1. Introduction
Complete edentulism continues to pose a significant public health concern, particularly among aging populations, with reported prevalence ranging between 7% and 70% globally depending on the age group and region [
1,
2,
3]. In Romania and other parts of Eastern Europe, edentulism remains relatively high due to delayed access to oral healthcare and limited prosthodontic interventions in underserved communities [
4,
5].
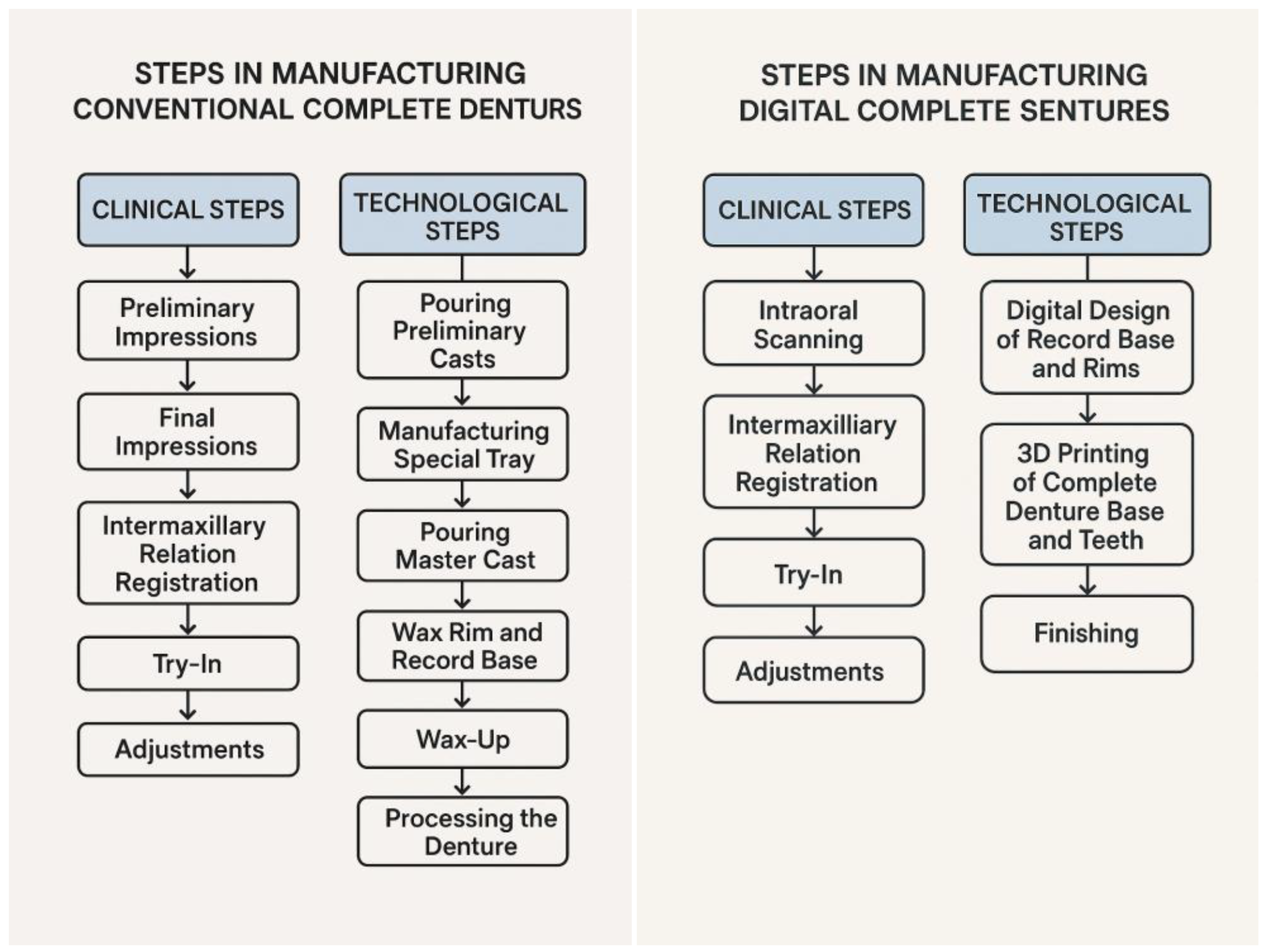
For decades,
conventional complete dentures (C-CD) have been the primary approach to rehabilitate fully edentulous patients. These prostheses, fabricated through traditional analog workflows, require multiple clinical steps including impressions (preliminary and final), bite registrations, try-ins and adjustments along with the technological stages: pouring preliminary and master cast, manufacturing special tray, wax rim and recorde base, wax up, processing the denture. While time-tested, conventional dentures are often associated with
clinical limitations such as material shrinkage, tissue distortion, reduced retention, and the need for frequent post-insertion corrections [
6,
7].
Recent advancements in dental technology have introduced
digitally fabricated complete dentures (D-CD) using computer aided design and computer aided manufacturing (CAD/CAM), milling or 3D-printing techniques. These approaches offer significant benefits, including improved precision and reproducibility, enhanced tissue adaptation, faster technological timelines, and better control over occlusion and aesthetics [
8,
9]. Digital workflows also reduce the number of clinical appointments, which is particularly beneficial for elderly patients with limited mobility or systemic conditions [
10].
Evidence is increasingly supporting the clinical efficacy and patient-centered outcomes of digital dentures. Studies have shown that digitally fabricated dentures are associated with better retention, reduced sore spots, and improved comfort compared to conventional dentures [
11,
12,
13]. However, few clinical trials have utilized a
crossover design, where patients directly compare both treatment modalities within the same study. Additionally, the
impact of this direct comparison on patient perception and final prosthetic preference remains underexplored.
Therefore, a research was performed to bridge the gap by allowing patients to directly experience both prosthetic options before expressing a preference. The primary aim of the study was to compare patient satisfaction with conventional and digital complete maxillary dentures in a fully edentulous population using a prospective, randomized, crossover design.
Secondary objectives included:
Assessing the change in patient perception after experiencing both prosthesis types.
Evaluating the internal consistency of a patient satisfaction questionnaire (PSQ).
Identifying the preferred prosthesis at the end of the study and patient recommendations for future users.
By integrating validated tools and allowing patients to evaluate both treatment modalities, this study aims to provide a robust, patient-centered comparison that reflects real-world clinical decision-making.
2. Materials and Methods
2.1. Participants
Forty complete maxillary edentulous patients were selected between 2023 and 2024, based on the following inclusion criteria: patients with complete maxillary edentulism, good oral hygiene, free of any systemic diseases that may affect oral health, no contraindications to the materials used for complete dentures The exclusion criteria were: uncontrolled systemic disease, infectious diseases, partial maxillary edentulism, temporo-mandibular disorders, xerostomia, oro-facial pain, patients who could not read informed consent form, patients with congenital or acquired defects in maxilla and/or mandible, patients considered ineligible for study inclusion by the principal investigator.
All participants signed an informed consent form that included a description of the intervention.
2.2. Study Design
The trial was designed as a prospective, randomized, single center study. The study protocol was approved by the institutional ethics committee (approval No: IRB/2024/7). No deviations were made from the registered protocol. The clinical trial was conducted in accordance with the Declaration of Helsinki and Consolidated Standards of Reporting Trials (CONSORT) guidelines.
The two prosthetic restorations assessed were the maxillary conventional complete denture (C-CD) and digital maxillary complete denture (D-CD).
Figure 1 presents the C-CD and D-CD manufacturing steps flowchart.
After completing the selection criteria, the participants were randomly divided into two groups: Group 1 (n1=20) and Group 2 (n2=20). One clinical staff member not involved in the study was responsible for group allocation. Group 1 received conventional complete denture (Ivobase+Phonare II, Ivoclar) for 6 months and Group 2 used digital complete denture (CAD/CAM-designed, Denture 3D+, NextDent+Harz Labs Dental Sand ) the same time period. Six months later, the treatments were switched. Patients who initially received a conventional complete denture changed it to a new digital one and digital complete denture wearers changed it to a conventional complete prosthesis after the same six months After experiencing both the conventional and digital treatment for six month each (twelve month in total), the participants were asked to select their preferred prosthesis and to continue using it. In this study, a wash-out between using C-CD and D-CD was not provided because the absence of a maxillary denture for an additional period was considered detrimental for edentulous patients and not being a feasible option.
2.3. Data Collection
I. Baseline Data: Age, gender, dental history, reason for tooth loss.
II. Patient Satisfaction Questionnaire (PSQ) adapted for removable complete dentures. During the follow-up of the two periods, patients were asked to complete a patient satisfaction questionnaire after 6 (T1) and 12 (T2) months with each denture.
A validated 9+1-items questionnaire was used in this study to measure patient satisfaction in terms of comfort, aesthetics, stability, ability to speak, masticatory efficiency, retention, need for adjustments, oral condition and general satisfaction. The patients rated each domain from 0 (lowest satisfaction) to 5 (highest satisfaction). The tenth item on follow-up after 12 month investigated which type of prosthesis patients would recommend.
Table 1.
Patient Satisfaction Questionnaire (PSQ) completed by the patients.
Table 1.
Patient Satisfaction Questionnaire (PSQ) completed by the patients.
Instructions: Please rate your level of satisfaction with your complete dentures by selecting the most appropriate response for each statement.
|
| Item |
1
Very Low |
2
Low |
3
Neutral |
4
High |
5
Very High |
1. Comfort:
How comfortable are your dentures when wearing them? |
☐ |
☐ |
☐ |
☐ |
☐ |
2. Aesthetics:
How happy are you with the way your dentures look? |
☐ |
☐ |
☐ |
☐ |
☐ |
3. Ease of insertion and removal:
How easy is it for you to put in and take out your dentures? |
☐ |
☐ |
☐ |
☐ |
☐ |
4. Speech clarity:
How well can you speak while wearing your dentures? |
☐ |
☐ |
☐ |
☐ |
☐ |
5. Chewing efficiency:
How well are you able to chew food with your dentures? |
☐ |
☐ |
☐ |
☐ |
☐ |
6. Retention and stability:
How well do your dentures stay in place during daily use? |
☐ |
☐ |
☐ |
☐ |
☐ |
7. Sore spots and irritation:
Have you experienced pain, sore spots, or irritation from your dentures? |
☐ |
☐ |
☐ |
☐ |
☐ |
8. Need for adjustments:
How often have you needed denture adjustments? |
☐ |
☐ |
☐ |
☐ |
☐ |
9. Overall satisfaction:
How satisfied are you overall with your complete dentures? |
☐ |
☐ |
☐ |
☐ |
☐ |
10. Recommendation:
Which denture would you recommend to other patients? |
☐ Conventional ☐ Digital |
| Scoring and interpretation: |
|
Timeline
2.4. Data Analysis
Data were analyzed using R Core Team (2024), Version 4.3.3. The following statistical tests were applied:
Descriptive statistics (median, interquartile range) for all outcome variables.
The Wilcoxon signed-rank test was used for within-subject comparisons between the two denture types (C-CD vs D-CD) in the crossover design.
The Mann–Whitney U test was used for group comparisons of independent samples, such as comparing patient satisfaction between groups at specific time points (e.g., Group 1 vs Group 2 at T1 or T2).
Cronbach’s alpha was calculated to evaluate the internal consistency and reliability of the PSQ items.
All statistical tests were two-sided, and a p-value ≤ 0.05 was considered statistically significant.
3. Results
3.1. Baseline Characteristics
Forty patients (mean age 58.7 years, (IQR 3.75–9.00) were enrolled, including 24 men (60%) and 16 women (40%). Regarding the opposing mandibular arch, 45% had complete dentures, 35% had removable partial dentures, and 20% had fixed prosthetic restorations (
Table 2).
3.2. Patient Satisfaction Questionnaire (PSQ)
Table 3 presents the descriptive statistics for all PSQ domains across both evaluation points. At the 6-month follow-up (T1), digital complete dentures (D-CD) demonstrated significantly higher patient satisfaction compared to conventional complete dentures (C-CD) in the domains of comfort (p=0.04), retention (p=0.04), mastication (p=0.04), and need for adjustments (p=0.02). No significant differences were observed in aesthetics, stability, speech, oral condition, or overall satisfaction at this point (
Table 4).
At the 12-month follow-up (T2), after the crossover period, patient satisfaction with D-CD was significantly higher than with C-CD across almost all domains, including comfort (p<0.01), aesthetics (p=0.03), stability (p<0.01), speech (p<0.01), retention (p<0.01), mastication (p<0.01), need for adjustments (p<0.01), oral condition (p=0.03), and overall satisfaction (p<0.01), (
Table 4).
3.3. Internal Consistency
High internal consistency was observed across all PSQ data sets, with Cronbach’s alpha coefficients exceeding 0.90 (
Table 5). This indicates excellent reliability of the questionnaire responses and supports the credibility of patient-reported satisfaction.
3.4. Change in Patient Perception
The crossover design revealed important shifts in patient perception. For conventional dentures, patient satisfaction either declined or remained unchanged between T1 and T2, notably in comfort (p<0.01). Conversely, D-CD satisfaction scores improved over time, particularly in aesthetics (p=0.04), stability (p=0.04), speech (p=0.02), retention (p=0.04), mastication (p=0.04), need for adjustments (p=0.04), oral condition (p=0.04), and overall satisfaction (p=0.04) (
Table 6).
These results suggest that direct comparison and prolonged experience with both prosthetic types significantly influenced patient perception in favor of digital dentures.
3.5. Patient Preference and Recommendations
A clear preference for digital complete dentures was recorded at the end of the study: 24 out of 40 patients (60%) recommended D-CD, compared to 16 (40%) who preferred C-CD. Gender-wise, 10 women and 14 men favored digital dentures, while 6 women and 10 men preferred the conventional type (
Table 7).
4. Discussion
This prospective randomized crossover study aimed to compare patient satisfaction between conventional complete dentures (C-CD) and digital complete dentures (D-CD) in maxillary edentulous patients. The results demonstrated significantly greater satisfaction with D-CD across nearly all measured parameters, especially after patients had experienced both prosthetic types. This not only affirms the functional and aesthetic advantages of digital dentures but also highlights a clear shift in perception once patients became familiar with both systems.
The superior ratings for comfort, retention, stability, aesthetics, and reduced need for adjustments among D-CD users confirm findings from recent literature. Abdelnabi et al. [
11] reported that 3D-printed complete dentures demonstrate promising clinical outcomes, including high accuracy, reduced sore spots, and fewer post-insertion adjustments, making them a reliable alternative to conventional dentures [
11]. Kim et al. [
9], in a randomized controlled trial, also concluded that digital dentures provided
a non-inferior oral health-related quality of life compared to traditional dentures, with patients appreciating faster fabrication and better comfort [
9]. Our findings echo these observations, as D-CD wearers in our study reported significantly better speech, comfort, and less irritation. The CAD/CAM and 3D-printing technologies used in digital denture fabrication improve base adaptation and reduce processing errors such as polymerization shrinkage or porosity [
14,
15]. Digital dentures often provide better mucosal contact and retention due to accurate scanning and virtual design, enhancing stability and reducing sore spots [
16]. This was reflected in the significant improvement in retention, comfort, and adjustment-related satisfaction scores in our study.
Patient satisfaction is not solely functional; it also encompasses
aesthetic perception, psychological comfort, and social reintegration. Patients in our study favored D-CD in esthetics and speech clarity after the crossover, likely due to improved tooth positioning and phonetic design facilitated by digital articulation software. Similar findings were documented by Bidra et al. [
17], who found that digitally designed teeth arrangements enhanced smile lines and lip support. Moreover, psychological literature highlights that
empowering patients with modern, tech-based solutions can enhance confidence and perception of care quality [
18]. As digital dentures are often associated with innovation and progress, patients may perceive them as higher quality, even prior to wear experience.
The crossover design uniquely enabled the observation of patient perception changes, a valuable insight often overlooked in parallel-group studies. Initially, at T1, the differences between C-CD and D-CD were moderate. However, after experiencing both prostheses, patients clearly favored the digital dentures at T2. This evolution suggests that initial familiarity with conventional prosthetics may bias early satisfaction scores, but actual comparative experience reveals the superiority of digital solutions.
As noted by Zandinejad et al. [
13], some patients initially hesitate to adopt digital dentures, but adaptation and perception improve over time, especially when the digital prosthesis is better customized to the individual’s anatomy.
Digital workflows significantly reduce clinical chair time and visits, which is particularly beneficial for elderly or systemically compromised patients. Several studies report time savings of 30–50% with D-CDs compared to traditional methods [
19]. This advantage, coupled with fewer post-insertion visits (as seen in our low adjustment needs), makes D-CDs a viable solution in both public and private dental systems.
In settings like Romania, where dental care access is uneven, streamlined digital workflows may help reduce treatment barriers and standardize prosthetic outcomes in underserved communities [
4,
20]. This echoes findings by Singh et al. [
21], who reported that patient satisfaction with digital dentures increased notably after a two-week adaptation phase. It suggests that initial resistance to digital prostheses is often temporary and resolves with wear experience.
The high internal consistency (Cronbach's α > 0.90) across all questionnaires and scales adds robustness to our findings and confirms the reliability of patient feedback. The inclusion of a validated 10-item satisfaction questionnaire provided comprehensive coverage of patient-reported outcomes. Similar reliability has been observed in prior prosthodontic surveys using multi-item tools [
22], reinforcing the value of using standardized, patient-reported outcome measures (PROMs) in clinical research.
Moreover, by involving patients with various mandibular opposing arch conditions, this study reflects a real-world edentulous population, increasing the external validity of the findings.
This design revealed a significant change in perception, with most patients favoring the digital option after having experienced both. Initially, some domains showed minimal differences, likely due to familiarity bias toward conventional prosthetics. However, by the end of the trial, the majority of participants (60%) preferred D-CD, and this preference was more pronounced in males.
The consistent preference for D-CDs suggests several clinical benefits:
Fewer follow-up visits due to reduced need for adjustments.
Improved patient compliance and adaptation, particularly for first-time denture wearers.
More efficient fabrication processes, reducing chair time and lab coordination.
As digital workflows become more accessible and affordable, these advantages could significantly enhance the standard of care in prosthodontics, especially for underserved populations.
Despite its strengths, the study has several limitations. The lack of a wash-out period could have introduced residual adaptation bias. However, this was ethically justified, as prolonged maxillary edentulism is not clinically acceptable. Additionally, long-term follow-up was beyond the scope of this study. Future research should examine the durability, maintenance, and long-term satisfaction of digital dentures over periods exceeding one year.
Also, the one year follow-up period may not capture long-term wearability or prosthesis durability. Future studies should explore l
ong-term satisfaction and maintenance over 12–24 months, However, a recent systematic review and meta-analysis revealed that milled complete dentures would be recommended in dental practice [
23].
5. Conclusions
This study demonstrates that digital complete dentures provide superior patient satisfaction compared to conventional methods across multiple domains, including comfort, retention, aesthetics, and speech. Patients who experienced both types of dentures consistently favored the digital option, indicating a strong perception shift toward modern, digitally fabricated prostheses.
Digital dentures represent not just a technological advance but a significant improvement in patient-centered care. Their continued integration into clinical practice has the potential to redefine technology of dental prosthesis standards and outcomes.
The outcomes of this prospective, randomized crossover study clearly demonstrate that digital complete dentures (D-CD) outperform conventional complete dentures (C-CD) in terms of patient satisfaction across multiple functional and psychosocial parameters. After experiencing both treatment options, patients reported significantly greater comfort, retention, stability, speech ability, and esthetic satisfaction with digitally fabricated dentures. This consistent preference, supported by high internal consistency in patient responses, emphasizes the clinical relevance and reliability of the findings.
As digital technologies continue to mature, their widespread adoption may become central to delivering high-quality, personalized care to edentulous patients globally.
Author Contributions
Conceptualization, A.B.; methodology, A.B., and G.B.; software, A.M.; validation, M.S.; formal analysis A.B, and A.M.; investigation, A.B; writing–original draft preparation, A.B., M.S., and G.B.; writing–review and editing, A.B., and M.S.; supervision, G.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol was approved by the institutional ethics committee (approval No: IRB/2024/7). All procedures followed ethical standards in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent to participate in this study was obtained from the patients.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Borg-Bartolo R, Roccuzzo A, Molinero-Mourelle P, Schimmel M, Gambetta-Tessini K, Chaurasia A, Koca-Ünsal RB, Tennert C, Giacaman R, Campus G. Global prevalence of edentulism and dental caries in middle-aged and elderly persons: A systematic review and meta-analysis. J Dent. 2022 ;127:104335. [CrossRef]
- Vemulapalli A, Mandapati SR, Kotha A, Rudraraju H, Aryal S. Prevalence of complete edentulism among US adults 65 years and older: A Behavioral Risk Factor Surveillance System study from 2012 through 2020. J Am Dent Assoc. 2024 ;155(5):399-408.
- Zheng H, Shi L, Lu H, Liu Z, Yu M, Wang Y, Wang H. Influence of edentulism on the structure and function of temporomandibular joint. Heliyon. 2023 23;9(10):e20307. [CrossRef]
- Bida FC, Agop-Forna D, Bulancea BP, Balcoș C, Forna NC. An Observational Study on Oral Health and Quality of Life for RPD Wearers in the N-E Region of Romania. Medicina (Kaunas). 2022;58(9):1247. [CrossRef]
- Bacali C, Nastase V, Constantiniuc M, Lascu L, Badea ME. Oral Hygiene Habits of Complete Denture Wearers in Central Transylvania, Romania.Oral Health Prev Dent. 2021;19:107-113. [CrossRef]
- Zarb GA, Hobkirk J, Eckert S, Jacob R. Prosthodontic Treatment for Edentulous Patients: Complete Dentures and Implant-Supported Prostheses. 13th ed. Elsevier; 2013.
- Felton DA. Edentulism and comorbid factors. J Prosthodont. 2009;18(2):88–96. [CrossRef]
- Goodacre BJ, Goodacre CJ, Baba NZ. CAD/CAM complete dentures: a review of two commercial fabrication systems. J Calif Dent Assoc. 2014;42(6):407–416. [CrossRef]
- Kim TH, Huh JB, Lee J, Bae EB, Park CJ. Retrospective Comparison of Postinsertion Maintenances Between Conventional and 3D Printed Complete Dentures Fabricated in a Predoctoral Clinic. J Prosthodont.2021;30(S2):158-162. [CrossRef]
- Tew IM, Soo SY, Pow EHN. Digitally versus conventionally fabricated complete dentures: A systematic review on cost-efficiency analysis and patient-reported outcome measures (PROMs).J Prosthet Dent. 2025 ;133(4):998-1007. [CrossRef]
- Abdelnabi MH, Swelem AA. 3D-Printed Complete Dentures: A Review of Clinical and Patient-Based Outcomes. Cureus. 2023;15(12):e47479. [CrossRef]
- Avelino MEL, Costa RTF, Vila-Nova TEL, Vasconcelos BCDE, Pellizzer EP, Moraes SLD.J Prosthet Dent. 2024 Oct;132(4):748.e1-748.e10.Clinical performance and patient satisfaction with digitally fabricated dentures: A meta-analysis. J Prosthet Dent. 2024;132(4):748.e1-748.e10.
- Zandinejad A, Franciele F, Lin WS, Naimi-Akbar A. Clinical outcomes of milled, 3D-printed, and conventional complete dentures in edentulous patients: A systematic review and meta-analysis. J Prosthodont. 2024 ;33(8):736-747.
- Casucci A, Verniani G, Giovanni B, Fadil S, Ferrari M. Analog and digital complete denture bases accuracy and dimensional stability: an in-vitro evaluation at 24 hours and 6 months. J Dent. 2025:105658.: 10.1016. [CrossRef]
- Kalberer N, Mehl A, Schimmel M. CAD/CAM denture base adaptation: Clinical relevance and in vivo performance. Clin Oral Investig. 2022.
- Campos Sugio C.Y., Mosquim V., Jacomine J.C., Zabeu G.S., de Espindola G.G., Bonjardim L.R., Bonfante E.A., Wang L. Impact of rehabilitation with removable complete or partial dentures on masticatory efficiency and quality of life: A cross-sectional mapping study. J. Prosthet. Dent. 2021;128:1295–1302. [CrossRef]
- Wulfman C., Bonnet G., Carayon D., Lance C., Fages M., Vivard F., Daas M., Rignon-Bret C., Naveau A., Millet C. Digital removable complete denture: A narrative review. Fr. J. Dent. Med. 2020;10:1–9.
- Anadioti E., Musharbash L., Blatz M.B., Papavasiliou G., Kamposiora P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health. 2020;20:343. [CrossRef]
- Kattadiyil M.T., Jekki R., Goodacre C.J., Baba N.Z. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J. Prosthet. Dent. 2015;114:818–825. [CrossRef]
- Oncescu Moraru AM, Preoteasa CT, Preoteasa E. Masticatory function parameters in patients with removable dental prosthesis.J Med Life. 2019;12(1):43-48. [CrossRef]
- Ghassan M, Rola M, Hani O, Nawal A, Boulos P, Salameh Z Adaptation of Complete Denture Base Fabricated by Conventional, Milling, and 3-D Printing Techniques: An In Vitro Study. The Journal of Contemporary Dental Practice. 2020;2(4): 368-372.
- Allen PF. Assessment of patient satisfaction with complete dentures: The use of rating scales. Gerodontology. 2005.
- 23. Vincze ZÉ, Nagy L, Kelemen K, Cavalcante BGN, Gede N, Hegyi P, Bányai D, Köles L, Márton K. Milling has superior mechanical properties to other fabrication methods for PMMA denture bases: A systematic review and network meta-analysis. Dent Mater. 2025 Apr;41(4):366-382. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).