1. Introduction
The management of the COVID-19 pandemic has profoundly affected the approach to care, and from this climate of change has emerged the need to define the development of the role and context of the Hospital Medical Directorate for the return to a “new normal”. Change must be seen as an opportunity to improve patient performance and services, such as reducing waiting lists and increasingly implementing best practices such as infection control. As is well known, health care companies and their hospitals are among the most complex systems in the business economy where even the smallest facility is different from another, even though it delivers similar services, because of the heterogeneity of the services that are offered and because of the number and specificity of relationships between professionals. Covid-19 has certainly accelerated the need to govern the internal dynamics of hospital facilities and their interactions in the territorial context, and also the need to define and codify the ways in which to deal with the daily routine, also highlighting new issues, or more simply known issues but in a new light to implement system governance.
The structure of Clinical Governance has been represented over the years in different ways, one of the must current ways is the Chambers’ tree [
1], within which the different “branches” i.e., “disciplines” find reference to, for example: quality management systems, risk management, audits and assessments, accountability, development and improvement of Diagnostic Therapeutic Care Pathways (DTCPs), etc. The new environment has required, and continues to require, increasing teamwork that accelerates and facilitates decision making.
While there is an increasing need for synergy among the different actors in corporate leadership and between them with the leadership of clinical care facilities, especially in large companies, there is also a demand for the development of new skills and the use of appropriate tools for the exercise of concrete governance.
Concreteness is provided by a business environment where health care organizations stimulate and develop awareness and responsibilities in the continuous improvement of the quality of performance and services in order to achieve-maintain high clinical-welfare standards.
Considering the above and with the commitment of the Health Management of AUSL Romagna, a project was designed to support the Medical Management role in governing change, with the following objectives:
Consolidate/develop the exercise of the role of the Rimini Hospital Medical Management (HMD) team from a ‘’business management system’’ perspective in order to increase the value of performance and services in operational management;
Define key competencies for the exercise of the HMD role and training priorities;
Share the results of the approach applied in the project as a premise for possible ways of consolidation and extension in other corporate and/or network settings.
The project was designed and implemented with the methodological support of Studio EmmEffe S.r.l. Milan Italy.
2. Materials and Methods
The project started in July 2021 and ended in March 2022, according to the work plan reported in
Table 1, which shows the project phases and their time extension.
The project has seen its preliminary contextualization in the logic of business management with specific focus related to the AUSL of Romagna and to the activities common to all the Doctors of the Rimini Medical Direction, such as the on-call-availability of the HMD Doctor. This premise was considered fundamental in order to operationalize and concretize the topics of business management from the perspective of the HMD Doctors on staff for the Rimini Area (Rimini, Santarcangelo and Novafeltria Hospitals) at the time of the project.
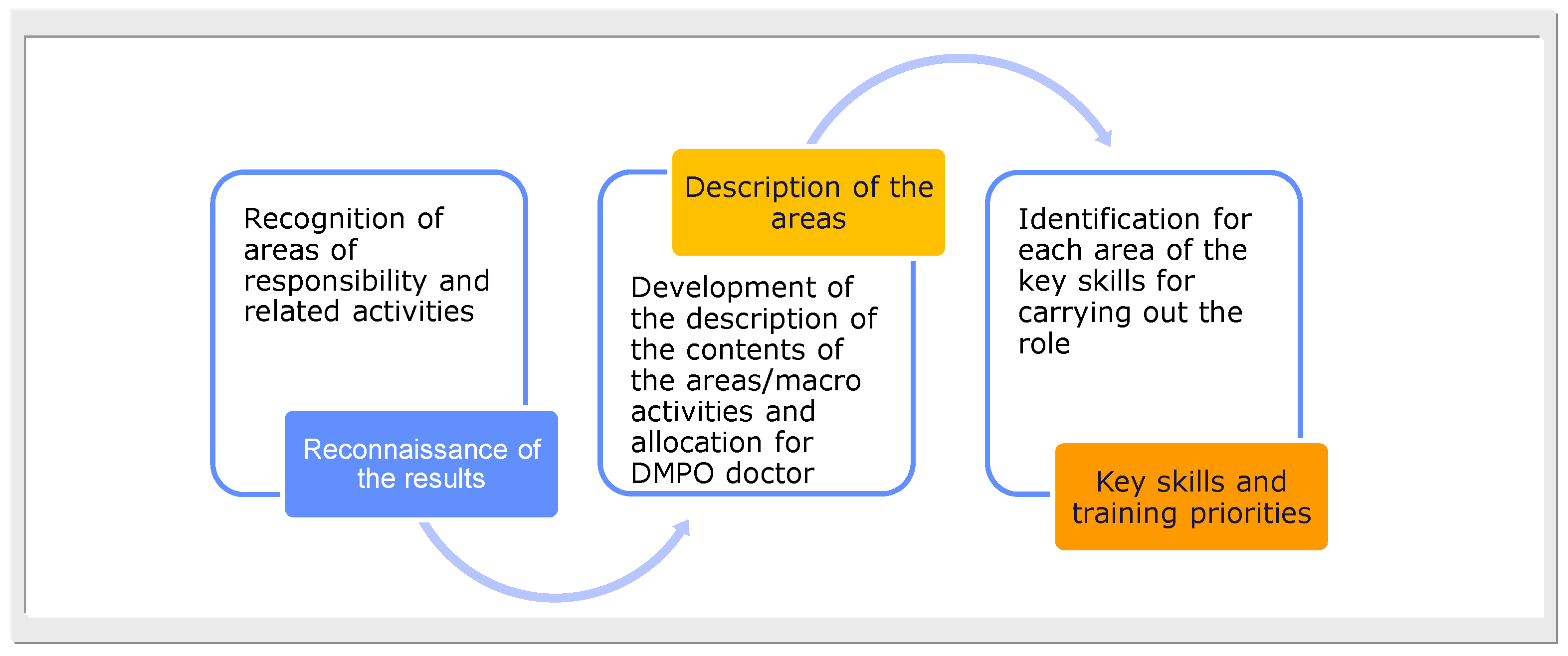
The methodology adopted for this project involved three key phases (
Figure 1):
Reconnaissance of areas of responsibility and related activities;
The development of the content description of the areas/macro activities and their allocation by HMD physician;
The identification for each area of key competencies for the exercise of the role.
The planning was developed through seven in-person workshops with the active participation of the Medical Management Team physicians and with remote checks to support the activities outcome of the previous meeting and the preparation of the next meeting.
In a general sense, the reconnaissance of the areas of responsibility exercised in a role has as its premise the purpose of the role of a function, in our case that of the Hospital Medical Directorate (HMD), to ensure that the area of work analyzed consistently reflects the expectations of all stakeholders involved.
That being said, the purpose of the role, i.e., the mission of the HMD as it was referred to in the corporate documentation, was therefore shared in the project: ‘’To ensure, the functionality and safety of the production system (structural, plant, technological resources, etc.) in compliance with the general and specific requirements for accreditation and in close integration with the transversal functions of technical, health, logistical and administrative support as far as the Facility is concerned.’’
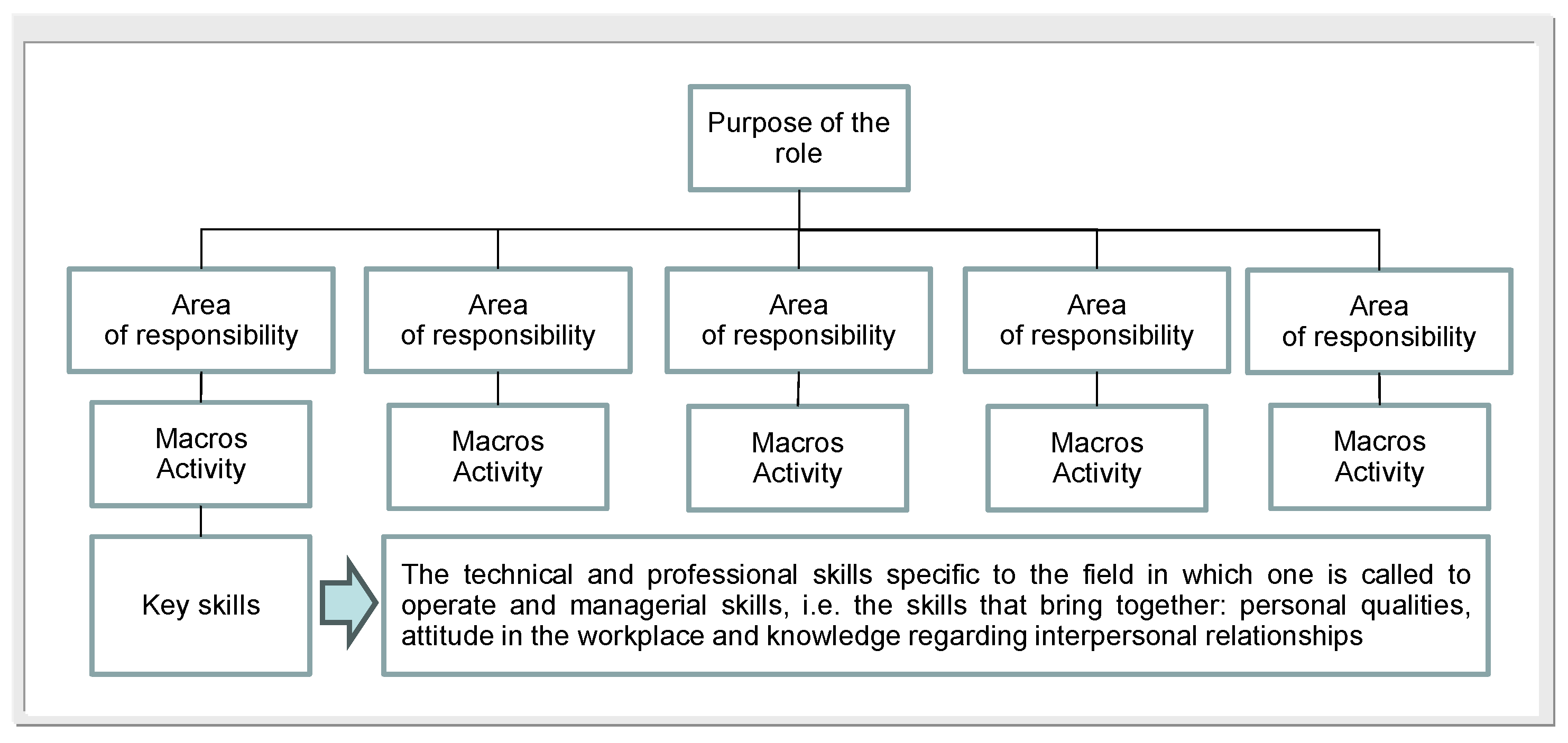
Sharing the purpose of the role of the HMD is the premise against which the methodological architecture described in
Figure 2 is developed. Following the methodological architecture, the following were gradually declined: areas of responsibility, the related macro-activities and then the key competencies, understood as hard skills (with reference to technical-professional competencies) and soft skills (with reference to relational competencies) to “guarantee” the development of the role.
The purpose of the role is usually related to a few areas of responsibility, which are considered “key” to achieving the objectives of the role. In order to achieve the purpose of the role, it is therefore necessary to manage the individual areas of responsibility, which may be developed to a greater or lesser extent depending on the business priorities in which the role is implemented and the scenario that is updated over time.
To best illustrate what the areas of responsibility are, it is possible to refer to the question “what must happen, what must be generated to achieve the purpose of the role?”
Since the areas of responsibility must be translated into activities of daily living, supported by the necessary competencies to guarantee the expected results and objectives, they must be described in order to be able to clarify their contents.
Also, for the description of macro-activities, as for the areas of responsibility, what emerged in the meetings was analyzed and the various findings were discussed, elaborated and revised with the participants at the various workshops that characterized the project.
It should be noted, moreover, that in identifying key macro-activities, attention was paid not only to the “current point of view” but also to the “perspective point of view.” Indeed, work was also done in terms of “challenging change” since change requires thinking and acting differently from what has been done in the past.
The third phase of the methodological approach, referred to in
Figure 1, involved defining key competencies for the exercise of the HMD role while also considering the new scenario. In fact, the ongoing evolution of work contexts in the health care field increasingly requires the search for professionals capable of operating in complex areas, called upon to deal with issues that are not always well defined, sometimes contradictory and often completely new.
The concept of competence, therefore, appears to be closely related to the ability to master new, articulated and multifaceted situations. The term “competence” has become increasingly attractive and important given its immediate association with professional skills, qualifications and experience, not simply applied, but increasingly managed in original and new ways in response to change.
Continuing education, in the international context, is considered indispensable for the success and competitiveness of organizations, as well as for the preservation and development of spendable professionalism in the world of work. This applies to all health care organization professionals working in clinical care processes who have been involved in continuing education programs, whether or not linked to CME credits, for decades, and it also applies to Physicians in Facility Medical Directorates. Obviously, the topic of training also applies to all administrative staff of health care organizations, but this is another topic that would deserve specific assessment in a perspective that encompasses the completeness of the system.
An analysis of the literature shows that it is not possible to be exhaustive with respect to the multiple definitions of “competencies.” Indeed, there are several definitions in this regard, and in the field of training sciences or human resource management for this topic great importance is given to contextualization.
In any case, to simplify the exposition, the competencies necessary for the exercise of a professional role, in our case that of the HMD, can be classified into two macro-categories:
- “technical skills, also referred to as “hard skills,” which are the technical and professional skills specific to the specific field and domain in which one is called upon to work;
- managerial skills, i.e., “soft skills,” which are those skills that group personal qualities, attitude in the work environment and knowledge in the field of interpersonal relations.
As illustrated by the literature and confirmed by daily practice, there is an increasing importance that managerial skills are acquired in this period of “crisis” in order to better cope with change.
In the implementation of the project, the work team contributed in a co-participatory way in the different methodological stages of the project. At the conclusion of the project was formalized a report, of which in the following chapter we report the summary of the outcomes, presented and shared with the Corporate Health Management, the Medical Management of AUSL Romagna and other components of the Health Management.
3. Results
Medical Directors are increasingly involved in managing corporate and budget objectives, as well as overseeing processes and care pathways. This involvement can/will grow more and more in the coming years for better corporate governance. To achieve this, they will increasingly take on an active role in supporting Departmental and Facility Management in change management, while also developing new competencies in clinical care processes, Diagnostic-Therapeutic Care Pathways (DTCPs), and related risk management, in collaboration with Corporate Directorates. This is in addition to their institutional and regulatory responsibilities.
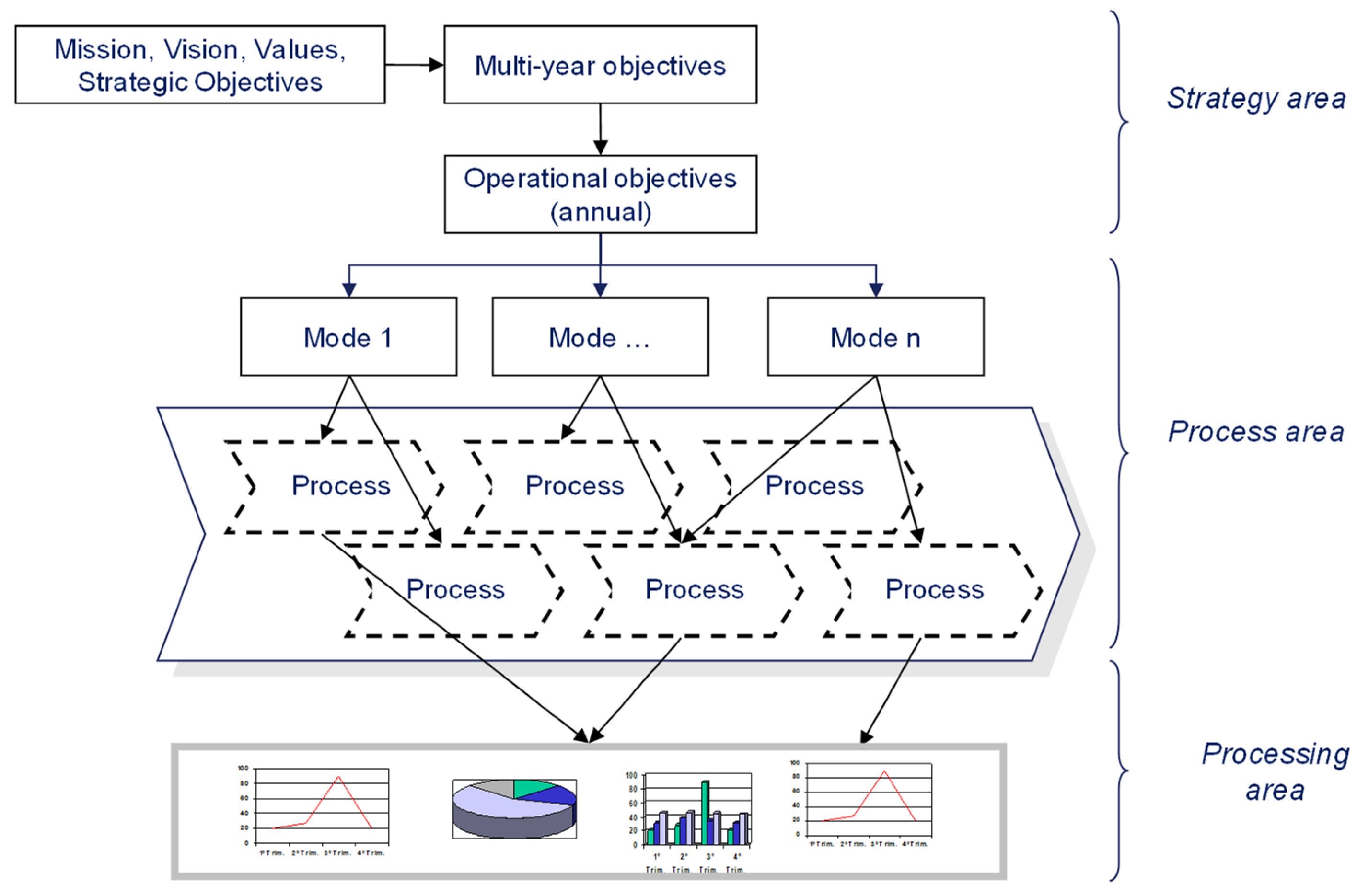
In order to best contextualize the overall potential of the project’s findings with regard to the role of the HMD, it is useful to consider the “role” and its possible developments in light of the Health Company’s objectives. To do this, it is necessary to frame the results in an overview of the health care organization related to the areas of business management. The areas of business management as reported in
Figure 3 are divided into: a) strategy area; b) process area; c) development area.
For the three areas below, we give a brief description and it is within this context that the role of the Facility Medical Management is developed.
The strategy area is represented by defining the mission (the organization’s raison d’être), vision (where we want/need to go), corporate values, and setting strategic and operational goals for the year. All in compliance with regional guidelines and relevant regional planning.
This stage of business management defines the references to be considered by all the organization’s staff in planning and programming the activities in their own context.
The process area is characterized by the correlation (deployment) between the objectives of the year and the business processes, in order to identify the contribution that each process will have to make to the operational translation of the business strategy. In addition to goal deployment, the process area is characterized by “process management,” which requires their identification, understanding and measurement. This area includes both process performance and risk management (e.g., clinical risk, administrative accounting risk, etc.), and it also includes the management of Diagnostic Therapeutic Care Pathways (DTCPs), the latter a theme that increasingly characterizes the integration of hospital and territory.
The elaborations’ area is characterized by the identification, collection and analysis of business data in order to activate feedback loops and give way to activate decision-making according to the results achieved in the period compared to the planned results.
Given the above and with reference to the purpose of the role for the HMD defined in the corporate acts: “Ensuring, the functionality and safety of the production system (structural, plant, technological resources, etc.) in compliance with the general and specific requirements for accreditation and in close integration with the transversal functions of technical, health, logistical and administrative support as far as the Facility is concerned” below we summarize the application results of the methodology adopted.
The areas of responsibility/interest identified for the exercise of the role are as follows:
Promotion, planning monitoring of construction, technology and maintenance development projects;
Performance improvement of processes/pathways;
Risk management and reduction in processes/pathways;
Supervision and controls;
Management of external communication.
According to the described methodology, the key macro-activities were defined in workshops with HMD physicians for each of the five areas of interest/responsibility (
Table 2,
Table 3,
Table 4 and
Table 5).
As the project developed, among the HMD professionals, there was also increased awareness and importance of defining the key competencies necessary for the exercise of their role in the context of change.
The reconnaissance of the areas of interest/responsibility and macro-activities also allowed for a participatory and conscious redefinition of the areas of action of the different HMD physicians in the Rimini Hospital Group: Rimini Hospital, Novafeltria Hospital and Santarcangelo Hospital.
The third phase of the methodological approach led to the identification, also participated by the whole team, of what are and/or what should be the key competencies for the different areas of responsibility and related key macro-activities. An example excerpt regarding some of the key competencies for the area related to “Process/Pathway Performance Improvement” is reported in
Table 7.
Whereas the Facility Medical Directorate is responsible for overseeing all hygienic and organizational aspects of the Facility of reference, in the specific context of clinical areas such as cardiology, for example, the area of expertise is up-to-date in its own particular innovations, and the Facility Medical Directorate is required to have a range of skills ranging from infection prevention, to support in the organization of clinical organizational pathways for patients; to support in the management of production processes, quality control of the levels offered, and clinical risk management.
Within the HMD team, various professionals took charge of certain aspects to deepen an understanding of the subject matter to challenge themselves and redefine aspects within the group. Infectious risk management, for example, cuts across several specialty areas and interpolates control in inpatient wards and the surgical patient pathway. Assigning responsibilities to management physicians is critical to ensure supervision and oversight of these processes for their improvement. With that being said, it is of paramount importance to agree/share with the HMD team members on the redefinition of duties in the various hospital settings within the directorate with appropriate expertise in this regard.
In addition, as part of the project, also in relation to corporate priorities, a new contact person was identified to support the holder of the hospital standing working group as a member of the HMD team that deals with the surgical part and oversees the entire pathway in order to preside over wound-related risks and prevention of peri-operative septic risk.
Finally, the implementation of the project allowed for a structured identification of individual and Team training needs according to shared priorities strongly related to regional and corporate activities and guidelines such as the issue of risk management. Through the various project workshops, therefore, training priorities for the short to medium term aimed at developing key skills/knowledge for some or several components of the Facility Medical Management Team emerged such as:
The use of the corporate dashboard and reporting;
The use of regional databases and related data analysis;
The use of data analysis tools (e.g., Excel and related macros);
Knowledge of process management and operational management;
Team management and meeting management;
Project management and planning (project management);
The techniques and tools of problem setting and problem solving;
The mediation and management of conflicts;
The techniques and tools for enterprise clinical risk mapping and process/structure risk prevention and management;
The management of infectious risk and hospital infections;
Knowledge of audit techniques with special reference to clinical audit
With the operational development of the project activities, other specific results were also achieved such as:
(a) The reconnaissance of the activities carried out within the medical on-call availability with identification of priority improvement actions on which to act at the system level;
b) The activation of a periodic meeting within the Rimini HMD as a mechanism for the functioning of the Directorate itself within the team and with relation to the other company functions;
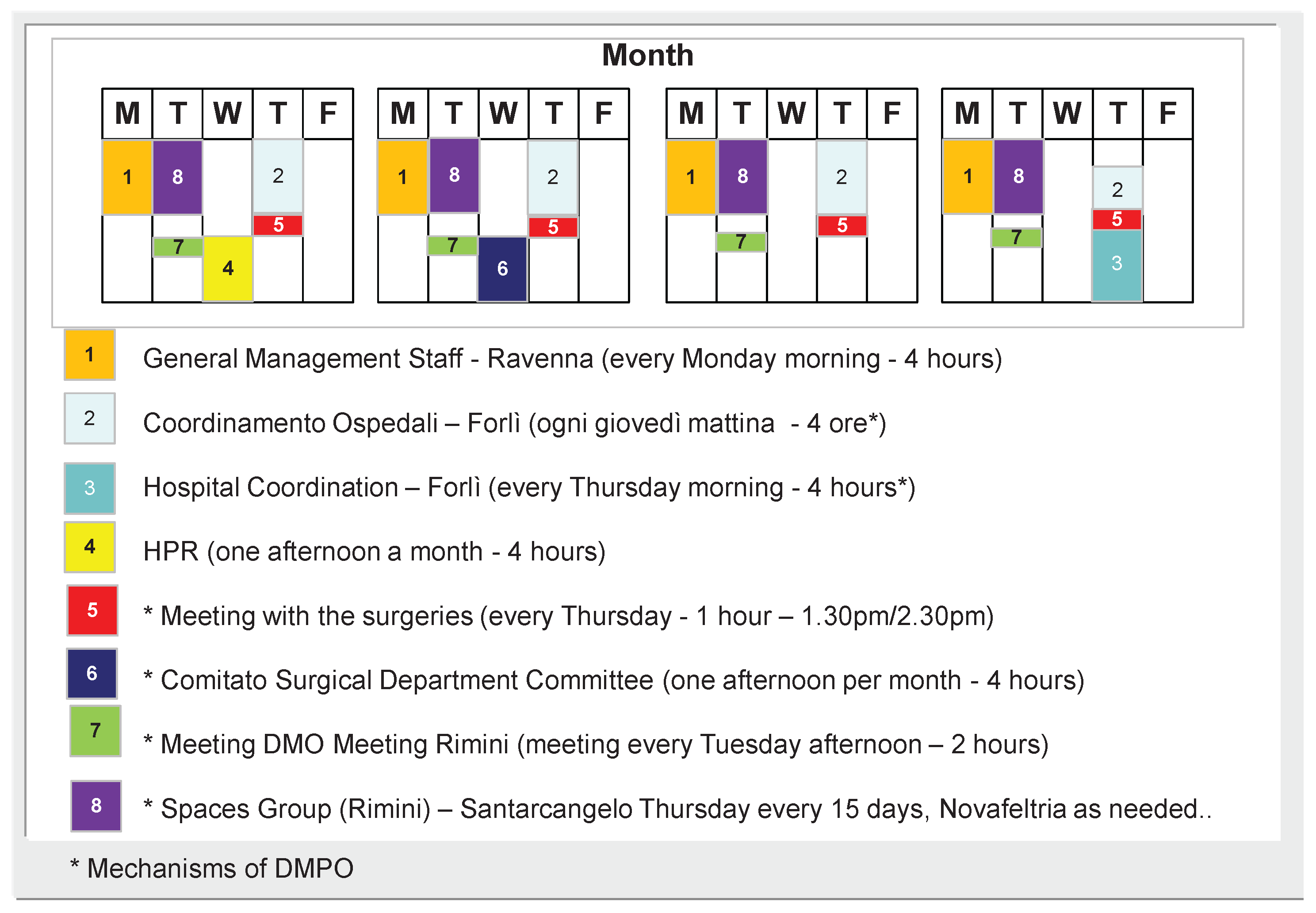
c) The reconnaissance of the operating mechanisms of the AUSL of Romagna that affect the Rimini HMD as shown in
Figure 4.
In particular, the last element related to the reconnaissance of the operating mechanisms of the Romagna AUSL that affect the Rimini HMD allowed for better contextualization of the periodic meetings of the HMD and the related sharing of priorities and also the reporting of results.
4. Discussion
The project made it possible to share and codify the HMD’s areas of responsibility in the context of the business system by declining key activities and in particular to initiate a structured definition of key competencies, with associated training priorities, for the exercise of the HMD’s role in a context of profound change.
The implemented project also helped the HMD Team to reflect on group dynamics. In the development of the project, in fact, there emerged the need for the sharing of operational approaches in the conduct of activities such as those related to the HMD doctor’s on-call with identification of priority improvement actions and the “standardization,” as far as possible, of shared and unambiguous actions in responding to the needs of citizens and professionals of the Rimini Hospital Facility.
It is still early to assess the improvement brought by the implementation of the project, but the process has been initiated and has already changed the way each professional works. A specific added value of the project, which is not secondary, in fact, has been to be able to preside over the different moments of communication within the HMD so that it is structured and full of useful information for the governance of processes, in this regard, in fact, periodic briefings and adequate tools to keep track of decisions and agree on tasks and timeframes have been introduced. Learning to unify codes is very important, especially among people who have to learn to collaborate in different ways. At this stage, the main challenge is to acquire new ways of working that encourage discussion and collaboration with others.
The outcomes of the project are to be considered as a first operational step developed in the context of the AUSL Romagna that was shared with the Medical Directorate of the Garrisons and the AUSL Health Directorate. In addition to breaking in the team of the Rimini HMD, the goal of Corporate Management may be the comparison with the Heads of the other Hospital Medical Directorates of the AUSL Romagna (which affects 1.2 million inhabitants) with possible additions to the elements that emerged within the project in order to define competence development plans structured at the corporate level.
A relevant step may also be to extend the outcomes of the project and its evolutions in the context of the various scientific reference societies involved and in university programs for the training of Medical Directors. In fact, the evolution of the role of Health Directorates, and specifically of Facility Medical Directors, will have to involve training programs structured in the medium to long term in order to respond proactively to change and thus be able to guide it with respect to their own areas of responsibility.
Author Contributions
Conceptualization, Paolo Parente, Mattia Altini, Massimo Farina and Francesca Raggi; methodology, Mattia Altini and Massimo Farina.; validation, Mattia Altini and Giuseppe Di Lorenzo; formal analysis, Massimo Farina and Francesca Raggi; resources, Massimo Farina and Francesca Raggi; writing—original draft preparation, Massimo Farina and Francesca Raggi; writing—review and editing, Paolo Parente and Giuseppe Di Lorenzo; supervision, Paolo Parente, Mattia Altini and Massimo Farina; project administration, Mattia Altini. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
“Not applicable”.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
Dutiful thanks to all the members of the Hospital Medical Directorate of the Rimini Hospital Facility who actively worked in the workshops for the realization of the project. Further thanks are due to Beckton Dickinson Italia S.p.A., whose nonconditional contribution enabled the realization of the project intended as an expression of the synergy, while respecting roles, of public and private structures for the development for the acquisition of methods and tools that can positively affect a development of clinical care activities in an increasingly organized, appropriate and safe way.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chambers R., Wakely G., Making Clinical Governance Work for You, Radcliffe Publishing Ltd., 2000.
- Bizzarri G., Canciani M., De Paoli G., Farina M., Guarneri C.,The development of the role profile of the homogeneous area pharmacist by intensity of care: from research design to practical application, Franco Angeli Editor, 2013.
- World Health Organization (WHO), The Helsinki Statement on Health in All Policies, The 8th Global Conference on Health Promotion, Helsinki, Finland, June 10-14, 2013.
- Ferrè L., Longo N., Roles and competencies in health care, Panorama Sanità Editor, 2011.
- Cergas Bocconi, Rapporto OASI 2010 - L’aziendalizzazione della sanità in Italia, Egea Editor, 2010.
- CEIS - Center for Economic and International Studies, Rapporto Sanità 2009: Sanità e sviluppo economico, Fondazione Economia Torvergata, 2009.
- Price Water House Coppers, HealthCast 2020: Creating a Sustainable Future, 2005.
- Drago R., The new maturity, Erickson Study Center, 2000.
- Le Boterf G., De la compétence: Essai sur un attracteur étranger, Ed. de l’Organisation, 1990.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).