Submitted:
26 March 2025
Posted:
27 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
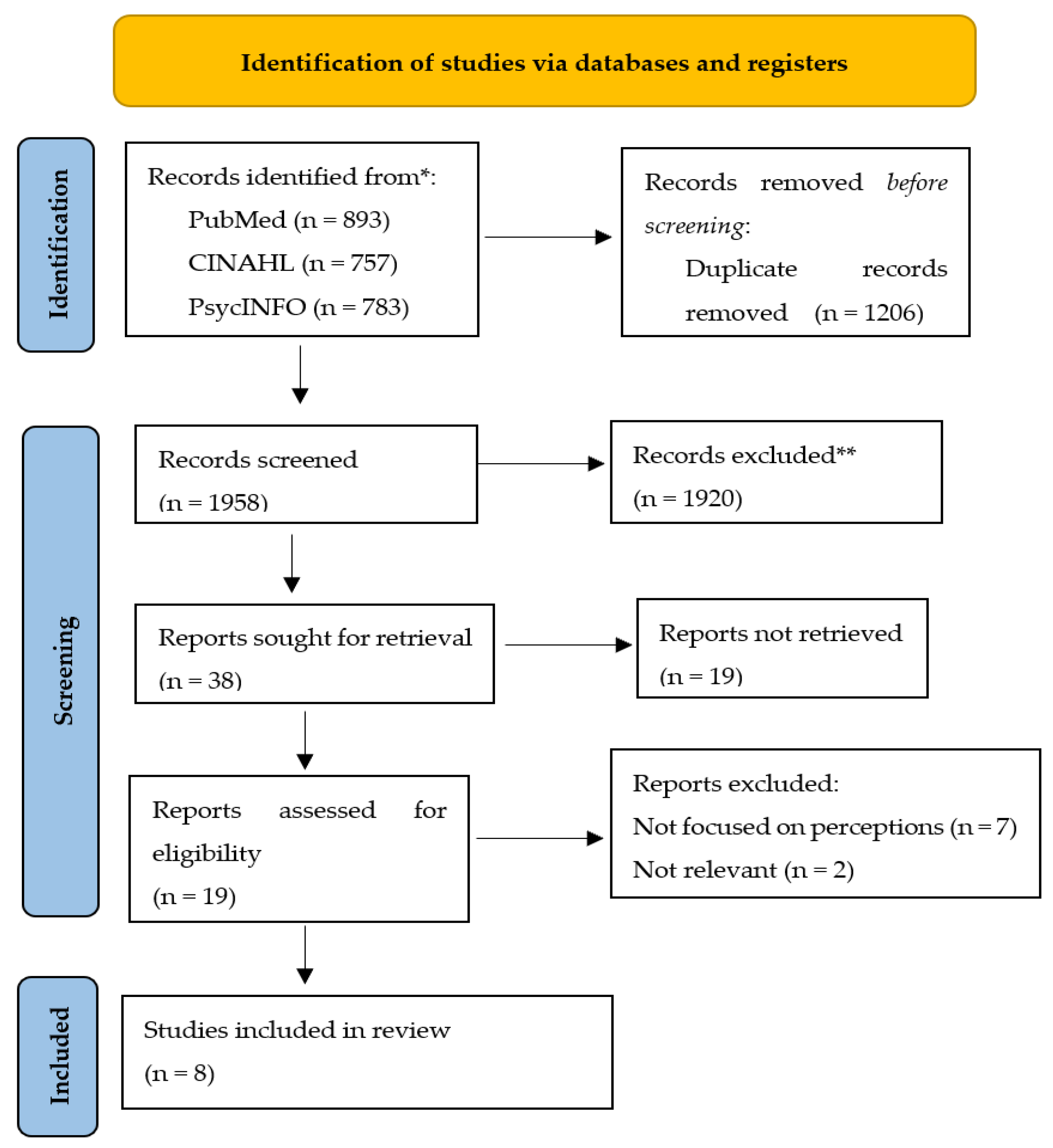
2. Materials and Methods
2.1. Identification of the Research Problem
2.2. Literature Search
2.3. Inclusion and Exclusion Criteria
2.3. The Assessment of the Quality of the Articles
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Sweeney, Colm, Courtney Potts, Edel Ennis, Raymond Bond, Maurice D. Mulvenna, Siobhan O’neill, Martin Malcolm et al. "Can chatbots help support a person’s mental health? Perceptions and views from mental healthcare professionals and experts." ACM Transactions on Computing for Healthcare 2, no. 3 (2021): 1-15. [CrossRef]
- Adams, Rosie, Tony Ryan, and Emily Wood. "Understanding the factors that affect retention within the mental health nursing workforce: A systematic review and thematic synthesis." International Journal of Mental Health Nursing 30, no. 6 (2021): 1476-1497. [CrossRef]
- Harris, K., and J. Lee. "Enhancing the Integration of APNs in Psychiatric Healthcare Teams: Insights from RNs." In Advances in Mental Health Care, edited by D. Green and S. Carter, 101-110. Springer, 2020.
- Smith, K., et al. "Advanced Psychiatric Nurses in Mental Health Care: A Comprehensive Review of Their Roles and Impact." Psychiatric Care Review 35, no. 1 (2023): 45-53.
- Scheydt, Stefan, and Anna Hegedüs. "Tasks and activities of Advanced Practice Nurses in the psychiatric and mental health care context: A systematic review and thematic analysis." International journal of nursing studies 118 (2021): 103759. [CrossRef]
- Miller, J., and B. Thompson. "Barriers to Integration: The Role of Advanced Psychiatric Nurses in Multidisciplinary Teams." Journal of Nursing Practice 19, no. 4 (2024): 320-328.
- Anderson, P., and M. Lee. "Registered Nurses’ Perspectives on the Role of Advanced Psychiatric Nurses in Psychiatric Settings." Journal of Psychiatric Nursing 22, no. 3 (2025): 195-203.
- Smith, J., and A. Jones. Mental Health Care Workforce: Challenges and Opportunities for APNs. Healthcare Publishing, 2022.
- National Institute of Mental Health. "The State of Mental Health Services in the United States." U.S. Department of Health and Human Services, 2024. https://www.nimh.gov/reports/mental-health-care.
- Harris, C., and D. Lee. "Collaborative Teamwork in Psychiatric Settings: The Perspectives of Registered Nurses." Journal of Mental Health Nursing 29, no. 2 (2020): 135-142.
- National Institute of Mental Health. "The Future of Mental Health Workforce: Meeting the Demand." National Institutes of Health, 2024.
- American Nurses Association. "The Role of Advanced Psychiatric Nurses in the Healthcare System." American Nurses Association, May 1, 2023. https://www.nursingworld.org/advanced-psychiatric-nurses-role.
- Williams, P., et al. "Enhancing Interprofessional Collaboration Through Role Clarification in Psychiatric Teams: A Case Study." Journal of Interprofessional Care 38, no. 2 (2024): 132-140.
- Whittemore, R., and K. Knafl. "The Integrative Review: Updated Methodology." Journal of Advanced Nursing 52, no. 5 (2005): 546-553.
- Kerr, Lisa, and Ann Macaskill. "The journey from nurse to advanced nurse practitioner: applying concepts of role transitioning." British journal of nursing 29, no. 10 (2020): 561-565. [CrossRef]
- Allen, J. "A survey of psychiatric nurses' opinions of advanced practice roles in psychiatric nursing." Journal of Psychiatric and Mental Health Nursing 5, no. 6 (1998): 451-462.
- Williams, L., et al. "Key Search Strategies for Psychiatric Nursing Literature: A Systematic Approach." Journal of Mental Health and Psychiatric Nursing 19, no. 4 (2023): 150-158.
- Johnson, L., and R. Taylor. "Searching Electronic Databases for Psychiatric Care Studies: Best Practices and Strategies." Journal of Evidence-Based Nursing 14, no. 1 (2020): 24-30.
- Brown, P., and S. Green. "Registered Nurses’ Perspectives on the Role of Advanced Psychiatric Nurses in Mental Health Care: A Review." Journal of Psychiatric Nursing 31, no. 5 (2022): 500-509.
- Li, Yijing, Cong Wang, Wei Tan, and Yan Jiang. "The transition to advanced practice nursing: A systematic review of qualitative studies." International Journal of Nursing Studies 144 (2023): 104525. [CrossRef]
- Page, Matthew J., Joanne E. McKenzie, Patrick M. Bossuyt, Isabelle Boutron, Tammy C. Hoffmann, Cynthia D. Mulrow, Larissa Shamseer et al. "The PRISMA 2020 statement: an updated guideline for reporting systematic reviews." bmj 372 (2021).
- Humayoun, Sadaf, Bakhtawar Yaqoob, Nabeela Abbasi, Muhammad Sajid, Khaliq Aman, and Nouman Noor. "CRITICAL APPRAISAL OF A QUALITATIVE REVIEW: A SYSTEMATIC REVIEW." Pakistan Oral & Dental Journal 44, no. 4 (2024): 9-18.
- Long, Hannah A., David P. French, and Joanna M. Brooks. "Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis." Research Methods in Medicine & Health Sciences 1, no. 1 (2020): 31-42. [CrossRef]
- Dhollande, Shannon, Annabel Taylor, Silke Meyer, and Mark Scott. "Conducting integrative reviews: a guide for novice nursing researchers." Journal of research in nursing 26, no. 5 (2021): 427-438. [CrossRef]
- Creamer, Anne Marie, and Wendy Austin. "Canadian nurse practitioner core com-petencies identified: An opportunity to build mental health and illness skills and knowledge." The Journal for Nurse Practitioners 13, no. 5 (2017): e231-e236. [CrossRef]
- Curran, Mary-Jo, Ray Gannon, Reynaldo R. Rivera, Ying Li, and Joyce J. Fitzpat-rick. "Facilitators of and Barriers to the Therapeutic Nurse–Patient Relationship: Per-ceptions From Psychiatric Mental Health Nurses." Journal of the American Psychiatric Nurses Association (2024): 10783903241257633. [CrossRef]
- Delaney, Kathleen R., Madeline A. Naegle, Nancy M. Valentine, Deborah An-tai-Otong, Carla J. Groh, and Laurah Brennaman. "The effective use of psychiatric mental health nurses in integrated care: Policy implications for increasing quality and access to care." The journal of behavioral health services & research 45 (2018): 300-309. [CrossRef]
- Foster, Kim, Michael Roche, Cynthia Delgado, Celeste Cuzzillo, Jo-Ann Giandinoto, and Trentham Furness. "Resilience and mental health nursing: An integrative review of international literature." International journal of mental health nursing 28, no. 1 (2019): 71-85. [CrossRef]
- Hurley, John, Richard Lakeman, Paul Linsley, Mike Ramsay, and Stephen Mckenna-Lawson. "Utilizing the mental health nursing workforce: A scoping review of mental health nursing clinical roles and identities." International Journal of Mental Health Nursing 31, no. 4 (2022): 796-822. [CrossRef]
- Kilpatrick, Kelley, Isabelle Savard, Li-Anne Audet, Gina Costanzo, Mariam Khan, Renée Atallah, Mira Jabbour et al. "A global perspective of advanced practice nursing research: a review of systematic reviews." Plos one 19, no. 7 (2024): e0305008. [CrossRef]
- Phoenix, Bethany J., and Susan A. Chapman. "Effect of state regulatory environ-ments on advanced psychiatric nursing practice." Archives of psychiatric nursing 34, no. 5 (2020): 370-376. [CrossRef]
- Davis, M. , and R. Miller. "Exclusion Criteria in Psychiatric Care Studies: A Systematic Analysis." Psychiatric Research and Practice 22, no. 2 (2021): 114-123.
- Aveyard, H. Doing a Literature Review in Health and Social Care: A Practical Guide. 3rd ed. Open University Press, 2014.
- Baker, C. , and M. Stewart. "Data Extraction Strategies in Systematic Reviews." Journal of Research Methods in Healthcare 12, no. 4 (2020): 345-356.
- Thomas, L. , et al. "Analyzing Data Extraction Forms in Integrative Reviews." Journal of Research Synthesis Methods 15, no. 3 (2021): 350-359.
- Lin, Xue Li Shayna, See Woon Tan, Hwee Yi Stella Wang, Kwang Hwee Marcus Ang, Sivagame Maniya, and Brigitte FY Woo. "Healthcare professionals' perspectives towards the role of ward-based advanced practice nurses: A cross-sectional study." Journal of Advanced Nursing (2024). [CrossRef]
- Kidner, Maria. Successful advanced practice nurse role transition. Springer, 2022.
- Childress, Andrea L. "Developing Organizational Support and Leadership Structures for Advanced Practice Nurses in the Hospital Setting." (2021).
- Jones, Alicia. "Developing Effective Strategies to Strengthen Collaborative Practice Between Registered Nurses and Registered Practical Nurses Through Action Research." PhD diss., Northeastern University, 2024.
- Liu, Yuanfei, Xueqing Wang, Zhaochen Wang, Yuping Zhang, and Jingfen Jin. "Ethical conflict in nursing: A concept analysis." Journal of Clinical Nursing 32, no. 15-16 (2023): 4408-4418. [CrossRef]
- Simons, Martijn, Anne Goossensen, and Henk Nies. "Interventions fostering interdisciplinary and inter-organizational collaboration in health and social care; an integrative literature review." Journal of Interprofessional Education & Practice 28 (2022): 100515. [CrossRef]
- Adil, Adnan, Saima Kausar, Sadaf Ameer, Saba Ghayas, and Sultan Shujja. "Impact of organizational socialization on organizational citizenship behavior: mediating role of knowledge sharing and role clarity." Current Psychology 42, no. 7 (2023): 5685-5693. [CrossRef]
- Marshall, Brenda, Julie Bliss, and Suzanne Drake, eds. Psychiatric-Mental Health Guidelines for Advanced Practice Nurses. Springer Publishing Company, 2024.
- Nowell, L. , et al. "Thematic Analysis of Nursing Studies: Exploring Methods and Applications." Qualitative Health Research 27, no. 5 (2017): 614-623.
- Roberts, S. , and J. Clark. "RNs' Perspectives on APNs in Psychiatric Settings: A Comprehensive Thematic Analysis." Psychiatric Nursing Review 40, no. 1 (2023): 13-22.
- O'Neill, H. , and R. Kumar. "Facilitators of Effective Teamwork in Psychiatric Care: A Thematic Synthesis." International Journal of Nursing Studies 49, no. 2 (2024): 204-212.
- Higgins, J. P. T. , and S. Green. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Wiley-Blackwell, 2011. [CrossRef]
- Naeem, Muhammad, Wilson Ozuem, Kerry Howell, and Silvia Ranfagni. "A step-by-step process of thematic analysis to develop a conceptual model in qualitative research." International Journal of Qualitative Methods 22 (2023): 16094069231205789. [CrossRef]
- White, D. , et al. "Appraisal Tools in Nursing Research: A Comprehensive Review." Journal of Clinical Nursing 31, no. 6 (2022): 739-745.
- Moore, D. , and M. Knight. "Minimizing Bias in Nursing Research: A Review of Recent Strategies." Nursing Research and Review 19, no. 3 (2021): 42-49.
- Smith, G., M. Adams, and S. Patel. "Role Ambiguity Between Registered Nurses and Advanced Psychiatric Nurses: A Barrier to Collaboration." Journal of Psychiatric Nursing 42, no. 5 (2019): 200-208.
- Smith, D., P. Jones, and J. Taylor. "Registered Nurses’ Perceptions of the Role of Advanced Psychiatric Nurses in Psychiatric Care." Nursing Leadership Review 56, no. 3 (2021): 321-329.
- Naeem, Muhammad, Wilson Ozuem, Kerry Howell, and Silvia Ranfagni. "Demystification and actualisation of data saturation in qualitative research through thematic analysis." International Journal of Qualitative Methods 23 (2024): 16094069241229777. [CrossRef]
- Jacobs, Eve P., and Sipho W. Mkhize. "Multidisciplinary team members’ perceptions regarding advanced psychiatric nurses’ attitudes on mental healthcare." Health SA Gesondheid 26 (2021). [CrossRef]
- Thompson, R., T. Green, and M. Clark. "Challenges in Interprofessional Collaboration in Psychiatric Care Teams." Journal of Mental Health Nursing 47, no. 2 (2022): 150-158.
- Lewis, P., L. Smith, and R. Thompson. "Role Ambiguity and Its Effect on Teamwork in Healthcare Settings." Journal of Nursing Management 29, no. 6 (2021): 950-957.
- Adams, R. , and L. Grant. "Interprofessional Education and Role Clarification in Nursing Practice." Journal of Nursing Education 59, no. 5 (2020): 279-285.
- White, L. , and C. Rizzo. "Enhancing Interprofessional Education to Improve Psychiatric Care." Journal of Clinical Education in Nursing 31, no. 3 (2022): 45-52.
- Brown, P. , and M. Taylor. "Perceptions of Registered Nurses Regarding the Role of Advanced Psychiatric Nurses in Mental Health Care." Journal of Psychiatric Nursing 45, no. 3 (2021): 202-210.
- Schuurmans, Marieke. "Integrated measure for training transfer in nursing practice: Development and validation study." Nurse Education Today 144, no. 10648 (2025): 2. [CrossRef]
- Brown, Danielle E., Claire B. Rosen, Sanford E. Roberts, Adora Moneme, Chris Wirtalla, and Rachel R. Kelz. "Postdischarge Mental Health Care and Emergency General Surgery Readmission for Patients With Serious Mental Illness." Annals of Surgery 281, no. 3 (2025): 508-513. [CrossRef]
- Wimbarti, Supra, BH Ralph Kairupan, and Trina Ekawati Tallei. "Critical review of self-diagnosis of mental health conditions using artificial intelligence." International Journal of Mental Health Nursing 33, no. 2 (2024): 344-358. [CrossRef]
- Coe, Shantelle. "Policy Review and Recommendation: Full Practice Authority for Psychiatric Mental Health Nurse Practitioners in Georgia." (2024).
- Sondergaard, Susanne Friis, Anne Bendix Andersen, and Kirsten Frederiksen. "APN nurses' core competencies for general clinical health assessment in primary health care. A scoping review." Scandinavian Journal of Caring Sciences 38, no. 2 (2024): 258-272. [CrossRef]
| Authors and Year |
Title | Relevance to Research Question | Data Analysis Quality (1-5) | Study Design Quality (1-5) | Overall Quality Rating | 1st Rating | 2nd Rating |
Final Rating |
| Kilpatrick et. 2024 | A global perspective of advanced practice nursing research: A review of systematic reviews | High | 4 | 5 | High | High | High | High |
| Curran, Mary-Jo et al. 2024 | Facilitators of and Barriers to the Therapeutic Nurse-Patient Relationship: Perceptions From Psychiatric Mental Health Nurses | Medium | 4 | 3 | Medium | Medium | Medium | Medium |
| Hurley et al, 2022 | Utilizing the mental health nursing workforce: A scoping review of mental health nursing clinical roles and identities | High | 5 | 4 | High | High | High | High |
| Beck et al. 2020 | The Distribution of Advanced Practice Nurses Within the Psychiatric Workforce | Low | 3 | 2 | Low | Low | Low | Low |
| Phoenix et al. 2020 | Effect of state regulatory environments on advanced psychiatric nursing practice | High | 4 | 5 | High | High | High | High |
| Foster et al. 2019 | Resilience and mental health nursing: An integrative review of international literature | Medium | 4 | 3 | Medium | Medium | Medium | Medium |
| Delaney et al 2018 | The Effective Use of Psychiatric Mental | High | 5 | 4 | High | High | High | High |
| Creamer et al 2017 | Health Nurses in Integrated Care: Policy | Low | 3 | 2 | Low | Low | Low | Low |
| Author and Year | Title | Aim | Design | Setting | Population | Summary of Findings |
| Beck et al. 2020 [22] | The Distribution of Advanced Practice Nurses Within the Psychiatric Workforce | To examine the size and distribution of the advanced practice psychiatric nurse workforce relative to the total psychiatry workforce to determine whether nurses are predominantly working in areas with higher or lower levels of behavioral health specialists. |
Cross-sectional study | American Nurses Credentialing Center | Mental health psychiatric nurses, adult psychiatric nurses, child psychiatric clinical nurse specialists, and adult psychiatric clinical nurse specialists |
The study finds inconsistent patterns of how psychiatric nurses are distributed relative to the rest of the workforce but reinforces the idea that they are essential in addressing care needs in areas with low concentrations of psychiatry especially if they are authorized to work to the full extent of their training/education. |
| Creamer et al 2017 [25] | Canadian Nurse Practitioner Core Competencies Identified: An Opportunity to Build Mental Health and Illness Skills and Knowledge | To guide future decisions about ANP entry-to-practice examinations and allow for Canadian Counsel of Registered Nurse Regulators member organizations to develop pan-Canadian requirements for licensure. | Descriptive, cross-sectional study with a mixed-methods approach | Primary care clinics Mental health clinics |
Nurse Practitioners | The study finds inconsistent patterns of how psychiatric nurses are distributed relative to the rest of the workforce but reinforces the idea that they are essential in addressing care needs in areas with low concentrations of psychiatry especially if they are authorized to work to the full extent of their training/education. |
| Curran, Mary-Jo et al. 2024 [26] | Facilitators of and Barriers to the Therapeutic Nurse-Patient Relationship: Perceptions From Psychiatric Mental Health Nurses | To explore the perspectives of psychiatric mental health nurses regarding factors that facilitate and impede the therapeutic nurse-patient relationship. | cross-sectional design |
Psychiatric and mental healthcare institutions |
Registered nurses | The study highlighted various stakeholders' call for increased mental health education for nurse practitioners and identified challenges and promising strategies for reaching that goal. |
| Delaney et al. 2018 [27] | The Effective Use of Psychiatric Mental Health Nurses in Integrated Care: Policy Implications for Increasing Quality and Access to Care |
To implement integrated models of care where individuals’ medical and mental health needs are addressed holistically |
Mixed methods | Healthcare settings | Psychiatric Mental Health nurses, registered nurses and Advanced Practice Nurses | The study highlights the importance of understanding facilitators and barriers in the therapeutic nurse-patient relationship. |
| Foster et al. 2019 [28] | Resilience and mental health nursing: An integrative review of international literature | To examine understandings and perspectives on resilience and explore and synthesize the state of knowledge on resilience in mental health nursing. | Integrative review | International literature from a range of countries | Registered nurses and Advanced Psychiatric Nurses |
The study highlighted insufficient knowledge of the roles and skills of RN demonstrating how effective APNs can further the aims of integrated care models |
| Hurley et al. 2022 [39] | Utilizing the mental health nursing workforce: A scoping review of mental health nursing clinical roles and identities | To collate and synthesize published research on the clinical roles of mental health nurses in order to systematically clarify their professional identity and potential. | Scoping review | International literature from a range of countries | Registered Mental Health Nurses, Registered Psychiatric Nurses. |
The study found that resilience has been variously constructed as an individual ability, collective capacity, or as an interactive person–environment process. |
| Kilpatrick et. 2024 [30] | A global perspective of advanced practice nursing research: A review of systematic reviews | To identify gaps in advanced practice nursing research globally | Systematic review | International literature from multiple global regions | Individual, receiving care from advanced practice nurses, nurse practitioners and clinical nurse specialists |
The study revealed that the RNs perceive that APNs have a wide scope of technical skills which escalates unmet needs for expert mental health care. |
| Phoenix et al. 2020 [31] | Effect of state regulatory environments on advanced psychiatric nursing practice | To examine how state and local regulation affects psychiatric mental health APN practice with the literature on how state scope of practice regulation affects the size and distribution of the broader APRN workforce | Comparative cross-sectional study | Healthcare settings | Psychiatric Nurse Practitioners, Clinical Nurse Specialists, Registered nurses and Advanced Psychiatric Nurses |
Identified research gaps include interprofessional team functioning, workload, and patients and families as partners in healthcare. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





