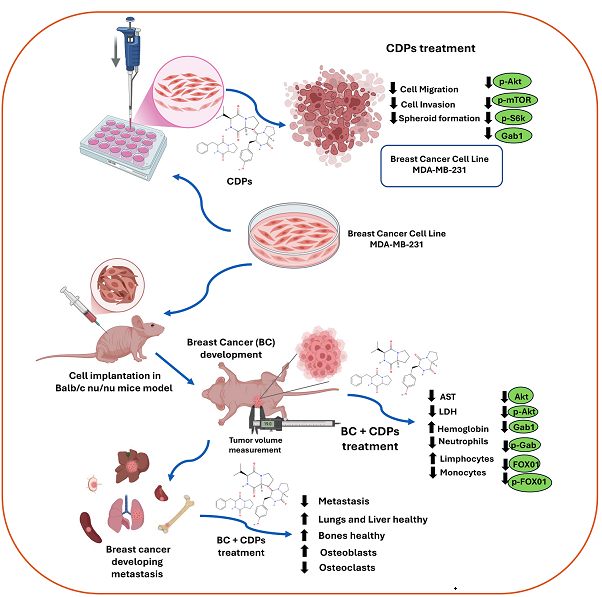
1. Introduction
Breast cancer is the principal cause of death in women worldwide; it is a clinically heterogeneous disease and around 10-15% of patients present aggressive phenotypes and develop metastasis [
1]. Triple-negative breast cancer comprises a group of diseases with different histological, genomic, and immunological profiles, characterized by lacking hormonal estrogen and progesterone receptors, as well as HER2 receptors. According to postulate in the “soil and seed” theory, tumor cells thrive in those tissues with genetic and metabolic characteristics similar to their needs. For example, breast cancer cells tend to metastasize the bone, lung, and liver [
https://www.cancer.gov]. Other factors in developing breast cancer, such as obesity, represent a poor prognosis for patients since the interaction of adipocytes with tumor cells provides an optimal microenvironment that favors proliferation, invasion, metastasis, or resistance to cell death[
2]. The tumor microenvironment also recruits the malignant cells with other types of cells, such as adipocytes, mesenchymal-type cells such as fibroblasts, and the cells of the immune system, such as macrophages, T-lymphocytes, and neutrophils. These interactions are mediated by secretion of chemokines, interleukins, or growth factors, which promote proliferation, invasion, and resistance to cell death, positioning these components as possible new therapeutic strategies[
3].
Among the first-line therapeutic options for treating metastatic breast cancer are taxanes, anthracyclines, methotrexate, carboplatin, PD-1 or PD-L1 inhibitors, PARP inhibitors, and their combination with immunotherapy, radiotherapy, and surgery[
4]. However, a significant percentage of patients negatively respond to these treatments, resulting in low survival and poor quality of life. Therefore, the search for new therapeutic options that improve the prognosis for patients with metastatic breast cancer is of great importance.
Bone metastasis is a common complication in advanced-stage breast and prostate cancer, disrupting the bone remodeling cycle mediated by osteoblasts and osteoclasts[
5]. Currently, available T cell-based immunotherapies promise in cancer treatment; however, potential benefits for patients with bone metastases remain unclear[
6]. Metastases predominantly occur in trabecular and red marrow-rich bones, suggesting that specific bone environments favor metastatic growth[
7]. Other common metastatic sites include the lungs and brain. Once bone metastases develop, the five-year survival rate drops to approximately 20%[
8]. Bone metastases significantly impact patient health, yet current treatments—including bisphosphonates and antiresorptive antibodies remain insufficient; therefore, develop of novel therapies that target both tumor cells and the bone microenvironment with dual antiresorptive (reducing bone remodeling) and anticancer properties are required[
9].
Cyclodipeptides are a class of molecules synthesized by a broad type of organisms, which possess enjoyable biological activities such as cytotoxic effects in different cancer cell lines[
10,
11,
12]. Previously, we described that CDPs produced by the
Pseudomonas aeruginosa PAO1 bacterium induce apoptosis in cervical, colon, leukemia, and melanoma cancer cells by inhibiting phosphorylation of multiple kinases from the PI3K/Akt/mTOR pathway, including mTORC1/C2 complexes[
11]. Furthermore, in a mouse murine melanoma model, a significant decrease of tumors in mice treated with CDPs at 0.1 mg/g of weight was found. Additionally, treatment with CDPs led to restoration of hematological parameters and decrease in tissue damage markers AST and ALT, as well as a marked decrease in the expression of proteins mediating pathways involved in energy metabolism, lipid synthesis, epithelial-mesenchymal transition, invasion, and metastasis[
13]. Interestingly, transcriptomic analysis in HeLa cells found that CDPs inhibit gene expression in the mevalonate pathway and lipid synthesis[
14]. Given this background, we sought to determine whether CDPs could have a promising effect on breast cancer and whether this effect could be observed in advanced stages of tumorigenesis[
15].
In this work, we first used monolayer culture to evaluate the migratory and invasive potential of MDA-MB-231 and MCF-7 human breast cancer cell lines treated with CDPs and combined with Methotrexate. Further, the effect of the CDPs on advanced-stage mammary tumors developed and their ability to prevent the appearance of metastatic foci through the implantation of the MDA-MB-231 cells in the mammary tissue of mice model was evaluated.
2. Materials and Methods
2.1. Chemicals, Reagents, and Cell Culture
Chemicals and reagents included are Dulbecco’s modified Eagle’s medium (DMEM; Sigma-Aldrich), fetal bovine serum (FBS; Gibco Life Technology), and trypsin solution (Sigma Life Science). Cyclodipeptides were isolated from
P. aeruginosa PAO1 cells-free supernatant[
16]. CDPs were dissolved in a DMSO-water ratio of 1:3 to prepare stock solutions (100 mg/mL). The MCF-7 is a human metastatic breast cancer cell line (adenocarcinoma) dependent on estrogen, progesterone, and glucocorticoid receptors (ATCC, Manassas, VA, USA)[
17]. The MDA-MB-231 cell line was obtained from invasive ductal carcinoma (ATCC, Manassas, VA, USA). This cell line is estrogen receptor (ER), progesterone receptor (PR), and E-cadherin negative, p53 mutated, lacking the growth factor receptor HER2, commonly used as a study model of triple-negative breast cancer[
18]. MDA-MB-231 cells, when implanted in xenografts, spontaneously metastasize to lymph nodes. MDA-MB-231 and MCF-7 cell lines were cultured in complete media [DMEM supplemented with 10% (v/v) FBS, 100 units/mL of penicillin, 40 µg/mL of streptomycin, and 1 µg/mL of amphotericin B (Sigma-Aldrich Co.), supplemented with 1.6 g/L of glucose. Cell culture media were changed twice a week, incubating at 37 °C under 80% humidity and an atmosphere of 5% CO
2 to confluency. Cells were then trypsin-treated, counted using a hemocytometer chamber, and used for subsequent assays. Cell cultures and other procedures were performed in class II biological safety cabinets.
2.2. Wound Closure Migration Assay
MDA-MB-231 and MCF-7 cell lines were grown in a 95% confluent monolayer, and three wounds were made per plate with a sterile pipette tip in assays by triplicate. Plates were washed with PBS twice, and fresh complete medium was placed; the CDPs, MTX, and combined treatments were placed for 48 h, and photographs were taken every 24 h to subsequently quantify the wound area using the ImageJ software (NIH).
2.3. Invasion Assay
MDA-MB-231 or MCF-7 cell lines were cultured in a transwell chamber previously coated with Matrigel (Corning, Life Sciences) with complete DMEM medium. Co-culture was carried out using Raw 264.7 macrophages seeded in the lower chamber with complete DMEM medium and treatments with CDPs or MTX at 0.01 and 0.005 mg/mL concentrations, respectively.
2.4. Multicellular Microspheroids
MDA-MB-231 or MCF-7 cell lines were cultured (2 x105 cells) under non-stick conditions (0.6% agarose) in complete DMEM medium for 14 days with periodic medium changes until the spheroids reached a size of 40-50 µm. Once, treatment with CDPs (0.1 mg/mL), CDPs+cd (0.1 mg/mL), or CDPs-MTX containing (0.1 mg/mL CDPs, 0.05 mg/mL MTX) was applied. Photographs were taken at 72 h of treatment, and a cell viability test was performed on the remaining cells using an MTT reduction assay. MTT, 50 mg/mL in PBS, was added to each well and incubated for 4 h at 37°C. Finally, 100 µL of 2-propanol/1M HCl (19:1, v/v) was added to dissolve the formazan crystals, and the absorbance was measured at 595 nm using a microplate reader (BioTek Instruments).
2.5. Western Blot
Confluent MCF-7 and MDA-MB-231 cells treated with 0.1 mg/ml of CDPs incubated for 15 min, 1 h, and 4 h were harvested after trypsin treatment and washed twice with PBS, subsequently centrifuged at 5000 × g at 4 °C for 10 min and resuspended in RIPA lysis buffer. The cell suspension or tumor tissue were lysed by three cycles of sonication at low intensity (20 kHz, 5 W) for 30 s each at 4 °C (Hielscher-LS24 Ultrasound Technol). The protein extract free of cellular debris was obtained by centrifugation at 7500 × g for 15 min, and the protein concentration was determined by the Bradford method (BioRad). Protein extract were separated on 10% (SDS-PAGE) polyacrylamide gels and transferred to PVDF membranes (Millipore, Billerica, MA, USA) in a BioRad transfer chamber at 15 volts for 45 min. Briefly, PVDF membranes were incubated with TBS-T (Tris-HCL 10 mM; NaCl 0.9%; tween-20 0.1%, dry milk 5%, pH 7.8). They were washed three times with TBS-T for 6 min each and incubated with primary antibodies dissolved in TBS-T at the concentration suggested by the manufacturer. Antibodies were used: anti-AKT, anti-p-AKT (Ser 473), anti-mTOR, anti-p-mTOR, anti-S6K, anti-p-S6K, anti-Vimentin; anti-Gab1, anti-FOX01, anti-p-FOX01, and anti-b-actin (Santa Cruz Biotechnology, Santa Cruz, CA, USA and Cell Signaling Technology, MA, USA). All primary antibodies were incubated for 12 h at 4°C and subsequently three washes by 6 min with TBS-T were performed and then incubated with anti-mouse secondary HRP-conjugated antibody (BioRad, CA, USA) at a concentration of 1:10,000 in TBS-T for 2 h; membranes were washed as above and developed with Supersignal West Pico Luminol (Pierce; Thermo Fisher Scientific, Waltham, MA, USA). Then, images were captured using a ChemiDoc™ MP System (Bio-Rad). Assays were conducted at least three times, and representative images are shown. The Image J software (NIH) was used to quantify image band intensities.
2.6. Orthotopic Model of Metastatic Breast Cancer
Immunosuppressed Balb/c nu/nu female mice aged 8 weeks were adapted for 15 days in a pathogen-free environment with a standard diet and drinking water ad libitum. The cages, water, food, and bedding were autoclaved. Animal manipulation was authorized by the Institutional Animal and Use Committee (IACUC) from the Universidad Michoacana de San Nicolás de Hidalgo (IIIQB-UMSNH-IACUC-2022-35). Experiments complied with standard guidelines for the welfare of animals following the Institutional Committee and recommendations of the Mexican Official Regulations for the Use and Care of Animals (NOM 062-ZOO-1999; Ministry of Agriculture, Mexico). Animal handling, feeding, and care were done by trained personnel under the NIH guide for the care and use of laboratory animals.
Once the adaptation period had concluded with 100% survival of the mice, 1 x105 MDA-MB-231 metastatic breast cancer cells suspended in Matrigel were inoculated by direct injection into the nearest breast fat pad to the right armpit. Mice were sedated with a ketamine (ket)/xylazine (xyl) solution intraperitoneally (IP) (80 mg/kg ket + 10-15 mg/kg xyl) and kept on a thermal mat during sedation to prevent hypothermia. The mice's weight was monitored, and the longest diameter “a” and the shortest diameter “b” of the tumor were measured with a caliper; the tumor volume was determined using the tumor volume formula (TV) = (0.4) (ab2), “a” was the long diameter and “b” the short diameter of the visual tumor. The treatment consisted of 0.25 mg/kg of body weight of CDPs (0.1 mg/mL CDPs) via the IP or 0.05 mg/kg of MTX in physiological saline by IP via or in CDPs+MTX (0.1 mg/mL CDPs, 0.05 mg/mL MTX) combined treatment. The CDPs treatments were carried out by three rounds of administration, each consisting of three doses administered every 3 days (two days between each administration) with a week of rest between each administration round, summing nine doses per mouse. The groups evaluated were the following: mice without tumor and without treatment (C); mice without tumor administered with the CDPs (C+CDPs); mice with tumor and without treatment (BC); mice with tumor and treatment with CDPs from cell inoculation in early stage [BC+CDPs(i)]; mice with tumor and treatment with CDPs at 35th-day post-inoculation in advanced stage (BC+CDPs (m)); advanced-stage tumor-bearing and MTX-treated mice [BC+MTX(m)]; mice with tumor and combined CDPs+MTX treatment [BC+CDPs+MTX(m)]; each group with n=5.
2.7. Animal Euthanasia and Biological Samples
All mice were injected with a lethal dose of sodium pentobarbital intraperitoneally (100-150 mg/Kg body weight) as recommended by IIQB/UMSNH/IACUC and NOM 062-ZOO-1999. The tumors were removed, whole blood was obtained by cardiac puncture, and collected in a microtube with EDTA anticoagulant. The liver, lungs, spleen, kidneys, and femur of both legs were also removed and weighed. Blood hematocrit (Hct) was determined in a capillary tube with heparin by centrifugation at 3500 rpm for 5 min, and Hemoglobin (Hb) was determined by the Hct value divided by 3.3. The whole blood was centrifuged at 3500 rpm for 10 min to separate the blood serum. Subsequently, the enzymes aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH) were determined using a Fuji Dry-Chem NX 700 Fujifilm equipment.
X-ray imaging and development of osteolytic lesions in mice was performed by radiography using a Faxitron MX-20 with a digital camera (Faxitron X-ray Corporation). The image analysis system MetaMorph software (Universal Imaging Corporation) quantified the lesion area.
2.8. Histological Analysis
All organs were fixed in a 4% paraformaldehyde (PFA) solution in PBS for at least 72 h and subsequently subjected to dehydration in increasing concentrations of ethanol and xylol. The dehydrated tissues were embedded in HYCEL paraffin, and 4 µm sections were cut on a microtome. Hematoxylin-eosin (H&E) staining tissues were mounted in epoxy resin and stored at room temperature. Histopathological and photographs were analyzed by optical microscopy.
2.9. Bones and Tissue Histology
After euthanasia, the lower limbs of the mice were dissected, removing skin and muscle tissue in the femurs. Femurs were fixed in paraformaldehyde and treated with 3 mL decalcification solution (10% EDTA, pH 7.4) for four weeks. For dehydration, samples underwent sequential ethanol treatments with increasing concentrations (80–100%), followed by xylene treatment and paraffin infiltration (Hycel) in two cycles before embedding in histological molds. The femurs were sectioned longitudinally to 5 μm-thick slices using a rotary HM 355S microtome (Thermo Fisher Scientific). To assess bone resorption activity, tumor area, and the presence of osteoclasts and osteoblasts, the bone sections were stained with hematoxylin and eosin (H&E).
Livers and lungs were fixed in 4% paraformaldehyde remained until dehydration. The samples were subjected to a dehydration process of 4 h at different concentrations of ethanol and xylene, and embedded in paraffin. Tissue sections of 4 μm were cut and placed on slides for subsequent staining with H&E. Photographs were taken under the optic microscopy and recorded using an Accu-Scope EXC-120 LED microscope camera at magnifications of 4x, 10x, 40x, and 100x across tissue sections.
2.10. Statistical Analysis
All data were evaluated using analysis of variance (ANOVA; significant differences (p < 0.05) are indicated by asterisks; * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001) and Dunnett's or with Bonferroni posthoc tests using GraphPad Prism 6.0 software (GraphPad Software).
4. Discussion
CDPs (diketopiperazines) have emerged as promising candidates for anticancer therapy due to their structural stability, high selectivity, and ability to effectively inhibit key cancer-related pathways[
20]. Previously, the cytotoxic and apoptotic effects of the bacterial CDPs have been demonstrated in various cancer cell lines [
10,
11,
12,
15,
19]; in addition, their impact on breast cancer lines MCF-7 and MDA-MB-231 cells was described, triggering apoptosis in both cell lines in a concentration-dependent manner [
12].
Several specific CDPs have exhibited potent anticancer activity; Cyclo(Phe-Pro) inhibits the growth of HT-29, MCF-7 and HeLa cells[
21], Cyclo(Tyr-Cys) inhibits cervical carcinoma cells HT-29 and MCF7 [
22], Cyclo(L-Leu-D-Arg) shows cytotoxicity against MDA-MB-231 cells [
23]. Diketopiperazines such as fumitremorgin C analogs have shown potential in overcoming multidrug resistance, including inhibition of the breast cancer resistance protein (BCRP), a key efflux transporter responsible for reducing intracellular drug accumulation. Moreover, the novel diketopiperazine-based compound HLY838 functions as an O-GlcNAc transferase (OGT) inhibitor, potentiating the anti-tumor effects of CDK9 inhibitors by downregulation c-Myc and E2F1 expression [
24]. Collectively, these findings highlight the CDPs as anticancer agents. Similarly, Verticillin A, a diketopiperazine-derived compound, suppresses c-Met phosphorylation and its downstream Ras/Raf/MEK/ERK signaling pathway, significantly reducing colon cancer cell metastasis [
25]. Bacterial CDPs have demonstrated significant potential as anti-metastasic agents by targeting key proteins involved in epithelial-mesenchymal transition (EMT) and metastasis. In the murine melanoma model, CDPs derived from the
P. aeruginosa bacterium significantly reduced the expression of critical EMT markers, including MMP-1, E-cadherin, N-cadherin, HIF-1a, Vimetin, and CK-1; indicating that CDPs may impact cancer cell migration and invasion [
13].
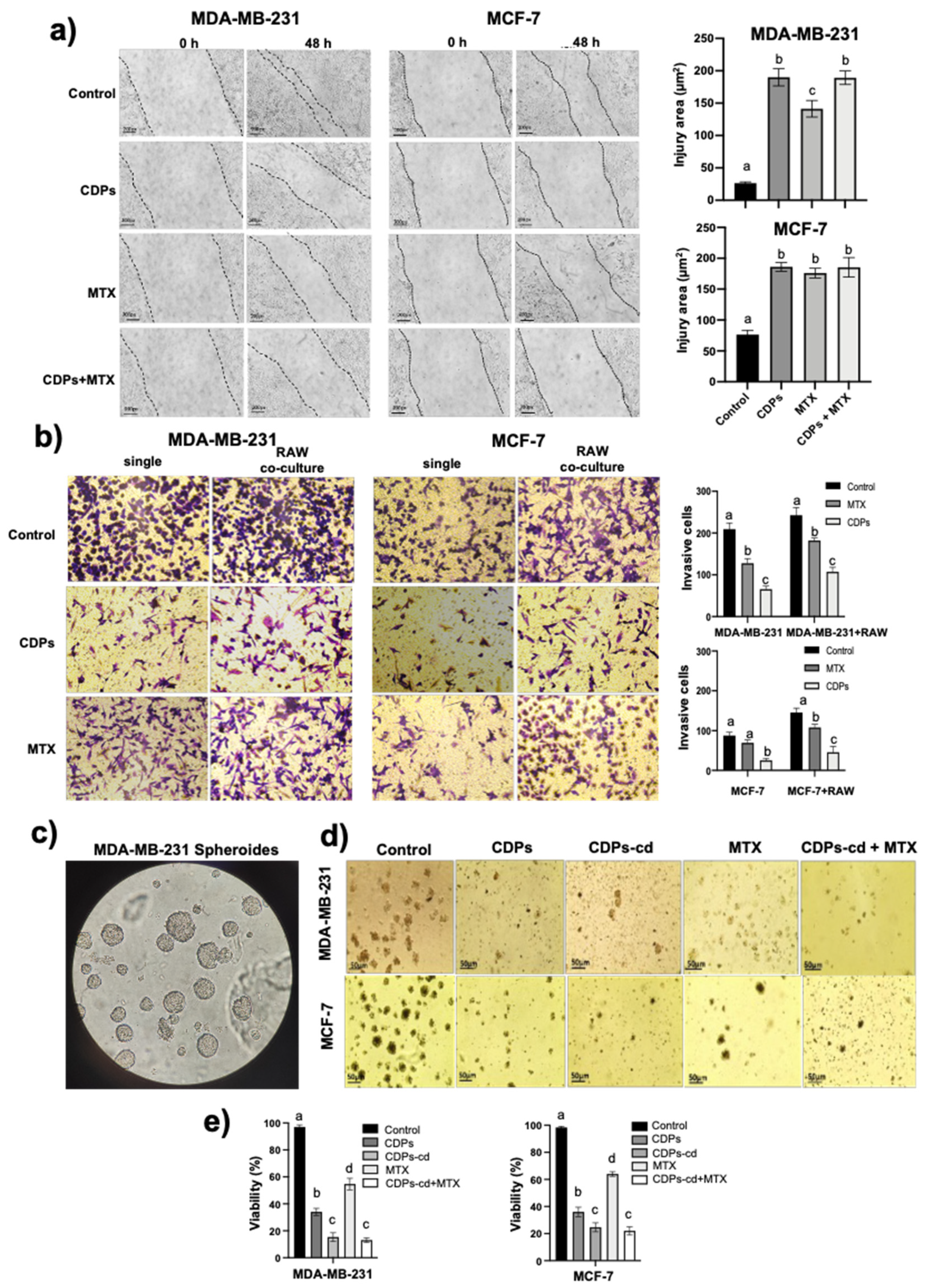
In this work, functional assays further confirmed the anti-metastasic effects of
P. aeruginosa CDPs. Wound healing assays in monolayers of cell lines cultures of the MCF7 and MDA-MB-231 breast cancer lines revealed that CDPs-treated cancer cells exhibited a wound area twice as large as the control and 1.5 times that of cells treated with methotrexate (MTX). MCF7 cells displayed lower migratory capacity than MDA-MB-231 cells in all conditions (
Figure 1a).
Transwell chamber assays using Matrigel and co-culture with macrophages revealed that tumor-associated macrophages (TMAs) enhanced cancer cell invasion by promoting Matrigel degradation and membrane penetration. However, treatment with CDPs significantly reduced the number of invasive cells in both monoculture and co-culture conditions, suggesting their potential as metastatic agents. This inhibitory effect was comparable to MTX, which has been evaluated in combination therapies for metastatic disease, including bone metastases (
Figure 1b). These findings align with previous reports indicating that TAMs play a crucial role in tumor progression by secreting chemokines and growth factors that facilitate cancer cells proliferation, migration and survival [
26]. Moreover, TAMs have been implicated in modulating drug resistance, further supporting their relevance as therapeutic targets. The ability of the bacterial CDPs to disrupt TAM cancer cell interactions highlights their potential dual role in inducing apoptosis and inhibiting metastasis.
The multicellular microspheroid model contains subpopulations of cancer stem cells (CSCs) [
27] exhibiting self-renewal capacity and therapy resistance. Our micro spheroids assay with MCF7 and MDA-MB-231 cells demonstrated distinct phenotypic differences between the two lines. MCF7 spheroids were more compact and more enormous, likely due to their epithelial phenotype and high E-cadherin expression [
28], while MDA-231-MB microspheroids were looser and more heterogeneous, reflecting their mesenchymal phenotype. Notably, the CDPs treatment significantly reduced spheroids size, number, and viability in both cell lines compared to untreated controls and MTX-treated (
Figure 1c-e). These results underscore the potential of bacterial CDPs as effective anti-metastatic agents by targeting both tumor cell invasion and CSC-associated resistance.
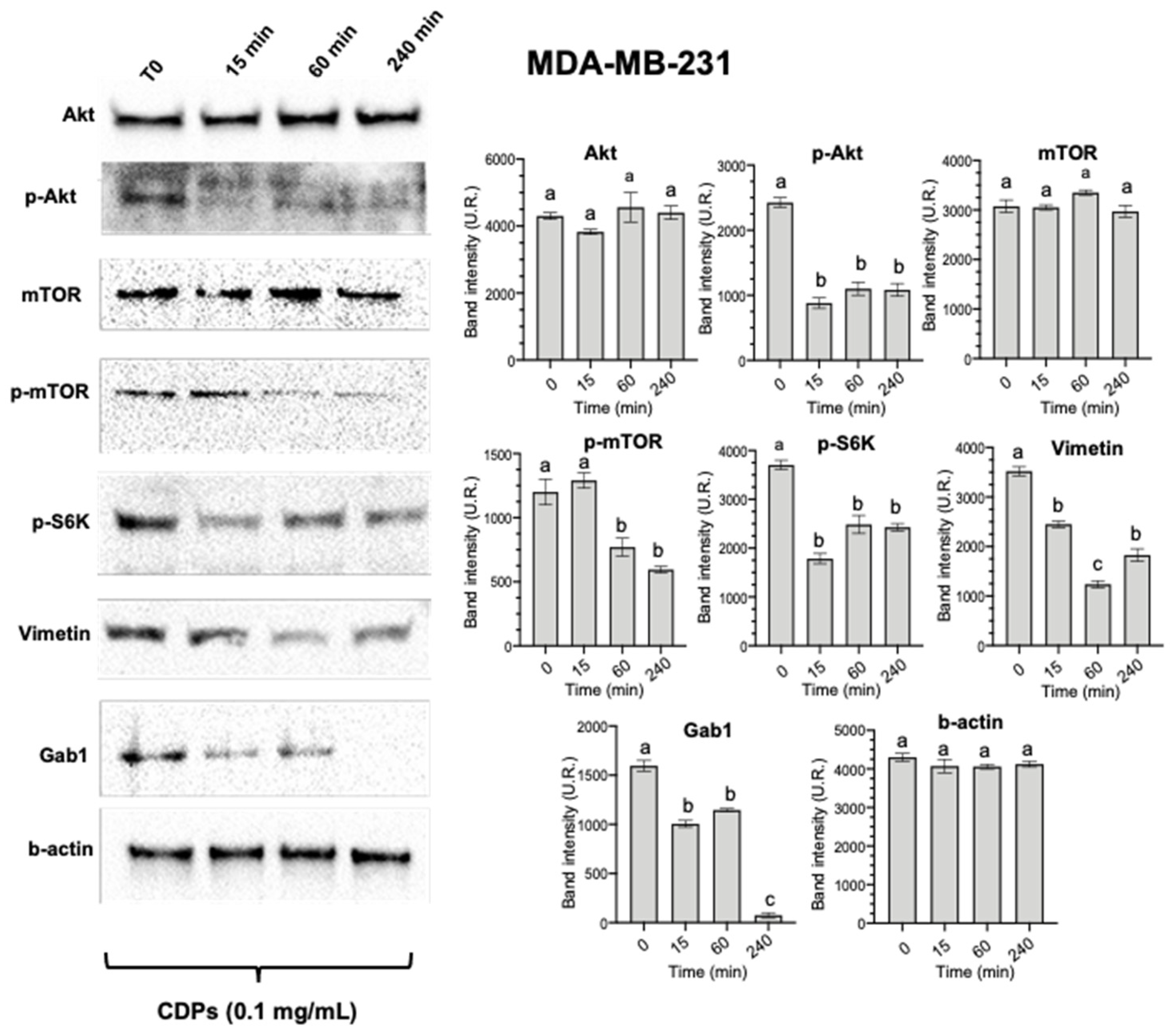
Previous studies from our group have demonstrated the involvement of the PI3K/AKT/mTOR pathway in the anticancer effects of PAO1-CDPs [
10,
11,
13]. Based on these findings, we analyzed key components of this pathway in the MDA-MB-231 cell line, observing a significant decrease in the phosphorylation levels of AKT, mTOR, and S6K (
Figure 2). This reduction in protein expression is associated with decreased cell viability, impaired tumor growth, and induction of apoptosis, corroborating previous observations [
12]. Additionally, our results revealed a notable decrease in the expression of Vimentin and Gab1 following treatment with CDPs, further supporting the role of these molecules in targeting metastatic and invasive pathways (
Figure 2). Gab1 overexpression has been linked to enhanced breast cancer metastasis [
29]. At the same time, Vimetin is a well-established marker of EMT and is consistently upregulated during cancer progression and metastasis [
30]. Therefore, the observed downregulation of Gab1 and Vimetin suggests reduced invasive and migratory capacities, which may translate into decreased tumor aggressiveness.
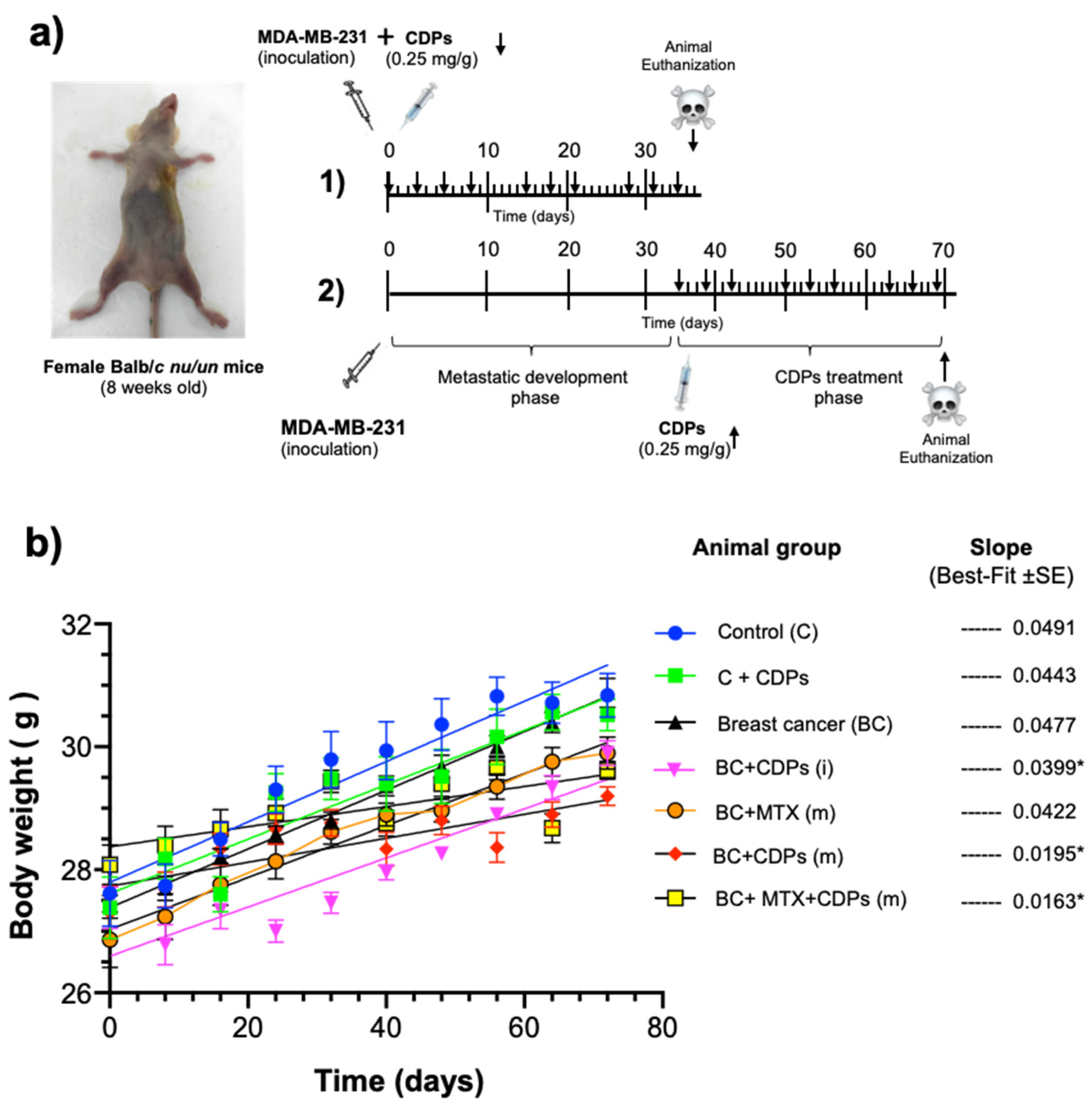
Weight loss is often one of the earliest detectable symptoms of cancer disease and its progression, leading to severe muscle wasting, which significantly contributes to morbidity and mortality. This condition is primarily driven by the increased production of cytokines and other pro-inflammatory molecules secreted by the immune system to inhibit tumor progression [
31,
32]. In our orthotopic model of metastatic breast cancer, body weight was monitored throughout the treatment period. While the overall pattern of weight gain remained consistent across groups, a transient weight loss was observed in animals treated with CDPs during the initial weeks of administration (
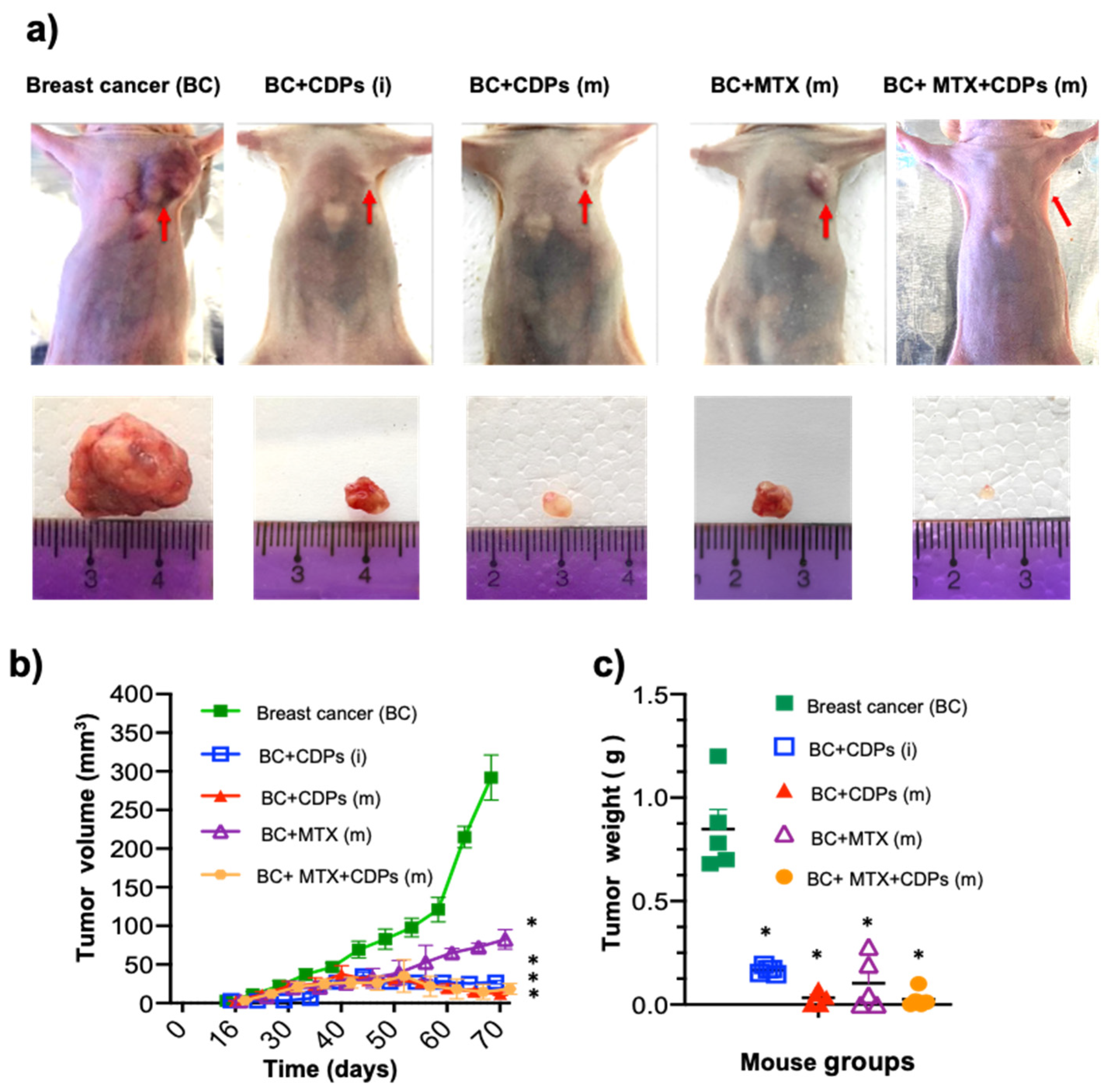
Figure 3b). Nevertheless, this effect did not persist; no behavioral changes or signs of deteriorating health were observed, suggesting that the temporary weight loss did not indicate toxicity or systemic distress. Although the volume and weight of the tumors generated in the BC group were significantly observed (
Figure 4), they did not significantly modify the weight of the animals (
Figure 3b). Notably, the administration of CDPs in mice prevented the generation of large and heavy tumors, observing that 40% of animals did not show tumors (
Figure 4).
In breast cancer patients, alterations in leukocyte composition, particularly in the neutrophil-to-lymphocyte ratio (NRL) have been documented. NLR is widely recognized as a prognostic biomarker in cancer, with elevated levels correlating with worse prognosis, increased tumor aggressiveness, and reduced overall survival [
33]. The findings suggest that changes in leukocyte distribution may have significant clinical implications in breast cancer progression. In our study, alterations in leukocyte composition were also observed in mice with breast cancer. NLR analysis revealed that the BC group exhibited the highest value (NLR=8). In contrast, the groups BC+CDPs(i) (NLR=3) and BC+MTX+CDPs (NLR=3.5) showed significantly lower values, suggesting a potential reduction in tumor aggressiveness following CDPs treatment. Anemia is also common among cancer patients (Muthanna et al., 2022). In our hematological analysis, hemoglobin levels showed improvement in animals treated with CDPs (
Figure 5d), indicating a potential benefit of these molecules in mitigating cancer-associated hematological alterations.
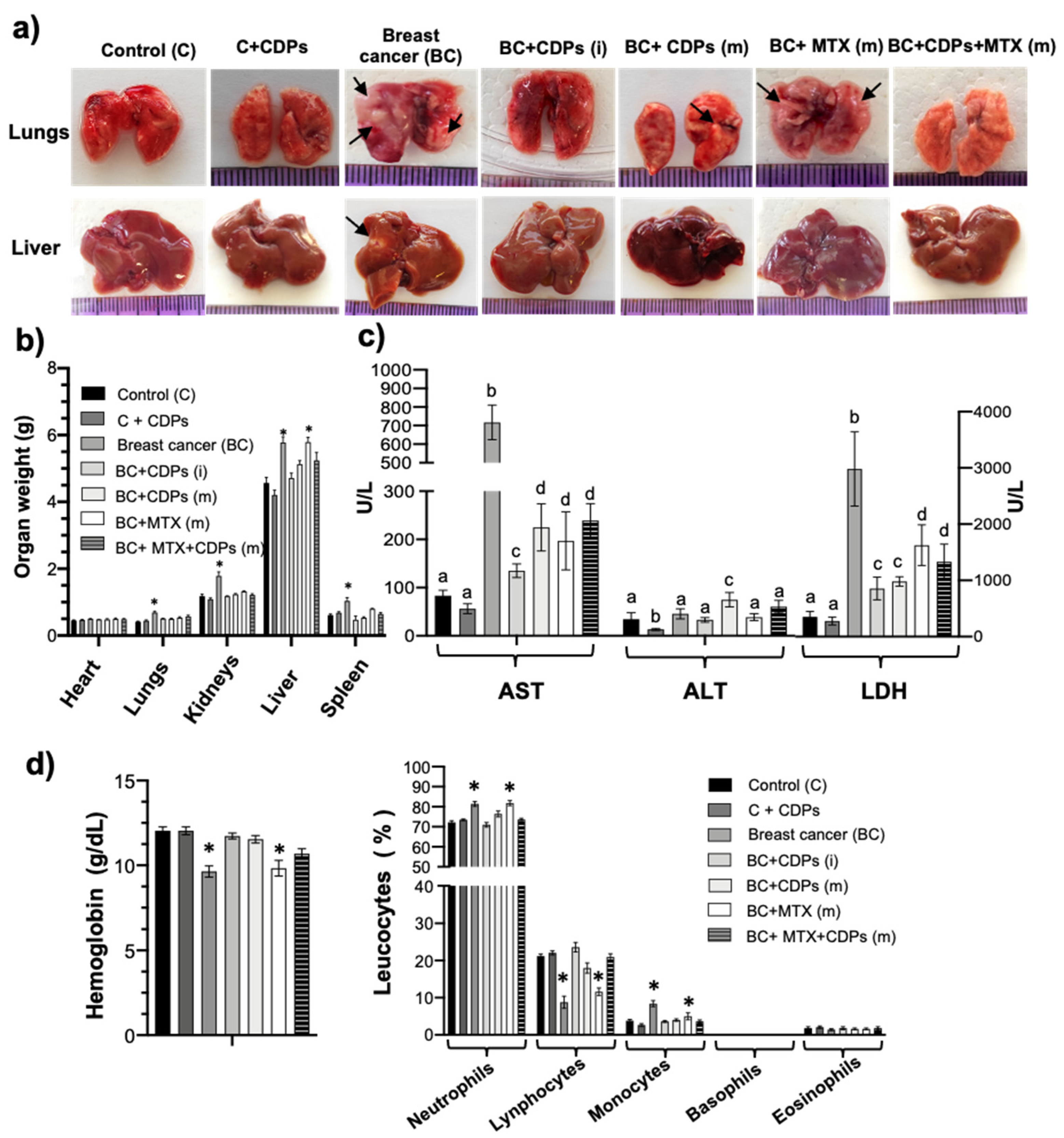
Liver metastases are common in patients with breast cancer. Previous studies have described that liver function is poor in 92% of all patients diagnosed with breast cancer liver metastasis (BCLM) [
34]. Moreover, ALT, AST, GGT, AP, and LDH levels are significantly higher in patients with BCLM (Nesbit et al., 2021). The determination of AST, ALT, and LDH showed a drastic increase in the group with BC and without treatment (
Figure 5c). The presence of metastatic foci was observed in this group of animals (
Figure 5a); consistent with these observations, an increase in the weight of this organ was also observed (
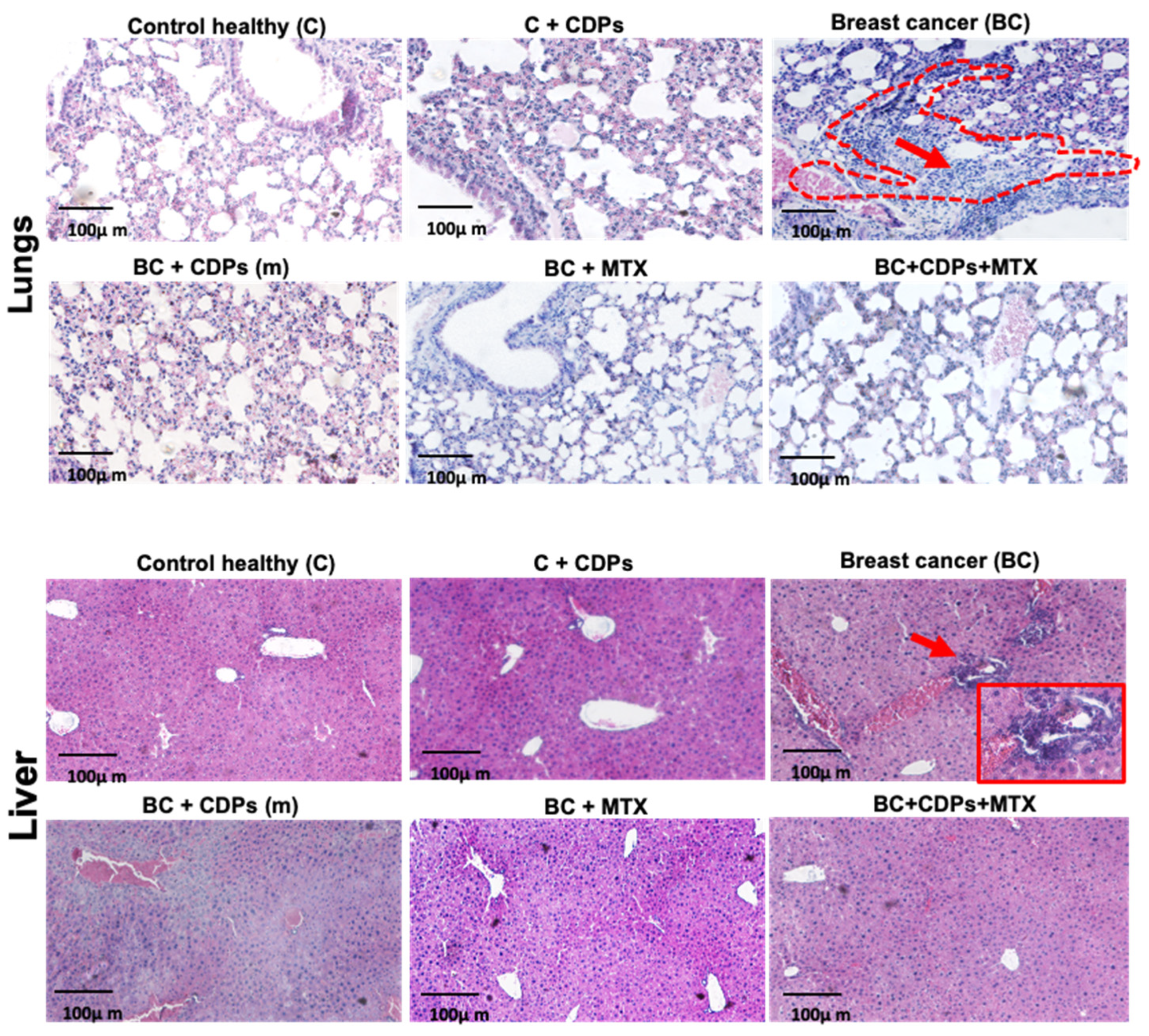
Figure 5b). Histological analysis of lung and liver in mice revealed that treatment with CDPs inhibited malign cells and tumor focus (
Figure 6). These findings suggest that the animals treated with CDPs presented levels of AST, ALT, and LDH and organs similar to the control without disease, indicating a positive anti-tumor capability associated with the CDPs treatment.
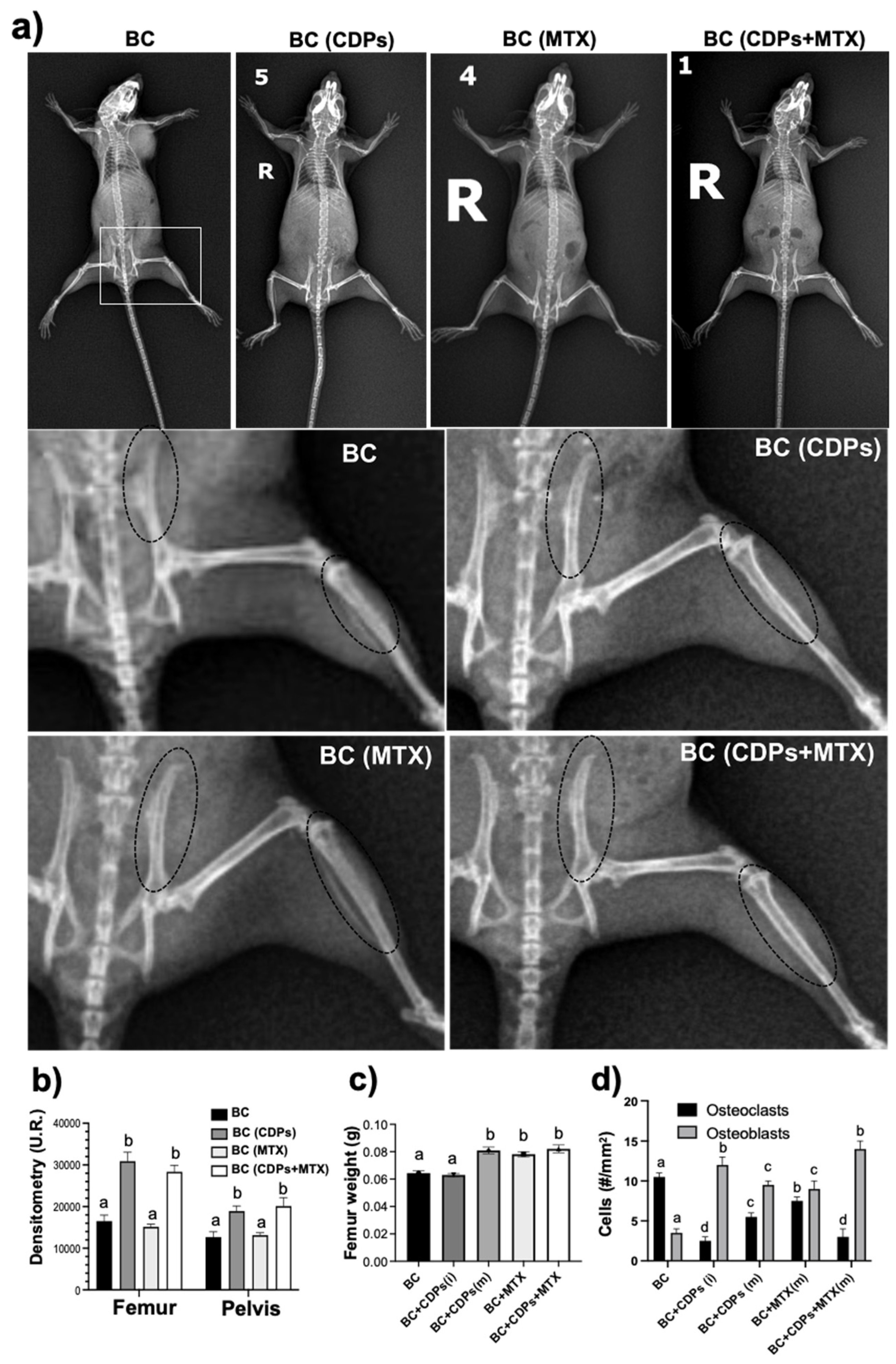
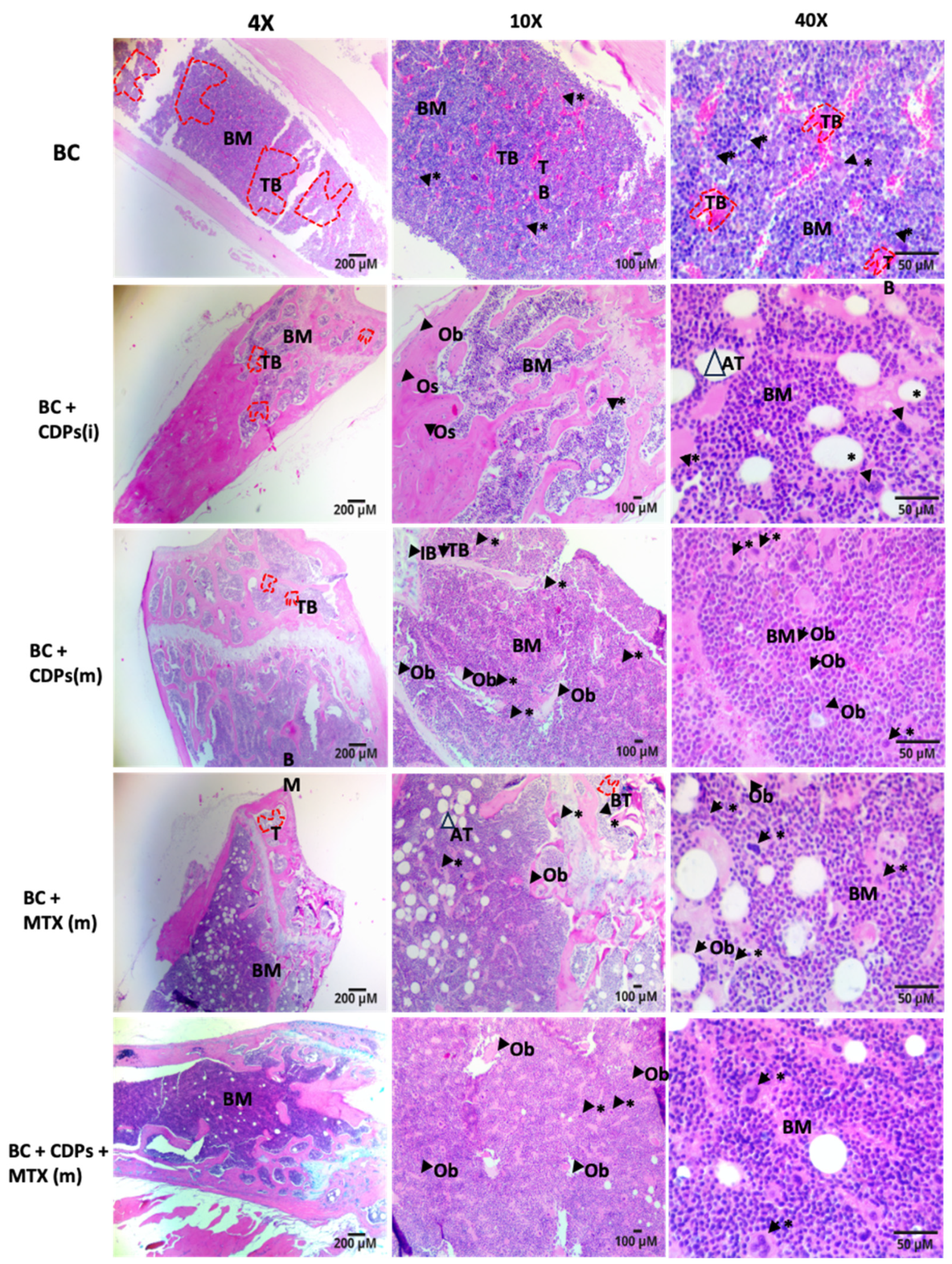
Histological analysis of the femur in mice revealed that treatment with CDPs led to an increase in the number of osteoblasts (
Figure 7d and
Figure 8). These cells play a crucial role in osteogenesis by producing and depositing the organic bone matrix [
35]. This finding suggests a potential pro-osteogenic effect of CDPs. A similar increase in osteoblast number was observed in the group treated with both CDPs+MTX (
Figure 7d). However, in the BC [CDPs+MTX(i)] group, a notable accumulation of bone marrow adipose tissue (BMAT) was also detected. This increase in BMAT was similarly observed in the sections of animals treated exclusively with MTX, indicating that the presence of BMAT was primarily driven by the administration of this chemotherapeutic agent (
Figure 8).
The development of BMAT is a normal physiological process; however, excessive BMAT accumulation may have a significant pathological implication [
36]. Previous studies have proposed that chemotherapy-induced bone defects arise from multiple mechanisms, including impaired nutrient absorption and malnutrition due to chemotherapy-induced intestinal mucosal damage and disruptions in bone modeling and remodeling (
Figure 5b). Densitometry analysis of bones further shows the decalcification of the pelvis and femur in the BC group, which was alleviated by the CDPs treatment (
Figure 7). In agreement, infiltration of breast cancer MDA-MB-231 cells and leukocytes in tissue was observed by histological analysis of the femur from the BC group, which was recovered in the mice treated with CDPs (
Figure 8).
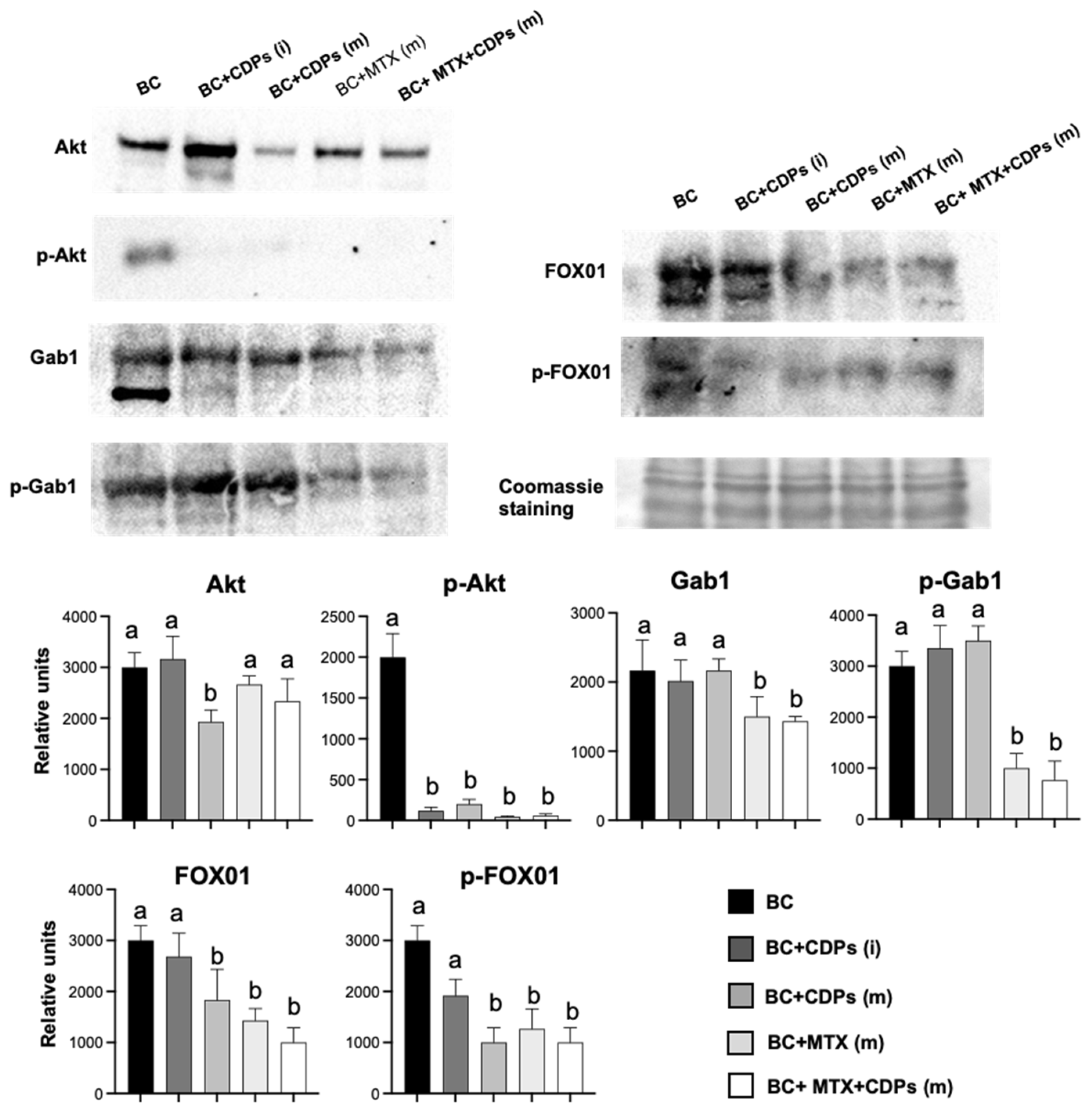
Furthermore, critical tumorigenic markers were repressed in the BC CDPs-treated mice, and a significant reduction in p-AKT levels was observed in tumors from rodents subjected to treatment (
Figure 9). Notably, animals treated with CDPs also exhibited a decrease in total AKT protein levels, suggesting a potential disruption of the PI3K/AKT/mTOR signaling pathway in tumors.
AKT is pivotal in regulating FOX01 phosphorylation, a key factor in cell cycle regulation and apoptosis. Under normal conditions, AKT phosphorylates FOX01, excluding it from the nucleus and suppressing its transcriptional activity. However, when FOX01 remains dephosphorylated, it is translocated to the nucleus, activating apoptosis-related genes and cell cycle arrest [
37].
FOX01, a member of the Forkhead box family of transcription factors, is known to regulate cell cycle arrest, autophagy, and apoptosis. Its tumor-suppressive role has been reported in several malignancies, including breast cancer, where its dysregulated is frequently observed [
38]. In our study, tumors from CDPs-treated mice exhibited reduced phosphorylation of FOX01, supporting that CDPs inhibit tumor progression (
Figure 9). These findings align with our previous transcriptomic analysis in HeLa cells treated with CDPs, where genes involved in the FOX01 signaling pathway, including GADD45A and SGK1, were upregulated [
14]. Suggesting a differential regulation of FOX01 by CDPs in the triple-negative breast cancer model.
Contrary to observations in the MDA-MB-231 cell line (
Figure 2), Gab1 levels remained unchanged in response to CDPs treatment alone. However, a notable decrease in both total Gab1 and phosphorylated Gab1 (p-Gab1) levels was detected in tumors from the BC (CDPs+MTX) and BC (MTX) groups. Given that Gab1 acts as a key integrator of multiple signaling pathways involved in cell survival, proliferation, angiogenesis, and invasion [
39]. The Gab1 downregulation suggests a potential mechanism through which CDPs, particularly in combination with MTX, inhibit tumor progression.
Figure 1.
Effects of CDPs on migratory and invasiveness of MDA-MB-231 and MCF-7 breast cancer cells. a) Representative photographs of wound closure migration assays taken at 0 h and 48 h in breast cancer cells treated with the saline solution vehicle, CDPs, MTX, or combined CDPs+MTX treatment. b) Representative photographs of the cancer cells that managed to invade the Matrigel-covered membrane stained with crystal violet. The simple culture conditions and co-culture with Raw 264.7 macrophages are shown. (a-b) On the right, the quantification of the wound area and invasive cells from (a) and cell number from (b) is done using ImageJ Software. c) Representative photographs of multicellular microspheroids of MDA-MB-231. d) Cell viability of the microspheroids of MDA-MB-231 and MCF-7 cell cultures submitted to CDPs treatments for 72 h. e) Cell viability of the microspheroids from (d) determined by the MTT assay. Bars represent means ±SE, n=3. Statistical analysis was performed using one-way ANOVA with Dunnett's posthoc test. SE values are shown as bars, and significant differences are indicated with different letters (p˂0.05). CDPs, cyclodipeptides; MTX, methotrexate; CDPs-cd, cyclodipeptides dissolved in β-cyclodextrins; CDPs-cd+MTX, combined treatment.
Figure 1.
Effects of CDPs on migratory and invasiveness of MDA-MB-231 and MCF-7 breast cancer cells. a) Representative photographs of wound closure migration assays taken at 0 h and 48 h in breast cancer cells treated with the saline solution vehicle, CDPs, MTX, or combined CDPs+MTX treatment. b) Representative photographs of the cancer cells that managed to invade the Matrigel-covered membrane stained with crystal violet. The simple culture conditions and co-culture with Raw 264.7 macrophages are shown. (a-b) On the right, the quantification of the wound area and invasive cells from (a) and cell number from (b) is done using ImageJ Software. c) Representative photographs of multicellular microspheroids of MDA-MB-231. d) Cell viability of the microspheroids of MDA-MB-231 and MCF-7 cell cultures submitted to CDPs treatments for 72 h. e) Cell viability of the microspheroids from (d) determined by the MTT assay. Bars represent means ±SE, n=3. Statistical analysis was performed using one-way ANOVA with Dunnett's posthoc test. SE values are shown as bars, and significant differences are indicated with different letters (p˂0.05). CDPs, cyclodipeptides; MTX, methotrexate; CDPs-cd, cyclodipeptides dissolved in β-cyclodextrins; CDPs-cd+MTX, combined treatment.
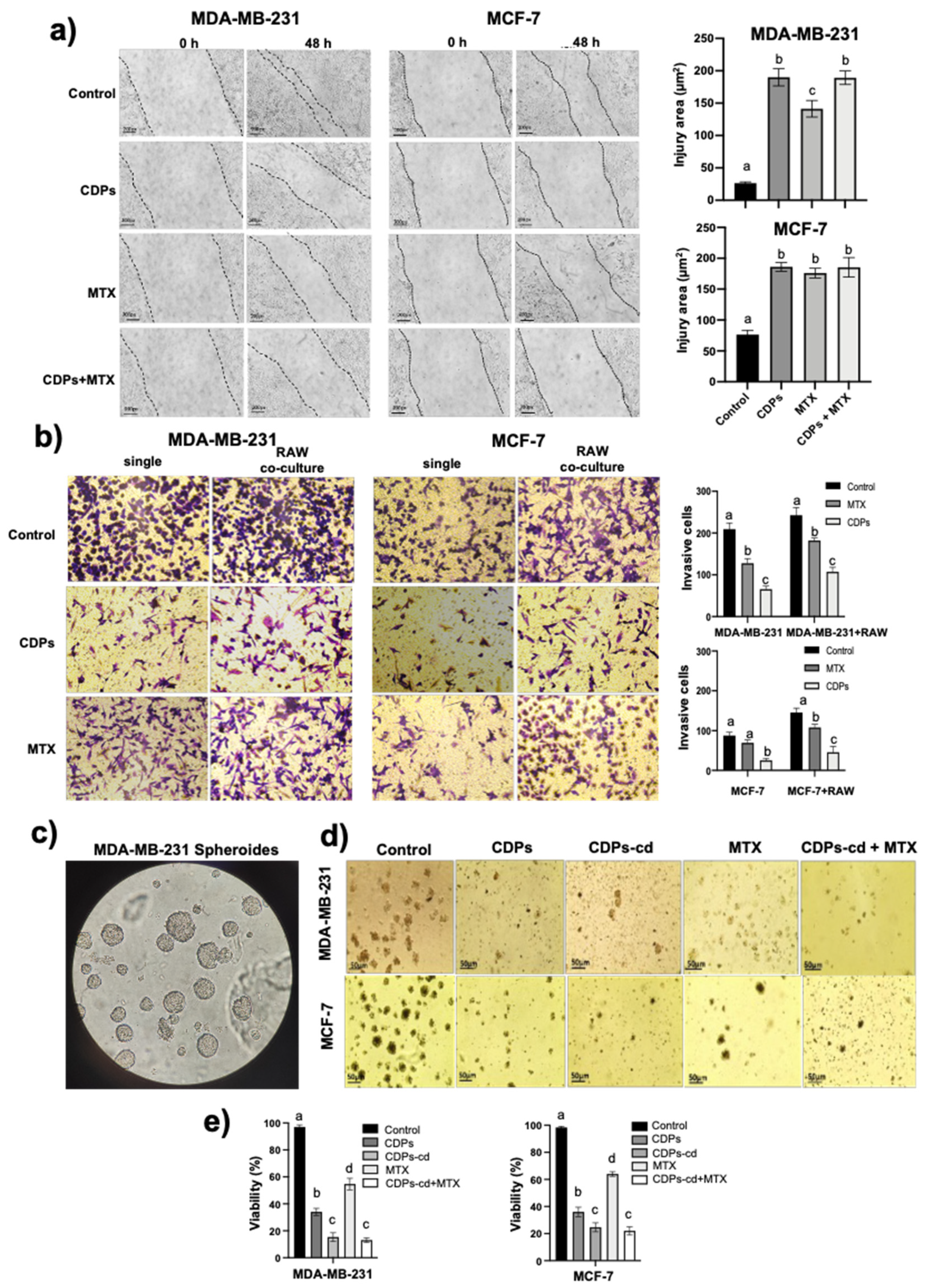
Figure 2.
Effect of CDPs on proteins involved in proliferation, invasion, and metastasis in MDA-MB-231 breast cancer cells. Protein extracts obtained from the cell cultures treated with CDPs (0.1 mg/mL) in function of time were subjected to immunodetection. Protein expression for the total Akt, phosphorylated Akt, total mTOR, phosphorylated mTOR, total S6K, phosphorylated S6K, Vimentin, and B-actin are shown. Densitometric analyses of the protein immunodetection results are presented on the right. The bars represent the means ± SE, n=3 per group. Statistical analysis was performed using one-way ANOVA, followed by Dunnett's post hoc test; SE values are shown as bars, and significant differences are indicated with different letters (p <0.05).
Figure 2.
Effect of CDPs on proteins involved in proliferation, invasion, and metastasis in MDA-MB-231 breast cancer cells. Protein extracts obtained from the cell cultures treated with CDPs (0.1 mg/mL) in function of time were subjected to immunodetection. Protein expression for the total Akt, phosphorylated Akt, total mTOR, phosphorylated mTOR, total S6K, phosphorylated S6K, Vimentin, and B-actin are shown. Densitometric analyses of the protein immunodetection results are presented on the right. The bars represent the means ± SE, n=3 per group. Statistical analysis was performed using one-way ANOVA, followed by Dunnett's post hoc test; SE values are shown as bars, and significant differences are indicated with different letters (p <0.05).
Figure 3.
Anti-tumor procedure in MDA-MB-231 immunosuppressed mice breast cancer model by CDPs treatment. Female Balb/c nu/un mice (8 weeks old) were submitted to an anti-tumor study by 60 days. a) Two treatment conditions were tested: i) the MDA-MB-231cell line inoculation joined with the CDPs treatment at the time of cell implantation, following the treatment of nine doses of CDPs (0.25 mg/g) under 35 days procedure (arrows). The second procedure consisted of the development of metastatic tumor by MDA-MB-231cell line inoculation during 30 days; after that, the CDPs treatment was started and followed by nine doses of CDPs (0.25 mg/g) during 35 days procedure (arrows). b) During the development of the study, the body weight was monitored. The slope of weight gain values is shown in all the mice groups (right). Statistical analysis was performed using t-student; values are displayed, and significant differences are indicated with asterisks (p <0.05). Control (C), animals that received standard rodent diet without treatment; C+CDPs, animals control that received CDPs treatment; BC, animals that developed breast cancer without treatment; BC+CDPs (i), BC animals that received CDPs treatment as the procedure (i); BC+CDPs (m), ), BC animals that received CDPs treatment as procedure (m); BC+MTX (m), ), BC animals that received methotrexate treatment as procedure (m); BC+CDPs+MTX (m), BC animals that received CDPs + methotrexate treatment as procedure (m).
Figure 3.
Anti-tumor procedure in MDA-MB-231 immunosuppressed mice breast cancer model by CDPs treatment. Female Balb/c nu/un mice (8 weeks old) were submitted to an anti-tumor study by 60 days. a) Two treatment conditions were tested: i) the MDA-MB-231cell line inoculation joined with the CDPs treatment at the time of cell implantation, following the treatment of nine doses of CDPs (0.25 mg/g) under 35 days procedure (arrows). The second procedure consisted of the development of metastatic tumor by MDA-MB-231cell line inoculation during 30 days; after that, the CDPs treatment was started and followed by nine doses of CDPs (0.25 mg/g) during 35 days procedure (arrows). b) During the development of the study, the body weight was monitored. The slope of weight gain values is shown in all the mice groups (right). Statistical analysis was performed using t-student; values are displayed, and significant differences are indicated with asterisks (p <0.05). Control (C), animals that received standard rodent diet without treatment; C+CDPs, animals control that received CDPs treatment; BC, animals that developed breast cancer without treatment; BC+CDPs (i), BC animals that received CDPs treatment as the procedure (i); BC+CDPs (m), ), BC animals that received CDPs treatment as procedure (m); BC+MTX (m), ), BC animals that received methotrexate treatment as procedure (m); BC+CDPs+MTX (m), BC animals that received CDPs + methotrexate treatment as procedure (m).
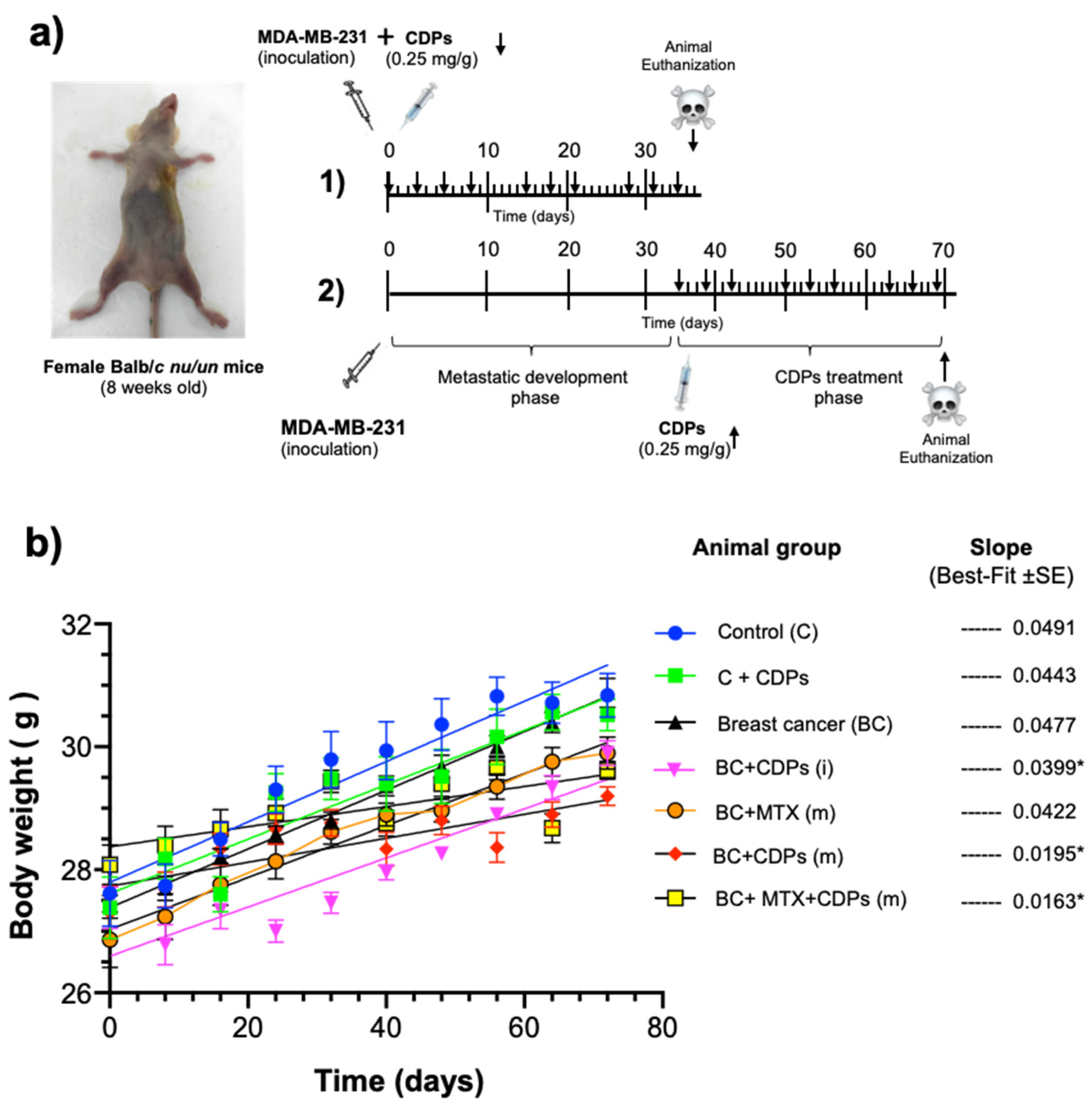
Figure 4.
Anti-tumor effect of CDPs on xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice.
a) Photograph of mouse groups on the 60th day of the experimental procedure before euthanizing. Representative photographs of tumors from each mouse group are shown; nomenclature is indicated in
Figure 3. The scale of the ruler corresponds to centimeters.
b) Determination of tumor volume expressed in mm
3.
c) Tumor weight expressed in grams. Bars represent the means ± SE, n = 5. One-way ANOVA with Bonferroni post-hoc test was used to compare treatments with the untreated group (BC); significant differences (
p< 0.05) are indicated with an asterisk (*).
Figure 4.
Anti-tumor effect of CDPs on xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice.
a) Photograph of mouse groups on the 60th day of the experimental procedure before euthanizing. Representative photographs of tumors from each mouse group are shown; nomenclature is indicated in
Figure 3. The scale of the ruler corresponds to centimeters.
b) Determination of tumor volume expressed in mm
3.
c) Tumor weight expressed in grams. Bars represent the means ± SE, n = 5. One-way ANOVA with Bonferroni post-hoc test was used to compare treatments with the untreated group (BC); significant differences (
p< 0.05) are indicated with an asterisk (*).
Figure 5.
Anti-tumor effect of CDPs on organs of xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice.
a) Photograph of lungs and liver of mice dissected on the 60th day of the experimental procedure. Arrows indicate metastatic foci in organs. Representative photographs of organs from each mouse group are shown; nomenclature is shown in
Figure 3.
b) Determination of organ weight expressed in grams.
c) Determination of enzyme activity of AST, ALT, and LDH in serum of mice groups.
d) Hematological profile, hemoglobin (g/dL), and leucocyte counts in mice with metastatic breast cancer implantation. Graphs represent the means ± SE, n = 5. One-way ANOVA with Bonferroni post-hoc test was used to compare treatments with the untreated group (BC); significant differences (
p< 0.05) are indicated as different letters or with asterisks (*).
Figure 5.
Anti-tumor effect of CDPs on organs of xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice.
a) Photograph of lungs and liver of mice dissected on the 60th day of the experimental procedure. Arrows indicate metastatic foci in organs. Representative photographs of organs from each mouse group are shown; nomenclature is shown in
Figure 3.
b) Determination of organ weight expressed in grams.
c) Determination of enzyme activity of AST, ALT, and LDH in serum of mice groups.
d) Hematological profile, hemoglobin (g/dL), and leucocyte counts in mice with metastatic breast cancer implantation. Graphs represent the means ± SE, n = 5. One-way ANOVA with Bonferroni post-hoc test was used to compare treatments with the untreated group (BC); significant differences (
p< 0.05) are indicated as different letters or with asterisks (*).
Figure 6.
Histological features of lungs and liver of xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice treated with CDPs. Female Balb/c nu/nu mice (8 weeks old) were submitted to an anti-tumor study by 60 days. Liver tissue sections were stained with hematoxylin and eosin and observed using microscopy; representative photographs of tissues dissected from the animal groups are shown and named in
Figure 3. Arrows show breast cancer MDA-MB-231 cell infiltration; boxes indicate leukocyte infiltration in liver tissue.
Figure 6.
Histological features of lungs and liver of xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice treated with CDPs. Female Balb/c nu/nu mice (8 weeks old) were submitted to an anti-tumor study by 60 days. Liver tissue sections were stained with hematoxylin and eosin and observed using microscopy; representative photographs of tissues dissected from the animal groups are shown and named in
Figure 3. Arrows show breast cancer MDA-MB-231 cell infiltration; boxes indicate leukocyte infiltration in liver tissue.
Figure 7.
Analysis of bone cancer in xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice treated with CDPs. Female Balb/c nu/un mice (8 weeks old) were submitted to an anti-tumor study by 60 days. Animal groups are named as in
Figure 3.
a) Radiographic images show representative images of animal groups implanted with breast cancer (BC) and treated with anti-neoplastic drugs. The zoom of the pelvis and femur are shown, and the zones of bone destruction are used to carry out a densitometric analysis using the Image J software.
b) Densitometry of Femur and pelvis. C) Determination of calcium in the femur. Graphs represent the means ± SE, n = 5. One-way ANOVA with Bonferroni post-hoc test was used to compare treatments with the untreated group (BC); significant differences (
p< 0.05) are indicated as different letters.
Figure 7.
Analysis of bone cancer in xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice treated with CDPs. Female Balb/c nu/un mice (8 weeks old) were submitted to an anti-tumor study by 60 days. Animal groups are named as in
Figure 3.
a) Radiographic images show representative images of animal groups implanted with breast cancer (BC) and treated with anti-neoplastic drugs. The zoom of the pelvis and femur are shown, and the zones of bone destruction are used to carry out a densitometric analysis using the Image J software.
b) Densitometry of Femur and pelvis. C) Determination of calcium in the femur. Graphs represent the means ± SE, n = 5. One-way ANOVA with Bonferroni post-hoc test was used to compare treatments with the untreated group (BC); significant differences (
p< 0.05) are indicated as different letters.
Figure 8.
Histological features of femurs from xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice treated with CDPs. Female Balb/c nu/un mice (8 weeks old) were submitted to an anti-tumor study by 60 days. Femur tissue sections were stained with hematoxylin and eosin and observed using microscopy; representative photographs of tissues dissected from the animal groups are shown and named as in
Figure 3. Arrows show breast cancer MDA-MB-231 cell infiltration; boxes indicate leukocyte infiltration in liver tissue. Representative sections stained by H&E (×4 magnification, Scale bar =200 μm; ×10 magnification, Scale bar =100 μm and ×40 magnification, Scale bar =50 μm) methods of the femur in experimental groups. Red dotted lines outline tumor cell populations indicating tumor bone (TB), which are represented as pink areas. The purple region represents the bone marrow (BM). Tumor bone (TB), osteoblasts (Ob), osteons (Os), immature bone (IB), osteoclasts (*), and bone marrow adipose tissue (AT). Quantification of osteoclasts and osteoblasts in H&E-stained femur sections. Bars represent mean ± SE (n = 3), with statistical significance at p < 0.05. Data were analyzed using one-way ANOVA followed by Tukey's test for multiple comparisons against the control. Statistically significant differences are indicated by letters. Abbreviations: BC (Breast Cancer, no treatment); BC+CDPs (i) (Cyclodipeptides treatment from the start); BC+CDPs (m) (Cyclodipeptides treatment in advanced cancer); MTX (Methotrexate treatment); BC+CDPs+MTX (m) (Combination of Cyclodipeptides and Methotrexate in advanced cancer).
Figure 8.
Histological features of femurs from xenografted breast cancer MDA-MB-231 cells in immunosuppressed mice treated with CDPs. Female Balb/c nu/un mice (8 weeks old) were submitted to an anti-tumor study by 60 days. Femur tissue sections were stained with hematoxylin and eosin and observed using microscopy; representative photographs of tissues dissected from the animal groups are shown and named as in
Figure 3. Arrows show breast cancer MDA-MB-231 cell infiltration; boxes indicate leukocyte infiltration in liver tissue. Representative sections stained by H&E (×4 magnification, Scale bar =200 μm; ×10 magnification, Scale bar =100 μm and ×40 magnification, Scale bar =50 μm) methods of the femur in experimental groups. Red dotted lines outline tumor cell populations indicating tumor bone (TB), which are represented as pink areas. The purple region represents the bone marrow (BM). Tumor bone (TB), osteoblasts (Ob), osteons (Os), immature bone (IB), osteoclasts (*), and bone marrow adipose tissue (AT). Quantification of osteoclasts and osteoblasts in H&E-stained femur sections. Bars represent mean ± SE (n = 3), with statistical significance at p < 0.05. Data were analyzed using one-way ANOVA followed by Tukey's test for multiple comparisons against the control. Statistically significant differences are indicated by letters. Abbreviations: BC (Breast Cancer, no treatment); BC+CDPs (i) (Cyclodipeptides treatment from the start); BC+CDPs (m) (Cyclodipeptides treatment in advanced cancer); MTX (Methotrexate treatment); BC+CDPs+MTX (m) (Combination of Cyclodipeptides and Methotrexate in advanced cancer).
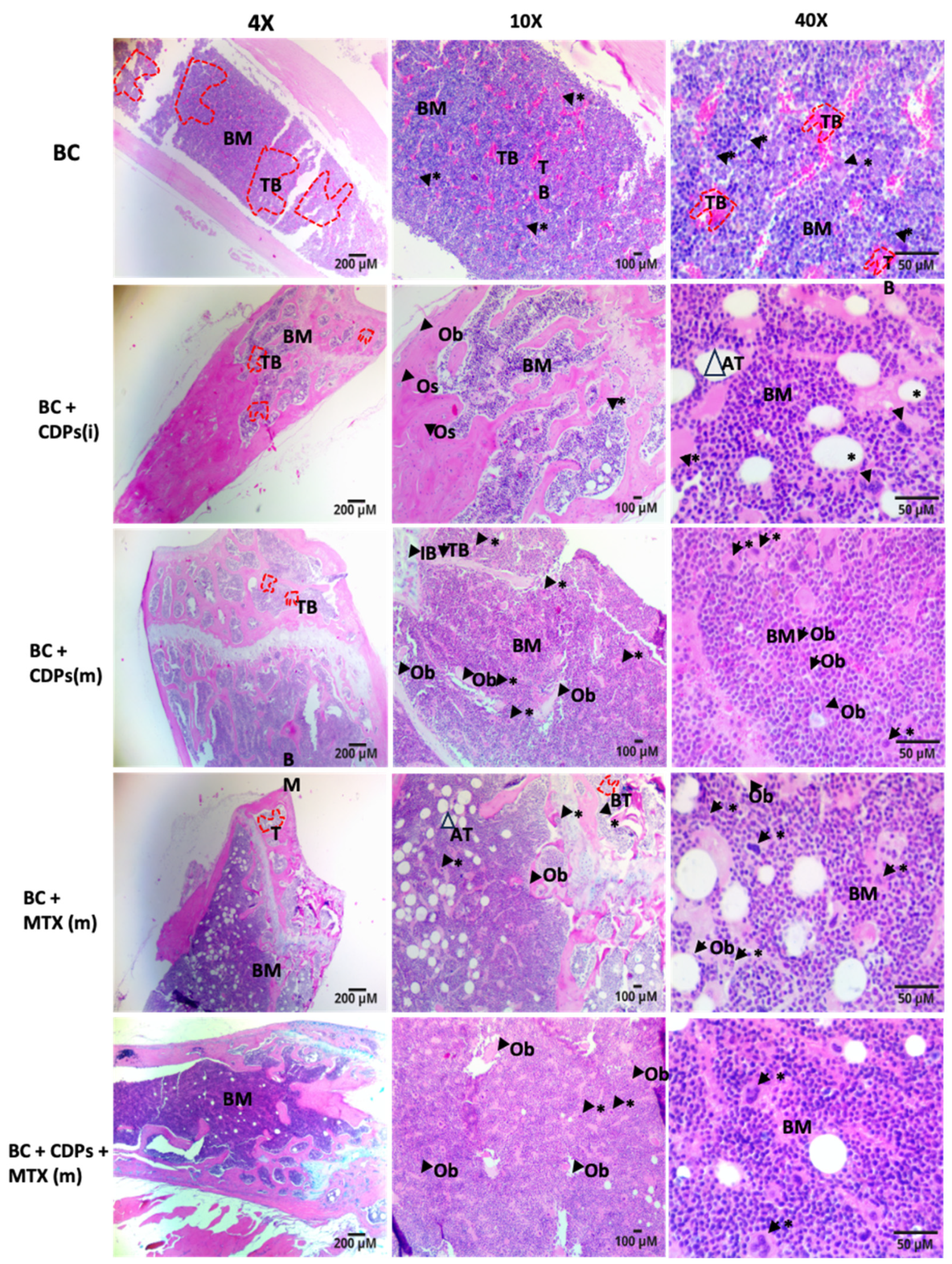
Figure 9.
Effect of CDPs on signaling proteins in tumor xenografted with MDA-MB-231 breast cancer cells in immunosuppressed mice treated with CDPs. Protein extracts obtained from the tumor dissected from the mice groups treated with CDPs (0.1 mg/ml) in function were subjected to immunodetection. Protein expression for the total Akt, phosphorylated Akt, total Gab1, phosphorylated p-Gab1, Total FOX01, and phosphorylates p-FOX01 are shown. Densitometric analyses of the protein immunodetection results are presented on the right. The bars represent the means ± SE, n=3 per group. Statistical analysis was performed using one-way ANOVA, followed by Dunnett's post hoc test; SE values are shown as bars, and significant differences are indicated with different letters (p <0.05).
Figure 9.
Effect of CDPs on signaling proteins in tumor xenografted with MDA-MB-231 breast cancer cells in immunosuppressed mice treated with CDPs. Protein extracts obtained from the tumor dissected from the mice groups treated with CDPs (0.1 mg/ml) in function were subjected to immunodetection. Protein expression for the total Akt, phosphorylated Akt, total Gab1, phosphorylated p-Gab1, Total FOX01, and phosphorylates p-FOX01 are shown. Densitometric analyses of the protein immunodetection results are presented on the right. The bars represent the means ± SE, n=3 per group. Statistical analysis was performed using one-way ANOVA, followed by Dunnett's post hoc test; SE values are shown as bars, and significant differences are indicated with different letters (p <0.05).