Liu et al, Medic- ina, 2020 |
Retrospective
Serie of 4 patients with malignant tumour of nail apparatus
3 patients with SUM suspicion (1F, 2M)
MA 55 y |
Left T1 (1)
Right T1 (2) |
SUM in situ (2)
hyperpig- mentation in basal layer of epidermis (1) |
Previous biopsy (2) WLE
Adequate margin control confirmed by intraoperative frozen sections |
Two stages reconstruction Immediate acellular dermal matrix (PELNAC)
At 10 days, the acellular der- mal matrix was removed and re-dressed in a new one at the outpatient clinic
FTSG at 3 weeks |
No Recurrence |
NA |
These patients expe- rienced minimal change in body con- tour, mild but ac- ceptable functional deficit, and satisfy- ing aesthetic results. |
9
months (5-13) |
Retrospective Monocentric Study of a Series of Patient
Population Characteristics
A total of ten patients with an average age of 62.4 ± 10.8 years (48 to 80) were included.
Seven were retired and three were working. There were no active smokers in our study, and the main comorbidities were arterial hypertension in three patients, type 2 diabetes in one, and obstructive lung disease in one patient who had stopped smoking. The mean follow-up period was 18 ± 7.1 months (7 to 29). Six cases involved involvement of the upper limb, including four of the thumbs and two of the long fingers, and four cases involved involvement of the lower limb, including three of the halluces and one of the second toe. There were seven cases of in situ melanoma and three cases of invasive melanoma, two of which were identified during the preoperative biopsy. The depth of the Breslow index reported after the operation was 0.9 ± 0.21 mm on average (0.7 to 1.2), for the invasive melanomas. Two cases involved margins affected after extended excision of the nail apparatus, treated respectively by amputation of the digit concerned and by re-doing the margins during the second stage of reconstruction, without additional treatment.
Per-Operative Data
A total of ten patients with an average age of 62.4 ± 10.8 years (48 to 80) were included. Seven were retired and three were working. There were no active smokers in our study, and the main comorbidities were arterial hypertension in three patients, type 2 diabetes in one, and obstructive lung disease in one patient who had stopped smoking. The mean follow-up period was 18 ± 7.1 months (7 to 29). Six cases involved involvement of the upper limb, including four of the thumbs and two of the long fingers, and four cases involved involvement of the lower limb, including three of the halluces and one of the second toe. There were seven cases of in situ melanoma and three cases of invasive melanoma, two of which were identified during the preoperative biopsy. The depth of the Breslow index reported after the operation was 0.9 ± 0.21 mm on average (0.7 to 1.2), for the invasive melanomas. Two cases involved margins affected after extended excision of the nail apparatus, treated respectively by amputation of the digit concerned and by re-doing the margins during the second stage of reconstruction, without additional treatment.
Post-Operative Data
From a carcinologic point of view, two patients had positive margins after WLE, one of whom was successfully treated by re-doing the margins during the second stage of reconstruction, and one of whom had the digit concerned amputated in the month following WLE and died because of metastatic dissemination of the disease.
No major post-operative complications were reported, and no emergency surgery was required. The main complications were late complications, such as hypoesthesia with difficulty in using the forceps in one case, but above all hyperesthesia to contact (two cases) and to temperature variations, with acro-vascular phenomena in patients with upper limb disease. One patient (case 10) presented with a nail spicule at the surgical site, which interfered with footwear and was taken back for the excision of this remnant.
Hyperpigmentation of the graft was observed in only one case, which had undergone a two-stage reconstruction with a dermal matrix followed by a total skin graft.
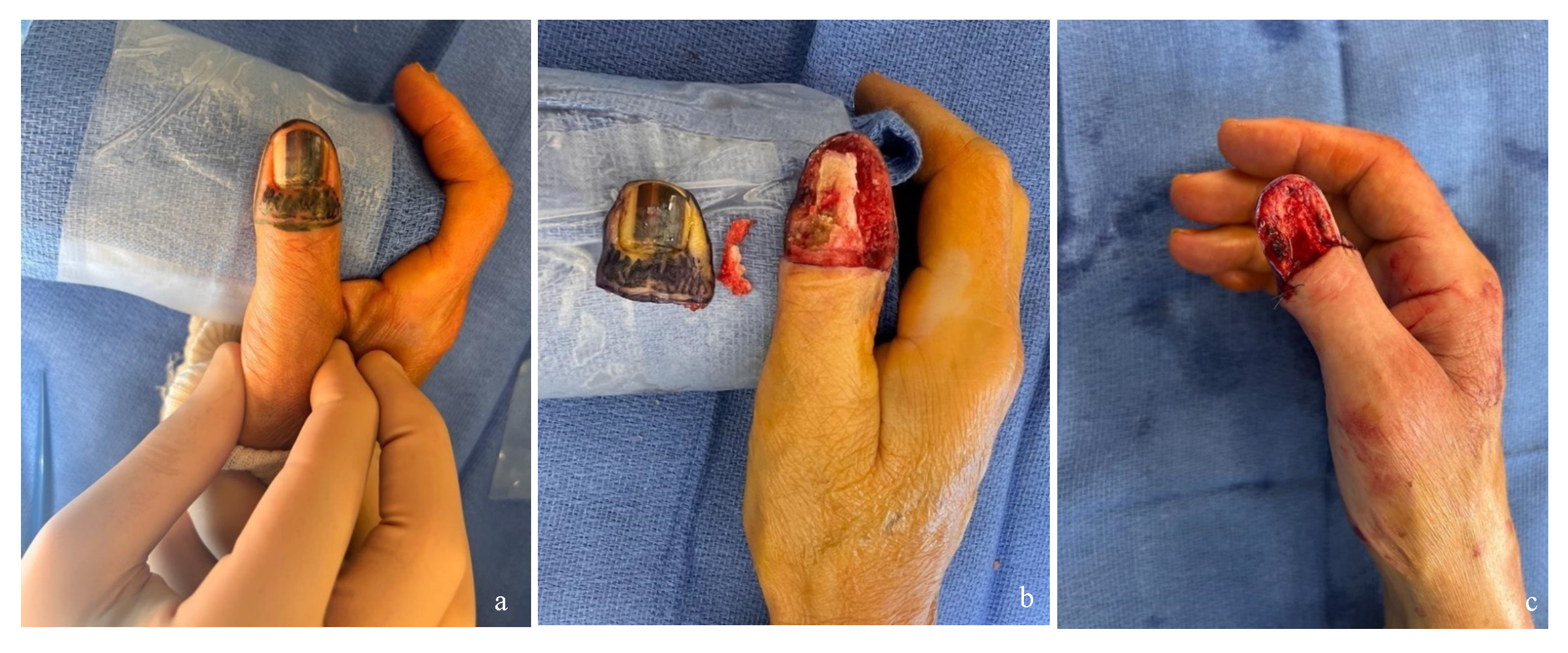
Figure 2.
Photographs of the dorsal surface of thumbs with SUM, treated with WLE, from our series. a. Intraoperative view before WLE. b, c. Intraoperative views after WLE, illustrating the extent of the soft tissue defect.
Figure 2.
Photographs of the dorsal surface of thumbs with SUM, treated with WLE, from our series. a. Intraoperative view before WLE. b, c. Intraoperative views after WLE, illustrating the extent of the soft tissue defect.
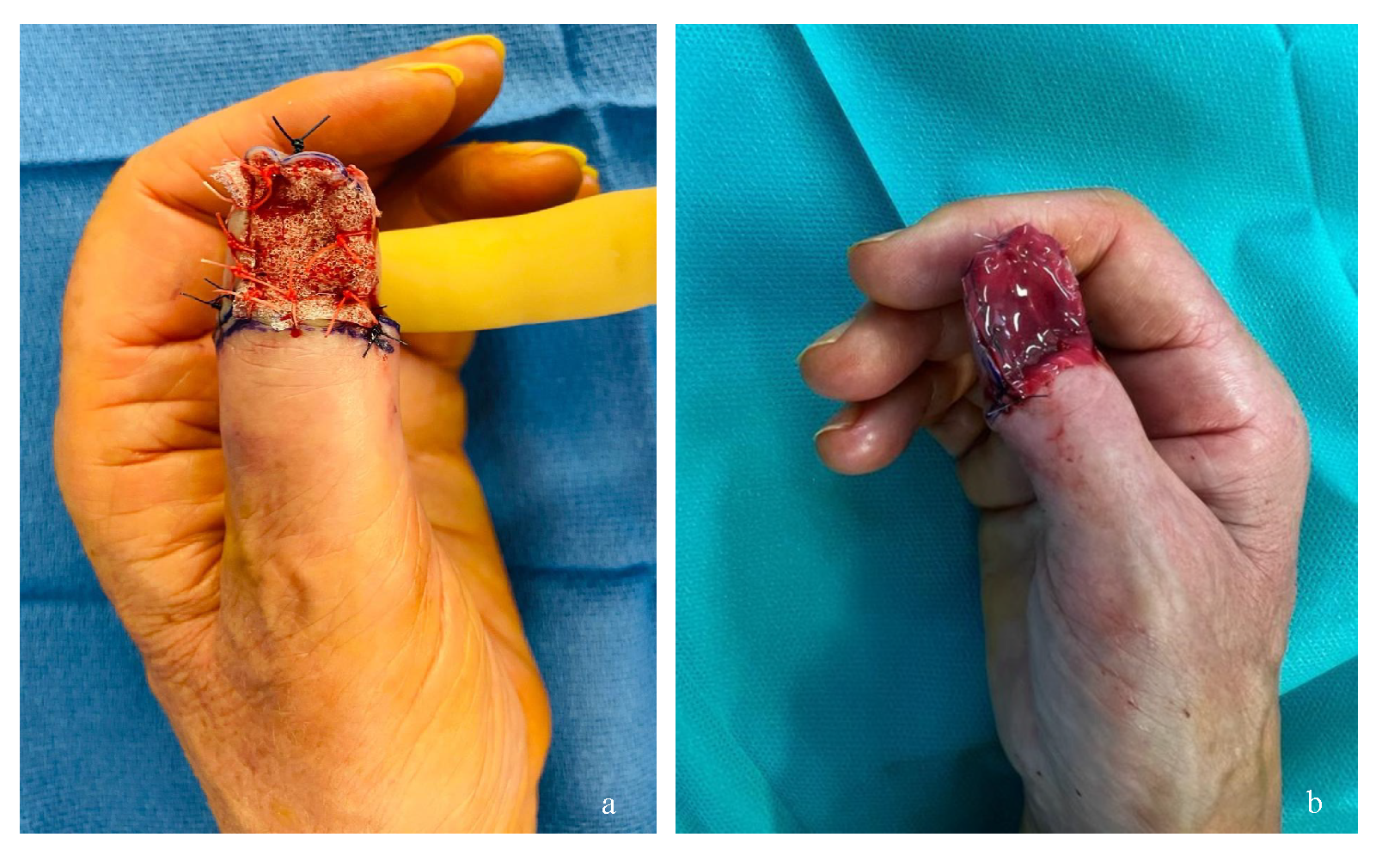
Figure 3.
Photographs of the dorsal aspect of thumbs in patients with SUM, treated with WLE and reconstructed using dermal matrices. a. Intraoperative view after WLE and placement of a fixed dermal matrix (Novosorb BTM). b. Intraoperative view after WLE and placement of a fixed dermal matrix (INTEGRA).
Figure 3.
Photographs of the dorsal aspect of thumbs in patients with SUM, treated with WLE and reconstructed using dermal matrices. a. Intraoperative view after WLE and placement of a fixed dermal matrix (Novosorb BTM). b. Intraoperative view after WLE and placement of a fixed dermal matrix (INTEGRA).
Figure 4.
Photographs of the dorsal surface of the right thumb and index finger treated by WLE in our series. a. Photographs of the right thumb reconstructed with dermal matrix and FTSG, with secondary hyperpigmentation of the graft. b. Photographs of the right index finger reconstructed with a distal pedicle adipofascial flap.
Figure 4.
Photographs of the dorsal surface of the right thumb and index finger treated by WLE in our series. a. Photographs of the right thumb reconstructed with dermal matrix and FTSG, with secondary hyperpigmentation of the graft. b. Photographs of the right index finger reconstructed with a distal pedicle adipofascial flap.
Figure 5.
Photographs of the dorsal aspect of the left foot in a patient with SUM of the hallux treated with WLE and reconstructed with an intermetatarsal pedicled flap from the first space. a. Preoperative: flap design based on the perforator of the first dorsal metacarpal artery in the first space. b. Intraoperative views after WLE, illustrating the extent of soft tissue defect. c. Aspect at 2 days post-operatively.
Figure 5.
Photographs of the dorsal aspect of the left foot in a patient with SUM of the hallux treated with WLE and reconstructed with an intermetatarsal pedicled flap from the first space. a. Preoperative: flap design based on the perforator of the first dorsal metacarpal artery in the first space. b. Intraoperative views after WLE, illustrating the extent of soft tissue defect. c. Aspect at 2 days post-operatively.
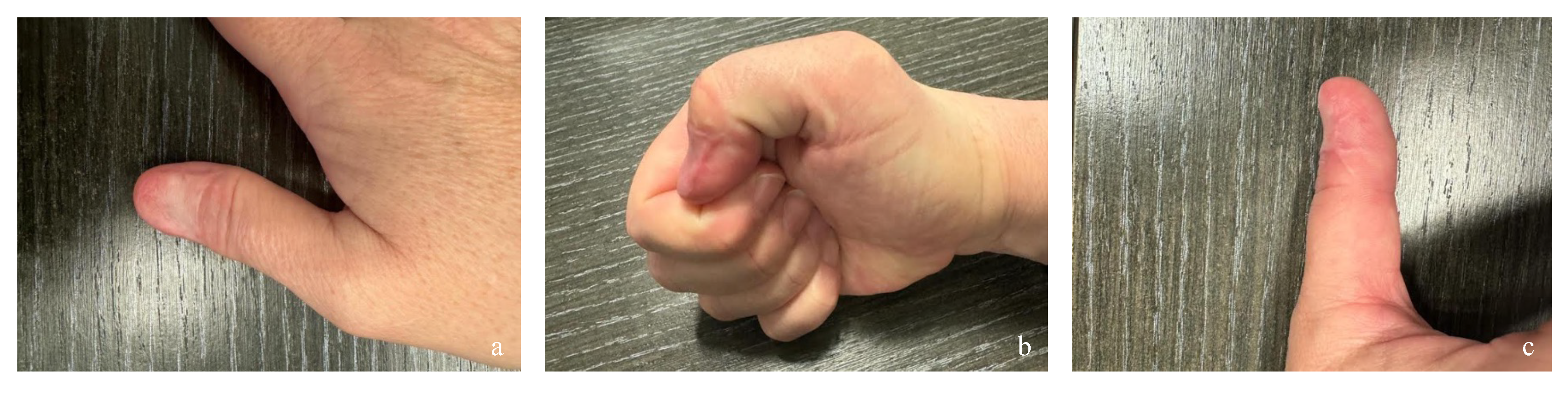
Figure 6.
Photographs of the dorsal aspect of thumbs in SUM patients treated with WLE and reconstructed with dermal matrices and FTSG in our series. a. Dorsal view. b. Radial edge view. c. Ulnar edge view.
Figure 6.
Photographs of the dorsal aspect of thumbs in SUM patients treated with WLE and reconstructed with dermal matrices and FTSG in our series. a. Dorsal view. b. Radial edge view. c. Ulnar edge view.
Regarding the objective of functional and cosmetic recovery, of the 9 patients who underwent functional surgery, 7 completed the questionnaire after an average of 19.2. There were 4 cases with lesions on the fingers and 3 on the toes. The mean Quick-DASH score was 25.5 ± 16.4 (2.3 to 41) (score ranging from 0, no handicap, to 100, maximum handicap) and concerned two patients reconstructed by matrix and total skin graft, with scores of 18 and 41 respectively, one patient reconstructed by adipo-fascial flap with distal pedicle, with a score of 2.3 and one patient reconstructed by FTSG alone, with a score of 41. The Modified Mayo Wrist Score (score ranging from 0, maximum disability, to 100, no disability) averaged 78.5 ± 4.8 (75 to 85), respectively 75 and 85 for the two cases of reconstruction by dermal matrix and FTSG, 75 for the case of reconstruction by distal pedicle adipofascial flap and 80 for the case of reconstruction by FTSG alone.
Finally, for cases with foot lesions, the mean AOFAS score was 86 ± 4.1 (80 to 90) (score ranging from 0, maximum disability, to 90, no disability). Details of the results are given in
Table 2.
4. Discussion
The management of subungual melanoma has evolved significantly since it was first described in the nineteenth century ((37). This topographical form seems to preferentially affect women, as shown by our review (67% of the 24 articles included were female), in line with the data of Neczyporenko et al (24).
Regarding the age of onset, the fifth decade is the most frequently reported, with a few exceptions such as the series by Lazar et al. (14), where the mean age was 40. Preoperative biopsy is not usually recommended for pigmented skin lesions, in favor of excisional biopsy (38). However, in certain functional or aesthetically sensitive areas, a biopsy may be justified as a first-line procedure. In our review, several studies did not specify the performance of a biopsy and its modality, or mentioned the absence of one, which exposes the risk of unnecessary mutilating surgery, even in the presence of effective reconstruction techniques. EAU is now preferred to amputation in cases of in situ or minimally invasive melanoma, although there is no agreed Breslow threshold (39, 40). Most articles support this strategy, with a recurrence rate comparable to that of amputation (14, 17, 26, 41, 42). Although some studies report more local recurrences after WLE, often after the operation, it should be remembered that this technique is aimed at less aggressive tumors, without metastatic disease. Furthermore, anatomopathological control may be incomplete, as pointed out by Kimyai-Asaidi et al. (43). This also explains why sentinel lymph nodes are rarely used in these cases. Conversely, amputations are reserved for more advanced forms, with a higher metastatic potential.
There is no clear consensus regarding immediate versus delayed reconstruction. Our literature review revealed a notable rate of local recurrence: 67 out of 373 patients (ap- 428 proximately 18%) experienced recurrence, most often requiring secondary amputation. Reported cases of amputation following histological analysis of the resection specimen—including two in our series and two in the literature—further support the rationale for delayed reconstruction, particularly in cases of invasive melanoma.
Two techniques have been proposed for margin assessment: intraoperative frozen section analysis, which is limited by the absence of specific immunostains (such as MART-1, HMB-45), and the Mohs micrographic surgery technique, either conventional or staged. While Mohs is not recommended as a standard treatment for melanoma, it is employed in certain specific cases, particularly for lentigo maligna (Dubreuilh's melanoma) (18, 57-59). It allows more precise histological control, but its accessibility remains limited and its efficacy in this context is still debated. Most articles support this strategy, with a recurrence rate comparable to that of amputation (28, 31, 40, 54, 55). Although some studies report more local recurrences after WLE, often after the operation, it should be remem- 441 bered that this technique is aimed at less aggressive tumors without metastatic disease. Furthermore, anatomopathological control may be incomplete, as pointed out by Kimyai-Asaidi et al (56). This also explains why sentinel lymph nodes are rarely used in these cases. Conversely, amputations are reserved for more advanced forms, with a higher metastatic potential.
Reconstruction approaches vary total skin grafts, dermal matrices, pedicled or free flaps. The choice depends on the location, the functional importance of the finger or toe, the need for mechanical strength or, on the contrary, aesthetic requirements. Free flaps or flaps with a temporary pedicle (flag flap type) may be too invasive for certain indications, whereas a graft combined with a dermal matrix is often a good compromise, especially for distal injuries with poor function. The inner arm is often used as a donor site, due to its hairless and discreet appearance. Dermal matrices provide post-operative comfort (less hypersensitivity) and allow coverage of ex-posed bone, enabling WLE with sub-periosteal resection or removal of the dorsal cortex of the last phalanx, although they require additional operating time. These approaches remain eligible for outpatient surgery under lo- 456 coregional anesthesia.
In our review, most of the reconstruction techniques described were based on skin grafting, alone or in association with a matrix or local flap, which could be explained by the low logistical and organizational constraints of this procedure, the quality of the results it provides, its simplicity of execution and its independence in relation to the size of the recipient site. Although a single surgical procedure is the most ergonomic option, our review found a similar number of one-stage and two-stage procedures. The latter, sometimes due to the time required to incorporate the matrix, could be dispensed with the advent of single-layer matrices. As for the functional and cosmetic results mentioned in our review, they were often judged as “good”, “acceptable” or “satisfactory”, which unfortunately made interpretation difficult and subjective. Objective results, at best reported by the patient using validated scores, would enable an effective comparison of the different techniques for a given patient profile.
In our experience, reconstruction should be adapted as far as possible to the patient's profile. However, for damage to the upper limb, the combination of a dermal matrix and a total skin graft seems to us to be the most suitable technique, due to the quality of the functional and cosmetic result. Indeed, the advantages of skin grafts, which are sensitive and dyschromic, contrast with the rest of the dorsal skin of the digit, combined with those of skin thickness restored by matrices, such as reducing the risk of hypersensitivity. The safety, simplicity and speed of the procedure mean that we can offer it as first-line treatment for most of our patients. For lower limb injuries, pedicled flaps, such as the intermetatarsal flap, are effective reconstructions. Sensitivity and aesthetics in this area are of- 478 ten secondary to the need for a final toe phalanx with maximum protection against hyper-sensitivity and pain, which is the case with thick skin coverings such as flaps. One of the disadvantages of this technique is the presence of a dorsal scar along the length of the digit and the commissural space removed, which is why we propose reconstruction by skin graft with dermal matrix as an alternative option.
Neoadjuvant immunotherapy, already used for resectable stage III melanoma, could represent a turning point for localized forms such as SUM (44). In the long term, it could make it possible to avoid certain amputations in favor of more conservative surgery such as WLE. However, these therapeutic options have not been widely studied, reflecting the persistent compartmentalization between medical and surgical disciplines.
The main limitations of our review are related to the lack of standardized functional evaluation of reconstructions, the heterogeneity of the techniques used, and the absence of precise data on histological stage. Our case series, although limited, is consistent with these observations. Prospective, multicenter studies with validated functional scores are needed to better define indications and optimize results.
5. Conclusions
The management of subungual melanoma is tending more and more towards WLE rather than amputation, particularly in situ forms or those with a low Breslow index.
Reconstructive techniques, such as total skin grafts or the use of dermal matrices, provide satisfactory functional and aesthetic results. However, objective assessments of these results remain limited, and adjuvant treatments such as radiotherapy or immunotherapy are rarely mentioned. Better standardization of practices and prospective studies are needed to refine the evaluation of long-term results.
Author Contributions
Conceptualization, O.C. and E.L.; methodology, E.L, O.C.; software, L.C.; validation, O.C., F.B. and E.L.; formal analysis, E.L, L.C.; investigation, L.C; resources, E.L, T.B., F.B, H.M..; data curation, L.C.; writing—original draft preparation, L.C..; writing—review and editing, E.L., O.C., T.B, H.M. visualization, O.C, E.L., F.B.; supervision, O.C, E.L., T.B.; project administration, O.C, E.L. T.B, H.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This research project has been approved by the institutional ethics committee (n°IRB00014528_2025_14).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be provided by the corresponding authors on demand.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| SUM |
Subungueal melanoma |
| WLE |
Wide local excision (of nail apparatus) |
| F |
Finger |
| T |
Toe |
| FTSG |
Full thickness skin graft |
| STSG |
Split thickness skin graft |
| NA |
Non available |
| COPD |
Chronic obstructive pulmonary disease |
| ScoreQuick DASH |
score Quick Disabilities of the arm, shoulder and hand, (score ranges from 0, no obstacles to 100, maximum obstacles) |
| MMWS |
score ranging from 0, maximum disability, to 100, no disability |
| Score AO- FAS |
the American Orthopedic Foot and Ankle Score (score ranging from 0, maximum disability, to 90, no disability) |
References
- Cancer IAfRo. https://gco.iarc.who.int/today/ 2022.
- Breslow A. Tumor thickness in evaluating prognosis of cutaneous melanoma. Ann Surg. 1978;187(4):440.
- Feibleman CE, Stoll H, Maize JC. Melanomas of the palm, sole, and nailbed: a clinicopathologic study. Cancer 1980;46(11):2492-504.
- Brodland DG. The treatment of nail apparatus melanoma with Mohs micrographic surgery. Dermatol Surg. 2001;27(3):269-73.
- Haneke, E. Ungual melanoma - controversies in diagnosis and treatment. Dermatol Ther. 2012;25(6):510-24.
- Nakamura Y, Ohara K, Kishi A, Teramoto Y, Sato S, Fujisawa Y, et al. Effects of non-amputative wide local excision on the local control and prognosis of in situ and invasive subungual melanoma. J Dermatol. 2015;42(9):861-6.
- Cochran AM, Buchanan PJ, Bueno RA, Jr., Neumeister MW. Subungual melanoma: a review of current treatment. Plast Reconstr Surg. 2014;134(2):259-73.
- Temple-Oberle C, Nicholas C, Rojas-Garcia P. Current Controversies in Melanoma Treatment. Plast Reconstr Surg. 2023;151(3):495e-505e.
- Baran R G-BSMI, Robert C. Traitement du mélanome de l’appareil unguéal. Annales de Dermatologie et de Vénéréologie. 2021;Vol 1 - N° 2:P. 128-32.
- Hovgaard C, Angermann P, Hovgaard D. The social and economic consequences of finger amputations. Acta Orthop Scand. 1994;65(3):347-8.
- Poumellec MA, Camuzard O, Dumontier C. Hook nail deformity. Hand Surg Rehabil. 2024;43s:101649.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372:n71.
- Anda-Juárez MC, Martínez-Velasco MA, Fonte-Ávalos V, Toussaint-Caire S, Domínguez-Cherit J. Conservative surgical management of in situ subungual melanoma: long-term follow-up. An Bras Dermatol. 2016;91(6):846-8.
- Lazar A, Abimelec P, Dumontier C. Full thickness skin graft for nail unit reconstruction. J Hand Surg Br. 2005;30(2):194-8.
- Puhaindran ME, Cordeiro PG, Disa JJ, Mehrara BJ, Athanasian EA. Full-thickness skin graft after nail complex resection for malignant tumors. Tech Hand Up Extrem Surg. 2011;15(2):84-6.
- Flores-Terry M, Romero-Aguilera G, Mendoza C, Franco M, Cortina P, Garcia-Arpa M, et al. Functional Surgery for Malignant Subungual Tumors: A Case Series and Literature Review. Actas Dermosifiliogr (Engl Ed). 2018;109(8):712-21.
- Moehrle M, Metzger S, Schippert W, Garbe C, Rassner G, Breuninger H. "Functional" surgery in subungual melanoma. Dermatol Surg. 2003;29(4):366-74.
- Goettmann S, Moulonguet I, Zaraa I. In situ nail unit melanoma: epidemiological and clinic-pathologic features with conservative treatment and long-term follow-up. J Eur Acad Dermatol Venereol. 2018;32(12):2300-6.
- Sinno S, Wilson S, Billig J, Shapiro R, Choi M. Primary melanoma of the hand: An algorithmic approach to surgical management. J Plast Surg Hand Surg. 2015;49(6):339-45.
- Oh BH, Lee S, Park JW, Lee JY, Roh MR, Nam KA, et al. Risk of recurrence of nail unit melanoma after functional surgery versus amputation. J Am Acad Dermatol. 2023;88(5):1017-23.
- Wollina U, Tempel S, Hansel G. Subungual melanoma: A single center series from Dresden. Dermatol Ther. 2019;32(5):e13032.
- Lee KT, Park BY, Kim EJ, Kim JH, Jang KT, Choi SH, et al. Superthin SCIP Flap for Reconstruction of Subungual Melanoma: Aesthetic Functional Surgery. Plast Reconstr Surg. 2017;140(6):1278-89.
- Sureda N, Phan A, Poulalhon N, Balme B, Dalle S, Thomas L. Conservative surgical management of subungual (matrix derived) melanoma: report of seven cases and literature review. Br J Dermatol. 2011;165(4):852-8.
- Neczyporenko F, André J, Torosian K, Theunis A, Richert B. Management of in situ melanoma of the nail apparatus with functional surgery: report of 11 cases and review of the literature. J Eur Acad Dermatol Venereol. 2014;28(5):550-7.
- Terushkin V, Brodland DG, Sharon DJ, Zitelli JA. Digit-Sparing Mohs Surgery for Melanoma. Dermatol Surg. 2016;42(1):83-93.
- Rayatt SS, Dancey AL, Davison PM. Thumb subungual melanoma: is amputation necessary? J Plast Reconstr Aesthet Surg. 2007;60(6):635-8.
- Imakado S, Sato H, Hamada K. Two cases of subungual melanoma in situ. J Dermatol. 2008;35(11):754-8.
- Liu TH, Hsieh MC, Chou PR, Huang SH. Reconstruction for Defects of Total Nail Bed and Germinal Matrix Loss with Acellular Dermal Matrix Coverage and Subsequently Skin Graft. Medicina (Kaunas). 2020;56(1).
- Crisan D, Gülke J, Janetzko C, Kastler S, Treiber N, Scharffetter-Kochanek K, et al. Digit preserving surgery of subungual melanoma: a case series using vacuum assisted closure and full-thickness skin grafting. J Eur Acad Dermatol Venereol. 2017;31(12):e537-e8.
- High WA, Quirey RA, Guillén DR, Munõz G, Taylor RS. Presentation, histopathologic findings, and clinical outcomes in 7 nail unit. Arch Dermatol. 2004;140(9):1102-6.
- Chow WT, Bhat W, Magdub S, Orlando A. In situ subungual melanoma: digit salvaging clearance. J Plast Reconstr Aesthet Surg. 2013;66(2):274-6.
- Duarte AF, Correia O, Barros AM, Azevedo R, Haneke E. Nail matrix melanoma in situ: conservative surgical management. Dermatology. 2010;220(2):173-5.
- Smock ED, Barabas AG, Geh JL. Reconstruction of a thumb defect with Integra following wide local excision of a subungual melanoma. J Plast Reconstr Aesthet Surg. 2010;63(1):e36-7.
- Bjedov S, Ježić I, Bulić K. Reconstruction of a Thumb Defect Following Subungual Melanoma Resection Using Foucher's Flap. Acta Dermatovenerol Croat. 2019;27(1):51-2.
- Motta A, López C, Acosta A, Peñaranda C. Subungual melanoma in situ in a Hispanic girl treated with functional resection and reconstruction with onychocutaneous toe free flap. Arch Dermatol. 2007;143(12):1600-2.
- Hayashi K, Uhara H, Koga H, Okuyama R, Saida T. Surgical treatment of nail apparatus melanoma in situ: the use of artificial dermis in reconstruction. Dermatol Surg. 2012;38(4):692-4.
- A. B. A fungus hematode du petit doigt. Gaz Med. 1834;1834:212.
- Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol. 2000;42(2 Pt 1):269-74.
- Tran KT, Wright NA, Cockerell CJ. Biopsy of the pigmented lesion--when and how. J Am Acad Dermatol. 2008;59(5):852-71.
- Guillot B, Dalac S, Denis MG, Dupuy A, Emile JF, De La Fouchardiere A, et al. French updated recommendations in Stage I to III melanoma treatment and management. J Eur Acad Dermatol Venereol. 2017;31(4):594-602.
- Park KG, Blessing K, Kernohan NM. Surgical aspects of subungual malignant melanomas. The Scottish Melanoma Group. Ann Surg. 1992;216(6):692-5.
- Jo G, Cho SI, Choi S, Mun JH. Functional surgery versus amputation for in situ or minimally invasive nail melanoma: A meta-analysis. J Am Acad Dermatol. 2019;81(4):917-22.
- Kimyai-Asadi A, Katz T, Goldberg LH, Ayala GB, Wang SQ, Vujevich JJ, et al. Margin involvement after the excision of melanoma in situ: the need for complete en face examination of the surgical margins. Dermatol Surg. 2007;33(12):1434-9; discussion 9-41.
- Blank CU, Lucas MW, Scolyer RA, van de Wiel BA, Menzies AM, Lopez-Yurda M, et al. Neoadjuvant Nivolumab and Ipilimumab in Resectable Stage III Melanoma. N Engl J Med. 2024;391(18):1696-708.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).