1. Introduction
Within a national healthcare system founded on the principles of universality, equity and accessibility, it is paramount to ensure that all citizens have access to effective, equal and safe care. However, healthcare systems worldwide face significant challenges, including regional disparities, an increased demand for care due to demographic shifts, and constraints in economic and organizational resources. These factors highlight the need for structured and well-defined approaches to optimise operational efficiency while maintaining high-quality care.
The introduction of quality management models in the healthcare sector has become imperative to address these challenges through systematic frameworks that that not only improve efficiency but also enhance patient and employee satisfaction.
Among the various existing approaches, the EFQM (European Foundation for Quality Management) model stands out for its holistic approach to quality management that integrates continuous improvement, innovation, sustainability and the active involvement of all stakeholders. Its application in the healthcare context is not limited to mere compliance with quality standards, positioning itself as a governance strategy that strengthens resilience and drives organizations toward sustained excellence.
This study aims to explore the applicability and benefits of the EFQM model in healthcare by assessing its impact on key dimensions such as quality of care, error reduction, resource optimization, staff motivation, and stakeholder engagement. To provide a structured analysis, we have chosen the Italian healthcare system as a case study, as it offers a complex and decentralized setting where the effects of EFQM implementation can be observed across diverse regional healthcare structures. While this research is conducted within the Italian context, its findings are intended to provide insights relevant to healthcare systems globally, demonstrating how EFQM principles can be successfully adapted to different organizational frameworks.
2. Italian National Health Service
To concretely assess the application of the EFQM model in the healthcare sector, we have chosen to analyze the Italian healthcare system, using it as a representative case study. Italy has a complex public healthcare system based on the principles of universality, equity, and accessibility, yet it is characterized by significant regional variations in the quality of services provided. These peculiarities make the Italian context an ideal testing ground for understanding the challenges and benefits associated with the adoption of the EFQM model in the healthcare sector.
The Italian National Health Service (Servizio Sanitario Nazionale, SSN) operates through a three-tiered governance structure—national, regional, and local—which significantly influences the management and delivery of healthcare services. At the national level, the Ministry of Health establishes the overarching objectives through the National Health Plan, thereby ensuring uniformity in the provision of Essential Levels of Care. These levels delineate the minimum services guaranteed to all citizens. The regions, on the other hand, manage healthcare autonomously, adapting national directives to local specificities. This decentralisation allows greater adaptability to territorial specificities but has also contributed to creating inequalities in access and quality of care between different areas of the country. Finally, at the local level, Local Health Authorities (ASL) and Hospital Authorities directly provide health services to citizens.
The SSN is financed through the National Health Fund (“Fondo Sanitario Nazionale” - FSN), which is primarily funded by tax resources. These tax resources are then allocated to the regions according to demographic and epidemiological criteria. The overarching objective of this funding mechanism is to ensure that all citizens have access to healthcare without encountering significant economic barriers. However, the devolution of power to regional authorities has resulted in significant disparities in healthcare management across the country. The Northern regions, which tend to offer more efficient services, stand in contrast to the Southern regions, where deficiencies in infrastructure and protracted waiting times persist.
The minimum requirements for public and private facilities operating in accordance with the SSN are recognised through institutional accreditation. In addition to national standards, the regions have also developed other specific criteria to guarantee control and improvement of service quality. However, it should be noted that compliance with regulatory standards alone is insufficient to address the existing system's deficiencies. To address the current challenges, it is imperative to adopt quality management models that facilitate operational efficiency, optimise resource utilisation, and reduce territorial disparities, thereby ensuring equitable and uniform access to healthcare for all citizens.
3. Models and Certification in the Healthcare
As previously mentioned, in addition to institutional accreditation, which is a mandatory requirement for operation within the SSN, numerous models and certifications have been developed to support healthcare facilities in continuous improvement. Among these, ISO 9001:2015 certification is one of the most widespread standards at international level. This standard is predicated on a process approach and the concept of continuous improvement, with the objective being the optimisation of organisational effectiveness and user satisfaction. It should be noted, however, that this standard is not specific to the healthcare sector. In conjunction with ISO 9001:2015, UNI EN 15224 certification, a healthcare-specific standard, exists, introducing further requirements pertaining to clinical risk management and patient safety.
A more focused alternative is Joint Commission International (JCI) accreditation, a model that aims to improve safety and quality of care through rigorous standards and regular audits. This model is predominantly utilised by private hospitals and facilities that operate on an international scale. JCI certification places significant emphasis on patient safety and clinical risk management. Conversely, Lean Healthcare is predicated on an approach that prioritises operational efficiency, with the objective of reducing waste and optimising workflows. This is achieved by the implementation of principles such as reducing waiting times and enhancing care pathways. While Lean Healthcare has been shown to enhance productivity, its implementation necessitates a robust cultural and organisational commitment.
Whilst these tools offer concrete benefits, they frequently focus on specific aspects of healthcare or organisational management. By contrast, a model such as EFQM allows for a more integrated and strategic approach, combining quality, innovation and sustainability in a single systemic vision. Its structured methodology has been implemented in diverse healthcare environments, proving its effectiveness in enhancing hospital performance and fostering a culture of continuous improvement across different national healthcare frameworks.
4. EFQM Model in the Healthcare
In the realm of healthcare quality management, the EFQM (European Foundation for Quality Management) Model emerges as a prominent paradigm, distinguished by its integrated, excellence-oriented approach. Conceptualised to facilitate continuous enhancement in organisations, the EFQM model encompasses a multifaceted evaluation that extends beyond mere compliance with predetermined standards. It delineates a strategic vision encompassing quality, leadership, innovation, sustainability, and the generation of value for stakeholders. The EFQM model is predicated on the recognition that healthcare organisations function within increasingly intricate and rapidly evolving contexts, wherein adherence to regulatory mandates alone is inadequate to ensure the efficacy and sustainability of services. Consequently, the model prioritises the internal workings of an organisation, as opposed to merely evaluating its outcomes, with a focus on the congruence between its strategic direction, operational processes, and overall performance.
The model is predicated on a series of principles and criteria that guide organisations on their journey of continuous improvement. In particular, the EFQM focuses on five key areas: leadership, strategy, people, processes, and results. These elements are interconnected and aim to create an environment conducive to innovation and sustainability.
The implementation of the EFQM model in healthcare settings facilitates the identification of critical issues, including:
Does the hospital have a clear vision that is aligned with the needs of patients and society?
Is the leadership capable of driving change and promoting a quality culture?
Are available resources used efficiently to create sustainable value?
Is the organisation able to innovate and adapt to a changing environment?
Are the results achieved consistent with strategic objectives and stakeholder expectations?
In order to address the aforementioned questions, the EFQM employs a structured framework that enables organisations to analyse their management practices, identify strengths and areas for improvement, and implement evidence-based strategies. The assessment is conducted through a self-assessment process, whereby the organisation measures itself against EFQM criteria using the RADAR (Results, Approach, Delivery, Implementation and Review) framework. The RADAR framework is a tool for monitoring progress over time and identifying areas for improvement. Following this, external assessments are conducted by accredited assessors.
Certification according to the EFQM Model is not merely a matter of compliance with specific standards; rather, it signifies a genuine commitment to excellence. The attainment of this certification is facilitated by a progressive pathway, with varying levels of recognition (ranging from 'Committed to Excellence' to the pinnacle level of 7 stars) based on the maturity of the quality management system and the outcomes achieved. Each assessment provides a detailed analysis of organisational performance and suggests actions for continuous improvement.
The adoption of EFQM in healthcare is advantageous for several reasons. Primarily, the model advocates a systemic approach, thereby fostering integration between strategy, processes and results. It assists healthcare facilities in enhancing governance by increasing transparency in resource management and communication with stakeholders. A further significant benefit is the orientation towards innovation, as the model encourages change and adaptability in a sector characterised by continuous challenges. Furthermore, the adoption of the model has the potential to enhance patient and staff satisfaction through the optimisation of processes and the enhancement of communication. From an operational perspective, EFQM facilitates the optimisation of internal efficiency by reducing waste and redundancies in processes, and the enhancement of the quality of care through an evidence-based approach. Finally, the EFQM certification process represents a distinctive element that can enhance a hospital's reputation and facilitate its positioning at national and international level.
5. EFQM: RADAR Framework
The RADAR framework is the assessment tool used within the EFQM model to analyse organisational performance and drive continuous improvement. The name comes from the four key dimensions on which it is based: Results, Approaches, Deploy, Assess & Refine. Results: This component focuses on the outcomes achieved by organisations, measuring the effectiveness of the strategies implemented. It is essential that the results are relevant and measurable in order to assess progress towards the set goals. Approaches: It concerns the strategies and methods adopted to achieve the desired results. A well-defined approach must be based on evidence and good practices, ensuring that the actions taken are consistent with the organisation's strategic objectives. Deploy: This element refers to how the approach is implemented and communicated within the organisational structure. It is crucial that all levels of the organisation are engaged and that there is a clear understanding of responsibilities and roles. Assess: focuses on the actual implementation of planned actions. It is essential that implementation is constantly monitored to ensure that activities are carried out as planned and to identify any areas for improvement. Refine: Finally, the review involves a periodic evaluation of the results obtained and the effectiveness of the approach adopted. This process makes it possible to make timely changes and adapt strategies based on the feedback received.
RADAR is not merely an evaluation system; rather, it is a governance instrument that enables organisations to align strategy and operations, thereby maximising the effectiveness of their quality and innovation initiatives. This approach enables healthcare facilities and other organisations to identify their strengths and areas for improvement, ensuring a structured and sustainable growth path.
Figure 1.
RADAR MODELLO EFQM 2025 (The maximum attainable score for each criterion).
Figure 1.
RADAR MODELLO EFQM 2025 (The maximum attainable score for each criterion).
7. Benefits and Results of the EFQM Model: Evidence from Real-World Applications
The analysis conducted demonstrates how the implementation of the EFQM model in healthcare facilities can yield substantial benefits in several areas, including management efficiency, patient care quality, humanisation of care, and the promotion of training and research. Facilities that have adopted the model have reported an increased capacity to plan and utilise resources, with a reduction in waste and an improvement in the management of healthcare staff.
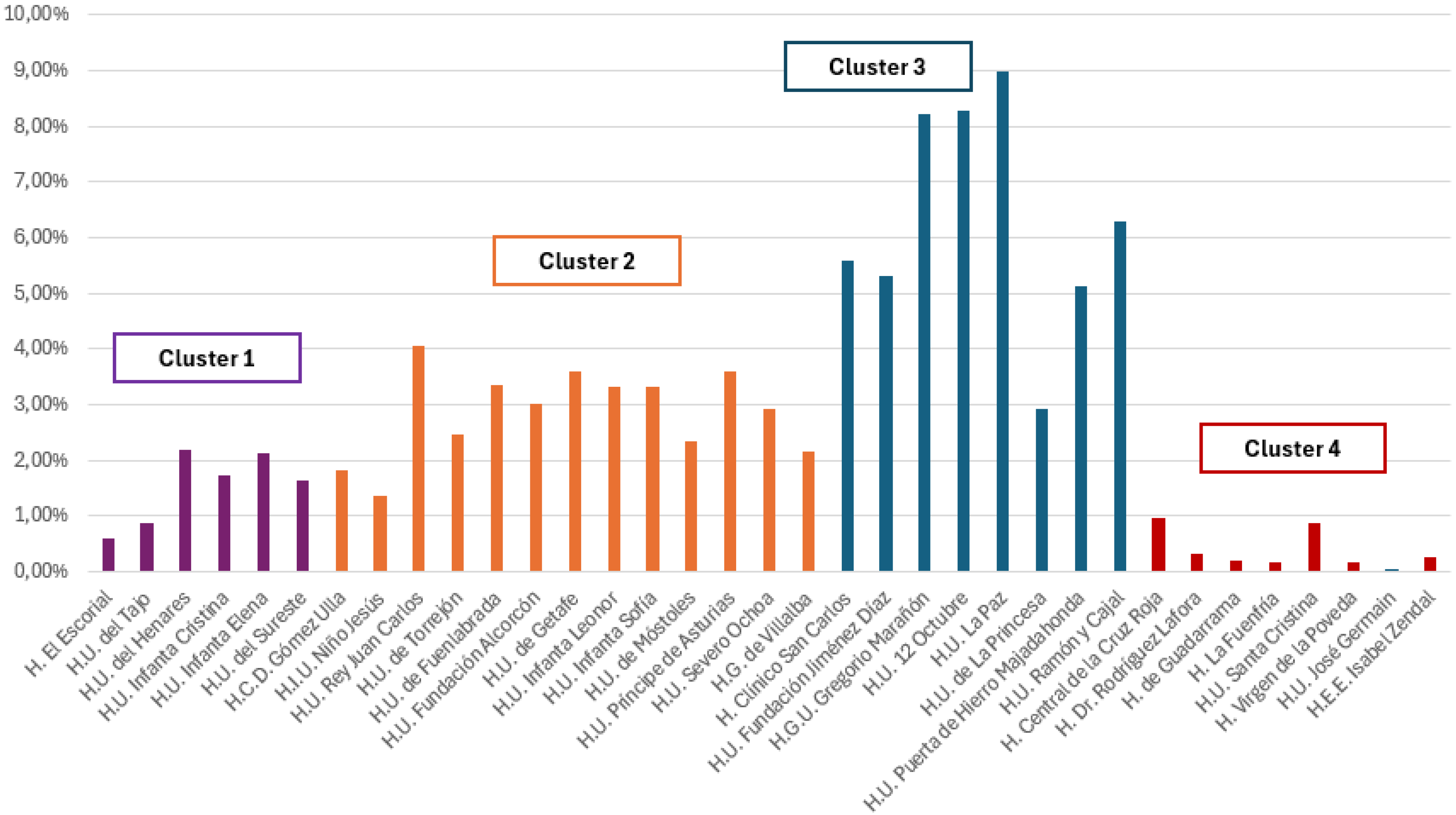
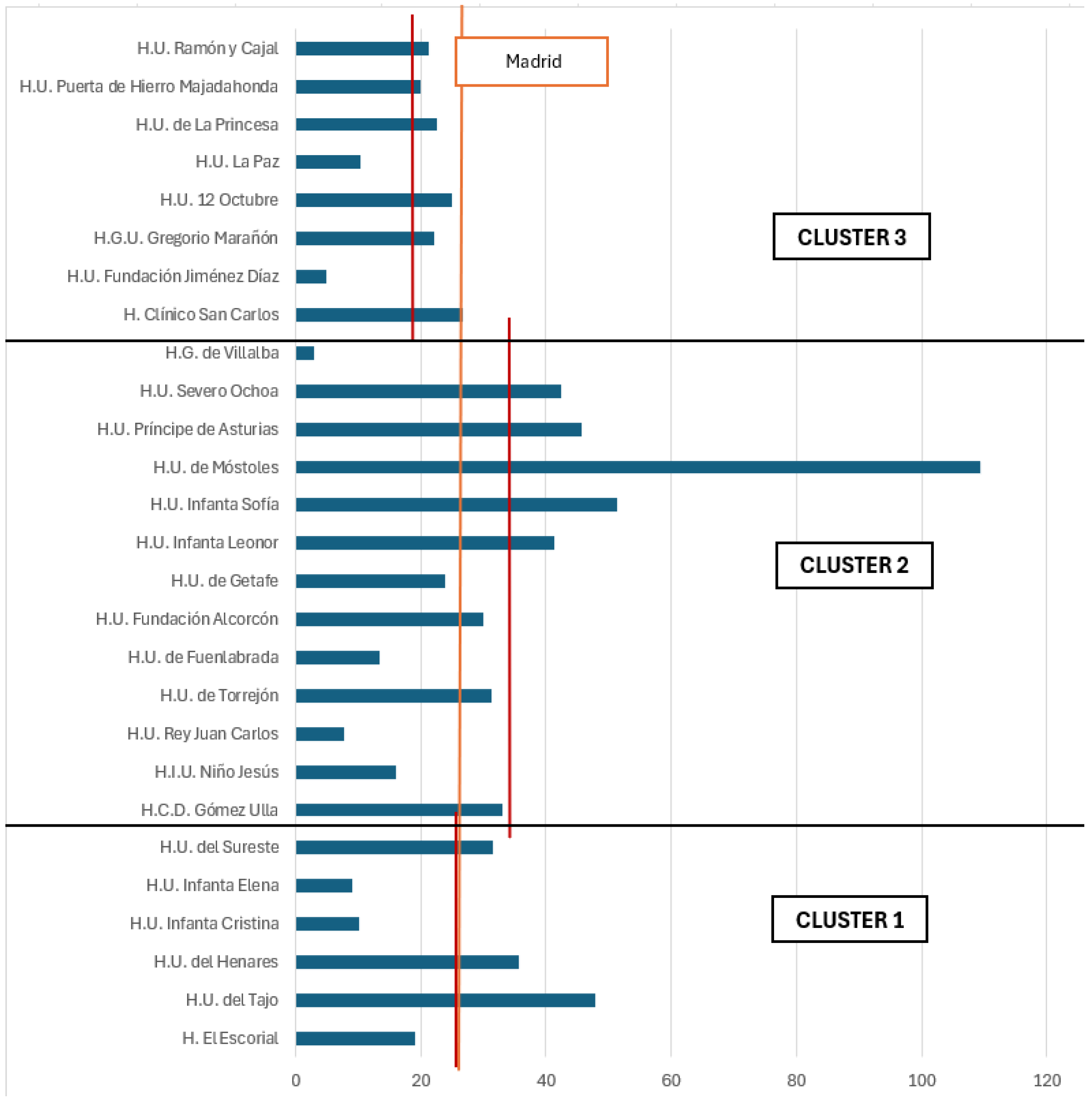
CONTEXT: The present study is based on a sample of 35 hospital facilities located in the Madrid community, a particularly suitable context for analysing the adoption of the EFQM model in healthcare. Madrid represents a national benchmark for the organisation of health services and offers a variety of facilities with different levels of complexity, thus allowing an effective comparison between hospitals that have implemented the EFQM model and those that have not. Furthermore, the demographic and organisational characteristics of Spain are comparable to those of Italy, thus rendering the results of the analysis particularly relevant for possible application in the Italian context. The survey is based on data from 2019-2022, analysing both facilities that have adopted the EFQM model and those that have not implemented it in order to assess the impact of certification on hospital management and identify its benefits.
CLUSTERISATION: The data were collected from two primary sources: AssesBase, which maintains information on EFQM-certified health facilities, and SERMAS (Community Health Service of Madrid), which provides data on non-certified facilities. To ensure greater representativeness, the sample was subdivided into four groups based on size, complexity of cases treated, and the clustering of hospitals done by SERMAS. This subdivision facilitates the comparison of hospitals with similar characteristics, thereby enabling the assessment of the influence of the adoption of the EFQM model on heterogeneous healthcare settings.
Cluster 1 (low complexity): H. El Escorial, H.U. del Tajo, H.U. del Henares, H.U. Infanta Cristina, H.U. Infanta Elena, H.U. del Sureste;
Cluster 2 (medium complexity): H.C.D. Gómez Ulla, H.I.U. Niño Jesús, H.U. Rey Juan Carlos, H.U. de Torrejón, H.U. de Fuenlabrada, H.U. Fundación Alcorcón, H.U. de Getafe, H.U. Infanta Leonor, H.U. Infanta Sofía, H.U. de Móstoles, H.U. Príncipe de Asturias, H.U. Severo Ochoa, H.G. de Villalba;
Cluster 3 (high complexity): H. Clínico San Carlos, H.U. Fundación Jiménez Díaz, H.G.U. Gregorio Marañón, H.U. 12 Octubre, H.U. La Paz, H.U. de La Princesa, H.U. Puerta de Hierro Majadahonda, H.U. Ramón y Cajal;
Cluster 4: H. Central de la Cruz Roja, H. Dr. Rodríguez Lafora, H. de Guadarrama, H. La Fuenfría, H.U. Santa Cristina, H. Virgen de la Poveda, H.U. José Germain, H.E.E. Isabel Zendal.
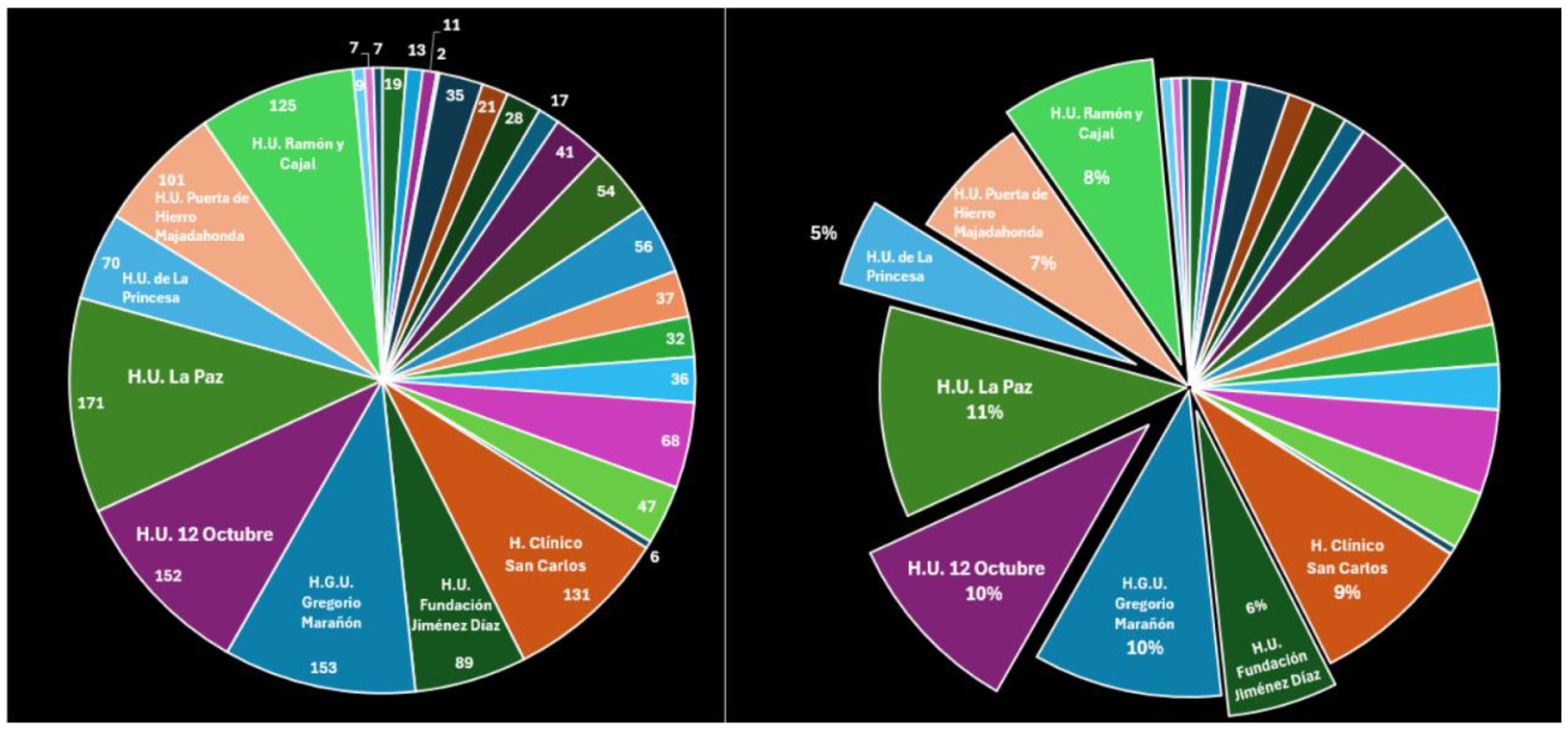
Figure 2.
percentage of admissions for each facility divided by the group.
Figure 2.
percentage of admissions for each facility divided by the group.
Hospitals in the fourth group are not classified according to their level of complexity; this category includes hospitals that support other centres, medium-stay hospitals and psychiatric hospitals. Among the 35 hospitals in Madrid, 12 have adopted the EFQM model, and in each group there are at least two EFQM-certified facilities. This ensures that each cluster has a point of reference for comparing management practices and results.
Cluster 1: H. U. El Escorial (4 star, 2023), H.U. Infanta Cristina (4 star, 2022), H.U. Infanta Elena (6 star, fino al 2017);
Cluster 2: H.U. Fundación Alcorcón (5 star, 2022), H.U. de Getafe (5 star, 2023), H.U. Infanta Leonor (4 star, 2022), H.G. de Villalba (6 star, 2022);
Cluster 3: H.U. Fundación Jiménez Díaz (Excellence Award, 2020), H.G.U. Gregorio Marañón (5 star, 2022), H.U. Puerta de Hierro Majadahonda (6 star, 2022);
Cluster 4: H. Dr. Rodríguez Lafora (3 star, 2023), H. de Guadarrama (6 star, 2022);
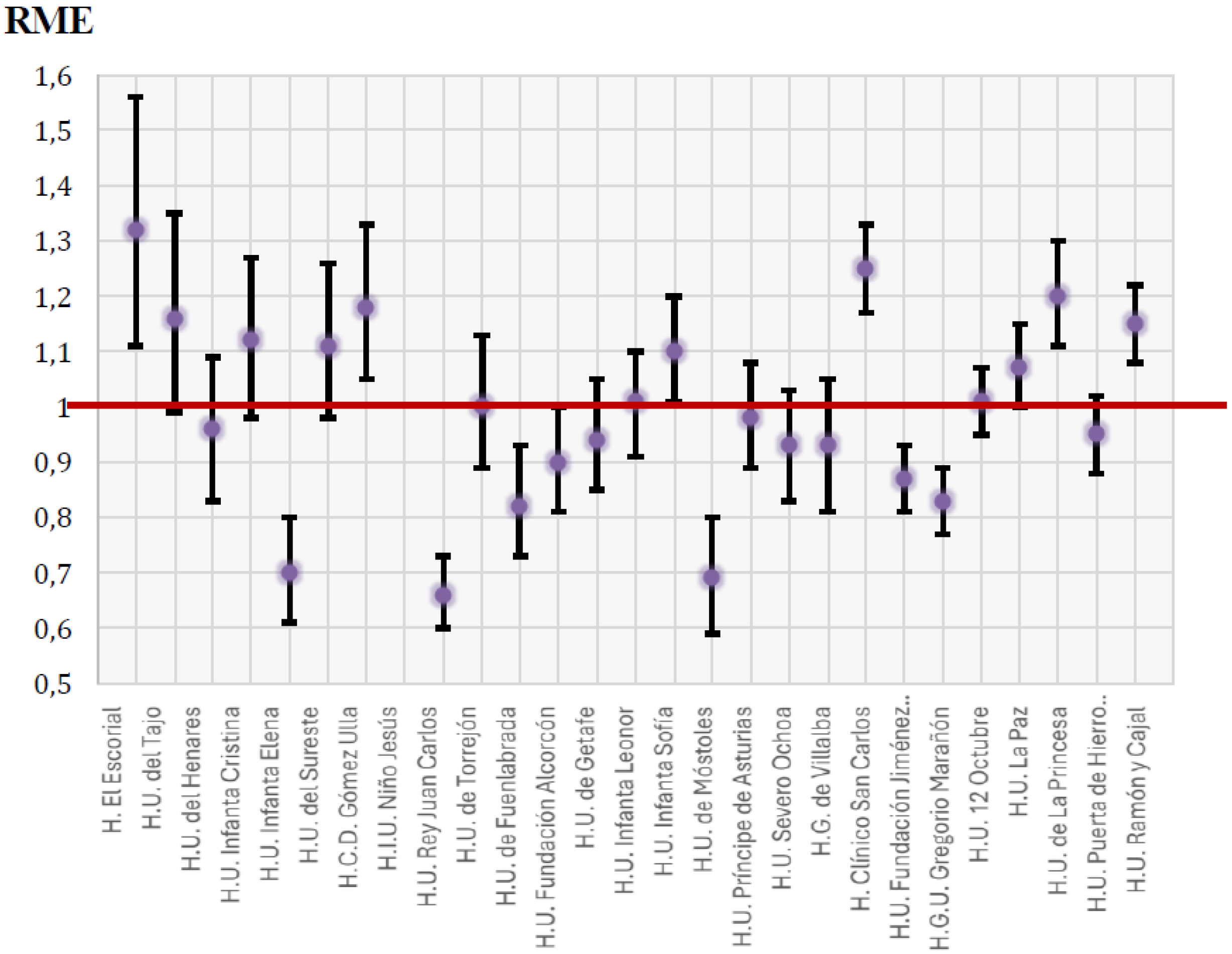
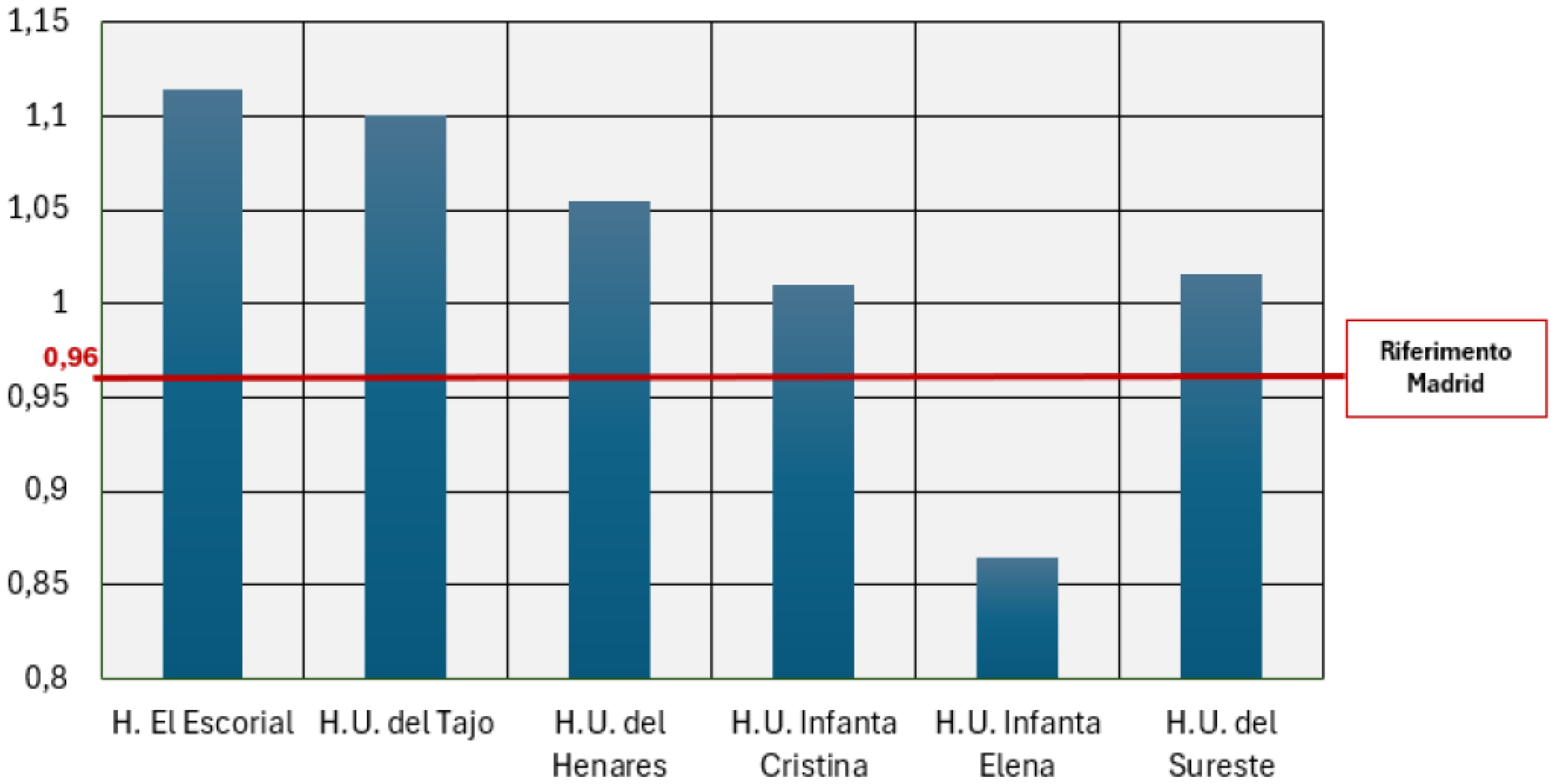
The following graph illustrates the Standardised Mortality Ratio (RME) in the first, second and third group of healthcare facilities under analysis. The aggregate mortality indicator measures the proportion of deaths among patients admitted for six relevant clinical conditions. Reliable data are ensured through the exclusion of hospitals with less than 30 cases, pediatric, psychiatric and intermediate care facilities, as well as palliative care patients. Logistic regression models are applied to correct for the influence of individual factors (age, severity, comorbidities). The Standardised Mortality Ratio (RME/HSMR) is a metric that compares the observed number of deaths with the expected number of deaths, thereby providing a comparative measure of hospital effectiveness. An RME value of less than 1 indicates a lower mortality rate than the Madrid standard, while a higher value indicates a higher mortality rate. The interpretation of the results includes a 95% confidence interval, which allows for the assessment of the statistical significance of the findings.
Figure 3.
RME from 2021 to 2022.
Figure 3.
RME from 2021 to 2022.
An analysis of data from 2017 to 2022 reveals a more pronounced reduction trend in EFQM-certified facilities compared to non-certified facilities. This finding suggests that the adoption of the EFQM model enhances internal organisation and operational efficiency, directly impacting clinical outcomes and contributing to a reduction in hospital mortality.
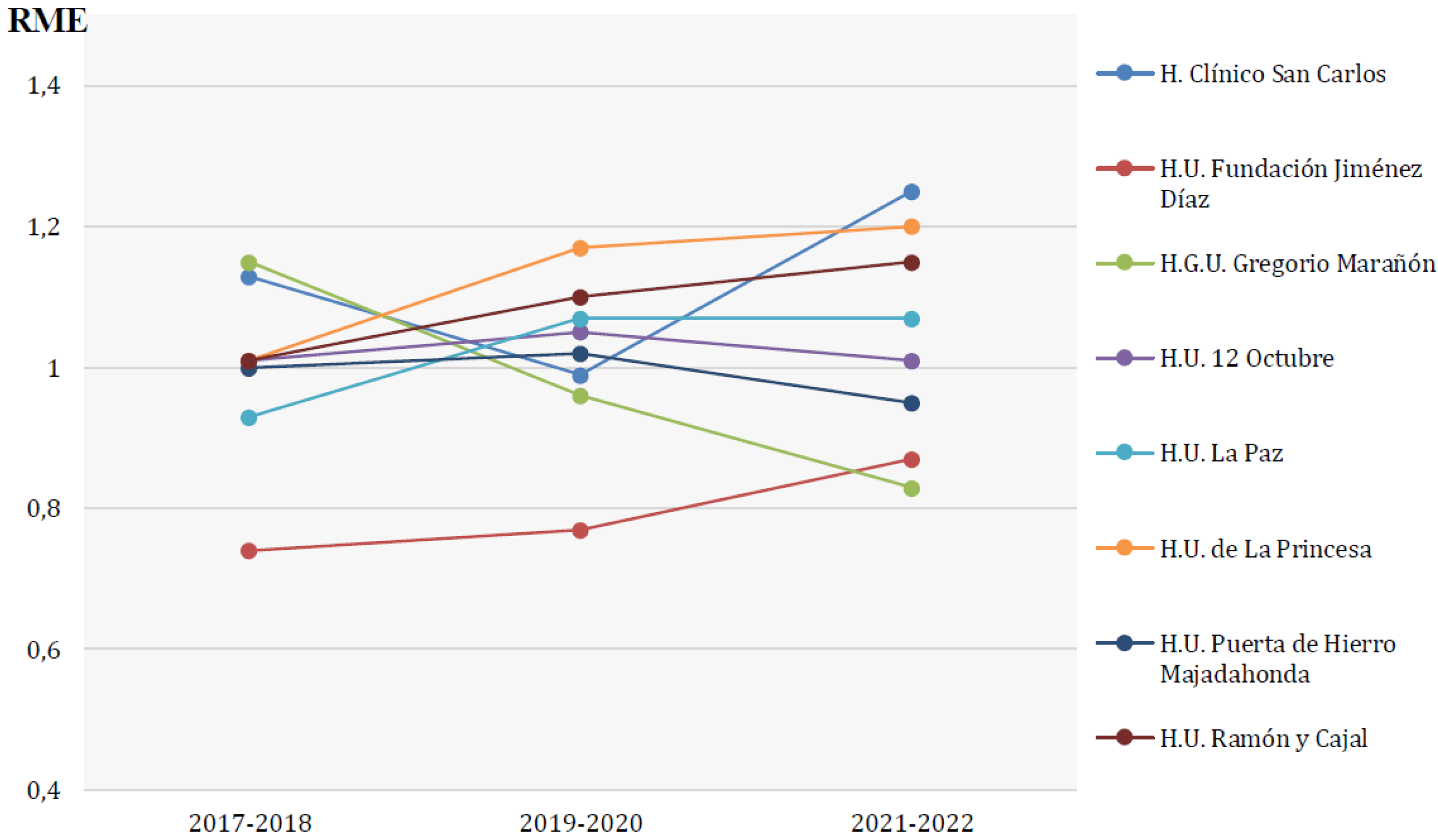
Figure 4.
RME from 2017 to 2022, Cluster 3.
Figure 4.
RME from 2017 to 2022, Cluster 3.
The Standardized Mortality Ratio (RME) does not permit direct comparison of hospitals with each other; however, it enables each facility to be evaluated against the Community of Madrid standard and its performance to be monitored over time. For instance, from 2017 to 2022, the Hospital Universitario Fundación Jiménez Díaz exhibited a slight increase in RME (from 0.74 to 0.87), maintaining its position among the top-performing facilities. Conversely, the Hospital General Universitario Gregorio Marañón exhibits a substantial decline in RME (from 1.15 to 0.83), indicative of an enhancement in the efficacy of care. The Hospital Universitario Puerta de Hierro Majadahonda maintains stability, with a modest decrease observed between 2020 and 2021 (from 1.2 to 0.95).
Analysis Dimensions: to assess the impact of the EFQM model in the hospitals analysed, four dimensions of analysis were identified: efficiency, patient care, humanisation, training and research. Each of these dimensions was explored through specific parameters measuring their performance and effects on healthcare management.
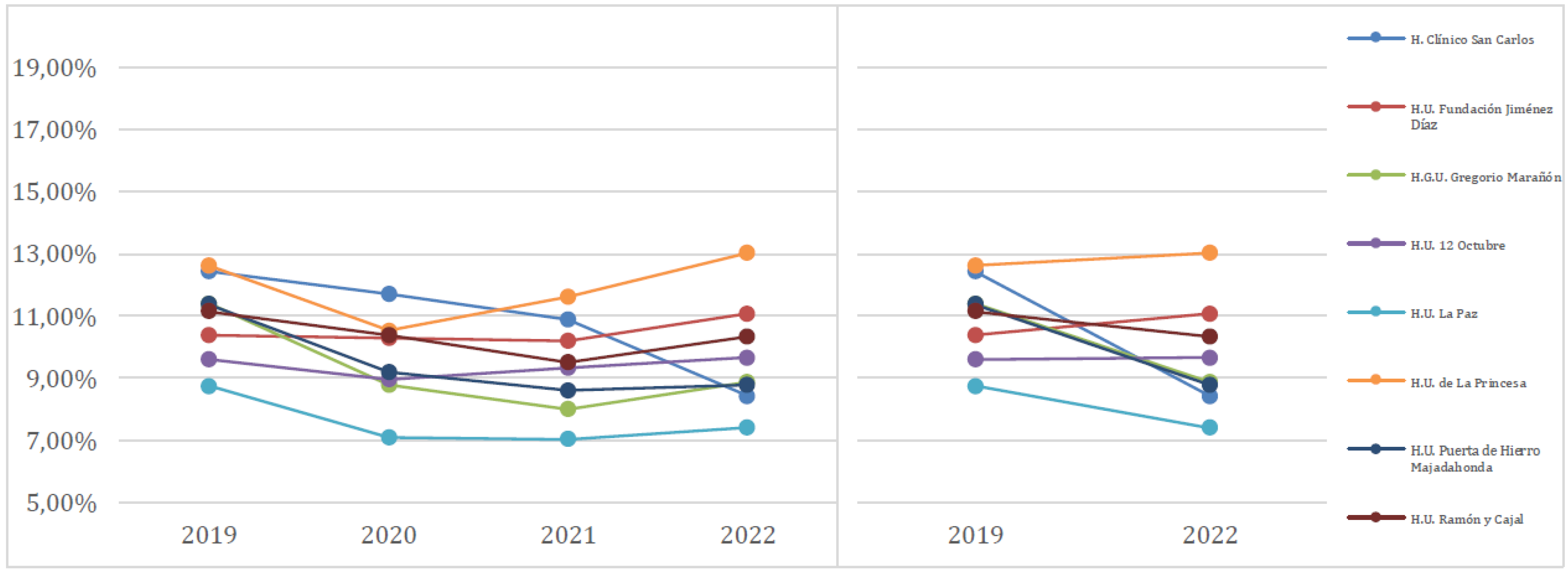
To assess the efficiency of hospital facilities, the following were considered:
- -
Potentially avoidable hospitalisations, which measures the ability of the system to prevent hospitalisations through appropriate outpatient care;
Figure 5.
Potentially avoidable hospitalisations, Cluster 3.
Figure 5.
Potentially avoidable hospitalisations, Cluster 3.
- -
Adjusted Average Length of Stay Index (IEMA), which compares the observed length of stay with the expected length of stay, excluding outliers (a lower value suggests optimal resource management, more effective treatment and more effective discharge planning);
Figure 6.
Adjusted average length of stay Index (IEMA), Cluster 1.
Figure 6.
Adjusted average length of stay Index (IEMA), Cluster 1.
- -
Cost per citizen, assesses health expenditure per capita;
- -
Cost per pack, measures the average cost of prescribed packs of medicines (recognising, of course, that institutions with high levels of care complexity often have higher costs per pack of medicines due to the use of advanced and personalised therapies);
- -
Water and electricity consumption, key indicators of environmental sustainability, measured in relation to hospital admissions and hospital space.
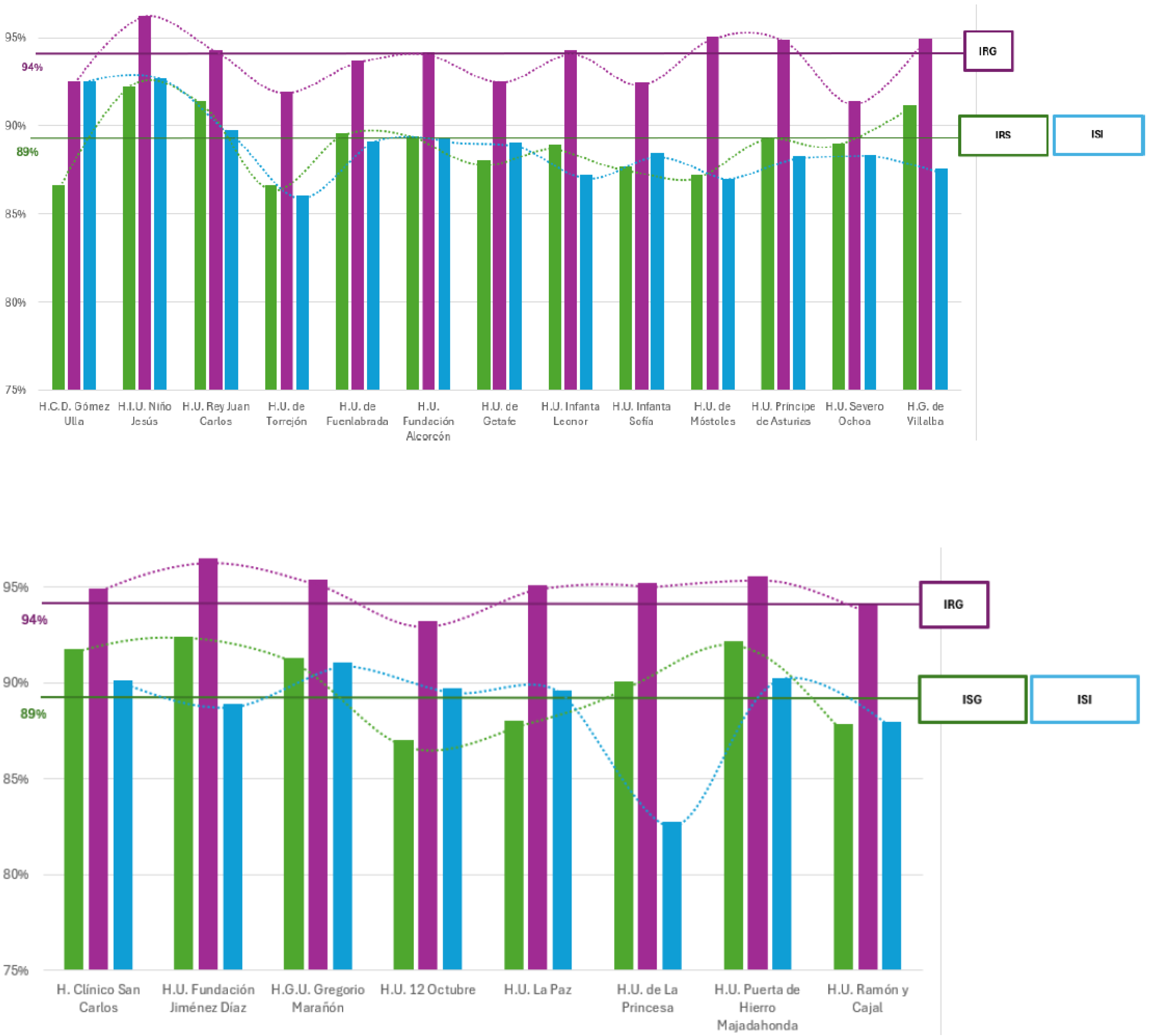
Patient care was analysed using four basic parameters:
- -
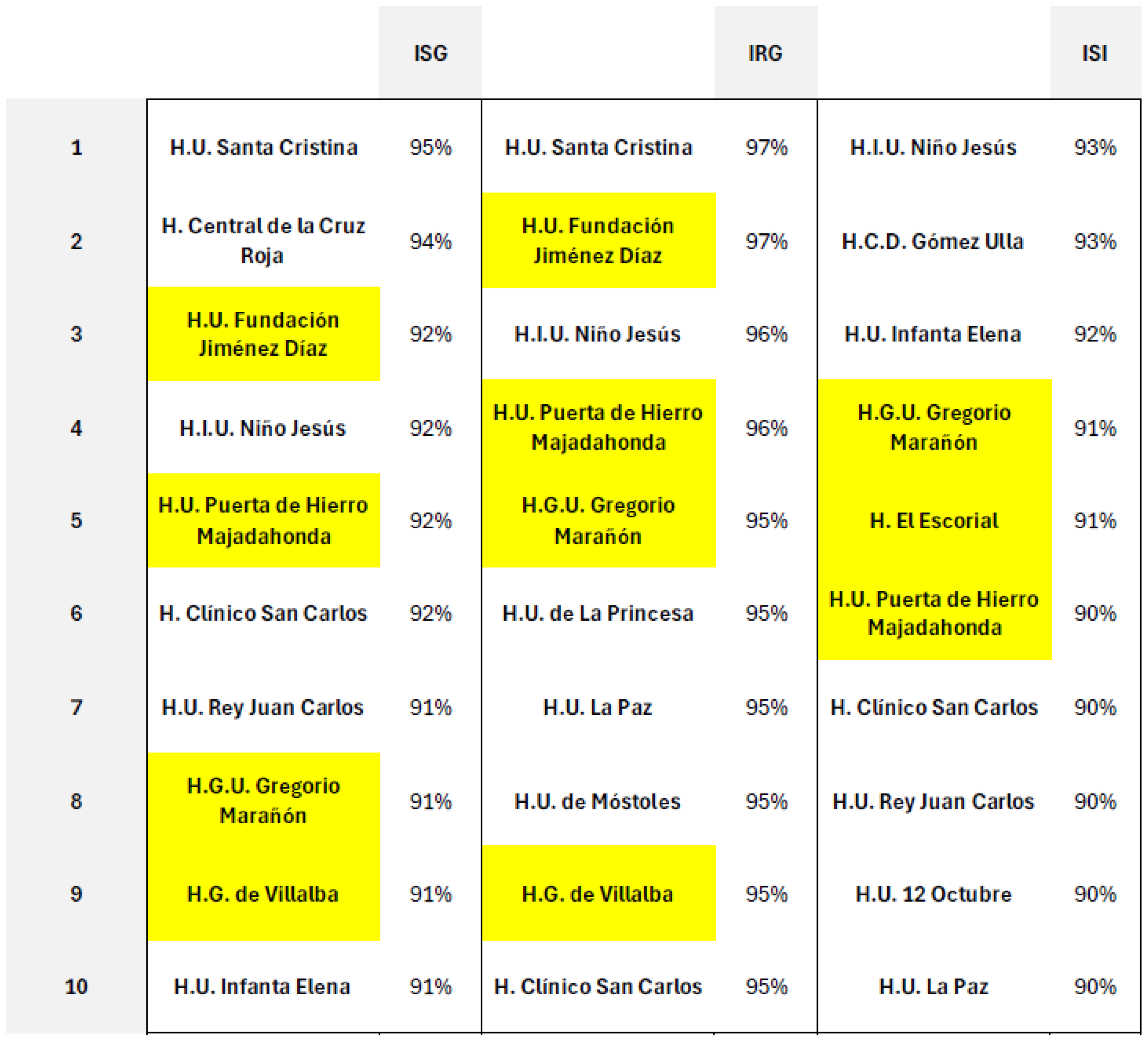
ISG, overall satisfaction index: percentage of patients satisfied with the care received in inpatient, outpatient, ambulatory surgery and emergency room.
- -
IRG Global Recommendation Index: measures the propensity of patients to recommend the service received.
- -
ISI information satisfaction index: assesses the percentage of patients satisfied with the information received on treatment and discharge.
- -
Complaint index: measures the number of complaints received, reflecting any critical aspects of the service
Figure 7.
ISG, IRG, ISI, Cluster 2 and 3.
Figure 7.
ISG, IRG, ISI, Cluster 2 and 3.
Figure 8.
Complaint Index, Cluster 1, 2 and 3.
Figure 8.
Complaint Index, Cluster 1, 2 and 3.
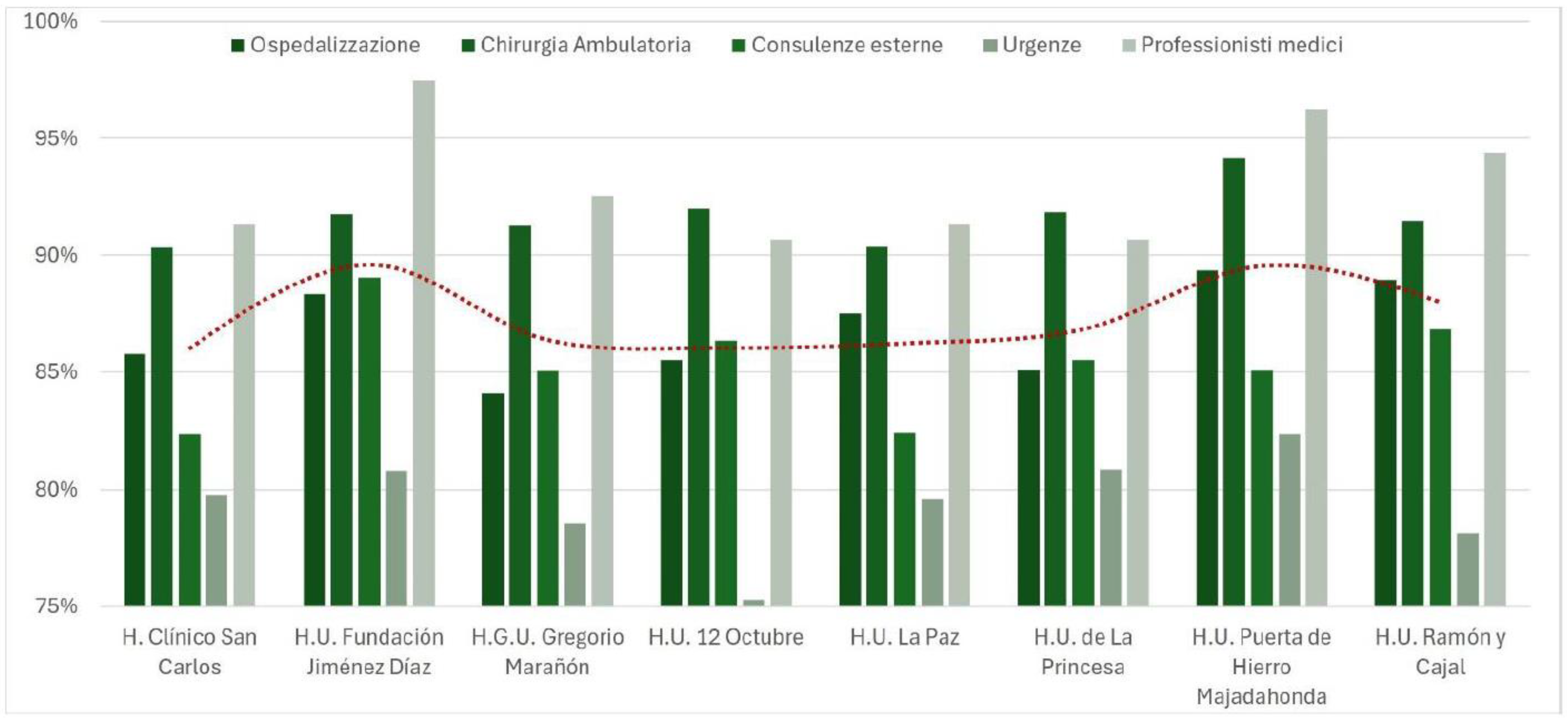
The third significant aspect pertains to the humanisation of care. The EFQM model, with its emphasis on stakeholder engagement and the social value it engenders, fosters a person-centred approach to care that considers not only clinical aspects but also psychological and emotional dimensions. Facilities that have adopted this approach have initiated programmes to enhance communication between healthcare professionals and patients, thereby increasing the transparency and clarity of the information provided. Furthermore, the development of more personalised care pathways has been observed, with the objective of enhancing the patient experience and reducing stress levels. These interventions have resulted in increased trust in healthcare facilities and adherence to proposed treatments.
The humanisation factor was assessed through five key areas:
- Hospitalisation
- Outpatient surgery
- External consultations
- Emergencies
- Medical professionals
In the context of hospitalisation, seven key aspects were considered:
1. Treatment and friendliness of operators
2. Quality of information provided
3. Time and dedication shown by health personnel
4. Respect for patient privacy
5. Maintenance of silence during night hours
6. Pain management
7. Involving the patient in decisions about his/her own care
Figure 9.
Humanisation of care, Cluster 3.
Figure 9.
Humanisation of care, Cluster 3.
Finally, the impact on training and research is to be assessed. The commitment of healthcare facilities in these terms was evaluated through the following metrics:
- -
Accreditation for specialist training and number of places available.
- -
Number of research projects and, especially, number of projects approved by the reference committees, number of active projects during the reference year and number of new projects (started during the evaluation period). A high number of projects indicates a growing commitment to innovation and scientific production.
Figure 10.
number of places available for each structure.
Figure 10.
number of places available for each structure.
6.1. Hospital Index 2023
The Hospital Excellence Index (IEH), a publication undertaken on an annual basis by the Instituto Coordenadas de Gobernanza y Economía Aplicada, is recognised as a leading instrument for the evaluation of hospital performance within Spain. The index is formulated on the basis of a range of criteria, including, but not limited to, quality of care, management efficiency, technological innovation, and patient satisfaction. The index is formulated based on data collected through over 2,000 interviews with healthcare professionals and a performance analysis of various hospitals. In 2023, the Hospital Universitario Fundación Jiménez Díaz retained its leading position for the eighth consecutive year, showcasing a management model that integrates clinical excellence, reduced waiting times, and optimised resource utilisation.
The adoption of the EFQM model by HUFJD has been identified as a significant factor in the hospital's success, enabling the development of a strategic and sustainable approach to healthcare management. The institution's integration of its missions of care, teaching, and research has been recognised with prestigious accolades, including the EFQM Global Award. The EFQM framework has been instrumental in promoting continuous quality improvement, stakeholder engagement, and the implementation of technological and organisational innovations. Significant investments have been made in advanced technologies, including the Da Vinci robotic surgery system and intraoperative MRI, enhancing diagnostic and therapeutic effectiveness. Additionally, the hospital has developed certified environmental and energy management systems (ISO 14001 and ISO 50001), demonstrating a strong commitment to sustainability.
The experience of HUFJD demonstrates the potential of the EFQM model to function as a strategic instrument for the enhancement of hospital performance. The integrated approach to quality adopted by HUFJD has not only led to improvements in clinical outcomes, but also resulted in the strengthening of staff and patient engagement, thereby fostering a culture of excellence and innovation. These results indicate that the adoption of a structured quality management model has the capacity to transform healthcare facilities into more resilient organisations, capable of addressing sector challenges and ensuring a sustainable and efficient healthcare service in the long term.
7. Discussion
The findings of the analysis indicate that the implementation of the EFQM Model has been proven to engender quantifiable advantages with regard to operational efficiency, the quality of care provided and the management of resources. EFQM-certified hospitals have demonstrated a greater capacity to adapt to change, a reduction in the number of avoidable hospital admissions and more efficient management of hospital stays. The data suggest that the EFQM is not merely a certification tool, but rather a strategic governance model that has the capacity to enhance the quality of care provided and optimise the use of resources. A further benefit of certification is the adoption of more efficient practices in energy and drug consumption by EFQM facilities, thus leading to economic and environmental sustainability.
In the domain of operational efficiency, the findings indicate that EFQM-certified facilities demonstrate a tendency to exhibit superior performance in comparison to non-certified hospitals, particularly with respect to the management of hospital stays and the optimisation of healthcare expenditures. The decline in the average hospitalisation rate and potentially avoidable hospitalisations suggests a heightened capacity for organisation and planning, accompanied by a more effective management of human and material resources. Furthermore, the analysis of the cost per pack indicates a heightened focus on the judicious utilisation of pharmaceuticals, thereby ensuring cost containment without compromising the quality of care.
In terms of patient care, the analysis demonstrates that the IRG generally exhibits a higher value in comparison to the ISG and ISI. This discrepancy is attributable to the characteristics of the inquiry and the specificity of the employed indicators. The ISG, being based on a detailed assessment of the entire care pathway, leads patients to consider both positive and negative aspects, such as disservices or expectations, and the resulting scores are more moderate; the IRG, on the other hand, offers a more synthetic and comprehensive view, influenced not only by direct experience but also by emotional and reputational factors, and results in tendentially higher values. Finally, the ISI, which focuses on the quality and clarity of the information received, leads patients to pay more attention to the details of communication. Consequently, any lack of information or perceptions of lack of clarity can have a negative impact on the scores, which remain lower than on the IRG. The latter, in fact, reflects a more general perception of the experience. The following is a ranking of the top ten hospitals in Madrid, classified according to the indicators described above:
Figure 11.
((Structures highlighted are those with EFQM certification).
Figure 11.
((Structures highlighted are those with EFQM certification).
On the other hand, as far as the complaints index is concerned, the EFQM-certified facilities show significantly lower values of complaints than both the Madrid average and the group average, highlighting excellent performance in this area.
The humanisation of care has been identified as a significant benefit of hospitals adopting the EFQM model. An analysis of indicators relating to the treatment of patients, quality of information and pain management reveals that the person-centred approach is more advanced in certified facilities. The active involvement of the patient in decision-making processes and greater attention to privacy and comfort during hospitalisation are distinctive elements that significantly improve the perceived quality of healthcare.
Finally, facilities that have adopted this approach have also developed structured systems for the professional growth of their staff. These systems include incentivising continuous refresher courses and creating dynamic learning environments. The focus on innovation and continuous improvement has fostered greater integration between clinical activity and scientific research, facilitating the adoption of new technologies and therapeutic methodologies. Moreover, the model has fostered collaboration between different healthcare facilities and academic institutions, creating a favorable ecosystem for sharing knowledge and expertise.
The findings of this study demonstrate that the implementation of the EFQM Model in healthcare facilities can serve as a strategic catalyst for enhancing performance in a sustainable and quality-oriented manner. While the integration of the model necessitates substantial investment in terms of training, organisational culture, and process adaptation, the outcomes underscore its efficacy as an integrated management instrument, adept in guiding hospitals towards enduring operational excellence.
7.1. Survey on Hospital Management Practices in the Italian Healthcare System
The implementation of the EFQM model in Italian healthcare facilities was analysed through a targeted survey conducted on a sample of general managers, quality managers and medical directors, with the aim of understanding the level of relevance attributed to the fundamental principles of the model. The aim of the study was not to measure knowledge of the EFQM model per se, but to assess the extent to which its fundamental principles, independent of any specific framework, are considered relevant and applicable in hospitals. In other words, the survey did not focus on direct knowledge of the EFQM model, but sought to assess the extent to which healthcare organisations already consider the principles on which the model is based to be central, regardless of their familiarity with it, in order to determine whether there is a real interest in deepening it and what the main organisational, cultural and structural barriers to its implementation might be. In particular, the survey identified critical issues relating to change management, the need for dedicated resources and potential difficulties in adapting to current National Health Service regulations.
In order to successfully adopt the EFQM model in the healthcare context, it is vital that leadership is actively involved in a gradual implementation process. Indeed, it is essential that the adoption of the model is supported by a shared strategic vision and a concrete commitment at the decision-making level, so the transformation must start from the top. Staff training is equally crucial; without adequate training and awareness of the principles of quality and continuous improvement, the model risks remaining a formal exercise without tangible impact. To ensure the optimal effectiveness of the EFQM, it is imperative that it be integrated into the strategic planning of healthcare facilities, aligning it with national and regional directives on the quality and sustainability of healthcare services.
To facilitate this implementation, it is imperative to employ the RADAR framework, as it provides a structured method to measure the performance of healthcare facilities and guide continuous improvement. It would be appropriate to rewrite the RADAR points from a healthcare perspective, adapting them to the specific needs of hospitals, with the aim of creating a practical and detailed guide that translates general guidelines into concrete actions, applicable in different healthcare contexts. Such an approach would facilitate greater measurability of the impact of EFQM, ensuring a more effective, systematic application that can produce significant improvements in the management and delivery of healthcare services.
8. Conclusions
The healthcare sector today faces complex challenges that require management models capable of ensuring quality, efficiency and sustainability. In this context, the EFQM model presents itself as a tool of extraordinary importance, capable of transforming healthcare organisations by promoting profound and systematic change. It is not just a framework for quality improvement, but a management philosophy that allows structures to redefine their identity by aligning their operational objectives with a long-term strategic vision.
The survey carried out in this study highlighted the interest of health care organisations in adopting the EFQM model, as well as some critical issues to be addressed, such as the limited knowledge of the model in many contexts and the need to involve staff. Nevertheless, the results show that EFQM is perceived as a tool that can bring about significant improvements in quality of care, operational efficiency and sustainability. The international experience and emerging evidence confirm that EFQM provides a structured and adaptable framework for planning, managing, and monitoring performance across different healthcare contexts.
What makes EFQM particularly suitable for the healthcare context is its flexibility and ability to adapt to the specificities of of different organisational and regulatory frameworks. Unlike other more prescriptive models, EFQM invites organisations to critically reflect on their practices promoting self-assessment as the foundation for continuous improvement. Through a holistic approach, the model integrates fundamental aspects such as leadership, organisational culture, innovation and social responsibility, providing a broad and structured view of excellence. Implementing the EFQM model requires a cultural shift, starting from leadership and progressively involving all levels of the organisation. This process enables the creation of a culture of continuous improvement that not only ensures more effective clinical outcomes but also promotes greater cohesion and involvement among staff. At the same time, the model encourages the adoption of advanced monitoring tools, such as the RADAR framework, which makes it possible to measure the effectiveness of the approaches adopted and ensure a continuous cycle of improvement.
Looking to the future, EFQM offers a scalable and universal approach that can be applied in any healthcare system. To explore its feasibility and impact, this study has used the Italian healthcare system as a case study, leveraging its complexity and regional variability as a testing ground. However, the findings are not limited to the Italian context; rather, they highlight the wider applicability of EFQM as a driver of excellence in healthcare management globally. The model enables healthcare organisations to develop and implement a clear and ambitious strategy that creates value for all stakeholders, fostering resilience and adaptability in an ever-evolving healthcare landscape. Tangible benefits extend beyond immediate improvements in clinical performance, reinforcing EFQM’s potential to redefine the role of healthcare organisations worldwide as key players in a system focused on excellence and continuous improvement.
References
- Abdallah, A. , "Implementing quality initiatives in healthcare organizations: drivers and challenges", International Journal of Health Care Quality Assurance, 2014.
- AGENAS, “Supporto all’implementazione dei programmi di accreditamento regionali”, 2012.
- Alkhurayji, K.S.; Alsuhaimi, A.; Alangari, H.; Alrayes, S.A.; Alumran, A. Factors Associated with Non-Compliance with Healthcare Accreditation in Saudi Arabia: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 580. [Google Scholar] [CrossRef] [PubMed]
- Bonazza Alessandro, “The Right to Health: the Italian Health Service”, 2020.
- Bukvič, V. , "The European Foundation for Quality Management (EFQM) Model as an Exquisite Tool for the Analysis of Business Excellence and Its Use in the Healthcare Industry", Medical Research Archives, 2023.
- “Certificaciones, acreditaciones, premios y reconocimientos en hospitales: Año 2022”; Madrid: Consejería de Sanidad, Servicio Madrileño de Salud, 2023.
- European Commission: Directorate-General for Health and Food Safety, "State of health in the EU – Synthesis report 2023", Publications Office of the European Union, 2023.
- Favaretti, C. , De Pieri P., Torri E., Guarrera G., Fontana F., Debiasi F., Flor L., "An EFQM excellence model for integrated healthcare governance", International Journal of Health Care Quality Assurance, 2015.
- GIMBE, " 7° Rapporto GIMBE sul Servizio Sanitario Nazionale ", GIMBE evidence for health.
- Guspianto, G. , Asyary, A & Ibnu, I. (2021). “Integration model of total quality management and six sigma in hospital quality management.” Management Science Letters, 11(4), 1439-1442.
- Hosseini, S.; Aalikhani, A. Investigating the level of customer oriented in an excellence business organization through EFQM method. Management Science Letters 2014, 4, 2371–2374. [Google Scholar] [CrossRef]
- Kamal, E. , "Implementation of business excellence models in healthcare for quality assessment: a systematic review", Glob J Qual Saf Healthc, 2023.
- Matthies-Baraibar, *!!! REPLACE !!!*; et al. , "Is organizational progress in the EFQM model related to employee satisfaction?", BMC Health Services Research, 2014.
- OECD/European Commission, "Health at a Glance: Europe 2024: State of Health in the EU Cycle", OECD Publishing, Paris, 2024.
- OECD/European Observatory on Health Systems and Policies, "Italia: Profilo della sanità 2023, State of Health in the EU", OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels, 2023.
- Observatorio de Resultados del Servicio Madrileño de Salud, "Undécimo Informe de Hospitales 2020-2022", Dirección General de Humanización, Atención y Seguridad del Paciente, Consejería de Sanidad.
- Proietti, S. , Cesarotti V., Lecce M., Fiocco E., "Application of the EFQM Model in the Healthcare Sector: Analysis and Practical Implications".
- Sappor, E.E.; Chakraborty, R. “Exploring Staff Perceptions of the Management of Clinical Trials and Its Impact on Enhancing Health Service Delivery”. Hospitals 2025. [CrossRef]
- Sistema de Información y Análisis de la Prestación Farmacéutica de la Comunidad de Madrid EFQM, “The Efqm Un SDG Lens: Breakdown Of The 17 Goals & 169 Targets”.
- Tradori, V. , Brescia V., Biancone P., “Dal concetto di qualità multidisciplinare in sanità a un modello di verifica”, Pavia, febbraio 2020.
- Van Schoten, S. , de Blok S., Spreeuwenberg P., Groenewegen P., Wagner C., "The EFQM Model as a framework for Total Quality Management in healthcare: results of a longitudinal quantitative study", International Journal of Operations & Production Management, 2016.
- Yousefinezhadi, T. , Mohamadi E., Safari Palangi H., Akbari Sari A., "The Effect of ISO 9001 and the EFQM Model on Improving Hospital Performance: A Systematic Review", Iran Red Crescent Med J, 2015.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).