1. Introduction
The residual bone cavities after enucleation of large radicular cysts are associated with an increased risk of infection and a decrease in bone strength in the area of the pathological focus, which makes the problem relevant [
1]. They can be treated by filling with various bone-plastic materials, as well as using biological substances that stimulate reparative osteogenesis [
2]. In recent years, platelet concentrates capable of inducing the proliferation and differentiation of mesenchymal stem cells have been widely used in regenerative medicine. For example, platelet-rich fibrin (PRF) can produce growth factors for at least seven days at the site of exposure, which stimulate osteoblast activity and accelerate bone regeneration by increasing fibroblast migration [
3]. We have described a case of successful use of PRF for the healing of residual bone cavities after enucleation of large maxillary radicular cyst.
2. Case Presentation
2.1. Chief Complaints
A 58-year-old female patient presented to the dental department with a complaints of aching pain and gradually increasing swelling in the maxillary area for 3-4 days.
2.2. History of Present Illness
The patient has not been examined by a dentist for 5-7 years. She felt discomfort in the maxillary area only during physical exertion in a forward-leaning position.
2.3. History of Past Illness
The patient denied that she had any significant diseases, major injuries and surgeries, blood transfusions, or allergies to food or medications.
2.4. Personal and Family History
The patient denied any family history.
2.5. Physical Examination Upon Admission
Clinical examination revealed a swelling in the maxillary anterior region. Oral examination revealed local hyperemia and swelling of the oral mucosa at the level of the alveolar part of teeth 13-21, smoothness of the transitional fold due to the rounded bulge. There was pain and fluctuation in this area during palpation. The teeth 13, 12, 11 and 21 with preserved crown parts without carious lesions were slightly painful upon percussion.
2.6. Laboratory Examinations
The laboratory tests showed no significant abnormalities.
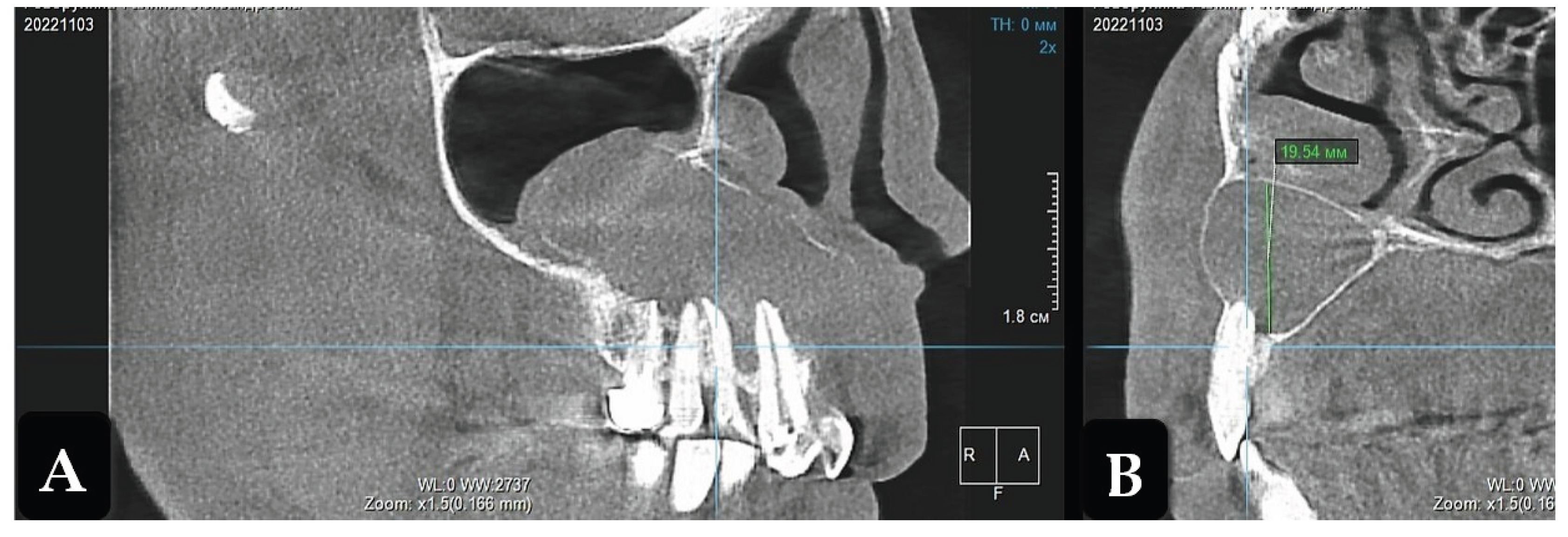
2.7. Imaging Examinations
Cone-beam computed tomography (CBCT) revealed osteolytic lesion with clear contours and a well-defined sclerotic margins of varying thickness. It extended 17 mm in the vestibulo-oral direction to the border of the maxillary sinus, significantly pushing it aside, and 22 mm along the alveolar bone in the mesiodistal direction from tooth 1.3 to 2.1. The endodontically untreated apical parts of the teeth roots 1.3, 1.2, 1.1 and 2.1 protruded into the periradicular lesion. Due to the preservation of sufficient bone thickness on the vestibular side, root divergence was not observed (
Figure 1).
2.8. Final Diagnosis
Based on the clinical signs and CBCT imaging, the final diagnosis was maxillary radicular cyst.
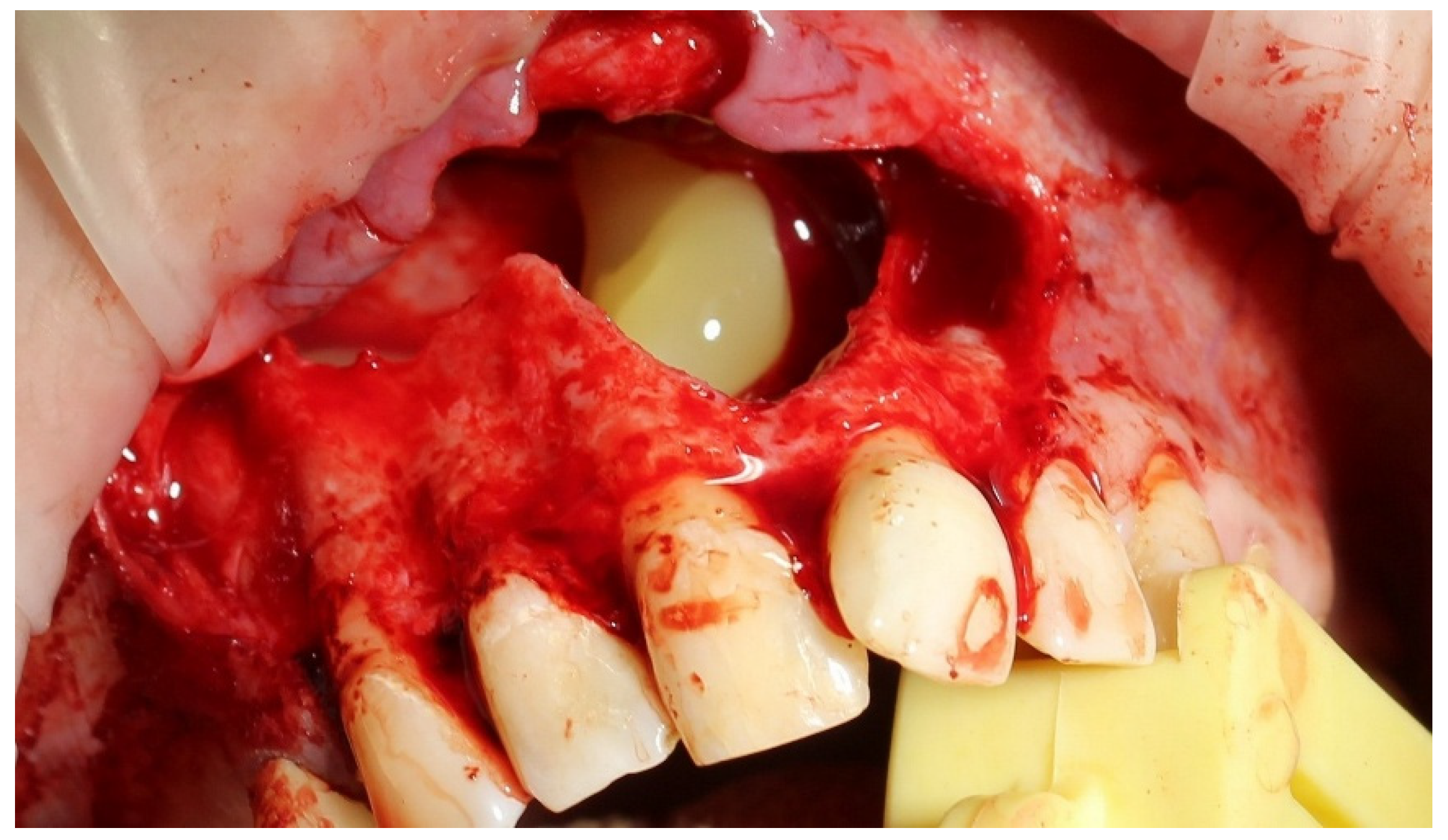
2.9. Treatment
For one month, the patient received complex conservative therapy to relieve acute inflammation. Before surgery, the cyst-related teeth 1.3, 1.2, 1.1 and 2.1 were endodontically treated. Cyst enucleation was performed with preliminary sedation under local anesthesia. Following the enucleation, histopathological analysis confirmed the presence of a radicular cyst. The apices of the teeth roots 1.3, 1.2, 1.1 and 2.1 protruding into the periradicular lesion were resected, the residual bone cavity was filled with PRF clot (
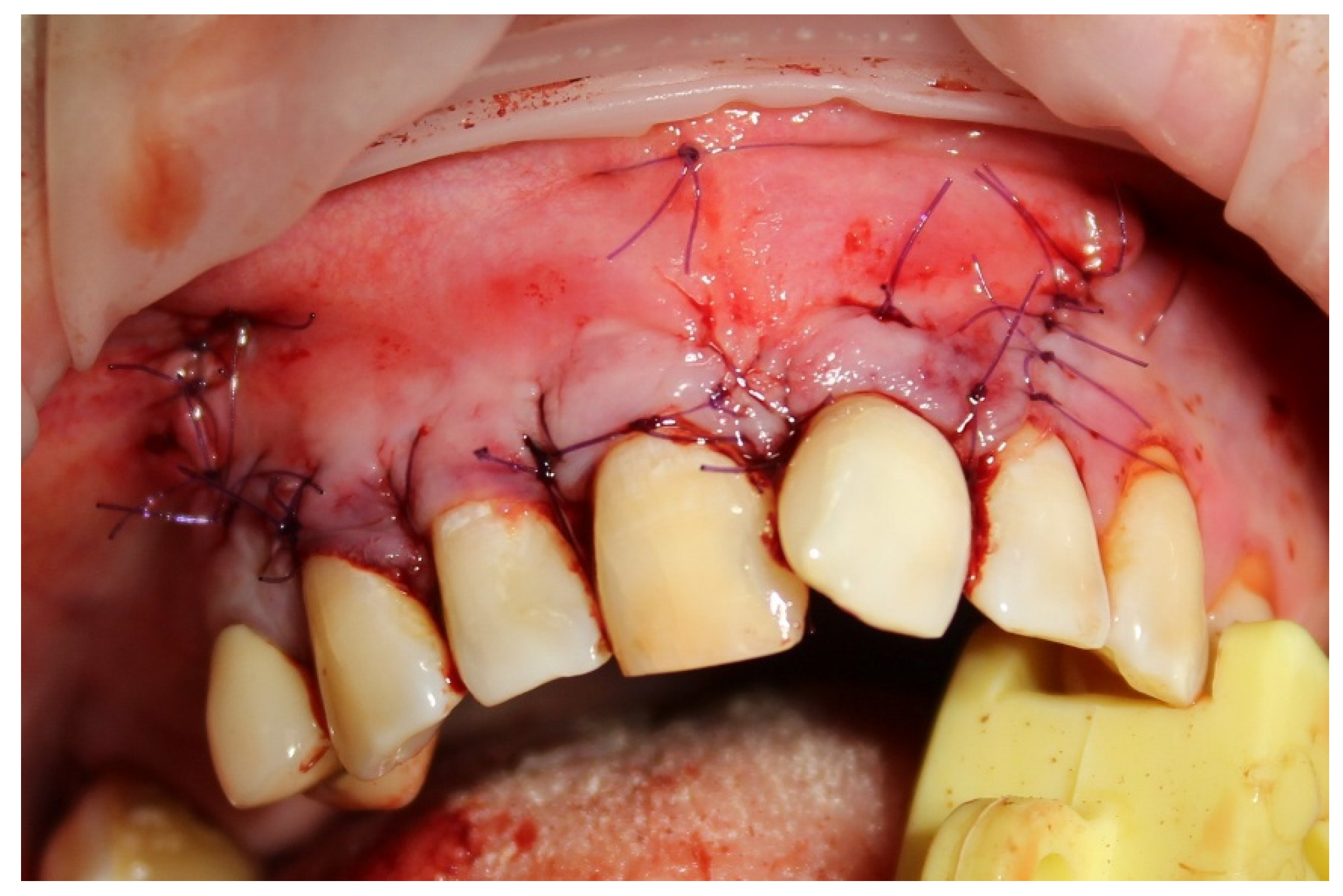
Figure 2), and the bone wound was completely covered with a mucoperiosteal flap (
Figure 3).
To prepare a PRF clot, 5 ml of whole venous blood was taken into each of two sterile vacutainer tubes without anticoagulant. The tubes were centrifuged at 3000 rpm for 10 minutes, resulting in three layers: the lower red fraction (red blood cells), the upper straw-colored layer (cellular plasma), and the middle fraction, which was collected 2 mm below the lower dividing line, representing the PRF clot [
4].
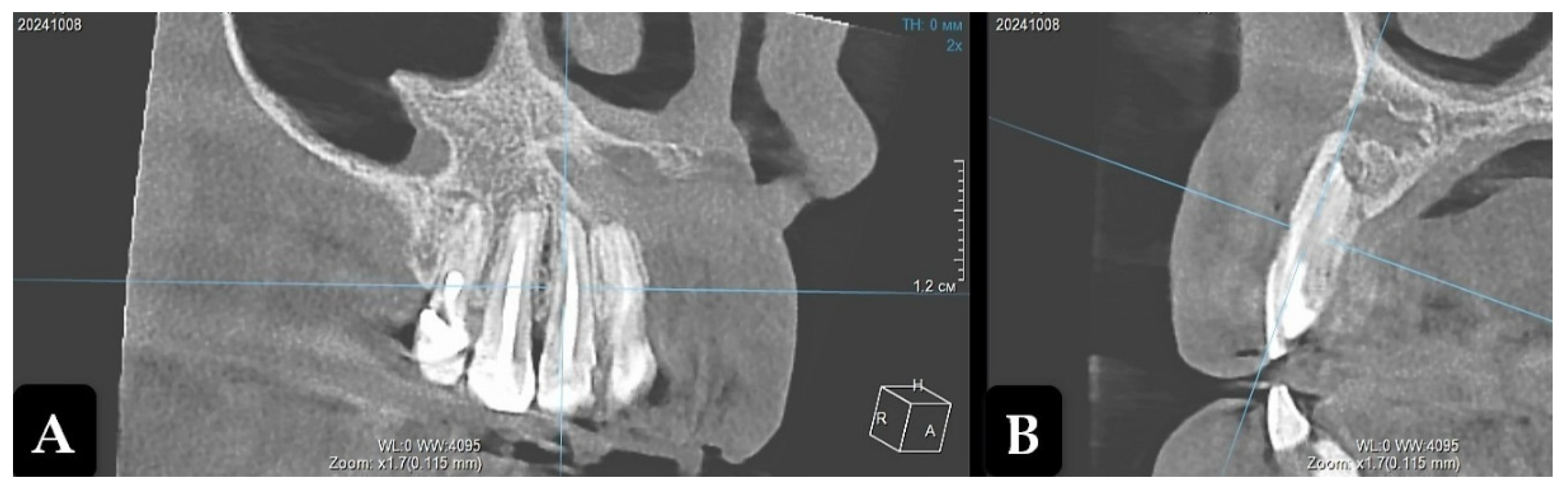
2.10. Outcome and Follow-Up
Long-term results were evaluated for up to 2 years. The patient did not experience any problems from the oral and maxillofacial organs. One year after the operation, CBCT visualized the vague contours of the residual cavity filled with bone trabeculae, which had significantly decreased compared to the preoperative findings. Parietal bone regeneration was detected, while no signs of organotypicity were recorded in the center (
Figure 4).
Two years after the operation, CBCT showed complete filling of the residual cavity with bone tissue to the level of the teeth roots, with beginnings of vestibular cortical formation. Separate sections of the cortical bone layer on the vestibular side at the level of teeth 1.2 and 1.1 were in the process of repair (
Figure 5).
The functioning preserved teeth 1.3, 1.2, 1.1 and 2.1 were in stable condition (
Figure 6).
4. Discussion
The problem of choosing the optimal method for the healing of residual bone cavities after enucleation of large radicular cysts does not lose its relevance. One of them may be using biological substances that produce growth factors that stimulate reparative osteogenesis. This approach has been approved by the U.S. Food and Drug Administration (FDA) and recommended for use in dental practice [
5]. PRF is a biological substance rich in platelets and growth factors which promote bone regeneration such as bone morphogenetic protein, insulin-like growth factor, platelet-derived growth factor, vascular endothelial growth factor, epithelial growth factor, fibroblast growth factor, and transforming growth factor-β1. Their gradual release correlates with PRF clot resorption [
6]. PRF enhance osteoblasts proliferation and the expression of collagen type I alpha-1, runt-related transcription factor 2, alkaline phosphatase, osteocalcin, and glyceraldehyde-3-phosphate dehydrogenase genes which play an important role in bone formation. PRF is easily manufactured and has bioactive elements not requiring anticoagulants in its preparation. It is resistant to stretching and elastic, and it can either be applied with or without combining it with various bone-plastic materials [
7]. At the same time, despite the obvious prospects use of PRF to stimulate reparative osteogenesis after enucleation of odontogenic cysts, the efficacy of the method has been shown mainly in descriptions of clinical cases.
5. Conclusions
In the case described by us, the use of PRF contributed not only to the healing of residual bone cavity after enucleation of large maxillary radicular cyst, which was confirmed by the results of CBCT, but also to the preservation of dental functionality in an aesthetically significant area.
Abbreviations
The following abbreviations are used in this manuscript:
| PRF |
Platelet-rich fibrin |
| CBCT |
Cone-beam computed tomography |
| FDA |
Food and Drug Administration |
References
- Ettl, T.; Gosau, M.; Sader, R.; Reichert, T.E. Jaw cysts - filling or no filling after enucleation? A review. J. Craniomaxillofac. Surg. 2012, 40, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Damsaz, M.; Castagnoli, C.Z.; Eshghpour, M.; Alamdari, D.H.; Alamdari, A.H.; Noujeim, Z.E.F.; Haidar, Z.S. Evidence-Based Clinical Efficacy of Leukocyte and Platelet-Rich Fibrin in Maxillary Sinus Floor Lift, Graft and Surgical Augmentation Procedures. Front. Surg. 2020, 7, 537138. [Google Scholar] [CrossRef] [PubMed]
- Zoltowska, A.; Machut, K.; Pawlowska, E.; Derwich, M. Plasma Rich in Growth Factors in the Treatment of Endodontic Periapical Lesions in Adult Patients: A Narrative Review. Pharmaceuticals (Basel) 2021, 14, 1041. [Google Scholar] [CrossRef] [PubMed]
- Rao, U.; Asim, M.A. Use of Autologous Platelet-Rich Fibrin (PRF) in the Surgical Management of Maxillary and Mandibular Radicular Cysts. JCPSP Case Rep. 2024, 2, 14–16. [Google Scholar] [CrossRef]
- Shimono, K.; Oshima, M.; Arakawa, H.; Kimura, A.; Nawachi, K.; Kuboki, T. The effect of growth factors for bone augmentation to enable dental implant placement: A systematic review. Jpn. Dent. Sci. Rev. 2010, 46, 43–53. [Google Scholar] [CrossRef]
- Egierska, D.; Perszke, M.; Mazur, M.; Duś-Ilnicka, I. Platelet-rich plasma and platelet-rich fibrin in oral surgery: A narrative review. Dent. Med. Probl. 2023, 60, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Alrayyes, Y.; Al-Jasser, R. Regenerative Potential of Platelet Rich Fibrin (PRF) in Socket Preservation in Comparison with Conventional Treatment Modalities: A Systematic Review and Meta-Analysis. Tissue Eng. Regen. Med. 2022, 19, 463–475. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).