1. Introduction
Mild traumatic brain injury (mTBI), often synonymous with concussion, represents a significant and growing public health concern, affecting millions annually across the globe. Although most individuals recover within weeks, a substantial minority experience persisting post-concussion symptoms (PPCSs) that extend beyond the expected recovery window and profoundly impact quality of life, occupational function, and psychosocial well-being [
1]. Persistent symptoms are often heterogeneous and multifactorial, necessitating nuanced, flexible, and interdisciplinary models of care [
2].
Clinical guidelines increasingly call for team-based, patient-centered approaches to PPCS, in which professionals from different disciplines coordinate to provide comprehensive rehabilitation. Yet, despite this consensus, implementation across systems remains inconsistent, with few studies exploring the dynamics of interprofessional collaboration in real-world contexts. This article reviews the literature on interdisciplinary rehabilitation for mTBI and synthesizes insights from 100 interviews with rehabilitation professionals—including neurologists, neuropsychologists, optometrists, speech-language pathologists, occupational and physical therapists, and others—to glean practical lessons and conceptual insights.
This investigation emerged from a Phase I NINDS-funded clinical trial conducted by the Perception Dynamics Institute, which sought to evaluate a novel intervention targeting dorsal stream visual processing deficits in individuals with mTBI. As part of the NIH I-Corps program—an initiative that supports the commercialization of academic research and the identification of unmet clinical needs—our team conducted over 100 in-depth interviews with potential stakeholders, including healthcare professionals from a diverse array of rehabilitation disciplines. The team consisted of the first author and second author. The I-Corps program emphasizes experiential learning and real-world discovery; it requires participants to validate the translational potential of their interventions through structured stakeholder engagement. Through this process, we gathered first-hand insights into the diagnostic and therapeutic challenges of mTBI, especially those related to fragmented care, under-recognized visual impairments, and the lack of standardized interprofessional collaboration.
These interviews offered an unexpectedly rich source of qualitative data, revealing consistent patterns in how rehabilitation professionals—neurologists, neuropsychologists, optometrists, speech-language pathologists, occupational and physical therapists, and others—conceptualize and coordinate care for individuals with mTBI. The convergence of their experiences highlighted both the promise and the pitfalls of interdisciplinary practice in brain injury rehabilitation. Accordingly, this article draws on those interviews to review the existing literature on interdisciplinary rehabilitation and to construct a conceptual framework grounded in real-world clinical practice. It aims to illuminate emerging trends, persistent barriers, and opportunities for systemic improvement in team-based recovery models for mTBI. Despite increasing advocacy for team-based models, no existing studies have systematically synthesized structured interviews across multiple clinical disciplines to inform a conceptual framework grounded in actual practice environments.
Literature Review
The multifaceted nature of post-concussion symptoms—encompassing physical, cognitive, emotional, and behavioral domains—necessitates a comprehensive and interdisciplinary approach to rehabilitation. While initial management often emphasizes rest and reassurance, individuals with persistent post-concussion symptoms (PPCSs) benefit from more structured and collaborative interventions [
3,
4].
Mashima et al. (2021) advocate for the formation of core interdisciplinary teams (IDTs) comprising speech-language pathologists (SLPs), neuropsychologists, care coordinators, and rehabilitation physicians. They highlight the critical role of consistent interprofessional communication, validation of patient experiences, and consideration of the sociocultural context in recovery. Such interdisciplinary management is posited to reduce fragmented care and promote resilience, functional restoration, and community reintegration.
Building upon this, Nguyen et al. (2023) provide empirical support for an interdisciplinary program—i-RECOveR—that integrates psychology, physiotherapy, and medical interventions over a 12-week period. Their study demonstrated that 80% of participants with PPCSs experienced moderate to significant improvements in symptom severity and quality of life. The application of Goal Attainment Scaling (GAS) further underscored the value of individualized, patient-centered outcomes over standard clinical measures.
The importance of shifting from a deficit-based, diagnostic paradigm to a strength-based, functional approach is a recurring theme in the literature [
5]. Neuropsychological assessments may not always detect impairments; however, patient-reported cognitive inefficiencies, often exacerbated by sleep disorders, anxiety, depression, and pain, are valid concerns [
6,
7]. Interdisciplinary collaboration is essential to contextualize these symptoms, validate patient experiences, and tailor interventions to complex biopsychosocial profiles.
Operational pillars of effective interprofessional practice include:
Despite the recognized benefits of interdisciplinary approaches, numerous challenges persist in their implementation. A significant barrier is limited access to comprehensive rehabilitation services, leaving many patients and their families with unmet needs [
12]. Cognitive and behavioral complications, such as deficits in attention, memory, executive functioning, and impulsivity, further complicate the rehabilitation process, particularly when compounded by co-existing metabolic disorders that may exacerbate cognitive dysfunction [
10,
11].
Systemic barriers—including fragmented communication channels, differing professional cultures, and logistical constraints—also impede effective interdisciplinary collaboration, leading to disjointed care and suboptimal patient outcomes [
13]. Gagnon-Roy et al. (2024) emphasize the necessity of minimal and highly individualized cognitive interventions provided by occupational therapists, reinforcing the need for flexible, tailored strategies within broader team-based frameworks.
Addressing these challenges requires fostering better interprofessional understanding across disciplines. Enhanced interdisciplinary communication, regular cross-disciplinary meetings, collaborative care planning, and structured cross-training can bridge professional silos, promote mutual respect, and ensure cohesive, patient-centered rehabilitation. Such interprofessional synergy is critical to overcoming the identified barriers and improving the overall effectiveness of rehabilitation practices.
In sum, the literature supports a robust, multifaceted, and human-centered model of interdisciplinary care as a promising paradigm for improving recovery outcomes in mTBI. Nevertheless, addressing systemic barriers and cultivating a strong collaborative culture are vital to realizing the full potential of team-based rehabilitation. In the sections that follow, we synthesize data from 100 interviews with diverse rehabilitation professionals to examine how these principles are implemented—and occasionally challenged—in clinical practice.
2. Materials and Methods
2.1. Participant Recruitment and Sampling
Interview participants were selected through an iterative process combining convenience and snowball sampling techniques. Recruitment was initially guided by hypotheses derived from the business model CANVAS framework, as required by the NIH I-Corps program. Specifically, early assumptions identified behavioral optometrists as likely early adopters of a visual-cognitive intervention for mTBI. However, as data collection progressed, it became evident that a broader array of allied health professionals—such as neuropsychologists, occupational therapists, and speech-language pathologists—held critical stakeholder roles.
Initial participants were identified through the authors’ professional networks and affiliations across California, Alabama, New York, Colorado, and other U.S. regions. These participants then referred colleagues with relevant expertise in the diagnosis and rehabilitation of cognitive and sensory symptoms following mTBI. Eligibility criteria required that interviewees hold a graduate-level clinical or research degree in their respective fields (e.g., Ph.D., O.D., M.D., M.S., or equivalent) and have a minimum of five years of post-licensure or professional practice experience.
Recruitment channels included email invitations, NIH I-Corps cohort interactions, and institutional outreach. Interviewees represented a wide range of clinical environments, including academic medical centers, rehabilitation clinics, private practices, and community health organizations.
2.1.1. Interview Structure and Administration
Interviews were conducted using a structured protocol derived from the I-Corps “customer discovery” framework but tailored for clinical relevance. Interviews were conducted by the lead author and second author. Each interviewee was told that the goal of the interviews was to understand the professional “pain points” in mTBI care delivery, particularly regarding diagnosis, rehabilitation, interdisciplinary communication, and technology adoption. Core questions addressed current treatment practices, challenges in managing cognitive symptoms, interprofessional communication strategies, and the use of technology or tools in patient care. All participants were told about the nature of I-Core, the reasons for conducting the interviews, and what we hoped to learn by conducting the interviews. The characteristics of the interviewers were disclosed, informing the interviewees that author one was an academic researcher at a southeastern university in the US, and that the second author was a neuroscientist, inventor, and founder of Perception Dynamics Institute. As per ICorps requirements, data was managed in the Air Table CRM software.
Although the interview protocol began as a fixed set of questions, it evolved into a semi-structured format as new insights emerged. This allowed interviewers to pursue emergent themes while maintaining consistency across participants. Interviews were conducted primarily via Zoom, with a minority occurring in person. For interviews conducted in clinical settings or at academic conferences fields notes were made in addition to those in the Zoom platform. Each session lasted approximately 30 to 45 minutes.
2.1.2. Qualitative Analysis and Thematic Synthesis
Following data collection, interview notes were reviewed and synthesized using a pragmatic thematic analysis approach. This thematic analysis followed a pragmatic, inductive methodology. Manual coding was conducted iteratively, and constant comparison methods were used to refine themes across stakeholder responses. Although influenced by grounded theory principles, such as inductive logic and theme saturation, the study did not pursue formal theoretical development. The orientation prioritized applied insights consistent with translational qualitative research practices under the NIH I-Corps framework. Initially, coding was conducted manually without the use of qualitative analysis software. The coding process was largely inductive, with major themes emerging from repeated patterns in participants’ responses. These emergent codes were then iteratively clustered into higher-order thematic categories, such as “discipline-specific interventions,” “barriers to care integration,” and “technology adoption.” This process was facilitated by custom machine learning categorization software coded in Python by the first author using the ChatGPT .api as the natural language processing agent.
Theme development was guided by constant comparison methods, wherein new interview data were compared against previously coded responses to refine thematic boundaries. The research team—comprising the primary author and two collaborators—engaged in consensus-based theme refinement to ensure analytic validity. Given the high degree of repetition in reported challenges and solutions by the 80th interview, thematic saturation was deemed to have been reached prior to the completion of all 100 interviews.
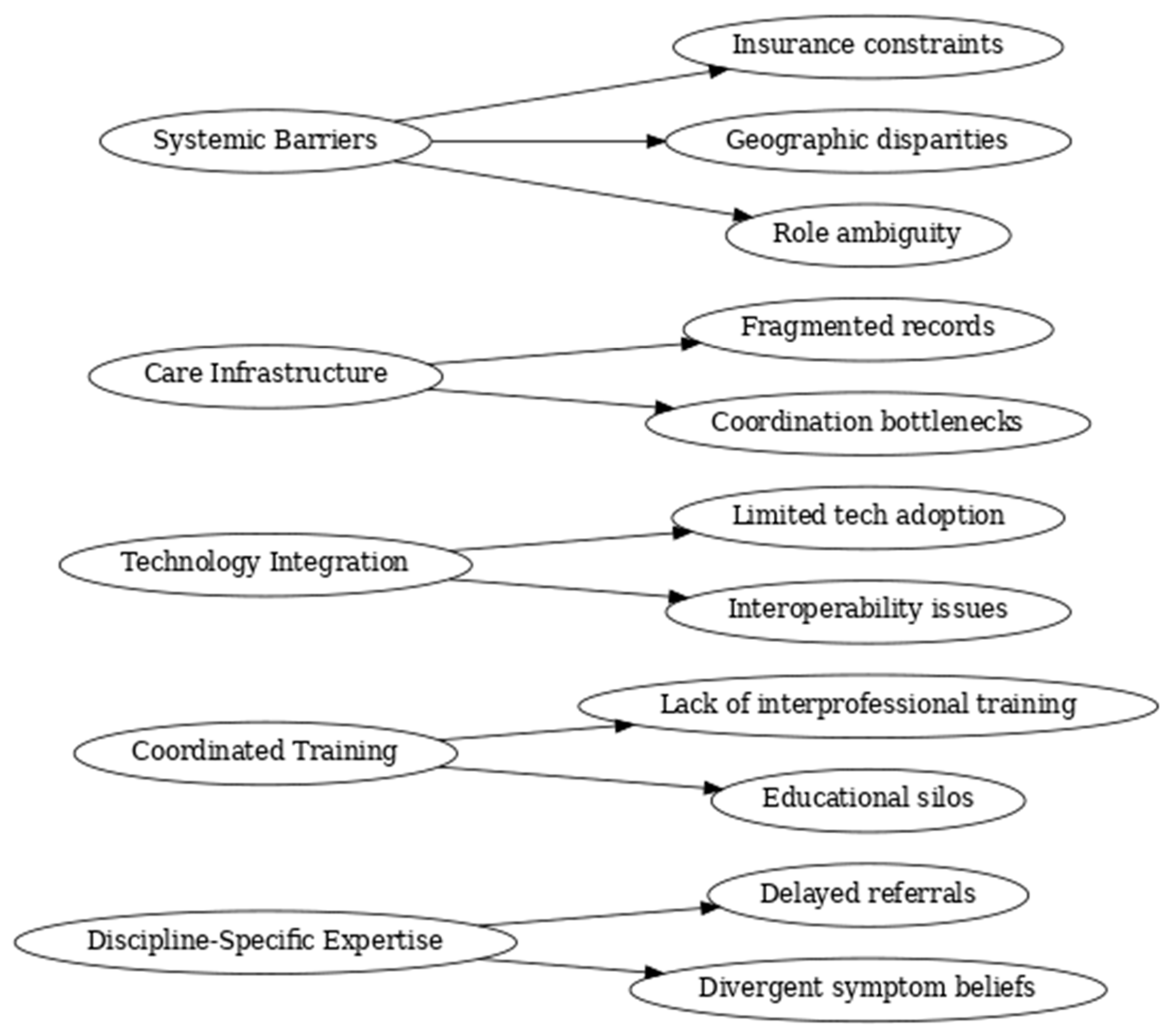
Figure 1.
Coding Tree Derived from Thematic Analysis of Stakeholder Interviews. This diagram illustrates the hierarchical structure of themes developed through inductive coding and constant comparison of 100 stakeholder interviews conducted as part of the NIH I-Corps program. Five core conceptual domains emerged: Discipline-Specific Expertise, Coordinated Training, Technology Integration, Care Infrastructure, and Systemic Barriers. Each domain is linked to specific subthemes reflecting clinician-reported experiences and challenges in the diagnosis, treatment, and coordination of mild traumatic brain injury (mTBI) rehabilitation. The coding tree reflects the analytic foundation of the study’s practice-informed conceptual framework for interprofessional care.
Figure 1.
Coding Tree Derived from Thematic Analysis of Stakeholder Interviews. This diagram illustrates the hierarchical structure of themes developed through inductive coding and constant comparison of 100 stakeholder interviews conducted as part of the NIH I-Corps program. Five core conceptual domains emerged: Discipline-Specific Expertise, Coordinated Training, Technology Integration, Care Infrastructure, and Systemic Barriers. Each domain is linked to specific subthemes reflecting clinician-reported experiences and challenges in the diagnosis, treatment, and coordination of mild traumatic brain injury (mTBI) rehabilitation. The coding tree reflects the analytic foundation of the study’s practice-informed conceptual framework for interprofessional care.
2.2. Ethical Considerations
This project was conducted under the auspices of the NIH I-Corps program, which is exempt from IRB oversight due to its focus on translational research and stakeholder discovery rather than human subjects research per se. Nonetheless, all participants provided informed verbal consent at the outset of each interview. Participants were specifically told that the authors were planning to turn the results of the interviews into an article, and verbal assent was obtained. Participants were assured of the voluntary nature of their involvement, and data were anonymized in all reporting and dissemination activities.
3. Results
3.1. Themes from Interdisciplinary Professional Interviews
A synthesis of 100 professional interviews with rehabilitation experts across disciplines reveals several converging themes regarding the treatment of mTBI. Professionals included neuropsychologists, optometrists, speech-language pathologists, occupational and physical therapists, neurologists, neurosurgeons, and rehabilitation case managers. While disciplinary perspectives varied, five dominant themes emerged.
1. Shared Commitment to Functional Recovery: Regardless of discipline, providers emphasized restoring daily functioning and life participation as central goals. Treatments were consistently tailored to real-world tasks (e.g., managing a calendar, navigating a classroom, returning to sport), reinforcing the practical, patient-centered nature of mTBI care.
2. Recognition of Cognitive Persistence in mTBI: Most clinicians acknowledged that mTBI can yield lasting cognitive symptoms, particularly in attention, working memory, and executive function. SLPs and neuropsychologists reported a strong correlation between cognitive symptoms and comorbidities such as anxiety, depression, or sensory overload. Optometrists noted similar persistence of visual symptoms. In contrast, some neurologists and surgeons questioned the duration and clinical significance of post-concussive cognitive complaints.
3. Barriers to Integration: Common frustrations included limited interdisciplinary communication, lack of shared medical records, role ambiguity, and insurance obstacles. Several professionals emphasized that the absence of structured team meetings and coordinated planning led to fragmented care. Others lamented the difficulty of getting referrals across disciplines.
4. Discipline-Specific Insights:
SLPs detailed their use of evidence-based cognitive-linguistic therapies, often tailored to executive deficits.
Optometrists emphasized neurovisual interventions such as syntonic phototherapy and digital eye tracking tools.
OTs highlighted sensory integration, vestibular rehab, and reflex modulation, often applying integrative methods like PATH neurotraining.
Physicians and Surgeons focused on diagnostic imaging and pharmacologic stabilization, generally deferring long-term rehab to allied professionals.
5. Technology, Training, and Advocacy: Participants highlighted the growing role of assistive software, from cognitive training programs to vision-tracking apps. However, adoption was uneven due to cost, training gaps, and interoperability. Many professionals described acting as advocates, guiding patients through complex rehabilitation systems and educating families to improve care continuity.
In summary, the interviews offer real-world confirmation of what the literature suggests: while interprofessional collaboration is essential to the effective treatment of mTBI, it remains hampered by systemic silos, training inconsistencies, and resource constraints. Nonetheless, the interviews also highlight innovation, shared purpose, and opportunities for reform.
3.2. Divergent Professional Perspectives on Symptom Persistence and Rehabilitation Roles
While there was broad consensus among professionals on the need for functional, patient-centered recovery approaches, interviews also surfaced notable divergences across disciplines—particularly in how providers conceptualize the persistence and clinical relevance of post-concussive symptoms. These differences, while not universally polarized, reflect underlying variations in professional training, epistemological frameworks, and clinical focus.
Speech-language pathologists (SLPs) and neuropsychologists, for instance, frequently emphasized the enduring nature of cognitive and communicative impairments following mTBI. One SLP observed, “We see patients months later who still can’t follow multistep instructions—this isn’t just anxiety, it’s real processing dysfunction.” A neuropsychologist echoed this sentiment, stating, “Even when standard batteries come back normal, patients report difficulties in executive function that meaningfully affect daily life.”
By contrast, several neurologists and neurosurgeons expressed skepticism regarding the prolonged trajectory of cognitive symptoms, often emphasizing objective findings over patient-reported experiences. One neurologist remarked, “From a neurological standpoint, if the scan is clean and it’s six months out, we start questioning whether the symptoms are neurologically driven or psychologically maintained.”
These differences were not purely academic; they shaped referral patterns, treatment recommendations, and expectations for recovery. Optometrists specializing in neurovisual rehabilitation noted that such skepticism often delayed referrals for visual interventions, despite persistent symptoms like photophobia or tracking deficits. Occupational therapists similarly reported that some patients arrived in therapy only after exhausting pharmacological or diagnostic avenues, by which point functional deterioration had already compounded.
This disciplinary heterogeneity underscores the importance of structured interprofessional dialogue and shared decision-making frameworks that validate patient-reported experiences while leveraging diverse clinical expertise. Without such integrative approaches, care risks becoming fragmented or hierarchically biased toward certain paradigms of evidence.
3.3. Equity, Access, and Structural Determinants of Interdisciplinary Care
While this study focused on the perspectives of clinicians, several participants independently raised concerns about disparities in access to interdisciplinary care. These disparities—rooted in insurance coverage, geographic proximity, and systemic inequities—pose substantial obstacles to the implementation of integrated rehabilitation frameworks.
Clinicians practicing in rural or underserved areas described limited access to allied professionals such as neuro-optometrists or SLPs trained in cognitive-communication therapy. One case manager in a midwestern community noted, “Our patients may have to drive three hours just to see a vestibular therapist, and that’s if their insurance even covers it.” Others lamented the logistical hurdles that prevent marginalized patients from participating in comprehensive team-based care, including transportation barriers, employment constraints, and caregiver burden.
These observations echo findings in the broader literature on health disparities in brain injury care. Research has shown that individuals from lower socioeconomic backgrounds and racial/ethnic minority groups are less likely to receive post-acute rehabilitation services, and when they do, the services tend to be shorter in duration and less comprehensive [
15,
16]. Additionally, structural racism in healthcare delivery—manifested through implicit bias, diagnostic overshadowing, and underrepresentation of minoritized clinicians—may contribute to differential treatment recommendations and patient engagement in rehabilitation settings.
To address these inequities, future models of interdisciplinary care must include strategies for equitable implementation. This includes expanding tele-rehabilitation networks, advocating for policy reform around Medicaid reimbursement, and embedding cultural competence training in interdisciplinary education. Ultimately, any scalable model must attend not only to the composition of the care team but also to the accessibility of that team across diverse populations.
Table 1.
Number of Interviewees by Profession.
Table 1.
Number of Interviewees by Profession.
| Profession |
Number Interviewed |
| Neuropsychologists |
18 |
| Speech-Language Pathologists |
16 |
| Occupational Therapists |
14 |
| Physical Therapists |
13 |
| Neurologists |
10 |
| Optometrists (Neuro) |
9 |
| Neurosurgeons |
8 |
| Rehabilitation Counselors |
7 |
| Recreation Therapists |
3 |
| Other (Case Managers, etc.) |
2 |
| Total |
100 |
Collectively, the findings from these 100 professional interviews converge around several interlocking domains critical to successful mTBI rehabilitation. These include discipline-specific expertise, coordinated training structures, integrated documentation and communication systems, and technology-enabled solutions, all shaped by the persistent influence of systemic barriers.
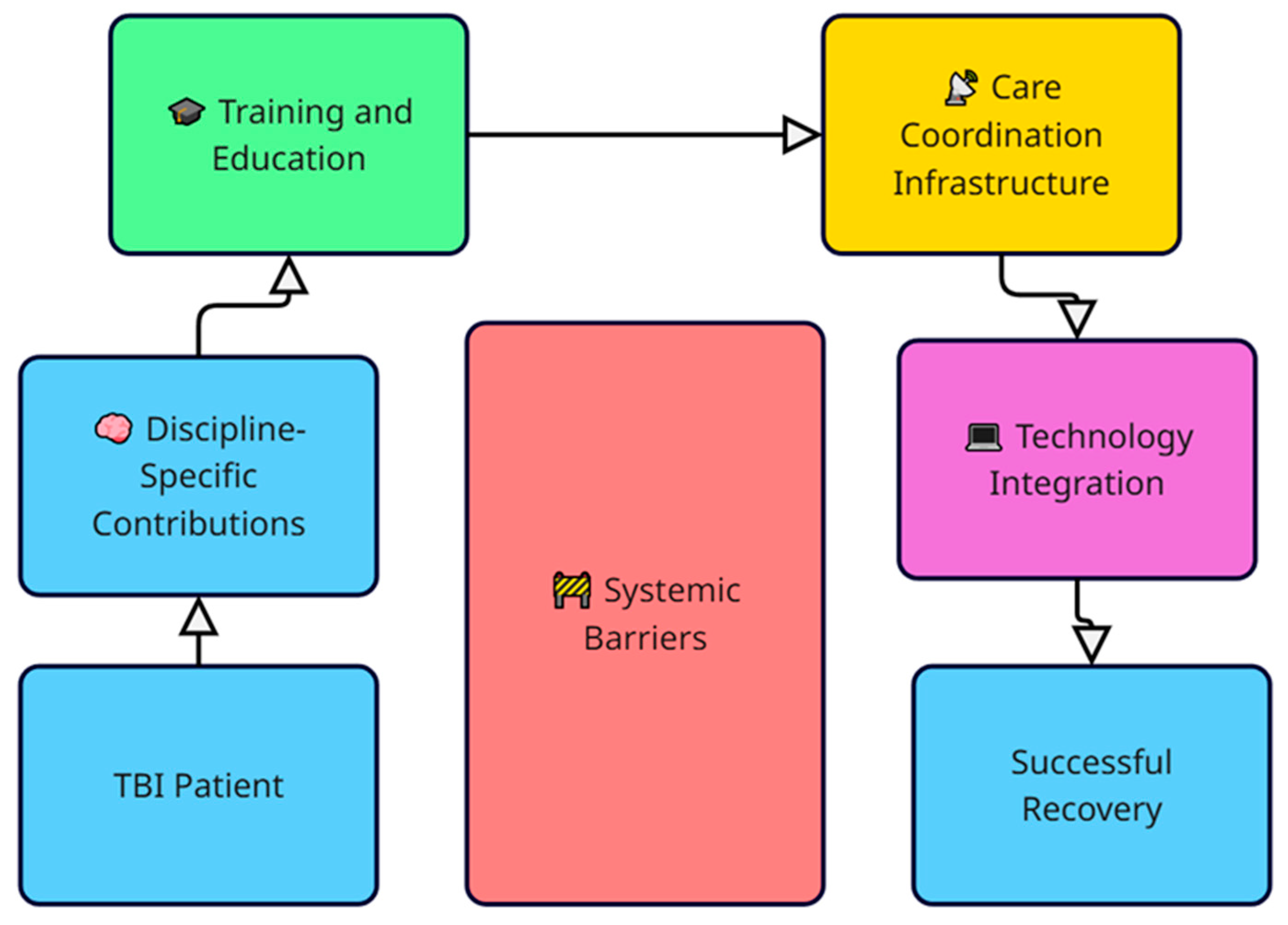
Figure 1 presents a conceptual framework synthesizing these domains and their interactions to illustrate the pathway toward successful recovery.
Figure 2.
Conceptual Framework for Interprofessional Rehabilitation in mTBI.
Figure 2.
Conceptual Framework for Interprofessional Rehabilitation in mTBI.
This model illustrates the proposed conceptual framework for interdisciplinary care in mild traumatic brain injury (mTBI) rehabilitation, derived from a synthesis of literature and 100 professional interviews. The framework begins with the TBI patient and emphasizes the importance of discipline-specific contributions, which feed into ongoing training and education. These educational structures support the development of care coordination infrastructure, which in turn enables technology integration to enhance communication, monitoring, and personalized interventions. Systemic barriers, including fragmented communication, reimbursement limitations, and role ambiguity, act as central impediments across all domains. Ultimately, the framework aims to support successful recovery by fostering dynamic, patient-centered, and technologically supported interprofessional collaboration.
4. Implications and Future Directions
The findings from this qualitative analysis provide several practical and conceptual implications for improving interdisciplinary care for patients with mTBI.
First, rehabilitation systems should prioritize the integration of care teams at both the structural and procedural levels. Interdisciplinary care models function best when supported by shared documentation systems, routine cross-specialty case reviews, and clearly defined communication protocols. Health systems can benefit from embedding care coordination roles or case managers whose primary responsibility is to facilitate interprofessional collaboration.
Second, there is a strong need for training programs to enhance interdisciplinary competence among healthcare providers. Many participants reported learning about collaboration on the job, often through trial and error. Introducing interprofessional modules into graduate-level clinical education for SLPs, OTs, PTs, optometrists, and medical doctors would address these training gaps and promote earlier exposure to team-based thinking.
Third, policy advocacy and reimbursement reform are essential. The fragmentation described by interviewees often stems from insurance limitations that disincentivize interdisciplinary consultations or undervalue non-physician services, such as neuro-optometric and recreational therapies. Policymakers and professional organizations should advocate for bundled or team-based reimbursement models that reflect the real-world needs of mTBI patients.
Fourth, the use of technology in interdisciplinary mTBI care deserves greater attention and standardization. While some professionals reported success with digital vision tracking, cognitive software, and virtual collaboration tools, adoption remains uneven. Clinical settings would benefit from curated guidelines that identify evidence-based digital tools and describe protocols for their implementation across disciplines.
Finally, future research should explore the longitudinal effects of collaborative care models on both clinical outcomes and cost-effectiveness. Quantitative studies measuring functional recovery, return-to-work rates, and quality of life following interdisciplinary versus siloed care would provide a robust evidence base for health systems aiming to redesign post-concussion services.
In sum, while challenges to integration persist, the voices of these 100 professionals point clearly toward a model of care that is not only collaborative in theory, but also flexible, patient-centered, and dynamically responsive to the evolving needs of individuals recovering from mTBI.
5. Conclusions
This study underscores the critical importance of interprofessional collaboration in the effective treatment of mild traumatic brain injury. The literature demonstrates clear advantages to a coordinated, patient-centered approach, particularly when dealing with persistent post-concussion symptoms. Insights from 100 diverse healthcare professionals reinforce this consensus, while also illuminating the ongoing challenges of fragmented systems, discipline-specific silos, and variable training in collaborative practices.
Collectively, the findings suggest that interdisciplinary care for mTBI must evolve beyond conceptual endorsement toward structural implementation. This includes adopting shared electronic health records, embedding interdisciplinary education within professional training pipelines, and advocating for insurance reform that supports coordinated care delivery.
Importantly, the voices of clinicians across neurology, optometry, speech pathology, and rehabilitation provide both validation and urgency to this call for reform. Their perspectives reveal a professional community eager to collaborate but constrained by outdated systems. Moving forward, research must rigorously evaluate the impact of interdisciplinary care models on long-term patient outcomes, while clinicians and institutions work to normalize collaborative frameworks in both acute and post-acute care settings.
Interdisciplinary rehabilitation for mTBI is no longer aspirational—it is essential. As the burden of concussion continues to grow, it is incumbent on the healthcare community to develop and sustain systems that reflect the complexity of recovery and the diversity of professional expertise required to support it.
Author Contributions
Conceptualization, J.S., T.L..; methodology, J.S..; software, J.S.; validation, J.S..; formal analysis, J.S..; investigation, J.S., T.L; resources, T.L.; data curation, J.S., writing—original draft preparation, J.S.,.; writing—review and editing, J.S., T.L.; visualization, J.S..; supervision, J.S..; project administration, T/L..; funding acquisition, T.L.. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by a Small Business Innovation Research (SBIR) grant to Perception Dynamics Institute from the National Institute of Neurological Disorders and Stroke (NINDS) at the National Institutes of Health (NIH), grant number 1R43NS132718.
Institutional Review Board Statement
The main study was conducted according to the guidelines of the Declaration of Helsinki, and approved by Pearl IRB, 29 E McCarty Street. Suite 100, Indianapolis, IN 46225, (317) 899-9341, info@pearlirb.com,
www.pearlirb.com for Protocol #23-PDI-101 on 1 March 2023. This interview project was conducted under the auspices of the NIH I-Corps program, which is exempt from IRB oversight due to its focus on translational research and stakeholder discovery rather than human subjects research per se. Nonetheless, all participants provided informed verbal consent at the outset of each interview.
Informed Consent Statement
Participants were specifically told that the authors were planning to turn the results of the interviews into an article, and verbal assent was obtained. Participants were assured of the voluntary nature of their involvement, and data were anonymized in all reporting and dissemination activities.
Data Availability Statement
Deindividuated data available on request from the corresponding author.
Acknowledgments
During the preparation of this manuscript/study, the author(s) used ChatGPT 4.0 for the purpose of creating a custom application to assist in coding and summarizing text and identifying themes. The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The second author (TL) has a potential conflict of interest, since she is the developer of the contrast sensitivity-based movement-discrimination training called PATH neurotraining and was employed by Perception Dynamics Institute. She had no part in analyzing the data, or writing the manuscript, however, thereby having no influence over the results that were obtained. The other authors declare that they have no potential conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| Abbreviation |
Full Text Equivalent |
| mTBI |
Mild Traumatic Brain Injury |
| TBI |
Traumatic Brain Injury |
| PPCSs |
Persistent Post-Concussion Symptoms |
| NIH |
National Institutes of Health |
| I-Corps |
Innovation Corps (NIH program) |
| NINDS |
National Institute of Neurological Disorders and Stroke |
| SLP |
Speech-Language Pathologist |
| SLPs |
Speech-Language Pathologists |
| OT |
Occupational Therapist |
| OTs |
Occupational Therapists |
| PT |
Physical Therapist |
| PTs |
Physical Therapists |
| IDT |
Interdisciplinary Team |
| GAS |
Goal Attainment Scaling |
| CRM |
Customer Relationship Management |
| IRB |
Institutional Review Board |
| PATH |
Perception-Attention-Timing-Harmony (neurotraining intervention) |
| SBIR |
Small Business Innovation Research |
References
- Nguyen, R.; O’Connor, E.; Williams, E.; Howe, M.; Saunders, R.; Mulhall, S. A single-case experimental design evaluation of the i-RECOveR interdisciplinary intervention for persistent post-concussion symptoms. Brain Injury 2023, 37, 286–296. [Google Scholar]
- Mashima, P. A.; Smith, K. M.; Sauder, C.; Pappadis, M. R.; Sander, A. M.; & Leon, A. C. Collaborative care for cognitive communication disorders in adults with mild traumatic brain injury: An interprofessional framework. Perspectives of the ASHA Special Interest Groups 2021, 6, 381–392. [Google Scholar]
- McCrea, M.; Guskiewicz, K. M.; Marshall, S. W.; Barr, W.; Randolph, C.; Cantu, R. C.; Onate, J. A.; Kelly, J. P. Acute effects and recovery time following concussion in collegiate football players: The NCAA Concussion Study. JAMA 2003, 290, 2556–2563. [Google Scholar] [CrossRef] [PubMed]
- Tapia, J. J.; Eapen, B. C. Concussion care: The role of early education. Federal Practitioner 2017, 34, 30–35. [Google Scholar]
- Sohlberg, M. M.; Turkstra, L. S. Optimizing cognitive rehabilitation: Effective instructional methods. Guilford Press, 2011. [Google Scholar]
- Rohling, M. L.; Binder, L. M.; Demakis, G. J.; Larrabee, G. J.; Ploetz, D. M.; Langhinrichsen-Rohling, J. A meta-analysis of neuropsychological outcome after mild traumatic brain injury: Reanalyses and reconsiderations of Binder et al. (1997), Frencham et al. (2005), and Pertab et al. (2009). The Clinical Neuropsychologist 2011, 25, 608–623. [Google Scholar] [CrossRef] [PubMed]
- McCrea, M.; Iverson, G. L.; McAllister, T. W.; Hammeke, T. A.; Powell, M. R.; Barr, W. B.; Kelly, J. P. An integrated review of recovery after mild traumatic brain injury (MTBI): Implications for clinical management. The Clinical Neuropsychologist 2009, 23, 1368–1390. [Google Scholar] [CrossRef] [PubMed]
- Suhr, J. A.; Gunstad, J. “Diagnosis threat”: The effect of negative expectations on cognitive performance in head injury. Journal of Clinical and Experimental Neuropsychology 2002, 24, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M. R. T. Coaching to promote executive function and strategy use for improved functional performance and self-regulation: A pilot study for adults with acquired brain injury. Disability and Rehabilitation 2017, 39, 1742–1751. [Google Scholar]
- Bryant, R. A.; O’Donnell, M. L.; Creamer, M.; McFarlane, A. C.; Silove, D.; Hadzi-Pavlovic, D. The psychiatric sequelae of traumatic injury. The American Journal of Psychiatry 2022, 169, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Prins, M. L.; Alexander, D.; Giza, C. C.; Hovda, D. A. Repetitive mild traumatic brain injury: Mechanisms of cerebral vulnerability. Journal of Neurotrauma 2013, 30, 30–38. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. (2022). Traumatic Brain Injury: A Roadmap for Accelerating Progress. The National Academies Press.
- Doig, E.; Fleming, J.; Kuipers, P. Interdisciplinary goal planning in brain injury rehabilitation: A process evaluation. Brain Injury 2023, 37, 513–525. [Google Scholar]
- Gagnon-Roy, M.; Bosquet, M.; Boudrias, M.-H. Personalized cognitive assistance for individuals with TBI: A feasibility study. Occupational Therapy International 2024, 2024, 1–11. [Google Scholar]
- Corrigan, J. D.; Selassie, A. W.; Orman, J. A. The epidemiology of traumatic brain injury. The Journal of Head Trauma Rehabilitation 2014, 25, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Gary, K. W.; Arango-Lasprilla, J. C.; Stevens, L. F. Do racial/ethnic disparities exist in post-injury rehabilitation outcomes after TBI? A comprehensive review. NeuroRehabilitation 2009, 24, 17–25. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).