1. Introduction
The restrictions placed on in-person contacts, even for health-related reasons, during the COVID-19 pandemic amplified the need for remote assessments and telerehabilitation [
1,
2]. In physical rehabilitation, there is a strong focus on gait and mobility, traditionally assessed only in person [
3,
4]. Gait is the manner of walking [
5]. Walking can be further classified according to capacity and performance using the ICF [
6]. Capacity is what the person can do as reflected by testing parameters such as gait speed and distance walked in a fixed time in a clinical setting [
7]. In measurement terminology, these tests fall under the rubric of Clinical Outcome Assessment (COA). COA can rely on different sources of information: Clinician Reported Outcomes (ClinRO) and Performance Outcomes (PerFOs) [
15,
16,
17]. ClinROs typically include a structured checklist (Powers et al., 2017). PerfOs on the other hand rate a person’s performance on a standardized test such as the 10-meter walking test (10MWT), Timed-Up and Go (TUG), or the 6-min walking test (6MWT). The results are interpreted as an individual’s capacity to walk or move [
9]. On the other hand, performance indicates what is done in the real-world setting and is often quantified as steps per day and walking bouts [
8,
9]. Capacity and performance quantify walking [
10]. Good gait quality is the foundation for both walking capacity and performance, making gait assessment and gait training the primary activities of rehabilitation [
11,
12,
13].
A wide array of methods is available for assessing gait, and one method will not fit all purposes. Gait assessment is crucial for treatment planning and evaluation and uncovering mechanisms of optimal and pathological gait [
14]. At one end of the spectrum are simple, inexpensive, and commonly used methods involving direct observation by an expert. At the other end are complex, costly, technologically aided methods, some of which require extensive infrastructure and specialized personnel. In a clinical setting, the direct observation method by a clinician is most widely used.
Observational methods are best suited for judging spatial gait parameters including posture and the observer has the benefit of a three-dimensional view of the client. These parameters are rated on an ordinal scale representing the degree to which the element is optimal. Observational methods have only moderate inter-rater agreement [
18] but are still widely used in a clinical setting [
19].
Advances in digital recording have made monitoring gait in daily life (outside a clinic or lab) practical. The person need not walk multiple times, and the image itself can provide valuable feedback to the client. Observational methods can now be applied to gait recorded remotely.
Another rapidly advancing and evolving method for gait assessment is using technology (TechO) [
15] to measure spatial, temporal, kinematic, and kinetic parameters and these assessments can be done using non-wearable or wearable technologies [
20]. Non-wearable technologies are considered the research gold standard [
21]. Their drawbacks are that they are fixed, expensive, and need extensive infrastructure, including space, and trained personnel to operate and manage data from these systems. They clearly cannot be used for remote monitoring. A newer method under the category of non-wearables for measuring many gait parameters of interest (spatial, temporal, kinematic) is based on pose estimation. This markerless motion capture technology arose from the animation industry [
22] and is suitable for remote monitoring as it takes advantage of video recordings.
Wearable technologies burst into the health and fitness industries [
23] owing to their availability and the miniaturization of the internal measurement units (IMUs) that detect raw inertial body movements. Wearable sensors today are lightweight, available for personal use, affordable, and can be used to collect data without disturbing daily life activities. New generation wearables connect to smartphone devices, and IMUs are also part of every smartphone now that track steps, stairs climbed, movement time, and even some aspects of gait such as stride length, unsteadiness, and asymmetry, making smartphone-based human motion assessment feasible [
24]. Wearable technologies can be used clinically, for research, and for remote monitoring [
25].
Of the remote methods of gait analysis, observation by an expert and pose estimation are only possible at set intervals, and as such, they capture only a small portion of the person’s everyday gait pattern and walking performance. Wearable technologies, on the other hand, can measure gait continuously and during planned and real-world activities.
No studies have carried out a head-to-head comparison of all possible remote gait assessment methods (observation, wearable and pose estimation), although pairwise comparisons of methods to the gold standard have been conducted. A 2021 systematic review by Follis et al. [
26], reviewed 14 studies conducted on participants with lower extremity arthroplasty, comparing COA metrics using wearable sensors to traditional methods of collecting COA data typically using tests like the 6MWT or the TUG. The authors emphasized the potential of wearable sensors to provide additional insights into recovery after arthroplasty and further research on clinical changes detected by wearables. The most common head-to-head comparison was between wearable sensors and non-wearable instrumented walkways [
27,
28]. A systematic review by Prisco et al. [
27], of 32 agreement studies, conducted on diverse populations estimated good to moderate agreement on kinematic gait parameters but greater variability for spatial and temporal parameters. Recent studies have also compared metrics from pose estimation libraries to marker-based instrumented walkways. A study conducted by Menychtas et al., in 2023 [
29], comparing 2-D pose estimation libraries from OpenPose and MediaPipe Pose to marker-based 3D motion capture system, Vicon, concluded that pose estimation libraries achieve motion tracking comparable to the fixed motion capture systems on metrics of joint angle, position of limb and velocity of movement although with inconsistencies in detecting smaller joint movements. Hii et al [
30], compared different pose estimation libraries in the study on marker-free gait analysis using the Pose Estimation Model in 2022 and inferred MediaPipe Pose is the best for assessing kinematics of lower limb joints in real-world applications. However, data comparing all three different methods of gait analysis (clinical observational, wearable sensor and pose estimation) was lacking.
PD has been the most widely studied for these comparisons [
27]. People with PD have a typical gait pattern that is well-described and known to clinicians making the gait pattern readily measurable. The gait pattern in PD is characterized by stooped posture, short shuffling steps, center of mass too far forward to be safe, and limited arm swing. This pattern is disabling and dangerous and negatively impacts other aspects of function and quality of life, making gait impairment the leading reason individuals with PD seek evaluation and physical rehabilitation [
31].
There is a gap in knowledge about head-to-head comparisons of methods suitable for remote gait analysis and their challenges. Specifically, the purpose was to estimate, for people with PD, the extent to which values on gait metrics compare among (i) observational analysis by physiotherapists, (ii) wearable sensors, and (iii) pose estimation. Information from this three-way head-to-head comparison would guide clinicians and researchers to choose the best technology for their purposes.
2. Materials and Methods
This study is embedded in a larger ongoing implementation trial of the wearable sensor – Heel2toeTM – as gait therapy for people with PD (ClinicalTrials.gov ID: NCT05801926). The study reported here used data from the initial assessment. Data from the following materials were used for analysis: (i) a checklist for observers to rate elements of gait that are specific to PD; (ii) remotely recorded videos of adequate quality for observing gait; (iii) a wearable sensor that detects the angular velocity of the ankle during the gait cycle - Heel2ToeTM wearable; (iv) a pose estimation library – MediaPipe Pose.
2.1. Sample
All participants gave their written informed consent in agreement with the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of the Faculty of Medicine and Health Sciences, McGill University, on 31st August 2022 (A05-B37-22A).
The trial participants included people with self-reported mild to moderate gait deficits equivalent to Hoen and Yahr grade ≤ 3 and able to perform a modified TUG test (walking a minimum of 15 steps instead of the standard 3 meters) without losing balance or freezing without recovery as observed on a personally recorded video. Participants received a comprehensive list of instructions for recording the video, with an example video recorded by the research team as a reference. Participants were asked to record both lateral and frontal views performing the modified TUG test wearing the Heel2ToeTM wearable sensor between 30 minutes to 2 hours after taking their medication (Levodopa/Carbidopa).
2.2. Measures
2.2.1. Observational Checklist
An observational checklist (see Appendix 1) was adapted for use in this study based on existing checklists described in the literature [
32,
33,
34,
35,
36,
37]. The checklist comprised 34 different gait parameters (items) rated by six raters for the degree to which each was optimal. Each item in the checklist was rated on a binary or three-point ordinal scale that, when summed, yielded a total score of 35 points, where a higher score indicated better gait quality. The checklist was iteratively tested and revised based on the experience of nine different gait experts. Videos of adequate quality were analyzed by six randomly assigned raters from a diverse group of ten experienced physiotherapists. Raters showed an average agreement of 86.4% across all items. There was 100% agreement on 3 out of 34 items. For each item with less than perfect agreement, a consensus rating was chosen after review by two expert raters. The intraclass correlation (ICC) across raters was 0.78.
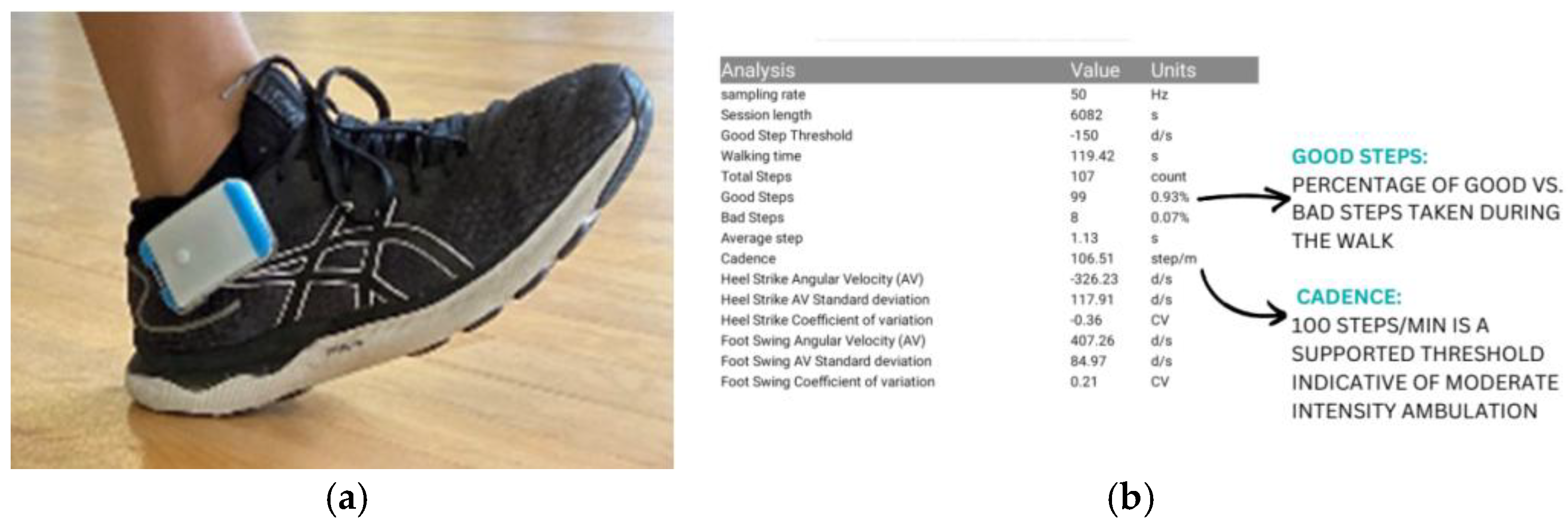
- (b)
Heel2ToeTM – wearable sensor
The Heel2Toe
TM wearable is a commercial product of PhysioBiometrics Inc. It is a small, wireless, inexpensive and lightweight wearable sensor that clips to the side of the shoe, as shown in
Figure 1a. The gyroscope in the sensor measures in real time the angular velocity of the ankle in the sagittal plane during each gait cycle. The angular velocities are negative with clockwise rotation and positive with counterclockwise rotation. An algorithm generates metrics related to heel strike and toe push-off which are clockwise rotations, and foot swing, which is counterclockwise rotation. The salient parameters are shown in
Figure 1b and fully described in
Appendix B. The version of the Heel2Toe
TM sensor used in this study transmitted raw data from the sensor to an application on an Android phone via Bluetooth and saved it on a cloud server.
Heel2Toe
TM can be used for both assessment and training purposes as it provides feedback for an optimal step. The development of the hardware and algorithm of the Heel2Toe
TM have been reported [
38,
39]. The algorithm has a step classification accuracy of 92.7% with sensitivity and specificity of 84.4% and 97.5%, respectively. The Heel2Toe
TM has been successfully tested among individuals with PD, demonstrating feasibility for home use and strong efficacy potential [
40,
41].
Figure 1.
(a) Heel2ToeTM sensor on the right foot; (b) Parameters displayed on the application.
Figure 1.
(a) Heel2ToeTM sensor on the right foot; (b) Parameters displayed on the application.
- (c)
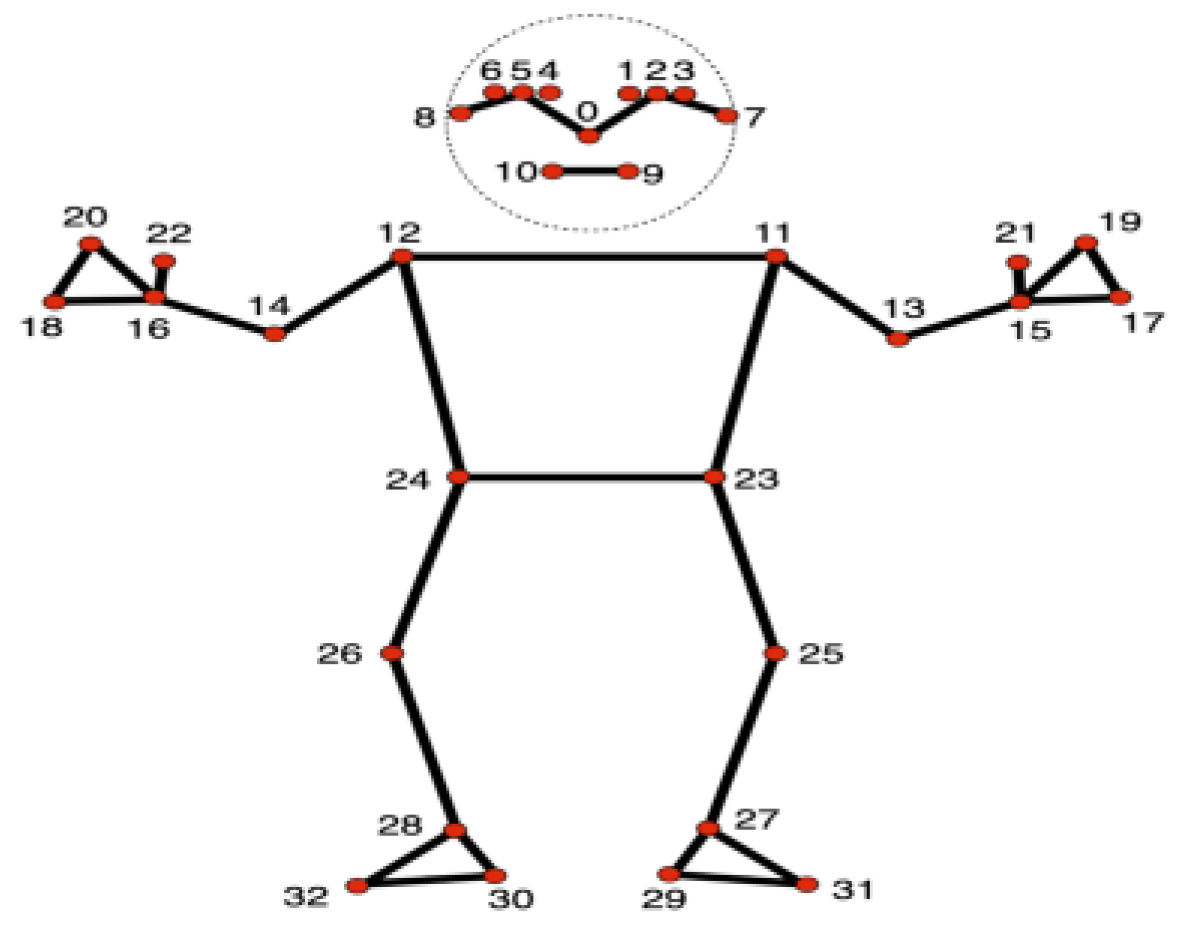
Analysis of video-recorded gait using MediaPipe Pose
The MediaPipe Pose Landmarker task, developed by Google, was used to analyze 20 gait videos using the Python PyPI package. The Pose Landmarker model uses a convolutional neural network to map human pose by estimating 33 3-dimensional (x, y, z) landmarks, also called anatomical landmarks, in real-time, as shown in
Figure 2. Compared to other open-source libraries, MediaPipe shows high accuracy in mapping anatomical landmarks of the lower limb [
30]. Furthermore, MediaPipe Pose has been tested for reliability in gait analysis and the detection of motor impairments in PD [
42,
43]. Studies done so far using the MediaPipe Pose library for gait analysis have reported detecting heel strike, push-off, step length, stance time, swing time and double support time [
30,
44]. As pose estimation is less explored, automated models for detecting only a few gait parameters have been developed, and clinically relevant normative values are not available.
To meet the need for detecting a broader range of temporal, spatial, and kinematic gait parameters for a comprehensive analysis best suited for clinical interpretation, a program inspired by the studies on pose estimation [
43,
45,
46] was customized specifically to the observational checklist developed in this study. We aimed to identify as many gait parameters as possible. In the process, each gait parameter was first defined, and the relevant anatomical landmarks were listed. After running multiple experiments attempting to estimate angles and distances on the videos shared by the participants, we were limited to estimating 5 out of the 31 parameters from the checklist. All videos were analyzed in the MP4 format at 60 frames per second. This tailored program was first tested on a video with no gait impairments shown in
Figure 3. This limitation was due to challenges of lack of an estimate of the ground, inconsistencies in the distance covered during the modified TUG test, fluctuating angles of the camera, inconsistent resolution, and unsteady recording, leading to variability in the video frames captured. The parameters thus possible to estimate were: (i) heel strike and push-off in degrees/second (°/sec) – values corresponded to the most optimally viewed frame of heel strike and push-off on the video, (ii) swing at the hip in degrees (°) – values corresponded to the mean±SD representing change in angles at the hip during one gait cycle identified by frames on the video, and (iii) forward and backward arm swing in degrees (°) - values corresponded to the most optimally viewed frame of forward and backward arm swing on the video. The libraries and modules used in the program are fully described in
Appendix B.
Table 1 presents gait parameters acquired from the three methods and illustrates the commonality of parameters across methods.
2.3. Analysis
Two types of analyses were carried out. The first was on the agreement between the observational checklist and values from the Heel2Toe
TM wearable. To match the qualitative categories from the observational checklist, values obtained from Heel2Toe
TM for heel strike and push-off were categorized as excellent, very good, good, fair, or poor; values for foot clearance and cadence were dichotomized. Categories were based on typical values generated from a sample of 88 students in health professional programs at McGill (see
Table 2). The crude agreement was calculated for each of the four parameters. For the four metrics and sample size of n, the number of person measures a total of 4*n. The agreement rate per person-measure and associated 95% confidence interval (CI) were calculated.
The second analysis related estimates of angle parameters (angular velocity or joint angle) from MediaPipe Pose to the categorical ratings from the Observational checklist and to the angular velocity from the Heel2ToeTM wearable. As the parameters compared across all three methods were on different measurement scales, the participants were ranked for each parameter, from highest to lowest, on the respective measurement scales. The differences in these rankings were compared using the Wilcoxon signed rank sum test. A significant p-value indicates a substantial difference between the median values of each pair of methods being compared. Finally, measured angular velocities from MediaPipe Pose and Heel2ToeTM wearable for heel strike and push-off were grouped based on ratings from the Observational Checklist and compared using t-tests.
Table 2.
Categories for gait parameters estimates that were recorded using the Heel2ToeTM wearable based on 88 healthy students.
Table 2.
Categories for gait parameters estimates that were recorded using the Heel2ToeTM wearable based on 88 healthy students.
Parameters/
Category ratings |
Excellent |
Very Good |
Good |
Fair |
Poor |
| |Maximum| |
25th or 75th percentile |
Median |
25th or 75th percentile |
|Minimum| |
|
Heel strike (ο/sec) |
-400 to < -320 |
-320 to < -280 |
-280 to < -200 |
-200 to < -120 |
< -120 |
| |
|
|
|
|
|
| CV% |
10 to < 20 |
20 to < 25 |
25 to < 30 |
30 to < 50 |
≥ 50 |
| |
|
|
|
|
|
|
Push-off (ο/sec) |
-600 to -481 |
-480 to -421 |
-420 to -301 |
-300 to -121 |
-120 to 0 |
| |
|
|
|
|
|
| CV% |
5 to < 15 |
15 to < 25 |
25 to < 30 |
30 to < 50 |
≥ 50 |
| |
|
|
|
|
|
|
Foot clearance (ο/sec) |
600 |
400 |
360 |
340 |
200 |
| |
|
|
|
|
|
| CV% |
5 to < 10 |
10 to < 15 |
15 to < 20 |
20 to < 30 |
≥ 30 |
2.4. Sample Size
The sample size was estimated during the planning stages based on having a feasibility sample ranging from 14 to 20 participants and calculating a person-measure agreement rate based on a minimum number of participants of 14 and 4 overlapping measures among the different methods yielding 56 person-measures. With a hypothesized agreement rate of 0.5, the associated 95% CI ranged from 0.33 to 0.72.
3. Results
Twenty-seven people submitted videos, and none were excluded based on safety considerations. Seven people submitted videos of insufficient quality for any of the gait quality assessments. The 20 participants had videos suitable for observational gait analysis and MediaPipe Pose. Of the 20 participants, 14 met the technology readiness criteria for home use of the Heel2ToeTM wearable.
The characteristics of the participants in terms of demographics and quality of video submitted at the initial assessment when recruited for the implementation trial are shown in
Table 3.
Table 4 presents agreement on the qualitative categories between the observational checklist and the Heel2Toe
TM wearable: heel strike, push-off, foot clearance and cadence. (The optimal values of these kinematic parameters were given in
Table 2). The first cell indicates that there was agreement at the optimal/excellent level on heel strike for 3 of the 14 comparisons, and the overall crude agreement was 9/14, 64% CI (0.39,0.89). For push-off, the crude agreement was 28% CI (0.04,0.52); for foot clearance, the crude agreement was 35.7% CI (0.12,0.61); for cadence, the crude agreement was 85% CI (1.01,2.71). Finally, overall agreement across all four parameters was 53.5% CI (0.41,0.66).
Table 5 presents values on matching parameters estimated from MediaPipe Pose and rated using the Observational Checklist and also from those recorded using the Heel2Toe
TM sensor. Given that common parameters from all three methods were measured on different metric system units, the Wilcoxon Signed Rank Test was conducted to see if paired common parameters were ranked the same. The difference in the ranks of paired observations between the pairs of methods compared was significant for all parameters except for push-off when estimates from MediaPipe were compared to the ratings from the Observational Checklist, W = 86 (p = 0.498).
Table 6 presents the differences between optimal and weak parameters as rated by expert viewers using the Observational Checklist when the parameters are assessed using each of the TechOs. For heel strike, there were 6 people rated optimal by viewers and 14 rated weak. For participants rated with optimal heel strike, the mean AV as estimated using MediaPipe was -222.8
o/sec.; for participants rated as weak, the value was -156.5
o/sec., not statistically different from those rated as optimal (p=0.133). The corresponding values when measured using Heel2Toe for these two groups of people were -290.6
o/sec and -241.8
o/sec, not statistically different (p=0.26). For people rated with optimal heel strike observationally, the values for heel strike as estimated using MediaPipe and as measured by the Heel2Toe sensor were similar as shown by the value on the paired t-test (1.5; p-0.219). For those rated weak observationally, the estimated value from MediaPose was not as strong than the value obtained from the Heel2Toe sensor (-241.8 (t=2.6; p=0.034). For push-off the results were similar with no difference in values between participants rated as optimal or weak; the values for push-off considerably different when measured using the Heel2Toe sensor.
4. Discussion
This study was motivated by the need for remote assessment, and hence, the methods compared are not commonly integrated into the clinical setting. Remote assessments can be conducted by analyzing videos recorded using a single camera through expert observation, pose estimation, or real-time analysis using wearable sensors [
48].
A scoping review of the status of clinical gait assessment published in 2022 by Hulleck et al. [
49], highlighted a gap between the technology available and current clinical practices, given most clinicians rely on methods of observation or performance for gait assessment due to the lack of clinical interpretability of data obtained from TechOs. To bridge this gap and provide comparable data, an observational checklist specific to gait assessment in PD was developed for this study and tested as one of the methods for evaluating gait from videos. This approach also allowed for the application of pose estimation to the same videos. Additionally, a wearable sensor was used for real-time analysis. To our knowledge, this is the first time that these three methods have been compared using data and videos from individuals with PD in their home environment, demonstrating how telerehabilitation might work for remote assessment.
A systematic review by Ridao-Fernández et al. in 2019 [
35], reported the reliability of 18 observational measures assessing spatial and temporal gait parameters as poor to fair. Furthermore, a study by Krebs et al., 1985 reported an ICC of 0.73 for the Observational Kinematic Analysis measure. This is similar to the ICC calculated for the Observational Checklist in our study, capturing both spatial-temporal and kinematic parameters, which was calculated as 0.78, suggesting it to be sufficient for treatment planning but not adequate for estimating individual change [
50]. This could be due to possible challenges related to a lack of sufficient optimization of the measure, insufficient training of the raters, ambiguity in phrasing questions positively/ negatively, the time-consuming nature of the checklist, inconsistencies in rating one side instead of both and poorly recorded videos.
Our results showed that observational gait quality ratings differed from those obtained using MediaPipe except for push-off and were also different from those obtained using Heel2Toe wearable sensor (see
Table 5). We also showed that observational ratings of quality (optimal and weak) did not correspond to values obtained from the TechOs (see
Table 6). There were also differences across TechOs as values from MediaPipe are really estimates of angular velocities while values from Heel2Toe are measured directly from IMUs embedded in the device.
A systematic review by Follis et al. in 2020 [
26], compared traditional observational methods, including Performance Outcomes (PerfOs) and Clinician-Reported Outcomes (ClinROs), to wearable sensors for assessing functional change after lower limb arthroplasty. The review reported varying levels of agreement between wearables and observational methods, ranging from poor to moderate correlations. It highlighted the holistic nature of observational methods for assessing gait, in contrast to the limited parameters obtained from a single sensor, despite the sensor’s ability to identify subtle biomechanical nuances overlooked by traditional methods. This challenge can be addressed by using multiple sensors to evaluate different aspects of gait. In our study, the highest degree of agreement between the Observational Checklist and the data from the Heel2Toe™ wearable was on cadence (92%), which can be used to detect variability in walking speed. Moderately high agreement was found for heel strike (62%), while poor agreement was observed for other gait parameters: push-off (28.6%) and foot clearance (35.7%) (see
Table 4). One major challenge while recording data using the Heel2Toe™ was the loss of connectivity signal due to an unstable Bluetooth connection and the wearable’s selective connection with Android operating systems. These issues have been addressed in newer versions of the Heel2Toe™.
A study by Harini Ramesh et al. in 2023 [
45], comparing an observational method of gait assessment to pose estimation reported a strong correlation of 0.8 between the Edinburgh Visual Gait Score, which captures spatial and-temporal parameters, and OpenPose, a pose estimation library. This contrasts with our findings, where the only parameter showing agreement between the Observational Checklist and MediaPipe was push-off; there was no agreement on other overlapping measurements such as heel strike, hip swing, and arm swing (see
Table 5). One of the greatest challenges is the absence of scores verified by ground truth. Additional challenges included a lack of robustness to variations in lighting, camera angles, resolution, and other objects in the video frame. The cumbersome nature of frame-by-frame analysis and the need for different views (frontal for temporal parameters and lateral for spatial parameters) complicate the recording of gait videos. Recording both views may not always be feasible in all scenarios [
51]. Furthermore, the lack of open-source automated libraries for pose estimation makes it challenging to integrate these technologies into clinical settings, posing computational difficulties for clinicians. Nonetheless, these technologies can detect subtle nuances missed by the human eye, offering promising possibilities for early detection of impairment during an assessment from the comfort of one’s home [
48].
While comparing pose estimation to wearable sensors, a study by Masataka Yamamoto et al. in 2022 [
52] reported a strong correlation of 0.89 in detecting mean joint angles between the two methods in the lateral view. Our study found no agreement when the difference in ranks from angular velocity values obtained from MediaPipe and Heel2Toe
TM were compared, as shown in
Table 5, possibly due to the challenge of varying camera angles, and clutter in the environment, which seldom affected tracking of key landmarks. These are challenges that would commonly exist in a scenario of a remote clinical setting. Nonetheless, both TechOs were able to differentiate between ratings from the Observational Checklist. When grouped based on those ratings, matching pairs showed an agreement (see
Table 6).
The limitation was a small number of subjects, only 20 and not everyone could be assessed on all three methods. However, given the low amount of agreement, a better use of resources would be to optimize the methods for remote assessment before assessing more people. As pose estimation becomes more robust for human motion, it could emerge as a very useful tool when used in combination with wearable sensors for remote assessment.
5. Conclusions
This results of this study would support that the wearable sensor has the most promise for regular clinical use as it is possible for patients to use themselves, and the data is readily interpretable by both the patient and clinician. The newest version of the Heel2Toe™ records data directly onto an SD card and can be transmitted for visualization and storage on to a computer, tablet, or smartphone via a standard USB cable. It does, however, provide a limited set of gait parameters. The observational checklist is too time-consuming and unreliable for individual assessment of change. Media Pipe pose requires too much expertise for the average clinician to use regularly but certainly provides rich data when used optimally. Advances in automating the program for estimating a variety of gait parameters and in image processing could change its real-world applications.
Author Contributions
“Conceptualization, N.M. and N.H.; methodology, N.M.; software, E.H.; validation, N.M., E.H. and N.H.; formal analysis, E.H. and N.H.; investigation, N.H.; resources, N.M.; data curation, E.H., N.H.; writing—original draft preparation, N.H.; writing—review and editing, N.M., H.D.; visualization, E.H.; supervision, N.M., H.D.; project administration, N.H.; funding acquisition, N.M. All authors have read and agreed to the published version of the manuscript.”
Funding
MedTeq, Mitacs, and Healthy Brains, Healthy Lives (HBHL) have funded the larger study on the use of the Heel2Toe™ sensor for individuals living with PD, in collaboration with PhysioBiometrics Inc. and McGill University: The APC was waived 100% by the Sensors Editorial Office.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board, Faculty of Medicine and Health Sciences, McGill University, on 31st August 2022, IRB Internal Study Number/ Info-Ed File Number: A05-B37-22A / 22-04-037.
Informed Consent Statement
Written informed electronic consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Acknowledgments
We sincerely thank all participants and their caregivers who contributed to this study. We gratefully acknowledge Dr. Nancy E. Mayo for her invaluable guidance and support throughout this work. Further, we thank PhysioBiometrics Inc. for the wearable sensors and the Centre for Outcomes Research and Evaluation, RI-MUHC, McGill University, for providing the resources and a collaborative environment to complete this study.
Conflicts of Interest
The authors acknowledge a potential conflict of interest in this study. The following authors report potential conflicts of interest: Prof Nancy Mayo, Founder and President, Dr Ted Hill, Co-Founder and VP Product Design, and Prof Helen Dawes, Director of International Affairs are affiliated with Physibiometrics Inc. The study involves the use of the Heel2ToeTM wearable, a device developed and commercialized by Physibiometrics Inc. These authors contributed to the design, development and commercialization of the wearable used in this study and are co-authors of this manuscript. Their involvement has been fully disclosed, and appropriate steps were taken to ensure that the research was conducted and reported with scientific rigor and objectivity. All remaining authors declare no competing interests
Appendix A
Appendix A.1. Final Checklist used for rating 20 videos by the raters
| Gait Parameters |
Description |
Classifier |
| Getting up from the chair |
|
| Freezing while getting up |
We are looking to see if the participant experiences the sudden inability to move despite the intention to while getting up from the chair |
0 Present
1 Absent |
|
| Needs arms |
Does the participant use support of the armrest/ side of the chair or do they place their arm on their thighs or knees as support to get up from the chair |
0 Yes
1 No |
|
| More than 1 tries to get up from a chair |
Does the participant try getting up more than once from the chair due to unsuccessful attempt/ attempts |
0 Yes
1 No |
|
| Walking |
|
| Narrow base of support |
Base of support (BOS) is the area formed by contact points of the feet with the ground. For e.g. when you stand with your feet shoulder width apart your BOS is the area covered between the feet. BOS changes with movement. Narrow BOS while walking can be noticed if there is crossing of feet noticed. Normal BOS is slightly less than shoulder width, the feet would be in line with the width of the hips. |
0 Yes
1 No |
|
| Freezes while walking |
Freezing is the sudden inability to move despite the intention to. We are looking to see if the participant experiences this sudden inability to move while walking |
0 Present
1 Absent |
|
| Looks at feet |
Does the participant look down at their feet while walking instead of looking forward |
0 Yes
1 No |
|
| Scuffs foot/Poor foot clearance |
Does the participant drag their foot (not lift it sufficiently to place it on the ground)? Please note you could select ‘Yes’ even if there is poor foot clearance on one side |
0 Yes
1 No |
|
| Unsteadiness while walking |
Experiences short instances of losing balance while walking without falling |
0 Yes
1 No |
|
| Pace dynamics while walking |
|
| Variable pace while walking |
A gait pattern where the pace of walking may fluctuate, with periods of slower movements interspersed with rapid uncontrollable acceleration. Does the participant experience bradykinesia and festination? |
0 Yes
1 No |
|
| Gait Parameters |
|
| Heel strike |
A heel strike is also known as initial contact. It is a phase of the gait cycle that occurs when the heel touches the ground while walking. Hint: When viewed anteriorly a complete visual of the sole when the heel contacts the ground indicates an optimal heel strike. |
2 Optimal
1 Weak
0 Absent
|
|
| Push-off |
The push-off phase involves the propulsion of the body forward as the foot pushes off the ground to initiate the swing phase of walking. Hint: A complete visual of the sole during the phase indicates an optimal push-off when viewed posteriorly. |
2 Optimal
1 Weak
0 Absent
|
|
| Fast Cadence |
Does the individual have an abnormal increase in speed or frequency of steps leading to a shuffling gait? |
0 Present
1 Absent |
|
| Swing at hip |
The swing phase is when the leg the leg is not in contact with the ground and actively moves forward to prepare for the next step. It is characterized by a series of movements at the hip joint including hip flexion, extension, and abduction/adduction which facilitate foot clearance and forward progression |
1 Optimal
(Step is initiated with an almost straight knee)
0 Weak
(Excessive movement of the knee from flexion to extension) |
|
| Symmetry |
|
| Gait Symmetry |
Gait symmetry refers to the equality between the movements of the left and right limbs during walking. This will be shown through differences in step length, time of foot contact with the ground and amplitude of joint movement |
1 Present
0 Absent
|
|
| Symmetry of arms while swinging |
The symmetry of the arms while walking refers to the equality between the arm swings on the right and left sides |
1 Present
0 Absent |
|
| Coordination of the arms with the legs |
This refers to balanced and alternating movement of the arms in coordination with the movement of the legs, contributing to a smooth and efficient gait pattern |
1 Present
0 Absent |
|
| Arm Swing |
|
| Forward arm swing |
The forward arm swing involves rotational movement of the arms alongside the body where the arm swing forward crossing the midaxillary line. Predominantly, forward arm swing is greater than backward arm swing |
2 Optimal
1 Reduced
0 Absent |
|
| Backward arm swing |
The backward arm swing entails rotational movement of the arms alongside the body where the arm swings backward crossing the midaxillary line. |
2 Optimal
1 Reduced
0 Absent |
|
| Posture |
|
| Flexed at hip |
Forward leaning of the trunk posture predominantly seen in those with PD is associated with flexion at the hip. This means the hips are bent or flexed forward, reducing range of motion at the hip contributing to an overall stooped appearance |
0 Yes
1 No |
|
| Rounded shoulders |
Rounded shoulders or slouches posture is a common postural issue where the shoulders are positioned forward, causing the upper back to appear rounded |
0 Yes
1 No |
|
| One shoulder lower than the other |
The shoulders may not be at the same level due to differences in muscle tone on either side of the body, which could lead to the asymmetric presentation of the shoulders |
0 Yes
1 No |
|
| Forward lean of the head |
It is a common postural misalignment, often evident when the head is positioned forward compared to the shoulders and the ear aligns ahead of the shoulder rather than directly over it |
0 Yes
1 No |
|
| Tremor |
|
| Tremor |
Arm tremors typically occur at rest and usually involve rhythmic shaking or oscillatory movements of the forearms/wrists/hands |
0 Present
1 Absent |
|
| Dyskinesia |
Dyskinesia is characterized by involuntary and uncontrolled movements that are often exaggerated or excessive. These movements can be jerky, writhing, or twisting, typically affecting the limbs, face, or trunk. Dyskinesia can manifest as chorea (rapid, jerky movements), dystonia (sustained muscle contractions causing twisting or repetitive movements) or athetosis (slow, writing movements) |
0 Present
1 Absent |
|
| Trunk while walking |
|
| Rotated |
The trunk would be twisted or rotated towards the affected side while walking due to differences in tone and muscle weakness |
0 Yes
1 No |
|
| Anteroposterior movement of the trunk |
Anteroposterior movement of the trunk refers to the normal forward and backward motion of the upper body during walking. For e.g. when we walk our trunk naturally sways back and forth in coordination with the movement of our legs |
0 Present
1 Absent |
|
| Turning |
|
| Unable to pivot |
Instead of pivoting on one foot (active rotation of the foot around its own vertical axis) to execute the turn, the individual may take small steps in a circle. |
0 Yes
1 No |
|
| Sitting on the chair |
|
| Unable to turn and sit in one motion |
Unable to turn and sit in one motion. Takes multiple small steps (more than 3 steps while turning to sit) |
0 Yes
1 No |
|
| Freezes while trying to sit on the chair |
Sudden inability to move despite the intention to. We are looking to see if the participant experiences this sudden inability to move while trying to sit on the chair. |
0 Yes
1 No |
|
| Uses arms as support to sit |
Does the participant us ethe support of the armrest/ side of the chair or place their arm on their thighs or knees to sit on the chair? |
0 Yes
1 No |
|
| Unable to control the descent |
The participant uses the support of both arms or one arm to control the descent on the chair or drops the entire body weight instantly |
0 Yes
1 No |
|
Appendix B
OpenCV library, SciPy library, NumPy, Pandas and the ‘os’ module. The parameters of heel strike and push-off were estimated using the angular velocity method in degrees/second (°/sec). and swing at the hip and arm swing were calculated by the angle in degrees (°) at the hip and shoulder, respectively. The angle at the joint was estimated using the dot product formula for two vectors,
where θ is the angle between a and b, ‖a‖ ‖b‖ is the magnitude of the vectors a and b. The angular velocity was estimated using the formula,
where
ω is the angular velocity, Δ
θ is the change in angle calculated using Δ
θ=
θn+1−
θn, Δ
t is the time interval between frames, Δ
t=1/
fps where fps is frames per second.
References
- Nguyen, G.; King, K.; Stirling, L. Telerehabilitation use and experiences in occupational and physical therapy through the early stages of the COVID-19 pandemic. PLOS ONE 2023, 18, e0291605. [Google Scholar] [CrossRef] [PubMed]
- Arntz, A.; Weber, F.; Handgraaf, M.; Lällä, K.; Korniloff, K.; Murtonen, K.-P.; Chichaeva, J.; Kidritsch, A.; Heller, M.; Sakellari, E.; et al. Technologies in Home-Based Digital Rehabilitation: Scoping Review. JMIR Rehabilitation and Assistive Technologies 2023, 10, e43615. [Google Scholar] [CrossRef]
- Arntz, A.; Weber, F.; Handgraaf, M.; Lällä, K.; Korniloff, K.; Murtonen, K.-P.; Chichaeva, J.; Kidritsch, A.; Heller, M.; Sakellari, E.; et al. Technologies in Home-Based Digital Rehabilitation: Scoping Review. JMIR Rehabilitation and Assistive Technologies 2023, 10, e43615. [Google Scholar] [CrossRef]
- Bernhardsson, S.; Larsson, A.; Bergenheim, A.; Ho-Henriksson, C.-M.; Ekhammar, A.; Lange, E.; Larsson, M.E.H.; Nordeman, L.; Samsson, K.S.; Bornhöft, L. Digital physiotherapy assessment vs conventional face-to-face physiotherapy assessment of patients with musculoskeletal disorders: A systematic review. PLOS ONE 2023, 18, e0283013. [Google Scholar] [CrossRef]
- Ali, A.; Sundaraj, K.; Ahmad, B.; Ahamed, N.; Islam, A. Gait disorder rehabilitation using vision and non-vision based sensors: A systematic review. Bosnian Journal of Basic Medical Sciences 2012, 12, 193. [Google Scholar] [CrossRef] [PubMed]
- Okochi, J.; Takahashi, T.; Takamuku, K.; Escorpizo, R. Staging of mobility, transfer and walking functions of elderly persons based on the codes of the International Classification of Functioning, Disability and Health. BMC Geriatrics 2013, 13, 16. [Google Scholar] [CrossRef]
- Hendriks, M.M.S.; Vos-Van Der Hulst, M.; Weijs, R.W.J.; Van Lotringen, J.H.; Geurts, A.C.H.; Keijsers, N.L.W. Using Sensor Technology to Measure Gait Capacity and Gait Performance in Rehabilitation Inpatients with Neurological Disorders. Sensors 2022, 22, 8387. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities. Medicine & Science in Sports & Exercise 2011, 43, 1575–1581. [Google Scholar] [CrossRef]
- Mate, K.K.V.; Mayo, N.E. Clinically Assessed Walking Capacity Versus Real-World Walking Performance in People with Multiple Sclerosis. International Journal of MS Care 2020, 22, 143–150. [Google Scholar] [CrossRef]
- Brandes, M.; Schomaker, R.; Möllenhoff, G.; Rosenbaum, D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait & Posture 2008, 28, 74–79. [Google Scholar] [CrossRef]
- Mate, K.K.; Abou-Sharkh, A.; Morais, J.A.; Mayo, N.E. Real-Time Auditory Feedback–Induced Adaptation to Walking Among Seniors Using the Heel2Toe Sensor: Proof-of-Concept Study. JMIR Rehabilitation and Assistive Technologies 2019, 6, e13889. [Google Scholar] [CrossRef]
- Hausdorff, J.M.; Hillel, I.; Shustak, S.; Del Din, S.; Bekkers, E.M.J.; Pelosin, E.; Nieuwhof, F.; Rochester, L.; Mirelman, A. Everyday Stepping Quantity and Quality Among Older Adult Fallers With and Without Mild Cognitive Impairment: Initial Evidence for New Motor Markers of Cognitive Deficits? The Journals of Gerontology: Series A 2018, 73, 1078–1082. [Google Scholar] [CrossRef] [PubMed]
- Keren, K.; Busse, M.; Fritz, N.E.; Muratori, L.M.; Gazit, E.; Hillel, I.; Scheinowitz, M.; Gurevich, T.; Inbar, N.; Omer, N.; et al. Quantification of Daily-Living Gait Quantity and Quality Using a Wrist-Worn Accelerometer in Huntington’s Disease. Frontiers in Neurology 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Kyriazis, V. Gait analysis techniques. Journal of Orthopaedics and Traumatology 2001, 2, 1–6. [Google Scholar] [CrossRef]
- Mayo, N.E.; Figueiredo, S.; Ahmed, S.; Bartlett, S.J. Montreal Accord on Patient-Reported Outcomes (PROs) use series – Paper 2: terminology proposed to measure what matters in health. Journal of Clinical Epidemiology 2017, 89, 119–124. [Google Scholar] [CrossRef]
- McLeod, L.D.; Coon, C.D.; Martin, S.A.; Fehnel, S.E.; Hays, R.D. Interpreting patient-reported outcome results: US FDA guidance and emerging methods. Expert Review of Pharmacoeconomics & Outcomes Research 2011, 11, 163–169. [Google Scholar] [CrossRef]
- Berg, A.T.; Ludwig, N.N.; Wojnaroski, M.; Chapman, C.A.T.; Hommer, R.; Conecker, G.; Hecker, J.Z.; Downs, J. FDA Patient-Focused Drug Development Guidances. Neurology 2024, 102. [Google Scholar] [CrossRef]
- Brunnekreef, J.J.; Van Uden, C.J.; Van Moorsel, S.; Kooloos, J.G. Reliability of videotaped observational gait analysis in patients with orthopedic impairments. BMC Musculoskeletal Disorders 2005, 6. [Google Scholar] [CrossRef]
- Anwary, A.R.; Yu, H.; Vassallo, M. Gait quantification and visualization for digital healthcare. Health Policy and Technology 2020, 9, 204–212. [Google Scholar] [CrossRef]
- Muro-De-La-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait Analysis Methods: An Overview of Wearable and Non-Wearable Systems, Highlighting Clinical Applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef]
- Shanahan, C.J.; Boonstra, F.M.C.; Cofré Lizama, L.E.; Strik, M.; Moffat, B.A.; Khan, F.; Kilpatrick, T.J.; Van Der Walt, A.; Galea, M.P.; Kolbe, S.C. Technologies for Advanced Gait and Balance Assessments in People with Multiple Sclerosis. Frontiers in Neurology 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, V.; Marín-Jiménez, M.; Zisserman, A. 2D Human Pose Estimation in TV Shows. Springer Berlin Heidelberg: 2009; pp. 128-147.
- Tao, W.; Liu, T.; Zheng, R.; Feng, H. Gait Analysis Using Wearable Sensors. Sensors 2012, 12, 2255–2283. [Google Scholar] [CrossRef] [PubMed]
- Guk, K.; Han, G.; Lim, J.; Jeong, K.; Kang, T.; Lim, E.-K.; Jung, J. Evolution of Wearable Devices with Real-Time Disease Monitoring for Personalized Healthcare. Nanomaterials 2019, 9, 813. [Google Scholar] [CrossRef]
- Liao, Y.; Thompson, C.; Peterson, S.; Mandrola, J.; Beg, M.S. The Future of Wearable Technologies and Remote Monitoring in Health Care. American Society of Clinical Oncology Educational Book 2019, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Follis; Chen; Mishra; Howe; Toosizadeh; Dohm. Comparison of wearable sensor to traditional methods in functional outcome measures: A systematic review - PubMed. Journal of orthopaedic research : official publication of the Orthopaedic Research Society 2021 Oct, 39. [CrossRef]
- Prisco; Pirozzi; Santone; Esposito; Cesarelli; Amato; Donisi. Validity of Wearable Inertial Sensors for Gait Analysis: A Systematic Review - PubMed. Diagnostics (Basel, Switzerland) 12/27/2024, 15. [CrossRef]
- Shanahan, C.J.; Boonstra, F.M.C.; Cofré Lizama, L.E.; Strik, M.; Moffat, B.A.; Khan, F.; Kilpatrick, T.J.; Van Der Walt, A.; Galea, M.P.; Kolbe, S.C. Technologies for Advanced Gait and Balance Assessments in People with Multiple Sclerosis. Frontiers in Neurology 2018, 8. [Google Scholar] [CrossRef]
- Menychtas, D.; Petrou, N.; Kansizoglou, I.; Giannakou, E.; Grekidis, A.; Gasteratos, A.; Gourgoulis, V.; Douda, E.; Smilios, I.; Michalopoulou, M.; et al. Frontiers | Gait analysis comparison between manual marking, 2D pose estimation algorithms, and 3D marker-based system. Frontiers in Rehabilitation Sciences 2023/09/06, 4. [CrossRef]
- Hii, C.S.T.; Gan, K.B.; Zainal, N.; Mohamed Ibrahim, N.; Azmin, S.; Mat Desa, S.H.; Van De Warrenburg, B.; You, H.W. Automated Gait Analysis Based on a Marker-Free Pose Estimation Model. Sensors 2023, 23, 6489. [Google Scholar] [CrossRef]
- Hausdorff, J.M. Gait dynamics in Parkinson’s disease: Common and distinct behavior among stride length, gait variability, and fractal-like scaling. Chaos 2009 Jun 29, 19. [CrossRef]
- Eastlack, M.E.; Arvidson, J.; Snyder-Mackler, L.; Danoff, J.V.; McGarvey, C.L. Interrater Reliability of Videotaped Observational Gait-Analysis Assessments. Physical Therapy 1991, 71, 465–472. [Google Scholar] [CrossRef]
- Guo, Y.; Yang, J.; Liu, Y.; Chen, X.; Yang, G.-Z. Detection and assessment of Parkinson’s disease based on gait analysis: A survey. Frontiers in Aging Neuroscience 2022, 14. [Google Scholar] [CrossRef]
- Krebs, D.E.; Edelstein, J.E.; Fishman, S. Reliability of Observational Kinematic Gait Analysis. Physical Therapy 1985, 65, 1027–1033. [Google Scholar] [CrossRef]
- Ridao-Fernández, C.; Pinero-Pinto, E.; Chamorro-Moriana, G. Observational Gait Assessment Scales in Patients with Walking Disorders: Systematic Review. BioMed Research International 2019, 2019, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.; Jankovic, J.; Suteerawattananon, M.; Wankadia, S.; Caroline, K.S.; Vuong, K.D.; Protas, E. Clinical gait and balance scale (GABS): validation and utilization. Journal of the Neurological Sciences 2004, 217, 89–99. [Google Scholar] [CrossRef]
- Rancho Los Amigos Medical Center Professional Staff, A.; Rancho Los Amigos Medical Center Pathokinesiology, S.; Rancho Los Amigos Medical Center Physical Therapy, D. Observational gait analysis handbook; Professional Staff Association, Rancho Los Amigos Medical Center: Downey, Calif., 1989.
- Vadnerkar, A.; Figueiredo, S.; Mayo, N.E.; Kearney, R.E. Classification of gait quality for biofeedback to improve heel-to-toe gait. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 26-30 Aug. 2014, 2014; pp. 3626-3629.
- Vadnerkar, A.; Figueiredo, S.; Mayo, N.E.; Kearney, R.E. Design and Validation of a Biofeedback Device to Improve Heel-to-Toe Gait in Seniors. IEEE Journal of Biomedical and Health Informatics 2018, 22, 140–146. [Google Scholar] [CrossRef]
- Carvalho, L.P.; Mate, K.K.V.; Cinar, E.; Abou-Sharkh, A.; Lafontaine, A.-L.; Mayo, N.E. A new approach toward gait training in patients with Parkinson’s Disease. Gait & Posture 2020, 81, 14–20. [Google Scholar] [CrossRef]
- Mayo, N.E.; Mate, K.K.V.; Fellows, L.K.; Morais, J.A.; Sharp, M.; Lafontaine, A.-L.; Hill, E.T.; Dawes, H.; Sharkh, A.-A. Real-time Auditory Feedback for Improving Gait and Walking in People with Parkinson’s Disease: A Pilot and Feasibility Trial. 2024. [CrossRef]
- Islam, M.S.; Rahman, W.; Abdelkader, A.; Lee, S.; Yang, P.T.; Purks, J.L.; Adams, J.L.; Schneider, R.B.; Dorsey, E.R.; Hoque, E. Using AI to measure Parkinson’s disease severity at home. npj Digital Medicine 2023, 6, 156. [Google Scholar] [CrossRef] [PubMed]
- Connie, T.; Aderinola, T.B.; Ong, T.S.; Goh, M.K.O.; Erfianto, B.; Purnama, B. Pose-Based Gait Analysis for Diagnosis of Parkinson’s Disease. Algorithms 2022, 15, 474. [Google Scholar] [CrossRef]
- Latreche, A.; Kelaiaia, R.; Chemori, A.; Kerboua, A. Reliability and validity analysis of MediaPipe-based measurement system for some human rehabilitation motions. Measurement 2023, 214, 112826. [Google Scholar] [CrossRef]
- Ramesh, S.H.; Lemaire, E.D.; Tu, A.; Cheung, K.; Baddour, N. Automated Implementation of the Edinburgh Visual Gait Score (EVGS) Using OpenPose and Handheld Smartphone Video. Sensors 2023, 23, 4839. [Google Scholar] [CrossRef]
- Yang, Y.; Liu, P.; Sun, Y.; Yu, N.; Wu, J.; Han, J. A Video-Based Method to Classify Abnormal Gait for Remote Screening of Parkinson’s Disease. 2021.
- Kiely; Butterworth; Watson; Wooden. The Symbol Digit Modalities Test: Normative data from a large nationally representative sample of Australians - PubMed. Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists 2014 Dec, 29. [CrossRef]
- Tang, W.; van Ooijen, P.M.A.; Sival, D.A.; Maurits, N.M. Automatic two-dimensional & three-dimensional video analysis with deep learning for movement disorders: A systematic review. Artificial Intelligence in Medicine 2024, 156, 102952. [Google Scholar] [CrossRef]
- Hulleck, A.A.; Menoth Mohan, D.; Abdallah, N.; El Rich, M.; Khalaf, K. Present and future of gait assessment in clinical practice: Towards the application of novel trends and technologies. Frontiers in Medical Technology 2022, 4. [Google Scholar] [CrossRef]
- Norman, G.R.; Streiner, D.L. Biostatistics: the bare essentials; PMPH USA (BC Decker): 2008.
- Kim, J.; Kim, R.; Byun, K.; Kang, N.; Park, K. Assessment of temporospatial and kinematic gait parameters using human pose estimation in patients with Parkinson’s disease: A comparison between near-frontal and lateral views. PLOS ONE 2025, 20, e0317933. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Shimatani, K.; Ishige, Y.; Takemura, H.; Yamamoto, M.; Shimatani, K.; Ishige, Y.; Takemura, H. Verification of gait analysis method fusing camera-based pose estimation and an IMU sensor in various gait conditions. Scientific Reports 2022 12:1 2022-10-21, 12. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).