Submitted:
10 March 2025
Posted:
11 March 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Period
2.2. Study Hospitals
- Cliniques Universitaires de Lubumbashi (CUL) is a tertiary-level health facility with 211 functional beds out of a total capacity of 230 beds. The ICU, part of the Anesthesia and Intensive Care Medicine Department, has six beds (3% of the hospital’s total capacity) and is staffed by four anesthesiologist-intensivists, four interns, eight nurses, and one auxiliary staff member.
- Hôpital de la Société Nationale des Chemins de Fer du Congo (SNCC) is a semi-public facility primarily serving railway employees but also functioning as a general referral hospital. It has 200 functional beds out of a total of 250 beds, with an ICU comprising eight beds (4% of the hospital’s capacity). The unit operates with one anesthesiologist-intensivist, five nurses, and one auxiliary staff member.
- Clinique Diamant de Lubumbashi (CMDL) is a private hospital with 65 beds, including four beds in the continuous care unit and eight beds in the ICU, representing 12% of the hospital's total capacity. The ICU is managed by eight physicians, including one anesthesiologist-intensivist, and eight nurses.
2.3. Study Population
2.4. Inclusion and Exclusion Criteria
2.4.1. Inclusion Criteria
- Suspected sepsis upon admission or during the ICU stay.
- Age ≥ 16 years, with suspected sepsis or septic shock.
- Hospitalized in the ICU or continuous care unit of the selected hospitals.
2.4.2. Exclusion Criteria
- Age < 16 years.
- Death within 24 hours of hospital admission.
- Pregnancy.
- Readmission for sepsis or septic shock during the study period.
- Lack of informed consent for study participation.
2.5. Sampling Technique
2.6. Data Collection
2.6.1. General Data Collection Process
2.6.2. Demographic and Clinical Data
2.7. Fungal Identification and Susceptibility Testing
2.7.1. Culture
2.7.2. Identification
- Gram staining (to visualize spores, pseudohyphae, or hyphae under ×100 magnification).
- Lactophenol blue staining (to observe fungal structures under ×40 magnification).
- Germ tube test (to differentiate Candida albicans based on germ tube formation without constriction at the base).
- Biochemical testing using the Integral System Yeasts Plus (Liofilchem® ref. 71822).
2.7.3. Antifungal Susceptibility Testing
2.8. Statistical Analysis
2.9. Ethical Considerations
3. Results
3.1. Characteristics of the Study Population
3.2. Clinical and Paraclinical Characteristics of the Patients Studied
3.3. Microbiology
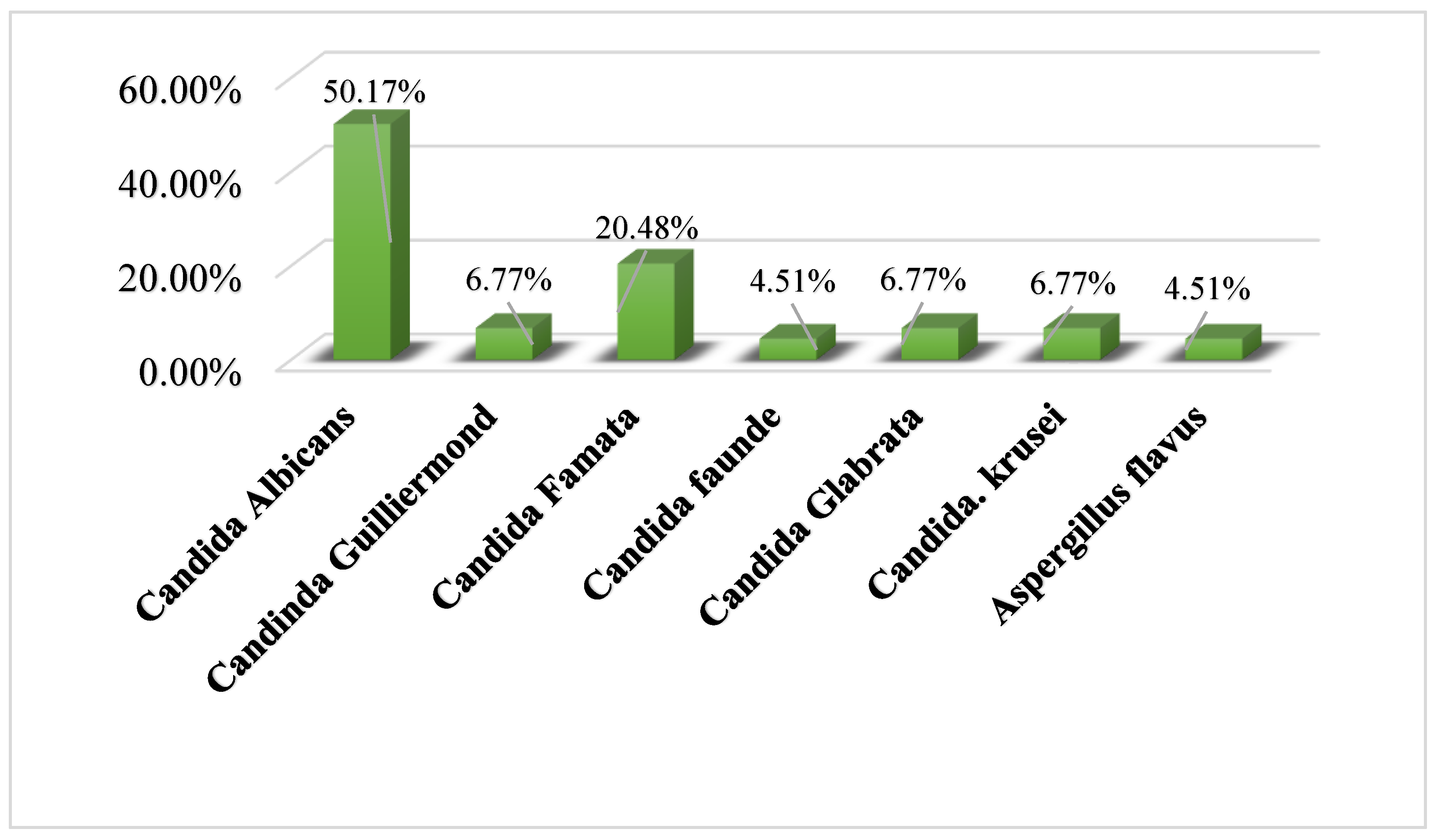
3.3.1. Microorganisms Isolated and Identified after Culture
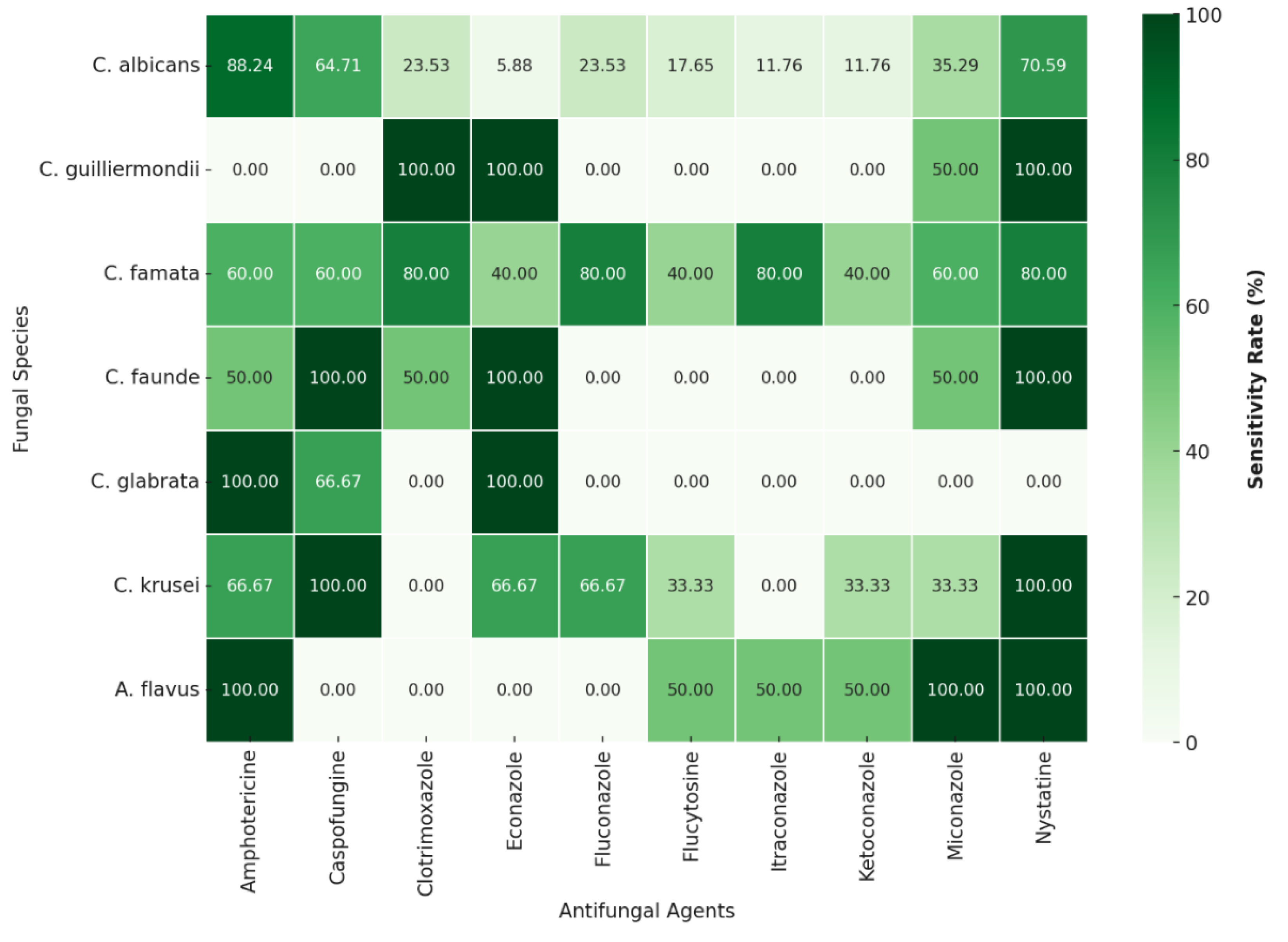
3.3.2. The Antifungal Susceptibility Profile
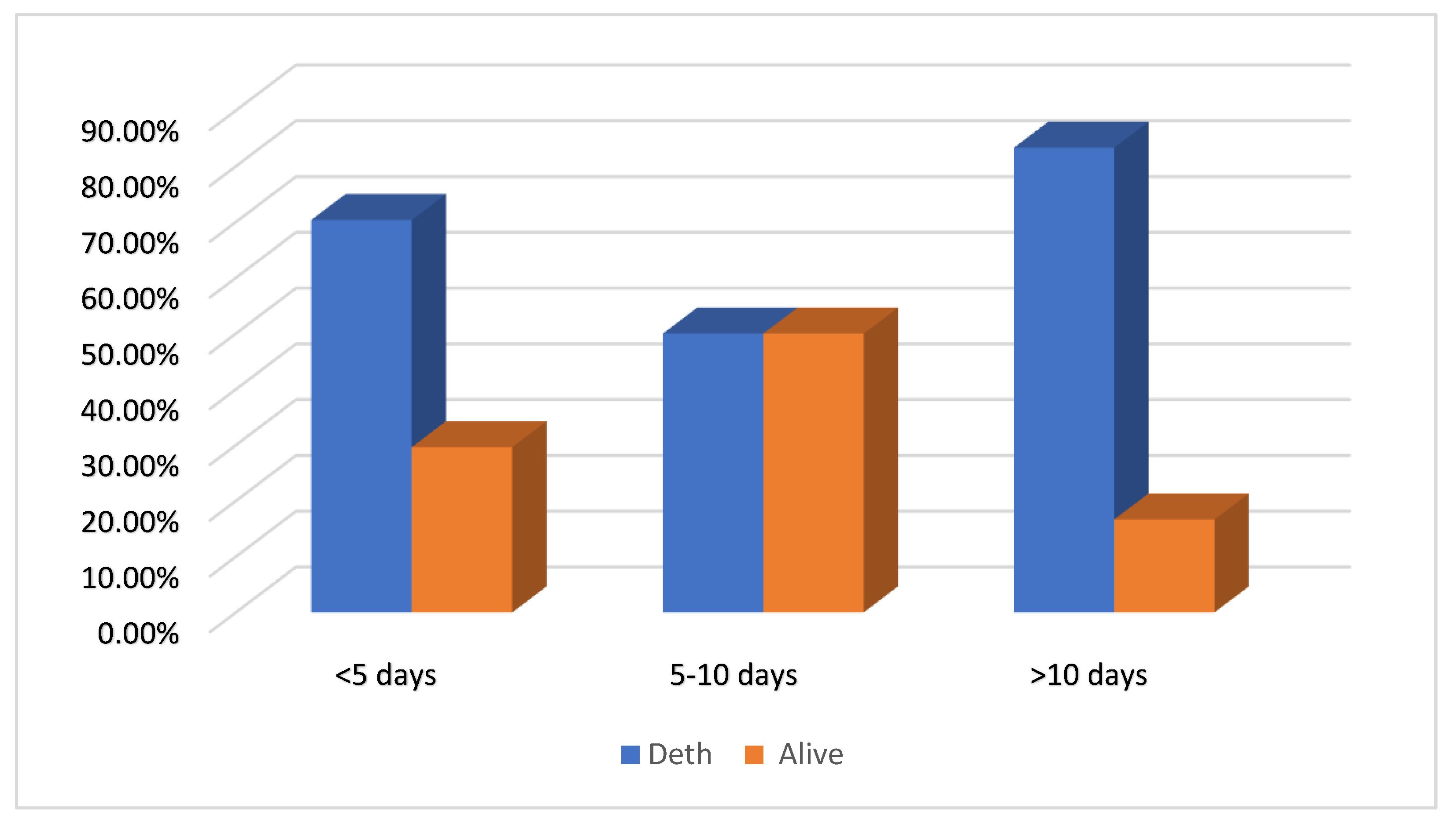
3.3.3. Outcomes
4. Discussion
4.1. Epidemiological Characteristics of Patients
4.2. Clinical Characteristics of the Population
4.3. Microorganisms Identified in Culture
4.4. The Antifungal Susceptibility Profile
4.5. Outcomes
4.6. Limitations of the Study
4.7. Clinical Implications
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Ethics Approval and Consent to Participate
Consent for Publication
Acknowledgments
Conflicts of Interest
References
- Fang F, Zhang Y, Tang J, et al. Association of Corticosteroid Treatment with Outcomes in Adult Patients with Sepsis: A Systematic Review and Meta-analysis. JAMA Intern Med 2019; 179: 213–223.
- Hing Chan JK, Leung YLE. A Retrospective Study on the Compliance with Surviving Sepsis Campaign Guideline in Patients with Sepsis Admitted to Intensive Care Unit in Hong Kong. J Intensive Crit Care 2017; 03: 1–10. [CrossRef]
- Durga CS, Gupta N, Soneja M, et al. Invasive fungal infections in critically ill patients: A prospective study from a tertiary care hospital in India. Drug Discov Ther 2018; 12: 363–367. [CrossRef]
- Azim A, Ahmed A. Diagnosis and management of invasive fungal diseases in non-neutropenic ICU patients, with focus on candidiasis and aspergillosis: a comprehensive review. Front Cell Infect Microbiol 2024; 14: 1–12. [CrossRef]
- Ostrosky-Zeichner L, Al-Obaidi M. Invasive Fungal Infections in the Intensive Care Unit. Infect Dis Clin North Am 2017; 31: 475–487. [CrossRef]
- Soriano A, Honore PM, Puerta-Alcalde P, et al. Invasive candidiasis: current clinical challenges and unmet needs in adult populations. J Antimicrob Chemother 2023; 78: 1569–1585. [CrossRef]
- Sirga S, Bindu KH, MS R, et al. Invasive Fungal Infections in A Teritiary ICU in Hyderabad. Acta Sci Med Sci 2023; 7: 183–191. [CrossRef]
- Bassetti M, Giacobbe DR, Agvald-Ohman C, et al. Invasive Fungal Diseases in Adult Patients in Intensive Care Unit (FUNDICU): 2024 consensus definitions from ESGCIP, EFISG, ESICM, ECMM, MSGERC, ISAC, and ISHAM. Intensive Care Med 2024; 50: 502–515. [CrossRef]
- Xu H, Yu SY, Zhou ML, et al. Epidemiology and antifungal susceptibility patterns of invasive fungal infections from 2012 to 2014 in a teaching hospital in central China. Infect Drug Resist 2019; 12: 3641–3651. [CrossRef]
- Garnacho-Montero J, Barrero-García I, León-Moya C. Fungal infections in immunocompromised critically ill patients. J Intensive Med 2024; 4: 299–306. [CrossRef]
- Dangarembizi R, Wasserman S, Hoving JC. Emerging and re-emerging fungal threats in Africa. Parasite Immunol 2023; 45: 1–13. [CrossRef]
- Arastehfar A, Wickes BL, Ilkit M, et al. Identification of mycoses in developing countries. J Fungi 2019; 5: 1–23. [CrossRef]
- Hassoun N, Kassem II, Hamze M, et al. Antifungal Use and Resistance in a Lower–Middle-Income Country: The Case of Lebanon. Antibiotics 2023; 12: 1–14. [CrossRef]
- Ahmad S, Kumar S, Rajpal K, et al. Candidemia Among ICU Patients: Species Characterisation, Resistance Pattern and Association With Candida Score: A Prospective Study. Cureus 2022; 14: 1–9. [CrossRef]
- Poissy J, Damonti L, Bignon A, et al. Risk factors for candidemia: A prospective matched case-control study. Crit Care 2020; 24: 1–11. [CrossRef]
- Vincent JL, Sakr Y, Singer M, et al. Prevalence and Outcomes of Infection among Patients in Intensive Care Units in 2017. JAMA - J Am Med Assoc 2020; 323: 1478–1487. [CrossRef]
- Bongomin F, Fayemiwo SA. Epidemiology of fungal diseases in Africa : A review of diagnostic drivers. Curr Med Mycol 2021; 7: 63–70. [CrossRef]
- Rajasingham R, Smith RM, Park BJ, et al. Global burden of disease of HIV-associated cryptococcal meningitis : an updated analysis. Lancet Infect Dis 2017; 17: 873–881. [CrossRef]
- Negm EM, Mowafy SMS, Mohammed AA, et al. Antibiograms of intensive care units at an Egyptian tertiary care hospital. Egypt J Bronchol 2021; 15: 1–15.
- Kamwiziku GK, Makangara JCC, Orefuwa E, et al. Serious fungal diseases in Democratic Republic of Congo – Incidence and prevalence estimates. Mycoses 2021; 64: 1159–1169. [CrossRef]
- Boussina A, Ramesh K, Arora H, et al. Differentiation of Fungal , Viral , and Bacterial Sepsis using Multimodal Deep Learning. medRxiv Prepr 2023; 10: 1-ç. doi:. [CrossRef]
- Brooks D, Polubothu P, Young D, et al. Sepsis caused by bloodstream infection in patients in the intensive care unit: the impact of inactive empiric antimicrobial therapy on outcome. J Hosp Infect 2018; 98: 369–374. [CrossRef]
- Akilimali A, Oduoye MO, Balume A, et al. Antimicrobial use and resistance in Democratic Republic of Congo: Implications and recommendations; A mini review. Ann Med Surg 2022; 80: 104183. [CrossRef]
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med 2021; 47: 1181–1247. [CrossRef]
- Boonstra JM, Märtson AG, Sandaradura I, et al. Optimization of fluconazole dosing for the prevention and treatment of invasive candidiasis based on the pharmacokinetics of fluconazole in critically ill patients. Antimicrob Agents Chemother 2021; 65: 1–11. [CrossRef]
- Al-Ahmadey ZZ, Al-Ahmadi SS, Aljohani ED, et al. Candida Bloodstream Infection and Antifungal Susceptibility Over Three Years in a Single Center from Medinah, Saudi Arabia. Microbiol Res J Int 2023; 33: 1–7. [CrossRef]
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016; 315: 801–810.
- Singh G, Pitoyo CW, Aditianingsih D, et al. Risk factors for early invasive fungal disease in critically ill patients. Indian J Crit Care Med 2016; 20: 633–639. [CrossRef]
- Singh T, Kashyap A, Ahluwalia G, et al. Epidemiology of fungal infections in critical care setting of a tertiary care teaching hospital in North India: A prospective surveillance study. J Clin Sci Res 2014; 3: 14. [CrossRef]
- Rodriguez L, Bustamante B, Huaroto L, et al. A multi-centric study of Candida bloodstream infection in Lima-Callao, Peru: Species distribution, antifungal resistance and clinical outcomes. PLoS One 2017; 12: 1–12. [CrossRef]
- Ragunathan L, Poongothai GK, Sinazer AR, et al. Phenotypic characterization and antifungal susceptibility pattern to fluconazole in Candida species isolated from vulvovaginal candidiasis in a tertiary care hospital. J Clin Diagnostic Res 2014; 8: 1–4. [CrossRef]
- vom Steeg LG, Klein SL. SeXX matters in infectious disease pathogenesis. PLoS Pathog 2016; 12: 1–6. [CrossRef]
- Rayens E, Rayens MK, Norris KA. Demographic and Socioeconomic Factors Associated with Fungal Infection Risk, United States, 2019. Emerg Infect Dis 2022; 28: 1955–1969. [CrossRef]
- Ahn YH, Lee J, Oh DK, et al. Association between the timing of ICU admission and mortality in patients with hospital-onset sepsis: a nationwide prospective cohort study. J Intensive Care 2023; 11: 1–9. [CrossRef]
- Driessen RGH, Heijnen NFL, Hulsewe RPMG, et al. Early ICU-mortality in sepsis–causes, influencing factors and variability in clinical judgement: a retrospective cohort study. Infect Dis (Auckl) 2021; 53: 61–68. [CrossRef]
- Wójtowicz A, Tissot F, Lamoth F, et al. Polymorphisms in tumor necrosis factor-α increase susceptibility to intra-abdominal Candida infection in high-risk surgical ICU patients. Crit Care Med 2014; 42: 304–308. [CrossRef]
- Rafat Z, Hashemi SJ, Ashrafi K, et al. Epidemiology, laboratory diagnosis and clinical aspects of fungal pulmonary infections in 384 patients hospitalized in pulmonary units in Guilan province, Iran. Iran J Microbiol 2020; 12: 353–363. [CrossRef]
- Li Z, Lu G, Meng G. Pathogenic fungal infection in the lung. Front Immunol 2019; 10: 1–20. [CrossRef]
- Ruan H, Zhang Q, Zhang YP, et al. Unraveling the role of HIF-1α in sepsis: from pathophysiology to potential therapeutics—a narrative review. Crit Care 2024; 28: 1–15. [CrossRef]
- Pavez N, Kattan E, Vera M, et al. Hypoxia-related parameters during septic shock resuscitation: Pathophysiological determinants and potential clinical implications. Ann Transl Med 2020; 8: 784–784. [CrossRef]
- Metoto Mbengo JA, Noutakdie Tochie J, Ndom Ntock F, Nzouango JB KS, NgonoAteba G, Tocko, C, Colibaly A, Beyiha G ZMJ. The Epidemiology, Therapeutic Patterns, Outcome, and Challenges in Managing Septic Shock in a Sub-Saharan African Intensive Care Unit: A Cross- Sectional Study. Hosp Pr Res 2019; 4: 117–121. [CrossRef]
- Al Omar S, Alshraideh JA, Khassawneh B, et al. The Prevalence of Sepsis and Septic Shock in a Middle-Income Country: Experience of Two Tertiary Hospitals in Jordan. J Crit Intensive Care 2021; 12: 75–79. [CrossRef]
- panelJin Zhu , Yanyan Dong , Pengda Liao , Xin Yin , Jianzhuo He LG. Prognostic value of hemoglobin in patients with sepsis: A systematic review and meta-analysis. Hear Lung 2024; 64: 93-çç.
- Zhong L, Zhong Y, Chen W, et al. Association between haemoglobin-to-red blood cell distribution width ratio at admission and all-cause mortality in adult patients with sepsis in an intensive care unit: a secondary analysis of the MIMIC-IV database. BMJ Open 2024; 14: 1–10. [CrossRef]
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 2017; 43: 304–377.
- Evaluation and management of severe sepsis and septic shock in adults. Updat Wolters Kluwer 2021; Gregory A: 1–22.
- Bagshaw RAKBLGM. Sepsis-Associated Acute Kidney Injury. Semin Nephrol 2015; 35: 2–11. [CrossRef]
- Manrique-Caballero CL, Del Rio-Pertuz G, Gomez H. Sepsis-Associated Acute Kidney Injury. Crit Care Clin 2021; 37: 279–301. [CrossRef]
- Tsegaye EA, Teklu DS, Bonger ZT, et al. Bacterial and fungal profile, drug resistance pattern and associated factors of isolates recovered from blood samples of patients referred to Ethiopian Public Health Institute: cross-sectional study. BMC Infect Dis 2021; 21: 1–10. [CrossRef]
- Lewis JM, Feasey NA, Rylance J. Aetiology and outcomes of sepsis in adults in sub-Saharan Africa : a systematic review and meta-analysis. 2019; 23: 1–11. [CrossRef]
- Delaloye J, Calandra T. Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence 2014; 5: 154–162. [CrossRef]
- Dasgupta S, Das S, Chawan NS, et al. Nosocomial infections in the intensive care unit: Incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med 2015; 19: 14–20. [CrossRef]
- Zeng ZR, Tian G, Ding YH, et al. Surveillance study of the prevalence, species distribution, antifungal susceptibility, risk factors and mortality of invasive candidiasis in a tertiary teaching hospital in Southwest China. BMC Infect Dis 2019; 19: 1–12. [CrossRef]
- Calandra T, Roberts JA, Antonelli M, et al. Diagnosis and management of invasive candidiasis in the ICU: An updated approach to an old enemy. Crit Care 2016; 20: 4–9. [CrossRef]
- Dabas Y, Xess I, Pandey M, et al. Epidemiology and Antifungal Susceptibility Patterns of Invasive Fungal Infections (IFIs) in India: A Prospective Observational Study. J Fungi 2022; 8. [CrossRef]
- Seyoum E, Bitew A, Mihret A. Distribution of Candida albicans and non- albicans Candida species isolated in different clinical samples and their in vitro antifungal suscetibity profile in Ethiopia. BMC Infect Dis 2020; 20: 1–9. [CrossRef]
- Guinea J. Global trends in the distribution of Candida species causing candidemia. Clin Microbiol Infect 2014; 20: 5–10. [CrossRef]
- Hernández-Pabón JC, Tabares B, Gil Ó, et al. Candida Non-albicans and Non-auris Causing Invasive Candidiasis in a Fourth-Level Hospital in Colombia: Epidemiology, Antifungal Susceptibility, and Genetic Diversity. J Fungi 2024; 10: 326. [CrossRef]
- Meradji A, Ranque S, Bachtarzi F, et al. Incidence, Species Distribution, and Antifungal Susceptibility of Candida Bloodstream Infections in a Tertiary Algerian Hospital. Biol Life Sci Forum 2024; 31: 1–7. [CrossRef]
- Guo LN, Yu SY, Xiao M, et al. Species distribution and antifungal susceptibility of invasive candidiasis: A 2016-2017 multicenter surveillance study in beijing, china. Infect Drug Resist 2020; 13: 2443–2452. [CrossRef]
- Xiao Z, Wang Q, Zhu F, et al. Epidemiology, species distribution, antifungal susceptibility and mortality risk factors of candidemia among critically ill patients: A retrospective study from 2011 to 2017 in a teaching hospital in China. Antimicrob Resist Infect Control 2019; 8: 1–7. [CrossRef]
- Soulountsi V, Schizodimos T, Kotoulas SC. Deciphering the epidemiology of invasive candidiasis in the intensive care unit: is it possible? Infection 2021; 49: 1107–1131. [CrossRef]
- Nascimento T, Guerreiro D, Toscano C. Insights into Candida Colonization in Intensive Care Unit Patients : A Prospective Multicenter Study. Fungi 2024; 10: 1–13.
- Riera FO, Caeiro JP, Angiolini SC, et al. Invasive Candidiasis: Update and Current Challenges in the Management of This Mycosis in South America. Antibiotics 2022; 11: 1–16. [CrossRef]
- Al-Dorzi HM, Sakkijha H, Khan R, et al. Invasive Candidiasis in Critically Ill Patients: A Prospective Cohort Study in Two Tertiary Care Centers. J Intensive Care Med 2020; 35: 542–553. [CrossRef]
- Badiee P, Badali H, Boekhout T, et al. Antifungal susceptibility testing of Candida species isolated from the immunocompromised patients admitted to ten university hospitals in Iran: Comparison of colonizing and infecting isolates. BMC Infect Dis 2017; 17: 1–8. [CrossRef]
- Bilal H, Shafiq M, Hou B, et al. Distribution and antifungal susceptibility pattern of Candida species from mainland China: A systematic analysis. Virulence 2022; 13: 1573–1589. [CrossRef]
- Brunetti G, Navazio AS, Giuliani A, et al. Candida blood stream infections observed between 2011 and 2016 in a large Italian University Hospital: A time-based retrospective analysis on epidemiology, biofilm production, antifungal agents consumption and drug-susceptibility. PLoS One 2019; 14: 1–17. [CrossRef]
- Bassetti M, Vena A, Bouza E, et al. Antifungal susceptibility testing in Candida, Aspergillus and Cryptococcus infections: are the MICs useful for clinicians? Clin Microbiol Infect 2020; 26: 1024–1033. [CrossRef]
- Aldardeer NF, Albar H, Al-Attas M, et al. Antifungal resistance in patients with Candidaemia: A retrospective cohort study. BMC Infect Dis 2020; 20: 1–7. [CrossRef]
- Ruiz-rodriguez M. Sepsis : A Review of Advances in Management. 2017; 2393–2411. [CrossRef]
| N=33 | % | |
|---|---|---|
| Age | ||
| 16-39 years old | 12 | 36.4 |
| 40-60 years old | 9 | 27.2 |
| ˃60 years | 12 | 36.4 |
| Middle Ages | 49.14±22.29 years | |
| Sex | ||
| F | 14 | 42.4 |
| M | 19 | 57.6 |
| Origin | ||
| Surgery | 2 | 6.1 |
| Internal Medicine | 2 | 6.1 |
| Neurology | 2 | 6.1 |
| CS Transfer | 16 | 48.5 |
| Emergency room | 9 | 27.3 |
| Admission time | ||
| ˃7 | 10 | 33.3 |
| ≤7 | 23 | 69.7 |
| Patient Type | ||
| Surgical | 6 | 18.2 |
| Gyneco-Obstétrical | 3 | 9.1 |
| Medical | 24 | 72.7 |
| Comorbidity (%) | |
|---|---|
| Alcohol | 6 |
| COPD | 6 |
| Cancer | 6 |
| C.puerperal | 9 |
| Diabetes | 15.5 |
| HTA | 24 |
| Obesity | 3 |
| Sinusitis | 3 |
| Site d’infection (%) | |
| Digestive | 3 |
| Pulmonary | 60 |
| Genitourinary | 67 |
| Undetermined | 3 |
| Multisite | 58 |
| Vital Signs at Presentation | |
| Score de Glasgow (%) | 11.24±2.9 |
| Oxygen saturation (%) | 90.03±10.2 |
| Temperature (°C) | 36.788±1.5 |
| Systolic blood pressure (mmHg) | 116.56±392 |
| Diastolic blood pressure (mmHg) | 69,62±22,2 |
| Mean arterial pressure (mmHg) | 82.7±24.5 |
| Heart rate (beats/min) | 109.12±20.5 |
| Respiratory rate (breathing/min) | 29.39±8.2 |
| Laboratory baseline values | |
| Hémoglobine(g/dl) | 10.69 ± 2.45 |
| Haematocrit | 32.27 ± 8.43 |
| Globules blancs ( /mm3) | 15013.64±6273.5 |
| Inserts ( /mm3) | 1152575.76±116595.5 |
| Serum creatinine (mg/dl) | 4.03±3.9 |
| Natremia(mEq/l) | 139.37±7.2 |
| Kaliemia (mEq/l) | 4±0.867 |
| Lactate (mEq/l) | 3.80 ± 3.531 |
| Blood urea (mg/dl) | 37.03 ± 26.29 |
| Bilirubine totale (mg/dl) | 3.08 ± 5.2 |
| PaCO2 (mmHg) | 38.31 ± 12.6 |
| Arterial Blood pH | 7.37 ± 0.16 |
| PaO2 / FiO2 | 232.9 ± 122.64 |
| Glycémie (mg/dl) | 183.32±146.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





