1. Introduction
Rectus diastasis (RD) was first classified by Rath et al. in 1996, however, available literature is still scarce.18. The soaring discussion on the topic reached international societies, and in 2021, the European Hernia Society (EHS) established a classification method based on the width of the rectus muscles, considering muscle separation, post-pregnancy state, and presence of concomitant hernia. Altered body image is the most common and relevant symptom, it is still unclear if the widening of the linea alba can negatively influence ventral hernia repairs. Most published studies associate widening of the linea alba with parity, with a positive correlation observed in prospective studies, especially up to 12 months postpartum 1-3,19,27.
In the late 1980s, mini-abdominoplasty was described as a way to treat RD and flaccidity, aiming to correct lower abdominal wall deformities 16,17. Recently, advances in minimally invasive abdominal wall reconstruction techniques have also allowed cranial deformities to be treated using SCOLA (Subcutaneous Onlay Laparoscopic Approach) and MILA (Minimally Invasive Lipoabdominoplasty Approach), which include liposuction and skin retraction devices associated with RD plication 4-6, 14,15,20-24. Given these advances, doubts arise about their effectiveness in addressing parity-related skin laxity 20.
New evidence and studies about RD and how to apply it at the general and specific levels make room for targeted treatment. Rather than a standardized treatment, a patient-fitted approach can increase the cost-effectiveness of this process, reduce superfluous procedures, and achieve a better health-related quality of life for our patients 25.
Our goal is to offer another surgical option for patients with rectus diastasis, with or without abdominal wall hernias, through a minimally invasive endoscopic correction approach, presenting a new method for abdominal contouring via minimally invasive mini-abdominoplasty (MAMI).
2. IDEAS
A widening greater than 2 cm of the linea alba is generally indicated for surgical correction, according to EHS 2. Newer approaches, such as MILA and SCOLA, are indicated for patients with a BMI up to 28, based on height and weight only. However, this criterion may be insufficient for some patient profiles. Despite advancements in skin retraction, there is still no evidence on how devices affect postoperative results when added to these techniques, since results depend on multiple factors such as age, skin firmness, number of passes, applied energy, etc. Therefore, even patients with a BMI up to 28 may present significant supra and infraumbilical flaccidity and poor skin quality (thin, flaccid, with stretch marks), making SCOLA or MILA surgery alone unsuitable due to possible skin redundancy. Likewise, even patients with a high-positioned umbilicus, moderate flaccidity, and rectus diastasis, who in the past would have been strictly indicated for abdominoplasty, may benefit from mini-abdominoplasty with a minimally invasive approach (MAMI). 5, 8, 10, 14,15,22-24.
The increasing appreciation for minimally invasive surgeries prompts us to bring another option for RD treatment, involving skin retraction technologies and optional skin removal. This opens a new range of candidates who would not benefit from SCOLA or MILA alone, as well as those who previously only had abdominoplasty as an option 7, 8.
To better assess the ideal treatment for each patient, metrics beyond BMI should be considered. BMI alone cannot predict skin laxity or body composition. In non-obese patients, bioimpedance, with or without the clinical pinch test and fat mass index, may provide more information to define the surgical approach
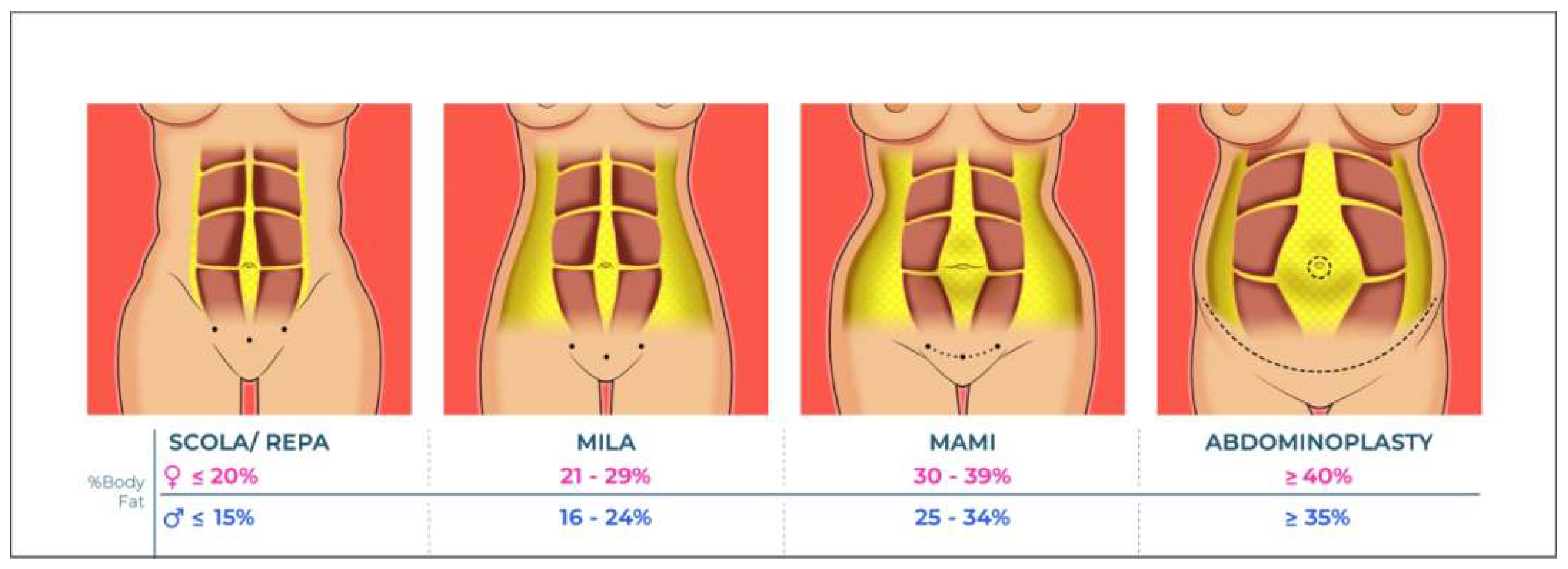
12. We propose, for this reason, adding to the pre-operative BMI assessment evaluation of body fat percentage (
Figure 1), taking into account that this technique should not renounce optimization with physical therapy, and weight loss stimulation before surgery.
MAMI Approach Steps:
Superwet infiltration with 1000 ml 0.9% saline + adrenaline 1:500,000 + 1 vial tranexamic acid — infiltrating 2 to 3 liters across the entire abdominal region. Wait 20 minutes for vasoconstriction and followed by 70% ultrasonic liposuction (Safer).
Total Definer liposuction with vibroliposuction device (Vibrofit), prioritizing negative zones along semilunar lines and linea alba at 0.5 cm thickness and positive zones at 1.5 cm, paying attention to the inferior flap near the scar and superior regions (deep liposuction with less intensity) using a 4.0 curved Mercedes-type cannula. The RD will be repaired with a minimally invasive approach, with supraponeurotic repair of midline hernias and rectus abdominis plication, assisted or not with the robotic platform. We recommend a midline suprapubic optical trocar and a minimal distance of 5 cm at the same height for the other 0.5 cm trocars. Initially, the subcutaneous layer will be accessed with blunt dissection, and after the endoscopic access is prompt, the dissection of the anterior rectus sheet must be performed bilaterally with a narrow dissection along the midline and up to the xiphoid appendix. At this moment, a careful dissection is made around the umbilical scar and the costal margins, avoiding vascular impairment of the perforator arteries in those areas. The dissected space can also make room for mesh and/or drain placement if the surgeon feels that it is best suited. The RD plication is followed by the use of argon plasma skin retraction technology at 30 W with 1.6 gas, 5 passes per region (5 minutes), mainly in the lateral regions of the dissection. It is crucial to excise the cesarean scar or skin excision or a smaller suprapubic excision in women with vaginal delivery or nulliparous aiming to avoid the sagging postoperative aspect.
3. Results
The main objective of this study is to provide another surgical option for RD patients and discuss the possible inadequacy of endoscopic correction indications based on typical clinical presentations used so far. Hubner et al. published in 2024 a series that studied the linea alba in fresh corpses, showing that the widening of the ligament is not associated with its thickness.26 High-quality evidence is still needed to associate RD with morbidity (as there is also no true abdominal wall defect that may cause incarceration, and its association with recurrence is still obscure) 27. However, RD is still a frequent postpartum complaint in clinical care. Up to one-third of patients may develop linea alba widening. Due to limited evidence to support the non-operative treatment and no standardized physiotherapy regimen, surgery is still frequently indicated in clinical practice 2, 7.
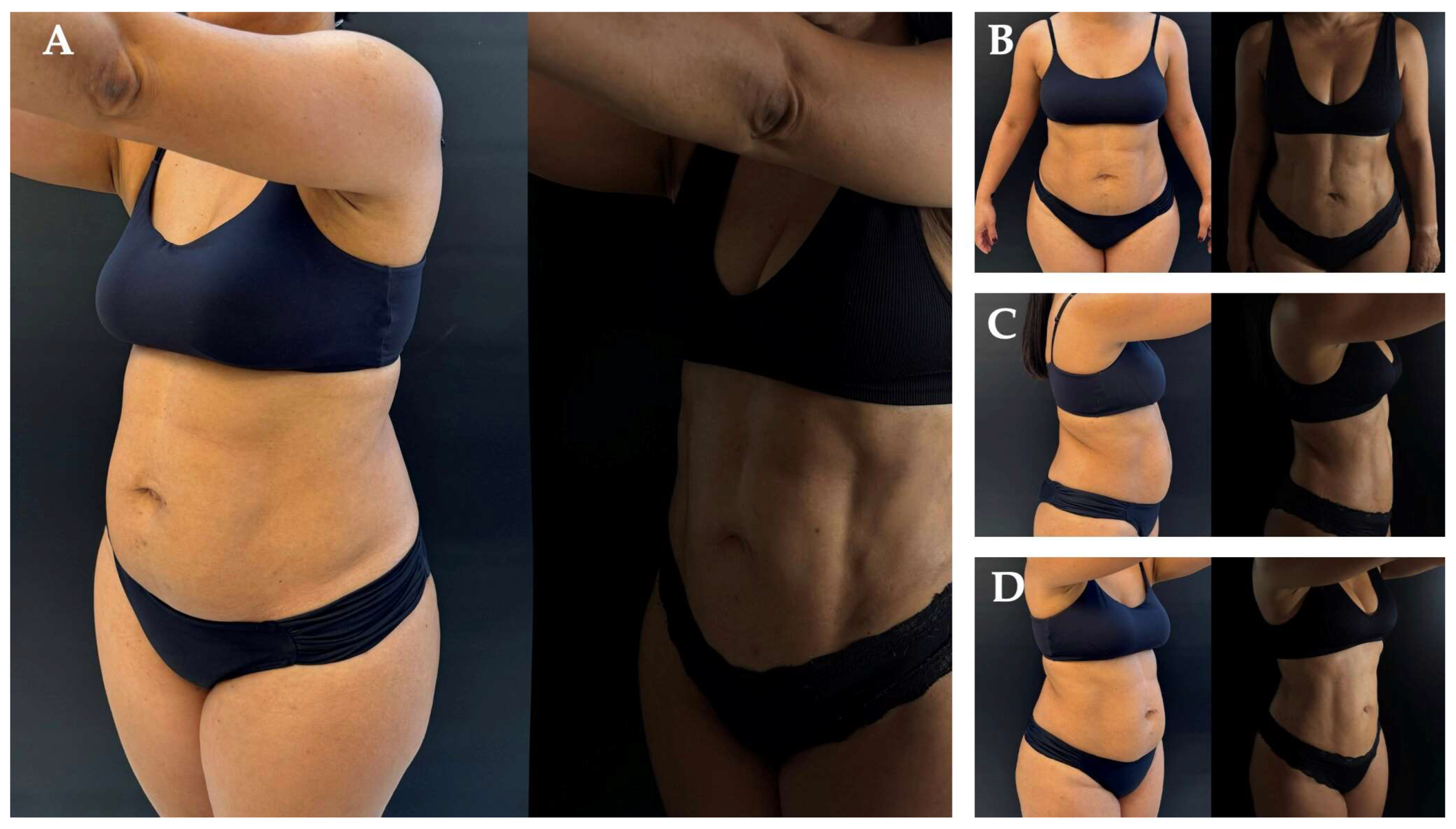
Various techniques have been described, with increasing general surgery involvement providing relevant contributions, as minimally invasive approaches may be used for RD assessment
8, 10, 14,15. Liposuction can enhance aesthetic outcomes in patients with RD without skin laxity. Although MILA can be performed with liposuction and skin retraction energy, patients with poor skin quality, higher body fat percentage and moderate flaccidity may need more aggressive measures to achieve the same aesthetic outcomes
8, 10, 14,15,22-24. (
Figure 1)
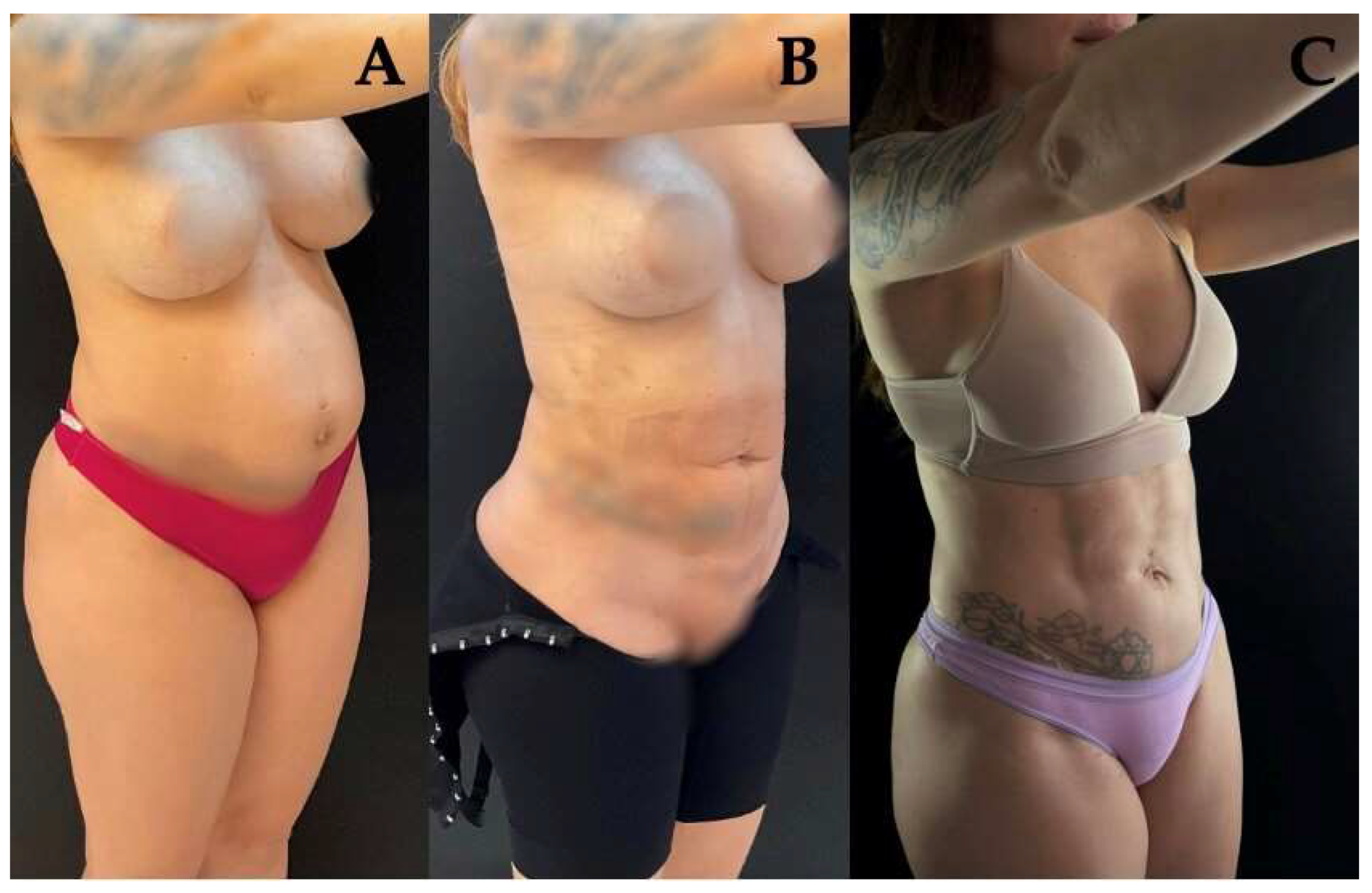
Additionally, patients diagnosed with RD and no previous signs of skin laxity may develop it after MILA or SCOLA correction, due to the low compliance of midline skin after rectus sheath suturing, resulting in slackness of the undermined skin, as described by Sahoo and collaborators
7, 14,15, 28. (
Figure 2)
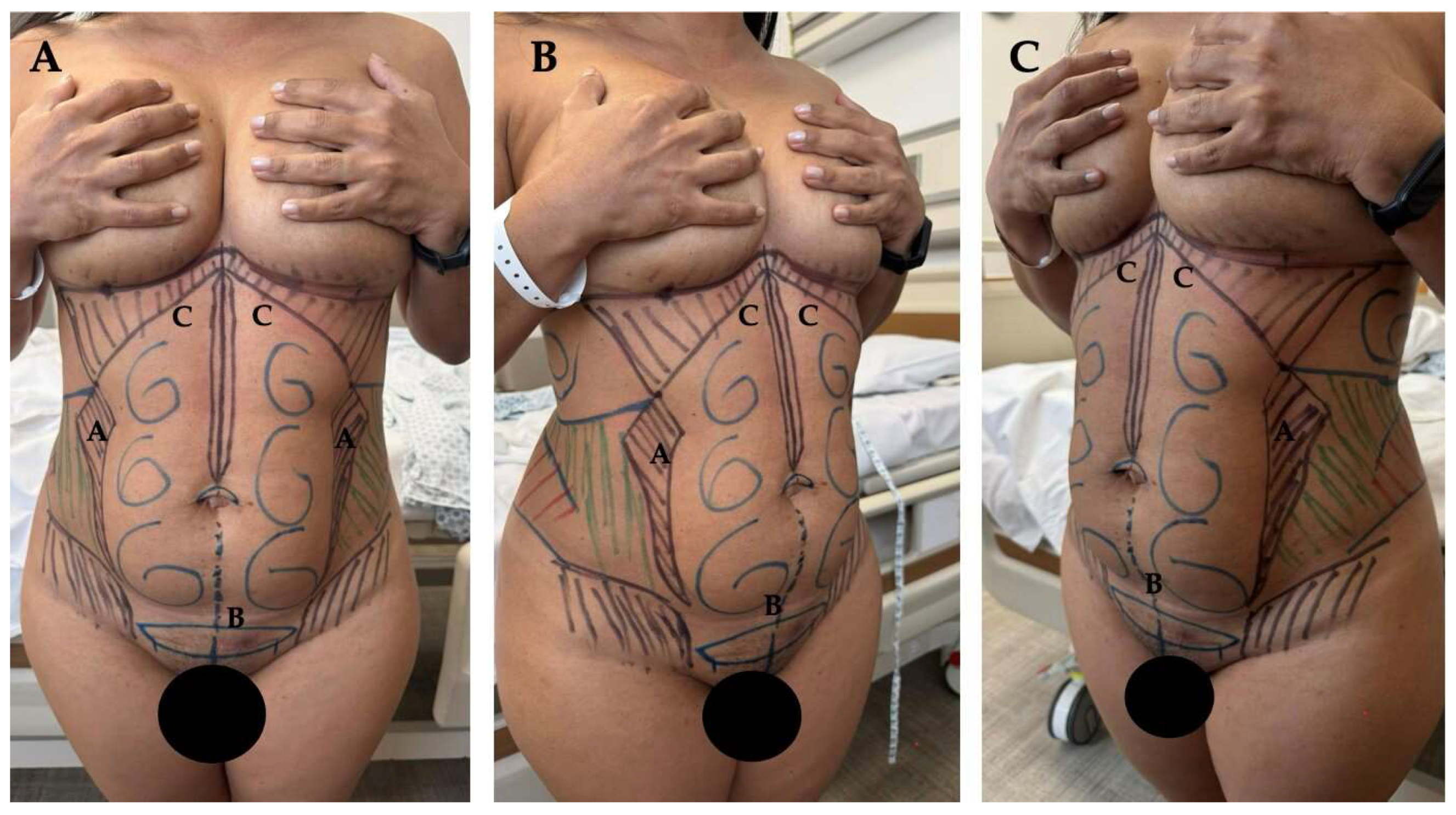
Meanwhile, mini-abdominoplasty remains indicated for such patients, especially those desiring smaller scars. Even with advances in skin retraction gadgets, more clarity is still needed on the long-term performance of these devices. In this context, wedge excision serves as an ally in surgery, becoming a complement to improve results and encompass a larger number of candidate patients
4, 5, 9, 10. (
Figure 3) (
Figure 4)
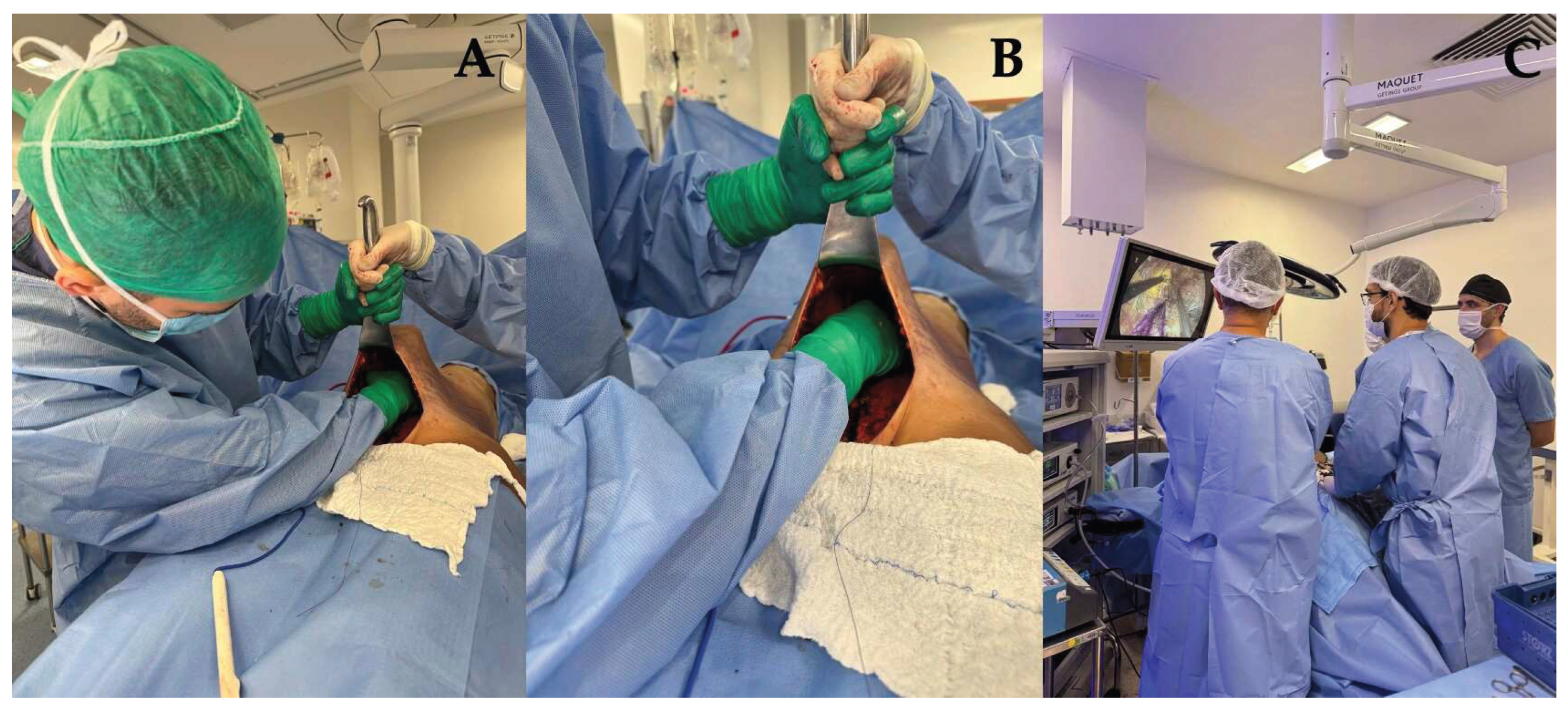
For surgeons, traditional mini-abdominoplasty is not ergonomic, as the inferior access does not allow full visualization of the abdominal wall. The surgeon has a small space to operate, requires special retractors, limited lighting, and assumes a very uncomfortable position. It also causes more trauma and risks to the abdominal flap and may even prevent the correction of epigastric hernias that could go missing. Subcutaneous dissection and RD correction through a small incision require uncomfortable positioning and excessive skin traction, potentially compromising the lower flap and increasing the risk of ischemia and skin necrosis 13.
In contrast, the minimally invasive MAMI approach eliminates the need to open the subcutaneous layer to access the abdominal wall, preserving the lower flap’s vascularization and making the procedure safer. Unlike traditional mini-abdominoplasty — which requires larger scars, full wall access, excessive flap traction, and greater subcutaneous exposure (linked to higher surgical site infection rates, as seen in ventral hernia repairs) — MAMI avoids these risks once the endoscopic camera provide an enhanced view of the subcutaneous layer within a closed antiseptic space. (
Figure 5)
The proposed technique — performed with the surgeon and assistant in upright positions — uses CO₂ insufflation to expand the subcutaneous tissue, eliminating the need for skin traction and enlarging the surgical field. After RD correction, the procedure allows umbilical scar fixation without needing neoumbilicoplasty and thus avoids stigmatizing umbilical scars (
Figure 3)
Figure 6.
Comparative surgeon, assistant positioning and exposure throughout surgery during Mini Abdominoplasty and Mini Abdominoplasty Mini Invasive (MAMI).
Figure 6.
Comparative surgeon, assistant positioning and exposure throughout surgery during Mini Abdominoplasty and Mini Abdominoplasty Mini Invasive (MAMI).
Based on our experience, mini-abdominoplasty with a minimally invasive approach (MAMI) has the potential to increase the number of eligible patients for minimally invasive surgery, improve access to RD correction, reduce complications, accelerate recovery compared to abdominoplasty, and provide smaller scars with no umbilical scarring and lower risk of skin dehiscence and other surgical site occurrences due to smaller incisions and less exposure of the anterior abdominal wall.
Therefore, conventional assessment based solely on BMI may not be the most suitable criterion for MILA correction indication, as observed in the literature. Similarly, not all patients with moderate flaccidity and diastasis are clear candidates for abdominoplasty.
However, this proposal of a novel approach for liposuction, minimally invasive RD plication followed by skin retraction technology and wedge skin excision, has not yet been compared to other surgical techniques in a prospective fashion study. These results are based solely on a single center, high-volume experience. The propagation of this study can make room for future research and collaborations that could substantiate a wider range of evidence for MAMI, reporting patients’ outcomes with validated questionnaires that include cosmetic outcomes, quality-of-life, and work impairment, as well as skin laxity and abdominal wall bulging after RD plication.
4. Conclusions
MAMI surgery has proven to be a safe and reproducible approach for selected women wishing to restore feminine body features after pregnancy and achieve quick recovery.
It encompasses a larger number of patients, as it is easily reproducible in patients who are candidates for MILA surgery but also require skin excision, as well as those who would be typically indicated for abdominoplasty but present a high umbilicus and moderate flaccidity with diastasis. It offers satisfactory aesthetic results due to the minimized scar, preservation of the natural umbilical scar, and improved surgical correction of rectus diastasis through better visualization.
It reduces the risks associated with traditional mini-abdominoplasty, such as abdominal flap ischemia and prolonged subcutaneous tissue exposure, and improves visualization during subcutaneous dissection and treatment of RD and associated hernias.
Author Contributions
Conceptualization, R.F.G, T.M. and A.C.C.; methodology, R.F.G, A.C.C, and R.N.; investigation, R.F.G, T.M., A.C.C., and R.N.; data curation, R.F.G., M.F.C.; writing—original draft preparation, R.F.G, A.C.C.; writing—review and editing, R.F.G., M.F.C., T.M. and R.N.; visualization, R.F.G; supervision, R.F.G, T.M, A.C.C, and M.F.C; All authors have read and agreed to the published version of the manuscript.
Funding
The authors have no sources of funding to declare for this manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived for this study due to the data used in this technical note are completely de-identified, so there is no risk to individual privacy.
Informed Consent Statement
Patient consent was waived due to the data used in this technical note are completely de-identified, so there is no risk to individual privacy.
Data Availability Statement
Data sharing is not applicable (only appropriate if no new data is generated or the article describes entirely theoretical research).
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016 Sep;50(17):1092-6. [CrossRef] [PubMed] [PubMed Central]
- Hernández-Granados P, Henriksen NA, Berrevoet F, Cuccurullo D, López-Cano M, Nienhuijs S, Ross D, Montgomery A. European Hernia Society guidelines on management of rectus diastasis. Br J Surg. 2021 Oct 23;108(10):1189-1191. [CrossRef] [PubMed] [PubMed Central]
- Turan V, Colluoglu C, Turkyilmaz E, Korucuoglu U. Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekol Pol. 2011 Nov;82(11):817-21. [PubMed]
- Wilkinson TS. Mini-abdominoplasty. Plast Reconstr Surg. 1988 Nov;82(5):917-8. [CrossRef] [PubMed]
- Greminger RF. The mini-abdominoplasty. Plast Reconstr Surg. 1987 Mar;79(3):356-65. [CrossRef] [PubMed]
- di Diego JM. Endoscopic Lipoabdominoplasty. Plast Reconstr Surg Glob Open. 2021 Jan 26;9(1):e3346. [CrossRef] [PubMed] [PubMed Central]
- Claus CMP, Malcher F, Cavazzola LT, Furtado M, Morrell A, Azevedo M, Meirelles LG, Santos H, Garcia R. SUBCUTANEOUS ONLAY LAPAROSCOPIC APPROACH (SCOLA) FOR VENTRAL HERNIA AND RECTUS ABDOMINIS DIASTASIS REPAIR: TECHNICAL DESCRIPTION AND INITIAL RESULTS. Arq Bras Cir Dig. 2018 Dec 6;31(4):e1399. [PubMed] [PubMed Central]
- di Diego JM. Endoscopic Lipoabdominoplasty. Plast Reconstr Surg Glob Open. 2021 Jan 26;9(1):e3346. [CrossRef] [PubMed] [PubMed Central]
- Malone, C.H., Walters, N., Stroh, R. et al. New Technologies in Skin Tightening. Curr Otorhinolaryngol Rep 9, 422–435 (2021). [CrossRef]
- Bank, David E. MD1,2; Perez, Maritza I. MD1,3. Skin Retraction After Liposuction in Patients Over the Age of 40. Dermatologic Surgery 25(9):p 673-676, September 1999. |. [CrossRef]
- Bozola AR. Abdominoplasty: same classification and a new treatment concept 20 years later. Aesthetic Plast Surg. 2010 Apr;34(2):181-92. [CrossRef] [PubMed]
- Peltz G, Aguirre MT, Sanderson M, Fadden MK. The role of fat mass index in determining obesity. Am J Hum Biol. 2010 Sep-Oct;22(5):639-47. [CrossRef] [PubMed] [PubMed Central]
- Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z. Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg. 2014 Sep;38(9):2233-40. [CrossRef] [PubMed]
- Claus CMP, DI-Biasio GA, Ribeiro RD, Correa MAMF, Pagnoncelli B, Palmisano E. Minimally invasive lipoabdominoplasty (MILA) tactic. Rev Col Bras Cir. 2024 Jun 14;51:e20243692. English, Portuguese. [CrossRef] [PubMed]
- Malcher F, Lima DL, Lima RNCL, Cavazzola LT, Claus C, Dong CT, Sreeramoju P. Endoscopic onlay repair for ventral hernia and rectus abdominis diastasis repair: Why so many different names for the same procedure? A qualitative systematic review. Surg Endosc. 2021 Oct;35(10):5414-5421. [CrossRef] [PubMed]
- Faria-Correa MA. Abdominoplasty: the South America style. In Ramirez OM,Daniel RK,eds. Endoscopic Plastic Surgery. New York: Springer-Verlag,1995.
- Faria-Correa MA. Abdominoplastia videoendoscopica (subcutaneoscopica). In Atualizacao em Cirurgia Plastica Estetica e Reconstrutiva. Sao Paulo: Robe Editorial,1994.
- Akram J, Matzen SH. Rectus abdominis diastasis. J Plast Surg Hand Surg. 2014 Jun;48(3):163-9. [CrossRef] [PubMed]
- Lelli G, Iossa A, DE Angelis F, Micalizzi A, Fassari A, Soliani G, Cavallaro G. Mini-invasive surgery for diastasis recti: an overview on different approaches. Minerva Surg. 2025 Feb;80(1):60-75. [CrossRef] [PubMed]
- Corrêa MA. Videoendoscopic subcutaneous techniques for aesthetic and reconstructive plastic surgery. Plast Reconstr Surg. 1995 Aug;96(2):446-53. [CrossRef] [PubMed]
- Palmisano EM, Di Biasio G. Alternativa de manejo miniinvasivo para el tratamiento de pacientes con diástasis abdominal y colgajo dermograso mediante la táctica VER: Vaser® + endoscopia + Renuvion®. REVISTA ARGENTINA DE CIRUGÍA PLÁSTICA 2022;28(1):20-24. [CrossRef]
- Faria-Correa MA. Robotic Procedure for Plication of the Muscle Aponeurotic Abdominal Wall. In New Concepts on Abdominoplasty and Further Applications. 11:161-177 Springer 2016.
- Faria-Correa MA. M.I.LA Minimally Invasive Robotic and Endoscopic Lipo-Abdominoplasty. In: Body Contouring: Current Concepts and Best Practices. 11:189-212, Springer; 20.
- Faria-Correa MA, Videoendoscopy in plastic surgery: brief communication. Rev Soc Bras Cir Plast Est Reconst 7:80-82,1992.
- López Cano M. Editorial: Rectus Diastasis. J Abdom Wall Surg. 2025 Mar 24;4:14296. [CrossRef] [PubMed] [PubMed Central]
- Hubner PNV, Alberti LR, Carvalho AC, Soares VC, Neto CS, Garcia DPC. Morphometric evaluation of the linea alba in fresh corpses. JPRAS Open. 2024 Mar 26;40:238-244. [CrossRef] [PubMed] [PubMed Central]
- Mommers EHH, Ponten JEH, Al Omar AK, de Vries Reilingh TS, Bouvy ND, Nienhuijs SW. The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. 2017 Dec;31(12):4934-4949. [CrossRef] [PubMed] [PubMed Central]
- Kumar AT, Sahoo MR. Laparoscopic plication and mesh repair for diastasis recti: a case series. Int J Case Rep Images. 2014;5(9):610. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).