1. Introduction
Although congenital cataract is a rare disease, it is one of the most common causes of blindness in children worldwide [
1]. Early surgery is considered essential in the treatment but is challenging for several reasons, including a high incidence and variety of associated comorbidities, the small size of the eyes and the differing behavior of tissues compared to adult eyes [
2]. In particular, the high elasticity of the lens capsule in children makes manual creation of the capsulorhexis more demanding and is associated with an enlargement and an increased risk of capsule tears [
3].
At the same time, a precise diameter and continuous circularity of the capsulorhexis is crucial to prevent capsular contraction, influences the position of the implanted intraocular lens (IOL) and hence stability of the postoperative refraction [
4,
5]. Especially when implanting a bag-in-the-lens IOL (BIL IOL; Morcher GmbH, Stuttgart, Germany) the accuracy of the capsulorhexis diameter and the integrity of the rhexis edge are important [
6,
7,
8].
In this context, the use of a femtosecond laser (FS-laser) can contribute to the accuracy of the capsulotomy while decreasing the number of intraocular manipulations [
9,
10]. Numerous studies of Femtosecond-laser-assisted cataract surgery (FLACS) in adult patients have shown that capsulotomies created by FS-lasers are precise, predictable, reproducible, allow better IOL centration and minimize the occurrence of surgically induced capsule tears [
9,
11,
12,
13,
14,
15,
16]
Clinical data related to the use of FLACS in children is limited [
17,
18,
19]. Despite the paucity of available data, femtosecond lasers have been used off-label in cataract surgery in children. Since 2020, the Femto LDV Z8 femtosecond laser is the only FS-laser system approved for capsulotomy and laser phacofragmentation in pediatric cataract surgery. It is also the only laser used in cataract surgery using low pulse energies in the nanojoule (nJ) range [
13,
20].
The aim of this study is to obtain prospective data on the safety and performance of the mobile, low-energy FS-laser Femto LDV Z8 for cataract surgery in children and to evaluate the applicability of the Bochum formula for capsulotomy diameter calculation.
2. Materials and Methods
This consecutive prospective case series was conducted at the Ophthalmology Department of the Antwerp University Hospital, Edegem Belgium (NCT05241756) in accordance with the tenets of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the University of Antwerpen (Edge 001299; 17 January 2022). Written informed consent was obtained from the patient's legal representatives and from the child when aged > 6 years old.
The study recruited and consecutively operated on children under the age of 18 who underwent lens surgery between January and July 2022. Criteria for exclusion were eyes with corneal diameter < 9 mm, a hazy cornea, or pregnancy. All children underwent preoperative and postoperative ophthalmological examinations including anterior segment biomicroscopy, refraction, eye fundus evaluation, and biometry (either optical biometry or a combination of keratometry and A-scan ultrasound in younger children). In case of insufficient cooperation, the ophthalmological examination was performed under general anesthesia directly prior to the surgery.
All surgeries were performed by one of two experienced pediatric cataract surgeons (LVO and MJT). The surgery was performed under general anesthesia with constant supervision of an anesthesiologist. After successful docking of the surgical equipment to the patient eye, anterior capsulotomy was performed with the FS-laser system, followed by complete aspiration of the contents of the lens, manual posterior capsulorhexis, and implantation of a BIL IOL. Apart from the laser capsulotomy and the verification of the capsulotomy size, the surgeries followed the standard pediatric BIL protocol [
8].
The programmed capsulotomy diameter was between 2.3 and 2.9 mm. Calculation was based on the targeted capsulotomy diameter and the Bochum formula [
18], to account for the enlargement of the capsulotomy in children due to the high elasticity of the lens capsule. The achieved capsulotomy diameter was measured intraoperatively using the Morcher ring caliper Type 4L (Morcher, Germany). This ring-shaped device with an internal diameter of 4.5 mm was inserted into the eye after creation of the capsulotomy and after injecting an ophthalmic viscosurgical device into the anterior chamber. This provides an immediate clinical impression of the real obtained size of the capsulotomy. To calculate the true size of the achieved capsulotomy, we extracted a still from the video documentation of the surgeries. Knowing the size of the caliper enabled us to calculate the achieved capsulotomy size using a rule of three. This method thus avoids any influence of the corneal curvature on the measurement of the capsulotomy size.
In order to assess the safety of the procedure (the study`s primary objective), any adverse event (AE) related to the surgery or any ophthalmic AE at 1 day, 1 week, 1 month, and 6 months postoperatively was documented.
The analyzed data set comprised all eyes with successful docking of the FS-laser. All statistical analyses were exploratory, and there were no predefined hypotheses. Statistical analysis was performed using Microsoft Excel 365 for data entry, organisation and structuring and the Data Analysis ToolPak for descriptive statistics and regression analysis. Regression analysis was used to describe the extent to which the capsulotomy enlargement factor was age dependent. To test the correlation between the patients` age and the capsulotomy enlargement factor, the Pearson correlation coefficient (r) was used. A P-value < 0.001 was considered statistically significant.
3. Results
The mean (SD) age of patients in the analysis set was 3.10 ± 2.38 years, the median age was 4 years (range 4 months to 8 years).
Table 1 shows demographic data and comorbidities of the patients as well as eye characteristics.
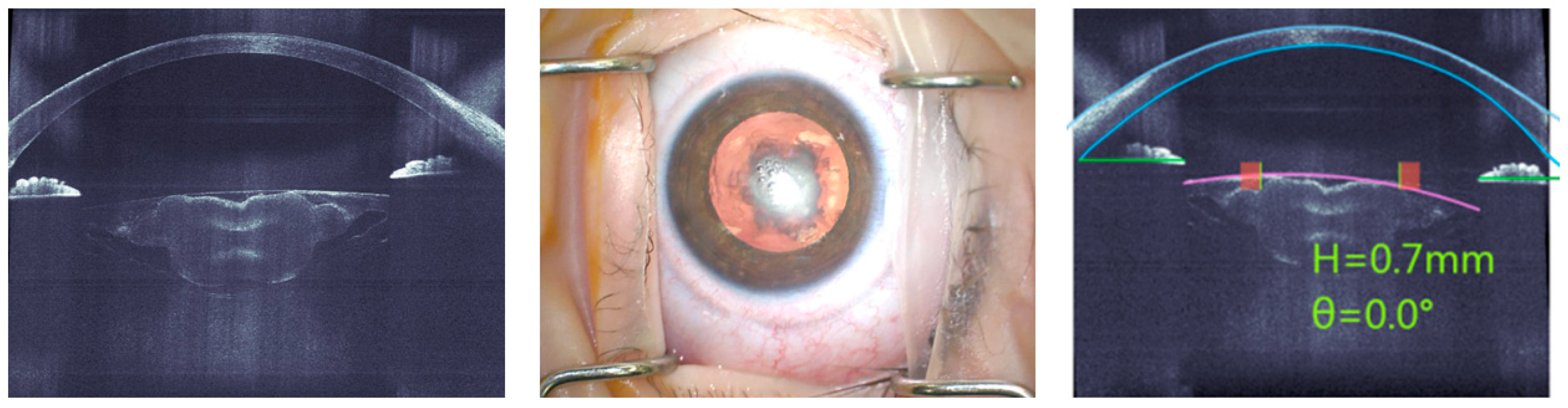
Due to small lid opening of the children’s eyes, very flat or steep cornea, and a bleb after glaucoma surgery, docking issues with the standard disposable attachment interface occurred in eight eyes of seven patients (in median 1.17 years; range 4 months to 17 years), and surgery was successfully completed manually. In all 13 eyes (10 patients) with completed docking, the anterior segment was immediately successfully imaged by the high-resolution spectral-domain optical coherence tomography (SD-OCT) of the FS-laser. The margins of the cornea and the lens capsule were automatically identified and displayed together with the planned capsulotomy diameter and the suggested position at the center of the pupil (
Figure 1). Manual adjustments were not necessary in any case. A well-centered and entirely circular anterior capsulotomy was successfully performed with the FS-laser in all eyes of the analysis set.
Figure 1 shows the case of a 7-month-old child with unilateral cataract, central lens opacity and large posterior plaque, which was overlying a pre-existing posterior capsule defect in the context of anterior vitreolenticular interface dysgenesis. The OCT image shows the central location and inhomogeneity of the lens opacity. As the capsulotomy was created with the FS-Laser, the anterior capsule did not require staining, which would have been necessary with a manual capsulorhexis.
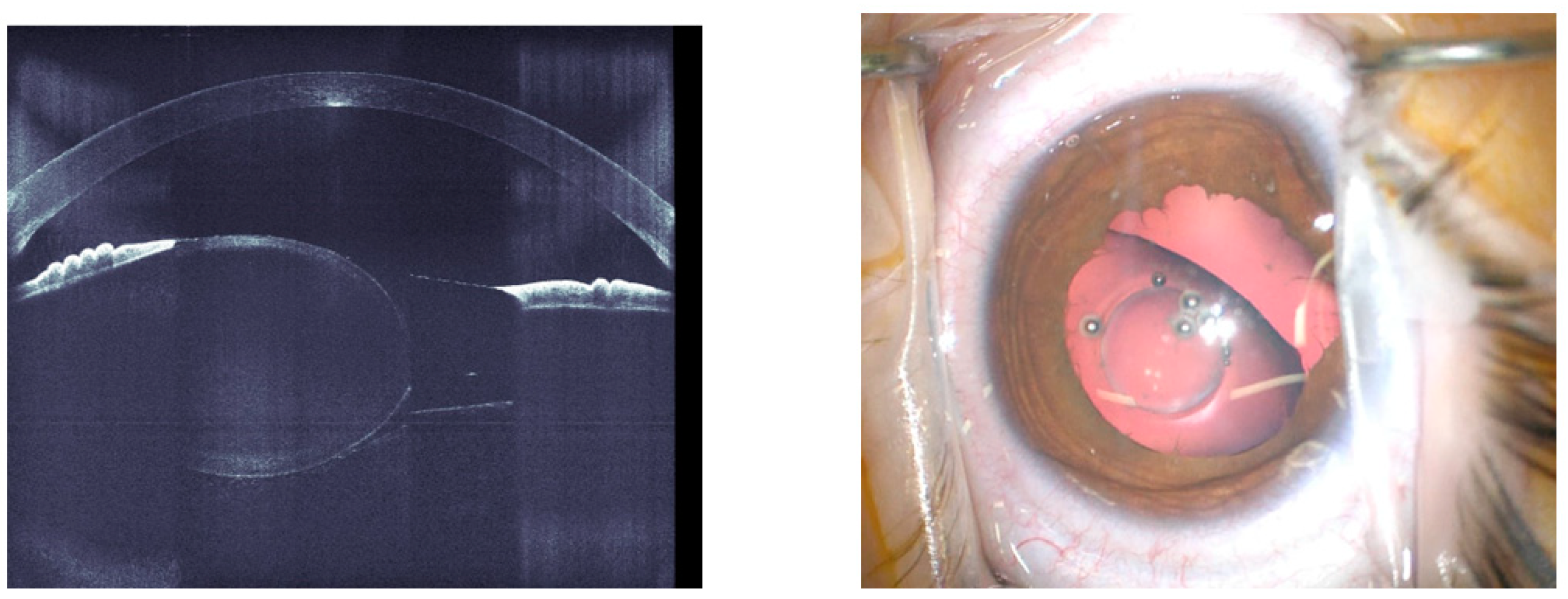
Even in the three eyes with lens subluxation, the FS-laser easily allowed for the creation of a capsulotomy.
Figure 2 shows the case of a 6-year-old child with unilateral familial lens subluxation. The OCT (left) illustrates the dislocation as well as the increased convexity of the lens due to the weak zonules. The intra-operative microscope image shows the capsulotomy with a small diameter of 3 mm which was created by the FS-laser. Through this small capsulotomy, the lens material could be removed by irrigation and aspiration. Afterwards, a capsule tension ring was inserted into the capsular bag and the capsulotomy was manually enlarged to 4.8 mm, which was needed for a BIL implantation. After creation of an equally sized posterior rhexis, the BIL was positioned. To further improve stability, two bean shaped ring segments (Morcher GmbH, Stuttgart, Germany) were inserted in the sulcus and the peripheral groove of the BIL and centration was enhanced with a Prolene 6/0 Loop fixed to the sclera. The technique has already been described in detail [
21]. In one eye with anterior capsule fibrosis, minimal tissue bridges were resolved manually with micro forceps. In three eyes, a small anterior capsular tear developed during the positioning of the BIL IOL, however, IOL implantation was successfully completed in all cases, with a stable IOL position at the end of the surgery. No clinically relevant FS-laser-related complications or ocular AEs were observed up to the end of the 6-month follow-up period. In particular, excessive shrinkage of the capsule, retinal detachment or unusual inflammation were not identified. All eyes were successfully implanted with a BIL IOL.
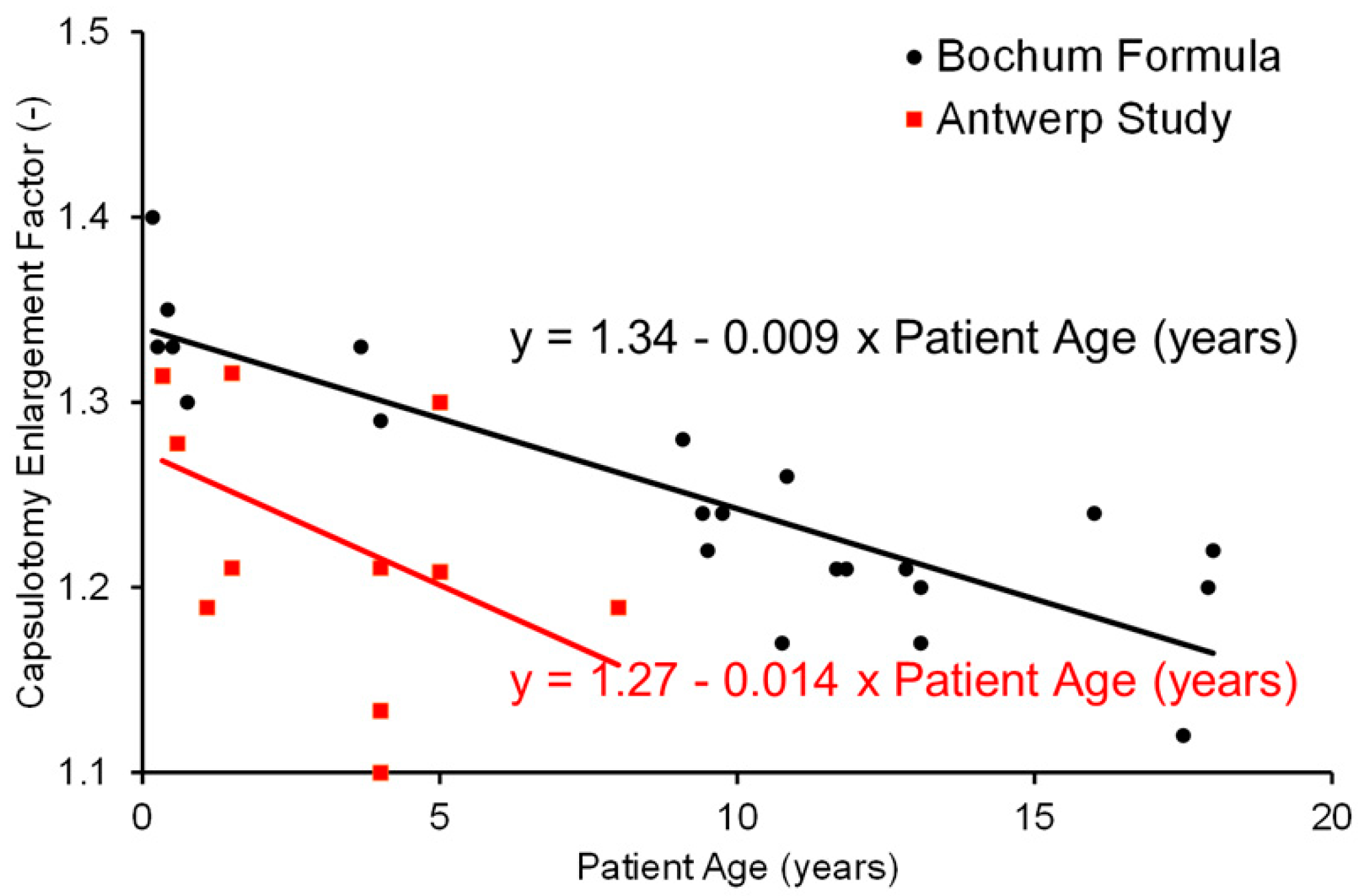
Immediately after FS-laser treatment, all eyes showed symmetrical enlargement of the anterior capsulotomy. The linear bivalent regression resulted in the following formula in our analysis set: 1.27 – 0.014 x patient age.
Figure 3 shows the enlargement factor in relation to patient age in this study compared to the data of the study by Dick et al. [
18]. The large variability in the data associated with the calculated age dependent capsulotomy enlargement factor is demonstrated by the weak r2 coefficient of 0.2356.
Calculation of the Pearson correlation was used to assess the applicability of the age dependence of the Bochum formula for calculating the capsulotomy diameter to be entered into the Femto LDV Z8 (
Table 2) [
18].
Other formulas have been proposed taking into account measured physical properties of the eye to calculate the enlargement factor. Liao et al. [
22] proposed a relationship between the anterior chamber depth and the axial length to predict the capsulorhexis enlargement factor. While there was only a very weak correlation between patient`s age or physical properties of the eye and the enlargement factor of Liao et al [
22], also the analysis with the new data from this study confirmed the strong correlation between age and the enlargement factor of the Bochum formula suggested by Dick et al. 2015.
4. Discussion
This study represents the first prospective analysis of FLACS in children utilizing the sole FS-laser system approved for this purpose, the Femto LDV Z8. Our findings demonstrate that using this low-energy FS-laser to create the anterior capsulotomy for lens surgery in children is safe. In all cases, a precise, accurately positioned, and perfectly circular capsulotomy was created by the FS-laser after successful docking.
Cataract surgery in children presents a unique set of challenges due to the highly variable anatomical situations and comorbidities, including amongst others a fibrotic lens capsule, lens luxation or a narrow anterior chamber [
2]. In these cases, the use of the FS-laser has already been shown to be advantageous in adults and contributed to greater safety in the clinical outcome and precision in the capsulotomy cut [
14,
15]. This is also confirmed by our case series in children.
In the three cases of lens luxation a precise capsulotomy was created reliably and with less manipulation using the FS-laser. Manual capsulorhexis in eyes with lens luxation or Marfan syndrome can be a major challenge and carries risks, as unstable zonules and varying vector forces make the manual preparation procedure unpredictable [
23]. In these cases, in particular, the use of the FS-laser for capsulotomy can contribute to greater safety and standardization of the clinical procedure. Creating a small capsulotomy with the FS-laser allows for removal of the lens tissue and subsequent positioning of a capsular tension ring in the capsular bag. This balances the tractional forces to a certain extent and facilitates enlarging the capsulotomy and improving centration.
Another common challenge in pediatric lens surgery is the presence of anterior capsule fibrosis [
24], which often makes manual capsulorhexis considerably more difficult and complex. In contrast, in our case of anterior capsule fibrosis, a completely circular and well-centered capsulotomy could be achieved with the FS-laser, and any remaining minimal tissue bridges were removed with minimal effort. In pediatric cataract surgery, staining of the anterior capsule is often necessary due to dense opacities and also to reduce the elasticity of the capsule to some extent. Using the FS-laser for anterior capsulotomy eliminates the need for staining and its potential negative effects.
In three eyes, slight capsular tears occurred during BIL-IOL implantation, which however did not affect the IOL implantation. This might be related to the smaller capsulotomy diameter in combination with the implantation of the BIL-IOL. Due to the enlargement factor given by the elasticity of the lens capsules in young eyes, the actual capsulotomy diameters cut with the laser were consistently smaller than in adults. At the same time, when positioning the BIL-IOL, a certain tension is exerted on the edge of the capsulotomy. This is usually not a critical step due to the high elasticity of the capsule, but can lead to a capsular tear if there is a small irregularity.
With regard to the calculation of capsulotomy size, our results confirm that there is an enlargement of the capsulotomy compared to the size that has been put into the FS-laser device. Despite the large variability in the data, the trends are consistent with the previous reported findings that younger children exhibit a greater capsulotomy enlargement and that an enlargement factor can be used to calculate the targeted capsulotomy diameter. The age dependence of the enlargement factor might be explained by the higher elasticity of the capsule in pediatric eyes [
18]. Another factor that might contribute is the maturation of the zonular fibers, that may present individual variations in length and strength and as a result may show variations in tensile forces exerted by them on the capsule and thus the enlargement effect on the capsulotomy [
25].
While the formula of Liao et al., which was determined for children aged 2-6 years based on anatomical parameters, only showed a very weak correlation of the enlargement factor with age (
Table 2) [
22], the Bochum formula also demonstrated an age-dependent enlargement factor. Accordingly, the use of a formula such as the Bochum formula with an age-dependent enlargement factor appears to be necessary for calculating the achieved capsulotomy diameter for the FEMTO LDV Z8. However, the younger population in this new data sample as compared to the population analyzed in Bochum [
18] does not permit a conclusion of whether the magnitude of the enlargement factor is appropriate over the wider age range reported in the determination of the Bochum formula.
Our results indicate a trend towards a smaller enlargement factor as compared to the Bochum formula, even though a higher enlargement factor could have been expected given the younger population in our study. Several factors could be influencing this, such as type of cataract, other lens characteristics or laser parameters that could influence the capsulotomy edge. Furthermore, because of the importance of capsulotomy size in BIL implantation, we preferred to rather end up with a slightly smaller capsulotomy than to risk a capsulotomy which would be too large. Further studies are necessary to substantiate this trend in a larger sample and to determine a more exact enlargement factor that is applicable for the FEMTO LDV Z8.
The Z8 is a femtosecond laser system which, thanks to its mobility and small footprint, enables operations to be performed without having to significantly change operating room workflows in terms of space and equipment, so that existing workflows are maintained [
13]. The mobility of the Z8 was particularly advantageous for these very young patients under general anesthesia, as the children did not have to be moved for the procedure, but could be operated on as usual. Although docking with the standard interface was not possible in some children of this first case series at our clinic, an improved docking rate is expected with increasing surgical experience in using the device. In general, it may be advisable for surgeons to gain initial experience with the FS-laser in adults before applying it to children.
During the 6-month follow-up time within this study, no ocular AE were registered. There were no cases of increased eye pressure related to the procedure, and there were no cases with an increased inflammatory postoperative reaction. The absence of postoperative inflammation might be related to the low-energy setting of this type of FS-laser [
15,
26].
Limitations of this prospective case series include the lack of a control group with manual cataract surgery, the small number of eyes in the data sample size, the exploratory data analysis without testing an existing hypothesis. Nevertheless, this study provides important prospective data on the safety and efficacy of cataract surgery with the FEMTO LDV Z8 in children. In the future, the possibility of posterior capsulotomy with the low-energy FS-laser could also be investigated.
5. Conclusions
FS-laser-assisted pediatric cataract surgery with the low-energy FS laser was safe to perform and contributed to enhanced reliability and easier surgical feasibility in often challenging lens surgery in children. The age dependency of the capsulotomy diameter enlargement factor was confirmed, which might be related to the higher capsular elasticity in pediatric eyes
Author Contributions
Conceptualization, LVO and MJT; methodology, LVO and MJT.; software, IDB; validation, LVO and MJT; formal analysis, LVO; investigation, LVO, IDB, MT and MJT.; resources, IDB, MT.; data curation, IDB, LVO.; writing—original draft preparation, LVO.; writing—review and editing, LVO, IDB, MT and MJT.; visualization, LVO.; supervision, MJT.; project administration, IDB and MT.; funding acquisition, MJT. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by Ziemer Ophthalmics, Bern, Switzerland.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, Ethical approval was obtained from the Ethics Committee of the University of Antwerpen (Edge 001299; 17 January 2022).
Informed Consent Statement
Written informed consent was obtained from the patient's legal representatives and from the child when aged > 6 years old.
Data Availability Statement
Dataset available on request from the authors.
Acknowledgments
Eva Stetzer, PhD, QuintesScience, provided medical writing assistance and editorial support.
Conflicts of Interest
MJT is consultant to Ziemer Ophthalmics, Bern, Switzerland, and has an intellectual property in the bag-in-the-lens and ring caliper licensed to Morcher/ Germany. LVO received a travel grant and writing assistance from Ziemer Ophthalmics, Bern, Switzerland. No COI for other authors.
Abbreviations
The following abbreviations are used in this manuscript:
| FS-laser |
Femtosecond laser |
| BIL |
Bag-in-the-lens |
| IOL |
Intraocular lens |
| AE |
Adverse events |
| FLACS |
Femtosecond laser-assisted cataract surgery |
| SD-OCT |
Spectral-domain optical coherence tomography |
References
- Wu, X.; Long, E.; Lin, H.; Liu, Y. Prevalence and epidemiological characteristics of congenital cataract: a systematic review and meta-analysis. Sci Rep. 2016, 6, 28564. [Google Scholar] [CrossRef]
- Self, J.E.; Taylor, R.; Solebo, A.L.; Biswas, S.; Parulekar, M.; Dev Borman, A.; Ashworth, J.; McClenaghan, R.; Abbott, J.; O’Flynn, E.; Hildebrand, D.; Lloyd, I.C. Cataract management in children: a review of the literature and current practice across five large UK centres. Eye 2020, 34, 2197–2218. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.E., Jr. Anterior lens capsule management in pediatric cataract surgery. Trans Am Ophthalmol Soc. 2004, 102, 391–422. [Google Scholar]
- Findl, O.; Hirnschall, N.; Draschl, P.; Wiesinger, J.O. Effect of manual capsulorhexis size and position on intraocular lens tilt, centration, and axial position. J Cataract Refr Surg. 2017, 43, 902–8. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Hu, Y.; Guo, R.; Shao, Y.; Zhao, J.; Zhang, J.; Wang, J. The effects of different shapes of capsulorhexis on postoperative refractive outcomes and the effective position of the intraocular lens in cataract surgery. BMC Ophthalmol. 2019, 19, 59. [Google Scholar] [CrossRef] [PubMed]
- Tassignon, M.J.; De Groot, V.; Vrensen, G.F.J.M. Bag-in-the-lens implantation of intraocular lenses. J Cataract Refract Surg. 2002, 28, 1182–1188. [Google Scholar] [CrossRef]
- De Groot, V.; Leysen, I.; Neuhann, T.; Gobin, L.; Tassignon, M.J. One-year follow-up of the bag-in-the-lens intraocular lens implantation in 60 eyes. J Cataract Refract Surg. 2006, 32, 1632–1637. [Google Scholar] [CrossRef]
- Tassignon, M.J.; De Veuster, I.; Godts, D.; Kosec, D.; Van den Dooren, K.; Gobin, L. Bag-in-the-lens intraocular lens implantation in the pediatric eye. J Cat Refract Surg. 2007, 33, 611–617. [Google Scholar] [CrossRef]
- Friedman, N.J.; Palanker, D.V.; Schuele, G.; Andersen, D.; Marcellino, G.; Seibel, B.S.; Batlle, J.; Feliz, R.; Talamo, J.H.; Blumenkranz, M.S.; Culbertson, W.W. Femtosecond laser capsulotomy. J Cat Refract Surg. 2011, 37, 1189–98. [Google Scholar] [CrossRef]
- Tereshchenko, A.V.; Trifanenkova, I.G.; Vladimirovich, V.M. Femtosecond laser-assisted anterior and posterior capsulotomies in children with persistent hyperplastic primary vitreous. J Cat Refract Surg. 2020, 46, 497–502. [Google Scholar] [CrossRef]
- Nagy, Z.Z.; Kranitz, K.; Takacs, A.I.; Mihaltz, K.; Kovacs, I.; Knorz, M.C. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg. 2011, 27, 564–9. [Google Scholar] [CrossRef] [PubMed]
- Palanker, D.V.; Blumenkranz, M.S.; Andersen, D.; Wiltberger, M.; Marcellino, G.; Gooding, P.; Angeley, D.; Schuele, G.; Woodley, B.; Simoneau, M.; Friedman, N.J.; Seibel, B.; Batlle, J.; Feliz, R.; Talamo, J.; Culbertson, W. Femtosecond laser-assisted cataract surgery with integrated optical coherence tomography. Sci Transl Med. 2010, 2, 58ra85. [Google Scholar] [CrossRef] [PubMed]
- Pajic, B.; Cvejic, Z.; Pajic-Eggspuehler, B. Cataract Surgery Performed by High Frequency LDV Z8 Femtosecond Laser: Safety, Efficacy, and Its Physical Properties. Sensors (Basel), 2017; 17, 1429. [Google Scholar]
- Kolb, C.M.; Shajari, M.; Mathys, L.; Hermann, E.; Petermann, K.; Mayer, W.J.; Priglinger, S.; Kohnen, T. Comparison of femtosecond laser-assisted cataract surgery and conventional cataract surgery: a meta-analysis and systematic review. J Cataract Refract Surg. 2020, 46, 1075–1085. [Google Scholar] [CrossRef] [PubMed]
- Salgado, R.; Torres, P.; Marinho, A. Update on Femtosecond Laser-Assisted Cataract Surgery: A Review. Clin Ophthalmol. 2024, 18, 459–472. [Google Scholar] [CrossRef]
- Riemey, J.; Latz, C.; Mirshahi, A. Intraoperative complications of cataract surgery using a low-energy femtosecond laser: results from a real-world high-volume setting. PLoS One 2022, 17, e0279023. [Google Scholar] [CrossRef]
- Trifanenkova, I.G.; Tereshchenko, A.V.; Isaev, S.V. Femtosecond laser-assisted anterior capsulotomy in children undergoing cataract surgery: a large case series. BMJ Open Ophthalmol. 2022, 7, e000945. [Google Scholar] [CrossRef]
- Dick, H.B.; Schelenz, D.; Schultz, T. Femtosecond laser-assisted pediatric cataract surgery: Bochum formula. J Cataract Refract Surg. 2015, 41, 821–6. [Google Scholar] [CrossRef]
- Dick, H.B.; Schultz, T. Femtosecond laser–assisted cataract surgery in infants. J Cataract Refract Surg. 2013, 39, 665–8. [Google Scholar] [CrossRef]
- Latz, C.; Asshauer, T.; Rathjen, C.; Mishahi, A. Femtosecond-Laser Assisted Surgery of the Eye: Overview and Impact of the Low-Energy Concept. Micromachines (Basel) 2021, 12, 122–143. [Google Scholar] [CrossRef]
- Van Os, L.; Hildebrand, G.D.; Tassignon, M.J. Adapted Bag-in-the-Lens Implantation Technique in Children with Congenital Ectopia Lentis. Klin Monbl Augenheilkd 2021, 238, 1058–1064. [Google Scholar] [CrossRef]
- Liao, M.; Guo, D.; Liao, S.; Zhang, W.; Lin, D.; Tang, Q. Study on the enlargement index of femtosecond laser-assisted capsulorhexis in 2–6-year-old patients with congenital cataract. BMC Ophthalmol. 2021, 21, 441. [Google Scholar] [CrossRef] [PubMed]
- Rezar-Dreindl, S.; Stifter, E.; Neumayer, T.; Papp, A.; Gschliesser, A.; Schmidt-Erfurth, U. Visual outcome and surgical results in children with Marfan syndrome. Clin Exp Ophthalmol. 2019, 47, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Kaur, S.; Sukhija, J.; Gupta, P.C.; Ram, J. Role of swept-source anterior segment optical coherence tomography in imaging pediatric cataract. Indian J Ophthalmol. 2023, 71, 2132–2138. [Google Scholar] [CrossRef] [PubMed]
- Avasthi, P.; Marshall, W.F. Stages of Ciliogenesis and Regulation of Ciliary Length. Differentiation. 2012, 83, S30–S42. [Google Scholar] [CrossRef]
- Lin, H.Y.; Chuang, Y.J.; Lin, P.J. Surgical outcomes with high and low pulse energy femtosecond laser systems for cataract surgery. Sci Rep. 2021, 11, 9525. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).