1. Introduction
Total Knee Arthroplasty (TKA) is a widely accepted and increasingly common surgical intervention for patients with end-stage osteoarthritis or severe degenerative joint disease. Its primary objective is to alleviate pain, restore joint function, and improve quality of life. As the global aging population grows, the number of TKA procedures continues to rise, placing increasing emphasis on optimizing postoperative care and rehabilitation pathways to maximize patient outcomes.
Postoperative rehabilitation is critical to the success of TKA, influencing both the speed and quality of recovery. Traditional in-clinic rehabilitation programs, while effective, are resource-intensive and may not be feasible for all patients due to factors such as geographic distance, socioeconomic barriers, and limitations in mobility. Moreover, hospital-based rehabilitation alone often does not guarantee long-term functional success, as many patients struggle with adherence and engagement in prescribed exercise regimens at home [
1].
In response to these challenges, the integration of sensor technologies into rehabilitation paradigms has emerged as a promising advancement. These technologies span from wearable motion tracking systems and inertial sensors (IMUs) to smart implants, mobile health (mHealth) platforms, and AI-enhanced feedback tools. Wearable sensors are now capable of capturing real-time data on patient movement, gait patterns, and range of motion, offering valuable feedback for clinicians and patients alike [
2].
In parallel, the rise of telerehabilitation platforms—such as ReHub® and BPMpathway—has provided a feasible and effective way to extend care into the patient’s home, offering continuous engagement and monitoring without requiring physical presence in a clinic [
3]. These systems not only improve compliance but also reduce healthcare costs and enhance access for remote or underserved populations. (Nuevo et al., 2024; Hong et al., 2024; Bell et al., 2020).Home-based rehabilitation systems embedded with sensors have been shown to be safe and non-inferior to traditional models in terms of outcomes [
4]. Additionally, intelligent systems powered by machine learning and real-time analytics have begun to redefine how patient recovery is assessed. For example, advanced platforms that incorporate algorithmic analysis of wearable sensor data have demonstrated high accuracy in predicting rehabilitation progression and customizing therapy plans accordingly [
5]. These tools bridge the gap between clinician supervision and patient self-management, enabling hybrid models of care.
In addition, on the other hand smart implant technologies are increasingly utilized intraoperatively and postoperatively. These devices provide surgeons with real-time feedback on ligament balance and alignment during surgery, potentially reducing complications such as arthrofibrosis [
6]. App-controlled systems for neuromuscular electrical stimulation have also been employed to support muscle recovery and reduce rehabilitation costs [
7].r, research continues to explore the impact of gamified rehabilitation platforms and portable systems that are both low-cost and highly engaging for patients. Such solutions can significantly improve adherence by increasing motivation and introducing real-time feedback mechanisms [
8]. Systematic reviews further affirm the effectiveness of digital interventions, highlighting their diagnostic accuracy and potential to enhance rehabilitation outcomes [
9].
In summary, the integration of sensors and intelligent monitoring systems into TKA rehabilitation represents a paradigm shift in postoperative care. These technologies address long-standing challenges in patient compliance, access, and personalization of therapy, thereby supporting a more holistic, data-driven, and patient-centered recovery model.
2. Materials and Methods
This overview paper adopts a narrative review approach, aimed at summarizing and synthesizing current developments in sensor technologies applied to rehabilitation after Total Knee Arthroplasty (TKA). The selection of literature was guided by a combination of structured and exploratory strategies.
A targeted literature search was conducted using PubMed, Scopus, Web of Science, and Google Scholar databases, focusing on studies published between 2017 and 2024, to incorporate the most recent literature on a relatively new issue.
Keywords included: “Total Knee Arthroplasty,” “rehabilitation,” “wearable sensors,” “telerehabilitation,” “mHealth,” “smart implants,” and “artificial intelligence in physiotherapy.”
Inclusion criteria:
Peer-reviewed original articles or systematic reviews.
Studies involving sensor-based rehabilitation tools for TKA.
Research that evaluated clinical, functional, or usability outcomes.
Exclusion criteria:
1. Non-peer-reviewed sources (e.g., editorials, letters).
2. Studies Focusing Solely on Surgical Techniques Without Post-Operative Rehab Focus
A total of 14 high-quality studies were selected for this review, comprising randomized controlled trials (RCTs), pilot studies, systematic reviews, and clinical validation research. The findings were categorized thematically across clinical applications, technology types, barriers, and future directions.
3. Challenges and Limitations in TKA Rehabilitation
Although Total Knee Arthroplasty (TKA) is a widely successful surgical intervention, its long-term outcomes are heavily influenced by the quality and consistency of postoperative rehabilitation. However, several systemic, technical, and behavioral challenges compromise the effectiveness of traditional rehabilitation protocols. These barriers are particularly evident in home-based recovery, which is becoming increasingly important as healthcare systems prioritize cost-effectiveness and outpatient care models.
3.1. Home Monitoring Limitations
A fundamental challenge in post-TKA rehabilitation is the limited monitoring capacity when patients are discharged from hospital settings. Without direct supervision, it becomes difficult to assess whether patients are performing exercises correctly or progressing as expected. In studies such as those by Pua et al. (2024), patients under hospital-based care showed more consistent recovery metrics compared to those in unsupervised environments, largely due to the lack of real-time feedback and clinician oversight [
1]. Similarly, Bell et al. (2020) noted that while remote systems offer great promise, their implementation often lacks adequate support mechanisms for patients to report issues, leading to underreported complications or incorrect usage [
10].
3.2. Variability in Patient Compliance
Patient adherence to rehabilitation programs is another persistent problem. Compliance varies due to multiple factors: pain perception, motivation, cognitive function, and ease of performing prescribed exercises. In a randomized controlled trial, Nuevo et al. (2024) demonstrated that even when telerehabilitation systems like ReHub® were deployed, consistent engagement was a challenge for some patients, particularly older adults or those unfamiliar with digital tools [
11]. On the same lines, studies like the Salehian et al. (2024) emphasized that home-based telerehabilitation systems are only as effective as the patient’s willingness and ability to follow structured routines. These systems require intrinsic motivation, which may fluctuate due to psychosocial stressors or lack of accountability mechanisms [
4]. On the same lines, Ramkumar et al. (2019) supported these findings through a machine learning-based remote monitoring platform which, while accurate in tracking data, showed that usage consistency varied significantly between patients [
12]. This highlights that even the best tools require strong user engagement to yield meaningful outcomes.
3.3. Lack of Individualized Therapy
Conventional rehabilitation often follows a one-size-fits-all model that does not account for inter-individual variability in healing, physical condition, or baseline function. This lack of personalization has been identified as a major limitation in optimizing recovery outcomes. In a systematic review, Raje et al. (2024) pointed out that most digital rehabilitation interventions failed to adjust protocols based on dynamic patient feedback or sensor-based metrics, thereby limiting their effectiveness [
9]. The same issue was explored by Xie et al. (2024), who demonstrated in their randomized controlled trial that intelligent monitoring systems led to superior outcomes primarily due to their ability to adapt therapy in real-time based on continuous data analysis [
13]. Van de Ven et al. (2023) emphasized that variability in gait entropy and peak frequency during treadmill recovery highlights the unique biomechanical recovery path of each patient, underlining the need for adaptive feedback models. Building on this, their 2023 study demonstrated that post-operative gait recovery is characterized by high individual variability in both motion complexity (sample entropy) and peak frequency, indicating that motor control does not follow a uniform pattern across individuals. This finding reinforces the importance of personalized rehabilitation approaches that utilize real-time biomechanical data to tailor therapy. Furthermore, in a complementary study, van de Ven et al. (2024) examined entropy in lateral body sway and confirmed that movement predictability also varies substantially among patients, further supporting the value of dynamic, sensor-informed feedback systems. Together, these findings provide compelling evidence for integrating adaptive feedback models in post-TKA rehabilitation to better align with each patient’s neuromuscular profile and optimize recovery outcomes.
3.4. Cognitive Load & Technology Literacy
An often overlooked but significant barrier involves the cognitive demands and technology literacy required to operate some sensor-based or telehealth systems. Hong et al. (2024) observed that elderly populations, who constitute the majority of TKA recipients, sometimes experienced difficulty navigating platforms like BPMpathway, despite its therapeutic potential [
14]. This demographic-specific challenge must be considered in the design of future solutions.
4. Sensor Technologies for TKA Rehabilitation
In recent years, the integration of sensor technologies into the rehabilitation process following Total Knee Arthroplasty (TKA) has revolutionized how clinicians monitor progress and deliver individualized care. These technologies offer objective, quantifiable insights into patient recovery, particularly in home-based and remote care settings. The four most prominent categories of such technologies include wearable sensors, smart implants, pressure-sensing systems, and mobile health (mHealth) platforms.
4.1. Wearable Sensors (IMUs, Accelerometers, Gyroscopes)
Wearable sensors represent one of the most widely studied and applied technologies in post-TKA rehabilitation. Inertial Measurement Units (IMUs), composed of accelerometers, gyroscopes, and sometimes magnetometers, are commonly attached to the lower limbs to assess joint angles, gait parameters, and overall mobility. These sensors enable high-resolution monitoring of range of motion (ROM), step count, and even biomechanical symmetry during walking.
Van de Ven et al. (2023) utilized IMU sensors to track changes in sample entropy and peak frequency during treadmill walking after TKA, demonstrating their value in capturing nuanced gait dynamics throughout recovery [15]. Similarly, Huang et al. (2020) confirmed that wearable devices could effectively evaluate ROM progression, making them a viable alternative to clinic-based assessments [16]. Despite their clinical potential, challenges remain related to calibration, placement standardization, and data interpretation. Still, the technology has matured to a point where it can provide reliable metrics outside clinical settings.
4.2. Smart Implants
Smart implants are an emerging field in orthopedics, combining traditional prosthetic components with embedded sensors. These intraoperative sensors measure parameters like joint alignment, ligament tension, and intra-articular pressure in real time, guiding surgeons to achieve optimal balance during TKA procedures. For example, Geller et al. (2017) demonstrated that the use of electronic sensor devices during surgery significantly reduced the incidence of arthrofibrosis, a common postoperative complication linked to improper ligament balancing [
6]. Furthermore, smart implants continue to evolve with biocompatible wireless components that allow postoperative monitoring without additional surgical intervention. Although promising, the application of such implants remains limited by high cost, surgical complexity, and limited long-term outcome data. Nonetheless, they offer a promising solution for high-risk or complex TKA cases.
4.3. Pressure Sensing Insoles & Mats
Pressure sensors embedded in insoles or pressure mats are another important category, particularly useful for assessing load distribution and gait asymmetries. These systems can measure plantar pressure profiles and ground reaction forces, which are critical for understanding compensatory movements and identifying abnormal gait patterns. While not as prominently featured in the recent clinical trials provided, Ramkumar et al. (2019) included ground force and motion sensors as part of their machine learning-enhanced monitoring platform, helping identify trends in rehabilitation progress across diverse patient groups [
12]. Such sensors are most often used in controlled research environments but are becoming increasingly accessible for clinical and home use. They are especially beneficial when paired with real-time feedback interfaces to guide patients during exercise sessions.
4.4. Mobile Health (mHealth) & Smartphone-Based Tools
Mobile health platforms and smartphone apps are playing an increasingly critical role in enabling remote monitoring, coaching, and feedback for TKA patients. These solutions often integrate data from wearable sensors allowing clinicians to track progress and modify rehab plans accordingly.
The ReHub® platform, evaluated by Nuevo et al. (2024), exemplifies how mHealth tools can support home-based rehabilitation with structured routines, video guidance, and performance analytics [
11]. Similarly, Salehian et al. (2024) demonstrated the feasibility of a home-based tele-rehabilitation system that required only basic patient interaction with a guided interface [
4]. In more advanced applications, Ramkumar et al. (2019) validated a wearable and smartphone-connected platform enhanced by machine learning to predict and monitor recovery trends in real time [
12]. In conclusion, mobile systems offer scalable, cost-effective solutions and are especially valuable in rural or underserved areas. However, barriers such as internet access, digital literacy, and data privacy remain challenges to widespread adoption.
5. Clinical Applications of Sensors
Sensor-based technologies have transformed the clinical landscape of post-operative rehabilitation for Total Knee Arthroplasty (TKA), enabling precise, real-time, and patient-centered care. By capturing kinematic and kinetic data, these systems allow clinicians to monitor and guide recovery in ways that was previously impossible with traditional subjective assessments. The main clinical applications of sensor technologies in TKA rehabilitation include mobility assessment, range of motion (ROM) monitoring, gait analysis, and real-time feedback delivery.
5.1. Mobility Assessment
One of the primary applications of wearable sensors is the assessment of mobility, especially during the early recovery phase. These sensors track spatiotemporal parameters such as step count, walking speed, cadence, and joint angles, which offer a reliable picture of a patient’s functional status. In a study by van de Ven et al. (2023), inertial sensors were used to track changes in gait complexity via sample entropy and peak frequency analysis during treadmill walking. These advanced metrics revealed distinct recovery patterns that could not be captured through conventional observation alone [15]. Similarly, Xie et al. (2024) reported that intelligent monitoring systems improved both mobility outcomes and therapy adherence by delivering real-time feedback on movement quality [
13]. These systems are especially beneficial for detecting subtle deficits in mobility that may predispose patients to falls or asymmetrical gait, enabling proactive therapeutic interventions.
5.2. Monitoring Range of Motion (ROM)
Another crucial parameter for TKA recovery is the restoration of joint ROM, which is directly linked to a patient’s ability to return to daily activities. Traditionally measured using manual goniometers in clinical settings, ROM can now be tracked continuously and objectively through wearable or portable sensors. Huang et al. (2020) utilized a sensor-based home rehabilitation system that accurately monitored improvements in knee flexion and extension angles. The system facilitated early detection of ROM plateaus and guided clinicians in adapting rehabilitation plans in real time [16]. Likewise, Bell et al. (2020) demonstrated that patients using a portable home system experienced consistent ROM gains that aligned closely with in-clinic standards [
10]. These findings underscore the utility of sensor-driven ROM monitoring not only for convenience but also for improving clinical precision.
5.3. Gait Anomaly Detection
Gait abnormalities such as limping, asymmetry, or abnormal weight distribution are common after TKA and, if left unaddressed, can lead to long-term biomechanical dysfunctions. Sensor-enabled gait analysis allows clinicians to identify these problems objectively and early in the recovery process. In the Ramkumar et al. (2019) study, a machine-learning-based remote monitoring platform analyzed wearable sensor data to detect deviations in gait patterns that correlated with delayed recovery outcomes [
12]. Raje et al. (2024) emphasized in their systematic review that sensor-based assessments significantly improved diagnostic accuracy for gait dysfunctions when compared to traditional observation [
9]. The ability to detect anomalies in real time can dramatically reduce recovery time and prevent compensatory movement patterns that hinder long-term joint health.
5.4. Real-Time Feedback to Patients
One of the greatest strengths of sensor-based systems is the delivery of real-time feedback, which is a powerful tool for improving patient adherence and motivation. Immediate insights into performance help patients self-correct and engage more meaningfully in their rehabilitation programs. Platforms such as ReHub®, as studied by Nuevo et al. (2024), offer structured sessions with real-time visual and auditory feedback to guide patients through exercises at home, leading to significantly improved adherence rates [
11]. On the same lines, Salehian et al. (2024) showed that a home-based tele-rehabilitation platform equipped with real-time feedback led to comparable, if not better, outcomes than traditional physical therapy sessions [
4]. This immediate interactivity enhances patient autonomy and builds confidence, particularly valuable for individuals in remote or underserved areas.
6. Recent Research and Developments
Recent advancements in sensor-based rehabilitation for Total Knee Arthroplasty (TKA) reflect a dynamic and rapidly evolving field that merges orthopedic care with digital health, artificial intelligence, and wearable technologies. These innovations are aimed at enhancing the precision, efficiency, and personalization of rehabilitation protocols both in clinical settings and at home.
One of the most notable trends is the proliferation of intelligent monitoring systems that leverage real-time sensor data to optimize recovery. Xie et al. (2024) conducted a randomized controlled trial evaluating such a system, which significantly improved mobility outcomes and rehabilitation efficiency. The system provided continuous tracking and adaptive feedback, highlighting the clinical potential of AI-assisted monitoring [
13]. In the realm of telerehabilitation, Nuevo et al. (2024) demonstrated that the ReHub® platform—an app-based digital program integrating real-time feedback and structured exercises—was both safe and effective compared to traditional physiotherapy. Patients using the platform showed comparable, and in some cases superior, functional recovery, underscoring the viability of remote interventions [
11]. Parallel studies have validated the feasibility of home-based sensor systems. For example, Salehian et al. (2024) and Hong et al. (2024) explored tele-rehabilitation platforms tailored for elderly patients in diverse geographic contexts, demonstrating excellent safety and patient satisfaction [17].
On the biomechanics front, van de Ven et al. (2023) applied inertial sensors to analyze treadmill gait patterns post-TKA, using advanced metrics such as entropy and frequency spectrum changes. This type of analysis not only deepens our understanding of biomechanical recovery but also enables early identification of abnormal gait trends [15]. Meanwhile, efforts to integrate machine learning into rehabilitation tools are gaining traction. Ramkumar et al. (2019) validated a surveillance platform that combined wearable sensors with predictive analytics to track patient recovery, thus reducing the need for frequent in-person evaluations [
12]. Overall, these developments are reshaping how TKA rehabilitation is delivered and monitored—shifting the focus from reactive, clinic-based care to proactive, data-driven, and remote strategies. As sensor technology becomes more affordable and interoperable, its adoption in routine orthopedic rehabilitation is expected to increase substantially.
7. Limitations and Barriers
Despite the promising advances in sensor-based rehabilitation technologies for Total Knee Arthroplasty (TKA), several critical limitations hinder their widespread clinical adoption and effectiveness. These barriers span technological, economic, demographic, and clinical domains.
7.1. Technological Limitations
One major challenge is the accuracy and consistency of sensor data. Variability in sensor placement, calibration, and movement artifacts can introduce errors in measurements, particularly in unsupervised home environments. van de Ven et al. (2023) highlighted the need for controlled conditions during gait assessments with inertial sensors, as entropy and frequency outputs were sensitive to environmental changes [15]. Raje et al. (2024) noted that many commercial platforms lack standardization in data interpretation, making cross-study comparisons and clinical integration difficult [
9].
7.2. Cost and Accessibility
High costs remain a substantial barrier, especially for low-resource health systems and patients without insurance coverage. While some tools like BPMpathway or ReHub® have shown cost-effectiveness in clinical trials, initial implementation expenses—such as sensors, software licenses, and training—can be prohibitive for smaller clinics [
3]. Additionally, smart implants, though clinically promising, are still limited to niche applications due to their complexity and financial cost, as noted by Geller et al. (2017) [
6].
7.3. Elderly Population & Digital Literacy
Many TKA patients are elderly and may struggle with digital interfaces and device handling. Salehian et al. (2024) observed that a portion of patients required frequent technical support, reducing the independence that remote rehab platforms aim to foster [
4]. Similarly, Msayib et al. (2017) emphasized that cognitive overload and low health tech literacy remain major roadblocks for widespread adoption of intelligent systems [18].
7.4.Data Interpretation and Clinical Integration
A final but crucial barrier is the interpretation and integration of high-volume sensor data into clinical workflows. Clinicians often lack the training or time to analyze raw sensor outputs or to act on AI-generated recommendations. Ramkumar et al. (2019) noted that despite their ML-powered surveillance platform’s potential, success depended on clinician trust and seamless data integration with electronic health records [
12].
8. Future Directions
The integration of advanced sensor technologies in Total Knee Arthroplasty (TKA) rehabilitation marks a paradigm shift in orthopedic care. As current systems evolve, future developments are expected to move toward more intelligent, individualized, and remotely accessible solutions that will empower both clinicians and patients.
AI-Based Personalized Rehabilitation
The findings of this review clearly demonstrate that recovery following Total Knee Arthroplasty (TKA) follows highly individualized trajectories, with significant variability in both gait patterns and patient adherence. Studies such as that of van de Ven et al. (2023) revealed substantial variability in indicators like gait entropy and peak frequency, reinforcing the need for dynamic and personalized feedback models. Similarly, Xie et al. (2024), through a randomized controlled trial, showed that intelligent monitoring systems which adapt therapy in real time based on continuous data analysis result in significantly better functional outcomes compared to static rehabilitation protocols.
In this context, artificial intelligence (AI) emerges as the next pivotal step. The ability of AI-enhanced systems to process sensor-derived data in real time, predict recovery trajectories, and automatically adjust therapy creates the foundation for truly individualized rehabilitation. The platform developed by Ramkumar et al. (2019), which integrated wearable sensors with machine learning algorithms, serves as an early example of this trend, supporting remote patient monitoring while reducing the need for frequent in-person visits.
As these technologies continue to mature, the future of post-TKA rehabilitation is shifting toward smart, interoperable, and remote solutions that can dynamically adapt to the needs of each patient. Achieving this vision will require cross-disciplinary collaboration between engineers, clinicians, and data scientists to develop platforms that are technically robust, clinically meaningful, and human-centered.
9. Conclusions
Sensor technologies have redefined the framework of postoperative recovery following Total Knee Arthroplasty (TKA), providing real-time, objective data that enhances both clinical decision-making and patient autonomy. From wearable IMUs and smart implants to mHealth platforms and AI-powered systems, these tools address persistent challenges in conventional rehabilitation—such as limited supervision, inconsistent adherence, and lack of personalization.
Contemporary evidence confirms that such technologies can reliably monitor mobility, assess range of motion, detect gait anomalies, and deliver immediate feedback. Particularly, studies highlight the clinical value of metrics like gait entropy and peak frequency in capturing the individualized nature of recovery trajectories. Despite remaining limitations—including technical complexity, digital literacy disparities, and barriers to integration—sensor-assisted rehabilitation now represents a validated, patient-centered alternative to traditional models.
By bridging the gap between clinical oversight and self-managed care, sensor-based systems are shaping a more flexible, accessible, and data-driven rehabilitation model. Their increasing adoption affirms their role not merely as supplementary innovations, but as fundamental tools in the advancement of modern rehabilitation practice.
Appendix
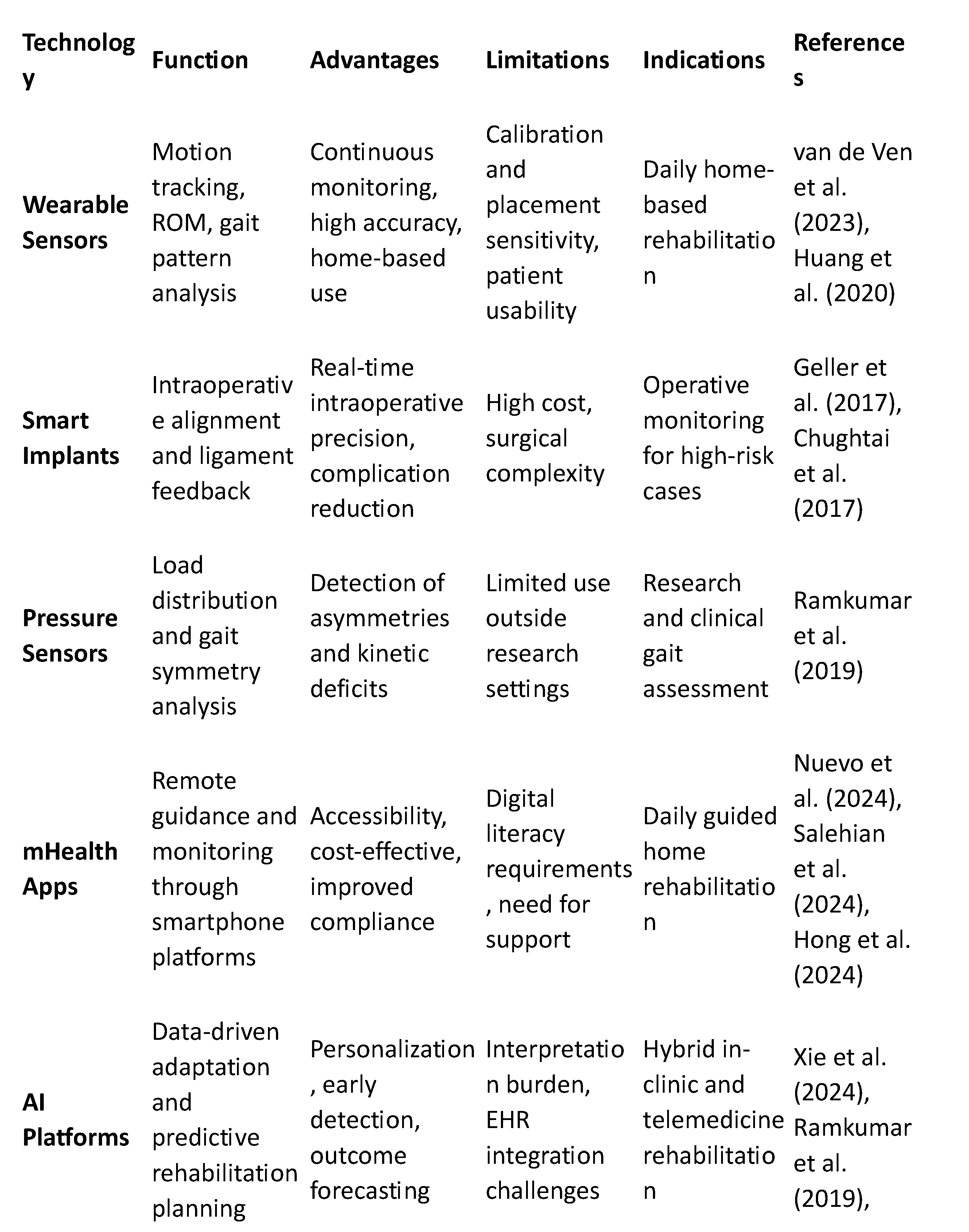
Table A1.
Sensor-Based Rehabilitation Technologies in Total Knee Arthroplasty (TKA).
Table A1.
Sensor-Based Rehabilitation Technologies in Total Knee Arthroplasty (TKA).
References
- Xie W, He M, Zheng S, Li H, Jin H, Ji B, Yang G, Li Y. Clinical application research of intelligent monitoring system for knee rehabilitation: a randomized controlled trial. J Orthop Surg Res. 2024 Aug 13;19(1):477. [CrossRef] [PubMed] [PubMed Central]
- Nuevo M, Rodríguez-Rodríguez D, Jauregui R, Fabrellas N, Zabalegui A, Conti M, Prat-Fabregat S. Telerehabilitation following fast-track total knee arthroplasty is effective and safe: a randomized controlled trial with the ReHub® platform. Disabil Rehabil. 2024 Jun;46(12):2629-2639. [CrossRef] [PubMed]
- van de Ven WAF, Bosga J, Hullegie W, Verra WC, Meulenbroek RGJ. Inertial-Sensor-Based Monitoring of Sample Entropy and Peak Frequency Changes in Treadmill Walking during Recovery after Total Knee Arthroplasty. Sensors (Basel). 2023 May 22;23(10):4968. [CrossRef] [PubMed] [PubMed Central]
- Msayib Y, Gaydecki P, Callaghan M, Dale N, Ismail S. An Intelligent Remote Monitoring System for Total Knee Arthroplasty Patients. J Med Syst. 2017 Jun;41(6):90. [CrossRef] [PubMed]
- Raje S, Shetty AG, Shetty S, Bhuptani B, Arun Maiya G. Application of digital technology in rehabilitation of total knee arthroplasty: A systematic review. J Orthop. 2024 Mar 15;54:108-115. [CrossRef] [PubMed] [PubMed Central]
- Ramkumar PN, Haeberle HS, Ramanathan D, Cantrell WA, Navarro SM, Mont MA, Bloomfield M, Patterson BM. Remote Patient Monitoring Using Mobile Health for Total Knee Arthroplasty: Validation of a Wearable and Machine Learning-Based Surveillance Platform. J Arthroplasty. 2019 Oct;34(10):2253-2259. [CrossRef] [PubMed]
- Huang YP, Liu YY, Hsu WH, Lai LJ, Lee MS. Progress on Range of Motion After Total Knee Replacement by Sensor-Based System. Sensors (Basel). 2020 Mar 18;20(6):1703. [CrossRef] [PubMed] [PubMed Central]
- Pua YH, Yeo SJ, Clark RA, Tan BY, Haines T, Bettger JP, Woon EL, Tan HH, Tan JW, Low J, Chew E, Thumboo J. Cost and outcomes of Hospital-based Usual cAre versus Tele-monitor self-directed Rehabilitation (HUATR) in patients with total knee arthroplasty: A randomized, controlled, non-inferiority trial. Osteoarthritis Cartilage. 2024 May;32(5):601-611. [CrossRef] [PubMed]
- Hong Y, Wang J, Zhang X, Zhao D, He H, Sun M. The effectiveness of home rehabilitation based on BPMpathway exercise rehabilitation system for patients after total knee arthroplasty in China. Int J Orthop Trauma Nurs. 2024 May;53:101062. [CrossRef] [PubMed]
- Liptak MG, Theodoulou A, Kaambwa B, Saunders S, Hinrichs SW, Woodman RJ, Krishnan J. The safety, efficacy and cost-effectiveness of the Maxm Skate, a lower limb rehabilitation device for use following total knee arthroplasty: study protocol for a randomised controlled trial. Trials. 2019 Jan 10;20(1):36. [CrossRef] [PubMed] [PubMed Central]
- Bell KM, Onyeukwu C, Smith CN, Oh A, Devito Dabbs A, Piva SR, Popchak AJ, Lynch AD, Irrgang JJ, McClincy MP. A Portable System for Remote Rehabilitation Following a Total Knee Replacement: A Pilot Randomized Controlled Clinical Study. Sensors (Basel). 2020 Oct 27;20(21):6118. [CrossRef] [PubMed] [PubMed Central]
- Salehian F, Mahmoudzadeh-Sagheb Z, Yoosefinejad AK, Zakerabasali S. A home-based tele-rehabilitation exercise system for patients after knee replacement surgery. BMC Musculoskelet Disord. 2024 Jul 31;25(1):605. [CrossRef] [PubMed] [PubMed Central]
- Chughtai M, Piuzzi N, Yakubek G, Khlopas A, Sodhi N, Sultan AA, Nasir S, Yates BST, Bhave A, Mont MA. Use of an App-Controlled Neuromuscular Electrical Stimulation System for Improved Self-Management of Knee Conditions and Reduced Costs. Surg Technol Int. 2017 Oct 12;31:221-226. [PubMed]
- Geller JA, Lakra A, Murtaugh T. The Use of Electronic Sensor Device to Augment Ligament Balancing Leads to a Lower Rate of Arthrofibrosis After Total Knee Arthroplasty. J Arthroplasty. 2017 May;32(5):1502-1504. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).