Introduction
Sports injuries can occur during competitive or recreational physical activity (PA), usually through falls or cardiovascular collapse. Regular PA also has many benefits, such as lower rates of obesity, heart disease and a better quality of life. Adults are usually encouraged to be physically active on most days of the week to better achieve the expected health benefits of regular exercise [
1]. The United Kingdom Chief Medical Officers’ Physical Activity Guidelines and the American College of Sports Medicine (ACSM) recommend 150 minutes of moderate-intensity aerobic exercise and 2 or more days per week of strengthening activity for adults and the elderly and 60 minutes of moderate / vigorous activity a day for children [
2,
3]. For Asian populations, modifications of such PA requirements have been proposed [
4]. The World Health Organisation (WHO) recommends at least 150-300 minutes of moderate-intensity PA weekly [
5].
To promote early identification of persons prone to injuries, pre-participation screening systems have been suggested for use by those wishing to participate in moderate or intense exercise or increase their level of PA [
6,
7]. These are intended to identify individuals with a likely risk for sudden cardiac death (SCD) or other major injury. Such at-risk individuals should require medical evaluation before being cleared for a PA program. One such system, when applied to adults over 40 years old, resulted in nearly 95 percent of those in that age group being referred to a physician before engaging in any form of exercise [
8,
9]. Refinement of preparticipation screening procedures in 2015 resulted in an approximately 41% decrease in the proportion of such referrals [
10].
In Singapore, over the years, different pre-participation questionnaires have been suggested by the Sports Safety Committee, beginning in 2007 with the Physical Activity Readiness Questionnaire (PAR-Q) followed by the Get Active Questionnaire (GAQ) in 2019 [
6,
7,
11,
12,
13]. However, concern has been expressed about the complexity and difficulty in self-administering these tools and that it did not address the occurrence of heat-related injuries for those exercising in hot and humid environments [
14,
15,
16].
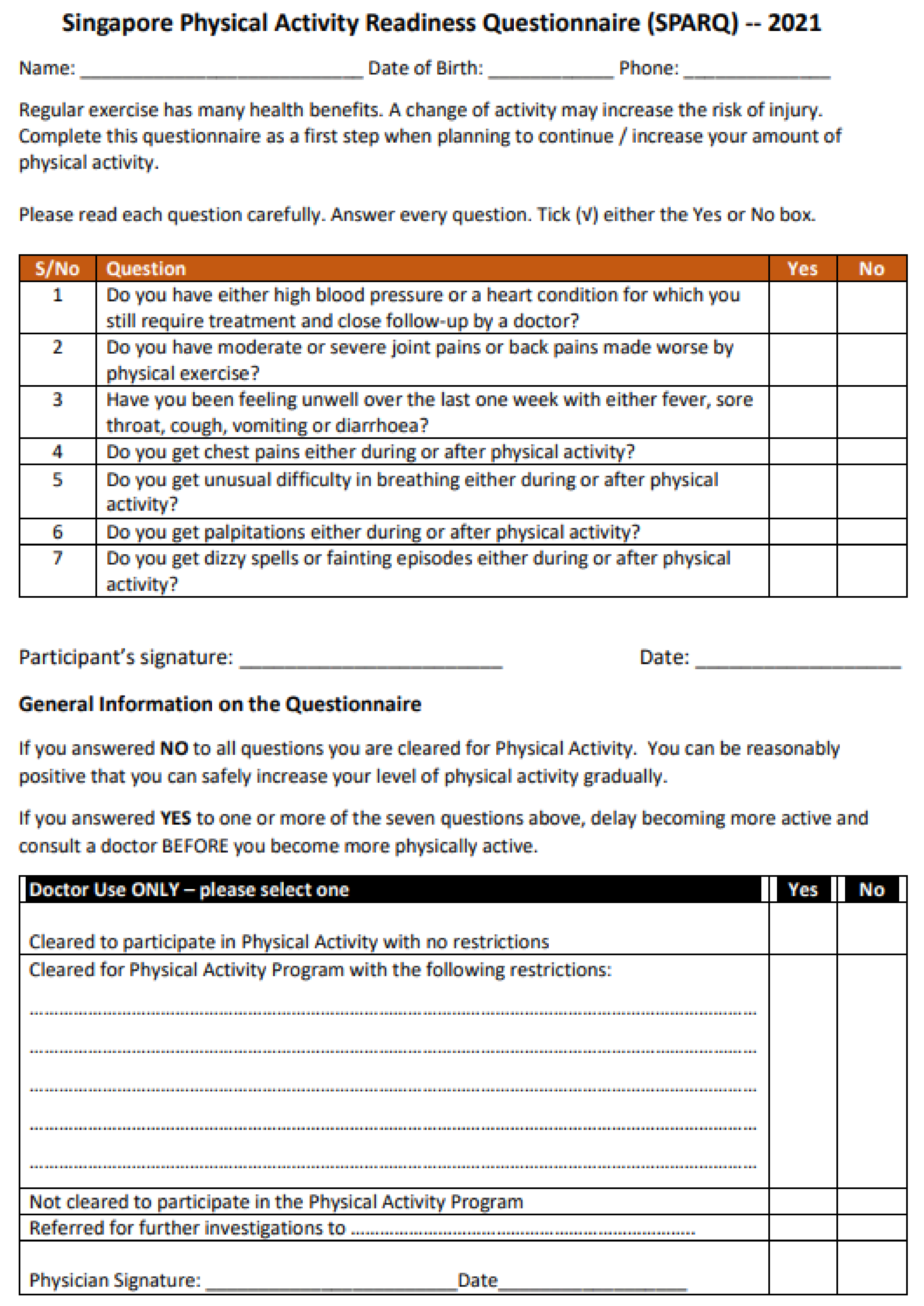
To address these concerns, the authors drafted a fresh pre-participation questionnaire for members of the public. Provisionally named as the Singapore Physical Activity Readiness Questionnaire 2021 (SPARQ –
Figure 1), this document had seven questions, each needing either a Yes or No answer. A Yes answer to any of the seven questions would suggest the participant is unfit for PA and require further medical evaluation.
The first question was “Do you have either high blood pressure or a heart condition for which you still require treatment and close follow-up by a doctor?”. This was intended to address those whose high blood pressure or heart conditions were not well controlled, potentially increasing the risk of cardiac arrest if they were to increase their exercise intensity.
The second question “Do you have moderate or severe joint pains made worse by physical exercise?” was to identify those with disabling symptoms that were likely aggravated by increasing PA or made one prone to injury.
The third question on “Have you been feeling unwell over the last one week with either fever, sore throat, cough, vomiting or diarrhoea?” was to address those acutely unwell and more prone to heat-related injuries.
The fourth question “Do you get chest pains either during or after physical activity?” was to identify those with anginal symptoms requiring further evaluation and stabilization before being advised on PA. This was to facilitate early identification of sudden cardiac arrest-prone individuals.
The fifth question “Do you get unusual difficulty in breathing either during or after physical activity?” was to identify those with either critical lung or coronary artery disease with likelihood of collapse during PA.
The sixth question on “Do you get palpitations either during or after physical activity?” was for those who felt their heart beating faster than with similar previous PA. Palpitations had previously been identified as one of the symptoms felt by some who collapsed during PA [
15].
The seventh question on “Do you get dizzy spells or fainting episodes either during or after physical activity?” was owing to similar previous reports [
17].
The primary objective of this study was to determine the level of difficulty in understanding of the SPARQ questions by members of the public. Secondary objectives were to determine the rate of persons declared unfit, if using the tool, and hence identify adults requiring further medical evaluation prior to participating in moderate or intensive PA, and obtain feedback on these questions.
Methods
This was a cross-sectional study on the use of the SPARQ. It was conducted as an anonymised public survey over a three-month period via an online platform SoGo Survey, marketed by qualtricsTM. Participation was voluntary and open to any member of the public 21 years of age and above. The study was publicised through governmental agencies, community grassroot and national sports agencies, professional societies and institutes of higher learning.
Prior to survey participation, respondents were provided with basic information regarding the need for a self-administered pre-participation screening tool to identify persons at greater risk of adverse events during PA. Once formal consent was obtained, participants completed the three sections of the survey.
One section collected demographic information (age, sex, height, weight, ethnic group, smoking history and frequency of PA). The second was the SPARQ itself. The third was a survey on difficulty of understanding each of the seven questions, the use of technical terms and the length of the questionnaire. Feedback was on a 5-point Likert scale. Participants were also asked for comments and suggestions on information included in the questionnaire, and their preferred frequency for completing the SPARQ.
Three participant sub-groups were created based on age. The study was powered to show a 10% difference in mean values between these sub-groups with a standard deviation of 25% using α = 0.50 and p = 0.05. This required a minimum number of 293 participants for each age-group in the study. Additionally, an incomplete survey response of at least 10% was expected. Hence, the minimum number was multiplied by 3 (for a total of 879) and raised to 1000.
The study was approved by the Institution Review Board of the Singapore Sports Institute (Approval Number SSG-EXP-002).
Data Analysis
The collected data was anonymised and automatically compiled into a Microsoft Excel database. Statistical analysis was carried out using IBP SPSS Statistics 21.
To conduct comparative analyses, respondents were categorized into three age groups (21-39.9 years, 40-59.9 years, and ≥60 years). Respondents' BMI and weekly PA were also grouped into five BMI categories (according to the WHO-proposed Asian BMI scale) and four PA groups (<150 minutes, 150–299 minutes, 300–449 minutes, and ≥450 minutes per week) [
18].
Descriptive statistics were applied to summarize nominal and ordinal data. Non-parametric comparisons of independent samples were conducted using the Kruskal-Wallis test, Mann-Whitney U test, and Chi-square tests, as appropriate. Parametric data comparisons were performed using t-tests and ANOVA
Feedback on SPARQ Data
In reviewing the responses from study participants, the authors considered satisficing in potentially influencing feedback results. Five types of satisficing behaviours were looked for amongst the survey respondents, viz. primary bias, acquiescence bias, early termination, non-response and straight-lining. Satisficing analysis was done using methods suggested by Barge, Vriesema and Gehlbach [
19,
20]. The apparently satisficed data were removed from the feedback analysis and, owing to lack of universally-agreed definitions of difficulty in understanding when attempting such questions, the means of the Likert scores were arbitrarily divided into four groups of levels of difficulty as shown below:
| Difficulty Likert Index |
Level of Difficulty |
| > 4.51 |
No Difficulty |
| 4.01 – 4.50 |
Slight Difficulty |
| 3.51 – 4.00 |
Moderate Difficulty |
| < 3.50 |
Significant Difficulty |
Free-text comments were also collected and grouped for possible feedback on future refinements of the questions.
Results
A total of 1137 persons participated in this study. One was under 21 years of age. No participants needed to be excluded from analysis for extensively incomplete data. Analysis was based on the remaining 1136 respondents.
Participant Characteristics (Table 1)
Males formed 56.5% of respondents and were older than females. The ethnic breakdown of the participants was generally similar to the population of Singapore. The BMI was lower in the 21-39.9 and >60 years age-groups compared to those between 40 – 59.9 years age (24.2 and 23.6 vs 24.7, p=0.001). About 23.8% had at least one illness. Of these 18.5% had only one co-morbidity. Overall, 9.0% had hypertension, 4.8% dyslipidemia, 2.2% heart disease, 0.4% cancer, 3.3% diabetes mellitus and 9.7% had other illnesses. Persons with known medical illnesses were, generally older than those without.
Only 52.6% of respondents reported exercising for at least 150 minutes per week. Those > 60 years of age spent more time on PA (318 minutes) versus 208 minutes for those between 40-59.9 years and 174 minutes for those <40 years age (p=0.000). There was no difference in the duration of PA per week for those with one or more forms of medical illness versus those without (p=0.120). There was no decrease in PA duration with increasing numbers of co-morbidities (P=0.862). Amongst persons with medical conditions, only those with cancer (median 150 vs 60 minutes, p=0.044) and those with other illnesses (median 160 vs 120 minutes, p=0.019) exercised less than those without such comorbidities.
Overall, 0.9% of participants stated that their medical conditions were not under control and 2.4% that the illness affected their ability to do PA.
Participants’ Responses to the Seven SPARQ Questions (Table 2)
Question 1 (Do you have either high blood pressure or a heart condition for which you still require treatment and close follow-up by a doctor?)
For this first question 13.2% reported either high blood pressure or heart disease still requiring treatment or close follow-up by a doctor. These were slightly older than those without heart disease or hypertension. There was no difference in their weekly duration of PA. Moderate difficulty in understanding the question was encountered by those answering Yes. Respondents fed-back that the question covered two medical conditions, viz. high blood pressure and heart disease, and was, therefore, double-barrelled.
Question 2 (Do you have moderate or severe joint pains or back pains made worse by physical exercise?)
For this question 16.9% reported Yes. There was no significant age difference between those with or without such pains. Those with pain exercised less and encountered moderate difficulty with this question. For the 47 (4.1%) who expressed difficulty with this question, the terms moderate and slight were subjective and unsure whether back pain and backache were the same condition.
Question 3 (Have you been feeling unwell over the last one week with either fever, sore throat, cough, vomiting or diarrhoea?)
For this question, 3.1% said Yes. There was no significant difference in age or usual duration of exercise with those who felt well. Those with symptoms expressed slight difficulty in understanding this question, while the others expressed no difficulty. Some felt that fever, cough, sore throat, vomiting and diarrhoea should have been enquired about separately since persons may not likely have all these conditions at the same time.
Question 4 (Do you get chest pains either during or after physical activity?)
For this question 2.5% answered Yes. There was no significant difference in age or numbers of cardiac risk factors from those not experiencing chest pain during PA. Those with symptoms generally exercised less and had moderate difficulty in understanding the question. The others did not encounter such difficulty. Those claiming difficulty were trying to grapple between what constituted chest pain and chest ache and wanted examples for better understanding.
Question 5 (Do you get unusual difficulty in breathing either during or after physical activity?)
Only 4.1% of participants experienced breathing difficulty that was unusual for that level of exercise. While there was no significant age difference amongst the groups, those with breathing difficulty exercised significantly less and experienced moderate difficulty in understanding the question. They felt that the word “unusual” was subjective and sometimes ambiguous. People who were exercising would always feel more breathless and wanted another word or phrase to better describe the abnormal symptoms.
Question 6 (Do you get palpitations either during or after physical activity?)
Up to 5.6% answered Yes. There was no significant age difference between those with or without palpitations. The symptomatic participants exercised less. Significant difficulty amongst symptomatic participants in understanding this question and moderate difficulty by others was because the word “palpitations” was considered too technical, and “medical jargon”, requiring simplification for better understanding.
Question 7 (Do you get dizzy spells or fainting episodes either during or after physical activity?)
For this question 6.1% answered “Yes”. Those with symptoms were generally younger, exercised much less and experienced slight difficulty in understanding. Those without symptoms had no difficulty. A few requested that the word “immediately” be added just before the words “after physical activity”. Some wanted the terms dizzy spells and fainting to be separate questions.
Participants Requiring Further Referral
Even though only 23.7% of the participants had a known prior medical condition, 35.7% of participants answered “Yes” to one or more of the seven questions posed in the SPARQ. For patients without known medical illnesses, 27.0% said Yes to one or more of the questions and would have been initially declared unfit for PA requiring further evaluation by a doctor versus 62.2% for those with a known medical illness (p=0.000). When distributed by age this would be 32.0% of those from age 21 – 39.9 years, 36.0% of those from 40 - 59.9 years, and 38.0% of those aged 60 years and above (p=0.277).
Participants Feedback on the SPARQ
Level of Difficulty in Understanding the SPARQ Questions
Generally, 90.0% of survey participants felt the quality of the advice provided in the SPARQ was adequate and 93.1% would be happy to follow it. The length of the questionnaire and the use of technical terms were felt to be adequate by 93.4% of the participants, regardless of presence of symptoms or co-morbidities. In spite of this, comments were received from 26.6% of survey participants. This included 28.8% from those with and 25.3% without symptoms.
The practice of satisficing was greater amongst those without symptoms (64.8%) versus 52.8% amongst those with symptoms (p=0.000). The level of difficulty in understanding the questions was greater amongst those with co-morbidities for the first six questions. For Question 7 on dizzy spells and fainting no significant difference in level of understanding between those with or without symptoms was noted.
Many participants commented that the questions were well drafted and simple to understand. The suggestions and comments by the participants on these questions are summarized in
Table 3.
Suggested Frequency of SPARQ Usage
While only 40.6% of participants preferred the SPARQ to be used by exercise participants once annually, 36.6% preferred it be done once every six months and the remaining 22.8% as frequently as needed. Those in older age groups preferred a once yearly schedule compared to those in younger age groups (p=0.038).
Discussion
The study’s objectives were to determine the level of difficulty in understanding the questions in the SPARQ, the likelihood of potential exercise participants being declared unfit and requiring further medical evaluation, and to obtain feedback from the public on the document. The participants came from a broad age-spectrum and different walks of life. Their feedback should be relevant for adult populations working and living in similar environments. This study was able to determine such difficulty in understanding the SPARQ questions.
With the draft SPARQ, approximately one-third would have been declared unfit to engage in moderate or intense PA and be referred to a doctor for further evaluation. This was similar to the what would have occurred in a similar population using the Canadian GAQ, but less than would have been seen with the PAR-Q+ [
15,
17]. The majority of referrals were from questions 1 and 2, which may have been phrased in general terms, without adequate differentiation to the degree of active symptom control. There would be a need to review these two questions to determine whether further refinement of these may help decrease unnecessary referrals. After all, only 0.9% of participants stated that their medical conditions were not under control and only 2.4% that their illness affected the ability to do PA. Such refinement may also be considered for questions 4, 5 and 6. Naturally, there is concern as to whether the large numbers of potential referrals may unduly stress health resources. In addition, for those whose symptoms or illnesses are well controlled, there should not be a need for further medical referral before continuing PA or gradually increasing their level of PA. Further referral may become a major disincentive to engage in PA, especially for the elderly. For reference, the use of the PARQ+ in the USA had seen much higher rates of referral in excess of 55%, even after appropriate modifications made [
21].
Active ischaemic heart disease, whether known or unknown, increases the risk of cardiovascular collapse during acutely stressful events such as unaccustomed PA, especially if not well controlled [
1,
14,
22]. Therefore, the question on heart disease needs to be retained and refined by language that highlights lack of adequate control.
The role of hypertension vis-à-vis PA needs careful evaluation. Though hypertension is a known risk factor for coronary artery disease, adverse events had not been reported if the baseline blood pressure was 140-180 mm Hg systolic and ≤90 mm Hg diastolic [
1]. The European Society of Cardiology 2020 guidelines recommend withholding maximal exercise stress testing if the BP exceeds 160/90 mm Hg [
22]. Otherwise, if medically stable and with BP<160/90 mm Hg further medical referral may not be required. The ACSM recommends that asymptomatic individuals with cardiovascular, metabolic or renal disease can continue exercising with progressive intensity unless new symptoms develop and that only patients with known uncontrolled BP (resting BP ≥140/90mm Hg), stage 2 hypertension (BP ≥160/100mm Hg) or target organ disease need undergo medical clearance before PA [
23,
24]. Therefore, only symptomatic, hypertensive patients or those with known uncontrolled high blood pressure may require medical evaluation before engaging in PA [
25].
For question 2 on joint pains, a relatively common complaint, regular low-impact PA can maintain physical function and reduce pain levels in patients with osteoarthritis [
26]. Understanding the International Olympic Committee’s concerns for musculoskeletal screening and increased risks of reinjury and contralateral side injury with recent ankle sprains, the language of this question needs refinement to minimise misunderstanding and reduce unnecessary referrals [
27,
28].
Short, acute illnesses can predispose to heat injuries [
29]. Heat disorders can occur with strenuous PA, especially when performed shortly after recent mild illnesses such as viral infections and gastroenteritis [
30]. Many jurisdictions advise rest and avoidance of PA if recent such illnesses occur. Heat stroke can also result in cardiac complications including sudden cardiac death [
31]. The very high understanding of this question suggests its retention.
The small number of participants experiencing chest pains had moderate difficulty with this question. Chest pain during exertion suggests acute ischaemic heart disease. Chest pain during exertion contributes to a high proportion of prodromal symptoms prior to collapse during PA [
32,
33,
34]. Modifications to this question may allow better understanding. The need to avoid duplication with Question 1 that concerns ischaemic heart disease should also be considered.
Unusual difficulty in breathing is a well-recognised prodromal symptom in previous studies on cardiac arrest during PA [
21,
35]. Unusual breathlessness may also portend a worsening respiratory condition [
36]. The words, “unusual breathlessness” may require review. Such symptoms are relevant to the questionnaire.
The question on palpitations needs review. While palpitations may be a prodromal symptom in cardiac arrest patients, it has been equally prevalent in non-cardiac arrest patients in another study [
37,
38]. With significant misunderstanding issues and conflicting evidence of its value, one would need to review including this question in any pre-participation questionnaire.
There was only slight difficulty for the seventh question on dizzy spells or fainting episodes during or after PA. Dizziness is a prodromal symptom amongst cardiac arrest patients, including among athletes [
17,
38]. While the causes of dizziness may not be obvious initially it merits careful evaluation. The suggestion on adding the word “immediately” before “after physical activity” appears reasonable.
Limitations of the Study
This study could not examine the reliability of the SPARQ in minimizing the likelihood of adverse events during moderate to intense PA. This would require a prospective long-term effort involving large numbers of community participants using this tool and monitoring of adverse outcomes after PA.
The presence of satisficing in the study was also a limitation as would be in similar questionnaires. However, efforts in identifying this helped to better understand the feedback from study participants.
A high proportion of data were noted to be likely satisficed and removed from feedback analysis. This must be recognized as a likely limitation in surveys of this nature. Prior expectation of high satisficing rates would have resulted in the need to appropriately increase sample size.
In this anonymized public survey, we could not have validated the presence / absence of actual conditions amongst those apparently unfit for PA. However, with actual individual use of the SPARQ, and further evaluation by a medical practitioner, if applicable, such validation may have been done.
Conclusion
Adopting the SPARQ as a primary pre-participation screening tool for PA may be considered with suitable modifications to the questions and after considering participants’ feedback. When applying such questionnaires across communities, large numbers of medical referrals may unduly strain existing medical resources. Refining the phraseology of the questionnaire may help to decrease unnecessary referrals.
Author Contributions
Conceptualization, Anantharaman Venkataraman; Data curation, Anantharaman Venkataraman and Tess Lin Teo; Formal analysis, Tess Lin Teo, Ian Zhirui Hong, Lisa Cuiying Ho, Stefanie Hwee-Chee Ang and Anantharaman Venkataraman; Investigation,; Methodology, Tess Lin Teo, Ian Zhirui Hong, Lisa Cuiying Ho, Stefanie Hwee-Chee Ang and Anantharaman Venkataraman; Resources, Stefanie Hwee-Chee Ang; Software, Stefanie Hwee-Chee Ang; Supervision, Anantharaman Venkataraman; Validation, Stefanie Hwee-Chee Ang; Writing – original draft, Tess Lin Teo and Anantharaman Venkataraman; Writing – review & editing, Tess Lin Teo, , Ian Zhirui Hong, Lisa Cuiying Ho, Stefanie Hwee-Chee Ang and Anantharaman Venkataraman.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Institution Review Board of the Singapore Sport Institute.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Thomas SG, Goodman JM, Burr JF. Evidence-based risk assessment and recommendations for physical activity clearance: established cardiovascular disease. Appl Physiol Nutr Metab. 2011;36 Suppl 1:S190-213.
- Davies SC, Atherton F, McBride M, Calderwood C. UK Chief Medical Officers' Physical Activity Guidelines UK 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf (accessed on 11 November 2021).
- Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM's Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc 2015; 47:2473-9.
- Iliodromiti S, Ghouri N, Celis-Morales CA, et al. Should Physical Activity Recommendations for South Asian Adults Be Ethnicity-Specific? Evidence from a Cross-Sectional Study of South Asian and White European Men and Women. PLoS One 2016;11:e0160024.
- WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
- PAR=Q+. The Physical Activity Readiness Questionnaire for Everyone. PAR-Q+ Collaboration. Available online: https://eparmedx.com/?page_id=75 (accessed on 17 December 2022).
- Canadian Society of Exercise Physiology. Get Active Questionnaire. Available online: https://csep.ca/wp-content/uploads/2021/05/GETACTIVEQUESTIONNAIRE_ENG.pdf (accessed on 12 June 2023).
- Whitfield GP, Pettee Gabriel KK, Rahbar MH, Kohl HW 3rd. Application of the American Heart Association/American College of Sports Medicine Adult Preparticipation Screening Checklist to a nationally representative sample of US adults aged >=40 years from the National Health and Nutrition Examination Survey 2001 to 2004. Circulation. 2014 Mar 11;129(10):1113-20. [CrossRef] [PubMed] [PubMed Central]
- Maranhão Neto G de A, Santos TM, Pedreiro RC de M, Carmo HA do, Jardim RTC, Lorenzo A de. Diagnostic Validity of Screening Questionnaire American College of Sports Medicine/American Heart Association. J Phys Educ [Internet]. 2019;30:e3035. [CrossRef]
- Whitfield GP, Riebe D, Magal M, Liguori G. Applying the ACSM Preparticipation Screening Algorithm to U.S. Adults: National Health and Nutrition Examination Survey 2001-2004. Med Sci Sports Exerc. 2017 Oct;49(10):2056-2063. doi: 10.1249/MSS.0000000000001331. [CrossRef] [PubMed] [PubMed Central]
- Sports Safety Committee. Overview and Recommendations for Sports Safety in Singapore - A Report by the Sports Safety Committee. 2007. Available online: www.sportsingapore.gov.sg/files/Sport%20Education/Sport%20Safety/Sports_Safety_Committee_26SEPO7.pdf (accessed on 26 June 2023).
- Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Canadian Journal of Sport Science 1992;17:4 338-345.
- Canadian Society for Exercise Physiology. Get Active Questionnaire – Reference Documentment. Available online: https://csep.ca/2021/01/20/pre-screening-for-physical-activity/#post/0 (accessed on 12 June 2023).
- Venkataraman A, Hong IZ, Ho LC, Teo TL, Ang SH. Public Perceptions on the Use of the Physical Activity Readiness Questionnaire. Healthcare (Basel). 2024 Aug 23;12(17):1686. [CrossRef] [PubMed] [PubMed Central]
- Ho CL, Anantharaman V. Relevance of the Get Active Questionnaire for Pre-Participation Exercise Screening in the General Population in a Tropical Environment. Healthcare (Basel). 2024 Apr 10;12(8):815. [CrossRef] [PubMed] [PubMed Central]
- Lisa Cuiying Ho, Ian Zhirui Hong, Tess Lin Teo, Stefanie Hwee Chee Ang and Venkataraman Anantharaman. Public Perceptions of the Get Active Questionnaire. Int J Orthop Sports Med. 2015; 6: 1015.
- Marijon E, Uy-Evanado A, Dumas F, et al. Warning Symptoms Are Associated With Survival From Sudden Cardiac Arrest. Ann Intern Med 2016; 164:23-9.
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004 Jan 10;363(9403):157-63. Erratum in: Lancet. 2004 Mar 13;363(9412):902. PMID: 14726171. [CrossRef] [PubMed]
- Scott B, Gehlbach H. Using the Theory of Satisficing to Evaluate the Quality of Survey Data. Research in Higher Education. 2012; 53 (2): 182-200. [CrossRef]
- Vriesema CC, Gehlbach H. Assessing survey satisficing: The impact of unmotivated questionnaire responding on data quality. Educational Researcher. 2021; 50(9): 618–27. [CrossRef]
- Cardinal BJ, Cardinal MK. Screening Efficiency of the Revised Physical Activity Readiness Questionnaire in Older Adults. Journal of Aging and Physical Activity. 1995; 3: 299-308.
- Pelliccia A, Sharma S, Gati S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J 2021; 42:17-96.
- Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM's Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015; 47:2473-9.
- Liguori G, Feito Y, Foutaine C, Roy B, eds. ACSM’s guidelines for Exercise Testing and Prescription. 11th Edition. Philadelphia: Wolters Kluwer, 2021.
- Centres for Disease Control and Prevention. 5 Surprising Facts About High Blood Pressure. National Centre for Chronic Disease Prevention. Available online: https://www.cdc.gov/bloodpressure/5_surprising_facts.htm (accessed on 11 November 2021).
- Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res (Hoboken). 2020; 72:149-62.
- Ljungqvist A, Jenoure PJ, Engebretsen L, et al. The International Olympic Committee (IOC) consensus statement on periodic health evaluation of elite athletes. March 2009. Clin J Sport Med 2009; 19:347-65.
- Fulton J, Wright K, Kelly M, et al. Injury risk is altered by previous injury: a systematic review of the literature and presentation of causative neuromuscular factors. Int J Sports Phys Ther. 2014; 9:583-95.
- Leyk D, Hoitz J, Becker C, Glitz KJ, Nestler K, Piekarski C. Health Risks and Interventions in Exertional Heat Stress. Dtsch Arztebl Int. 2019;116(31-32):537-44 C, Glitz KJ, Nestler K, Piekarski C. Health Risks and Interventions in Exertional Heat Stress. [CrossRef] [PubMed] [PubMed Central]
- Harris KM, Mackey-Bojack S, Bennett M, et al. Sudden Unexpected Death Due to Myocarditis in Young People, Including Athletes. Am J Cardiol 2021;143:131-4.
- Marchand M, Gin K. The Cardiovascular System in Heat Stroke. CJC Open. 2021 Oct 12;4(2):158-163. [CrossRef] [PubMed] [PubMed Central]
- D’Silva A, Papadakis M. Sudden cardiac death in athletes. Eur Cardiol. 2015;10: 48–53.
- Risgaard B, Winkel BG, Jabbari R, et al. Sports-related sudden cardiac death in a competitive and a noncompetitive athlete population aged 12 to 49 years: data from an unselected nationwide study in Denmark. Heart Rhythm. 2014;11: 1673–81.
- Fanous Y, Dorian P. The prevention and management of sudden cardiac arrest in athletes. CMAJ. 2019 Jul 15;191(28):E787-E791. [CrossRef] [PubMed] [PubMed Central]
- Herlitz J, Karlson BW, Sjöland H, Albertsson P, Brandrup-Wognsen G, Hartford M, Haglid M, Karlsson T, Lindelöw B, Caidahl K. Physical activity, symptoms of chest pain and dyspnoea in patients with ischemic heart disease in relation to age before and two years after coronary artery bypass grafting. J Cardiovasc Surg (Torino). 2001 Apr;42(2):165-73. [PubMed]
- Smoliga JM, Mohseni ZS, Berwager JD, Hegedus EJ. Common causes of dyspnoea in athletes: a practical approach for diagnosis and management. Breathe (Sheff). 2016 Jun;12(2):e22-37. [CrossRef] [PubMed] [PubMed Central]
- Sohail H, Ram J, Hulio AA, Ali S, Khan MN, Soomro NA, Asif M, Agha S, Saghir T, Sial JA. Prodromal Symptoms in Patients Presenting With Myocardial Infarction. Cureus. 2023 Aug 18;15(8):e43732. e: 18;15(8). [CrossRef] [PubMed] [PubMed Central]
- Reinier K, Dizon B, Chugh H, Bhanji Z, Seifer M, Sargsyan A, et al. Warning symptoms associated with imminent sudden cardiac arrest: a population-based case-control study with external validation. Lancet Digit Health. 2023; 5: e763–73.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).