Submitted:
08 February 2025
Posted:
08 February 2025
You are already at the latest version
Abstract
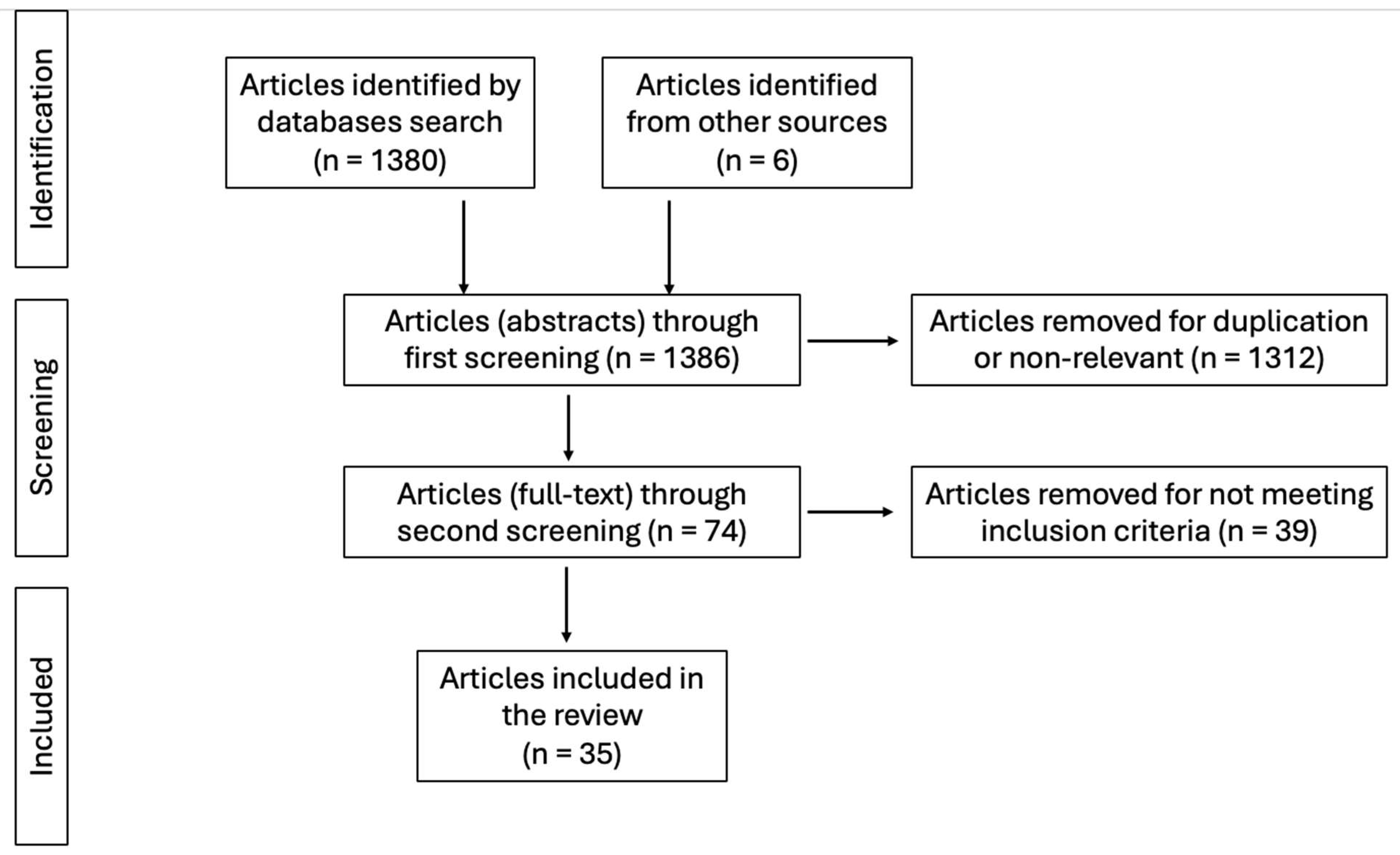
Background/Objectives: The quality of life (QoL) in patients undergoing pelvic prolapse surgery is a critical area of research in urogynecology. Pelvic organ prolapse (POP) is a prevalent condition affecting a significant number of women, leading to various physical and psychological symptoms that can severely impact their quality of life. Surgical intervention aims not only to correct the anatomical defects but also to enhance the overall well-being of patients. Methods: A comprehensive literature search in the main databases was conducted for studies evaluating quality of life after surgical treatment using techniques with and without mesh. Results: A total of 35 studies met de inclusion criteria, involving a total of 4603 patients. Twenty-two distinct patient-reported outcomes (PRO) questionnaires have been identified as post-surgical QoL assessment tools. Conclusions: Quality of life is significantly improved by surgical treatment of pelvic organ prolapse. Post-surgical PRO scores do not seem to be influenced by the surgical technique used, with no significant differences between methods using mesh or not.
Keywords:
1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of the Studies Included
3.2. Characteristics of the Population Included
3.3. Surgical Techiques
3.4. Time of Assessment
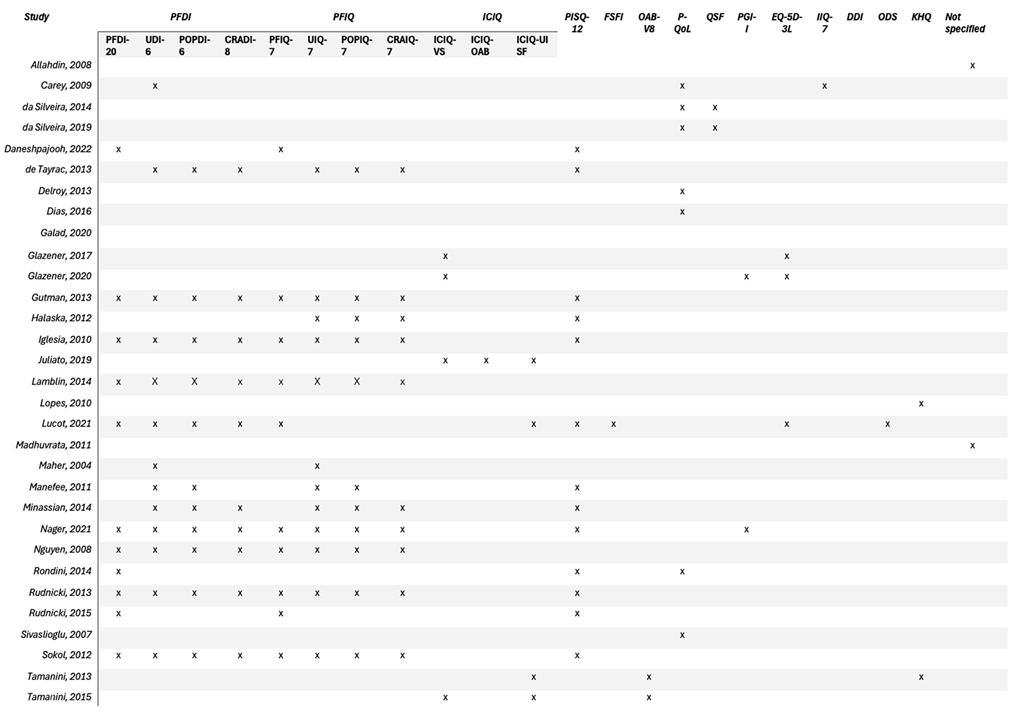
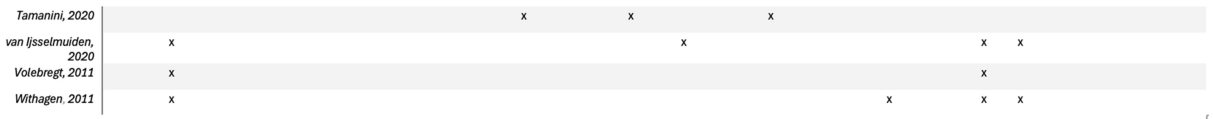
3.5. Quality of Life Assessment Methods
3.5.1. Pelvic Floor Distress Inventory (PFDI)
3.5.2. Pelvic Floor Impact Questionnaire (PFIQ)
3.5.3. The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire
3.5.4. Prolapse Quality of Life Questionnaire
3.5.5. Other PROs
3.6. Quality of Life Outcomes After POP Surgery
| Study | Year | Design | Population | Outcome |
|---|---|---|---|---|
| Allahdin | 2008 | RCT | 66 | Significant improvement with no difference between groups |
| Carey | 2009 | RCT | 139 | Significant improvement with no difference between groups |
| da Silveira | 2019 | RCT | 122 | No significant difference in domains of general health perception and personal relationship limits but significant improvement in all the other domains |
| da Silveira | 2014 | RCT | 184 | Significant improvement in mesh group for anterior compartment only; no difference for apical and posterior compartments; |
| Daneshpajooh | 2022 | RCT | 32 | Improvement with no difference for all questionnaire scores |
| de Tayrac | 2013 | RCT | 147 | Significant improvement with no difference between groups |
| Delroy | 2013 | RCT | 79 | Significant improvement with no difference between groups |
| Dias | 2016 | RCT | 88 | Significant improvement with better satisfaction in mesh group - probably by cofounders |
| Galad | 2020 | RCT | 146 | Significant improvement with no difference between groups |
| Glazener | 2020 | RCT | 154 | No difference between groups with exception of EQ-5D-3L at 1 year in favor of mesh kit vs native |
| Glazener | 2017 | RCT | 865 | Significant improvement with no difference between groups |
| Gutman | 2013 | RCT | 65 | Significant improvement with no difference between groups |
| Halaska | 2012 | RCT | 168 | Significant improvement with no difference between groups |
| Iglesia | 2010 | RCT | 65 | Significant improvement with no difference between groups |
| Juliato | 2018 | RCT | 71 | Significant improvement with no difference between groups |
| Lamblin | 2014 | RCT | 78 | Significant improvement with no difference between groups |
| Lopes | 2009 | RCT | 32 | Significant improvement with no difference between groups |
| Lucot | 2021 | RCT | 262 | Significant improvement with no difference between groups |
| Madhuvrata | 2011 | RCT | 66 | Significant improvement with no difference between groups |
| Maher | 2004 | RCT | 96 | Significant improvement with no difference between groups |
| Menefee | 2011 | RCT | 99 | Significant improvment with not difference between groups |
| Minassian | 2014 | RCT | 70 | Significant improvment with not difference between groups |
| Nager | 2021 | RCT | 118 | Significant improvment with not difference between groups excepting for UDI with a significant improvement for HT group |
| Nguyen | 2008 | RCT | 76 | Significant improvment with not difference between groups |
| Rondini | 2014 | RCT | 124 | Significant improvment with not difference between groups |
| Rudnicki | 2013 | RCT | 161 | Significant improvment with not difference between groups |
| Rudnicki | 2015 | RCT | 138 | No difference between groups |
| Sivaslioglu | 2007 | RCT | 90 | Significant improvement in both groups |
| Sokol | 2012 | RCT | 65 | Significant improvment with not difference between groups |
| Tamanini | 2020 | RCT | 92 | No significant difference; mesh group associated with negative impact after adjusting for other variables |
| Tamanini | 2013 | RCT | 100 | Significant improvement in both groups |
| Tamanini | 2015 | RCT | 100 | Significant improvement in both groups |
| van Ijsselmuiden | 2020 | RCT | 126 | Significant improvement in both groups, OAB (from UDI) and fecal incontinence (from DDI) worse after LSH group |
| Volebregt | 2011 | RCT | 125 | Significant improvment with not difference between groups |
| Withagen | 2011 | RCT | 194 | Significant improvment with not difference between groups |
| PRO questionnaire | Mean preop. score – mesh | Mean preop. score – no mesh |
Mean postop. score – no mesh |
Mean postop. score- no mesh |
|---|---|---|---|---|
| PFDI-20 | 95.6 (±28.5) | 112 (±33.4) | 32.7 (±11.8) | 32.9 (±13.3) |
| p = 0.97 | ||||
| UDI-6 | 53.5 (±25.7) | 56.1 (±27.1) | 15.3 (±8.6) | 14.1 (±6.7) |
| p = 0.69 | ||||
| POPDI-6 | 60.9 (±34.2) | 66.7 (±28.5) | 10 (±10.4) | 13.4 (±11.6) |
| p = 0.52 | ||||
| CRADI-6 | 32.9 (±31.6) | 42.9 (±33.2) | 15.6 (±9.6) | 18.6 (±15.1) |
| p = 0.62 | ||||
| PFIQ-7 | 42.3 (±23.4) | 48.9 (±20.4) | 9.05 (±8.6) | 10.9 (±9.8) |
| p = 0.65 | ||||
| UIQ-7 | 29.7 (±24.2) | 37.0 (±31.8) | 10.8 (±10.8) | 12.5 (±14.6) |
| p = 0.78 | ||||
| POPIQ-7 | 20.6 (±21.8) | 27.2 (±25.8) | 2.57 (±3.9) | 5.31 (±7) |
| p = 0.32 | ||||
| CRAIQ-7 | 11.1 (±11.2) | 18.1 (±24.6) | 3.19 (±3.49) | 8.97 (±15.4) |
| p = 0.28 | ||||
| PISQ-12 | 21.8 (±13.2) | 21.8 (±13.3) | 22.7 (±14.4) | 22.9 (±14.4) |
| p= 0.97 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hadizadeh-Talasaz, Z.; Khadivzadeh, T.; Mohajeri, T.; Sadeghi, M. Worldwide Prevalence of Pelvic Organ Prolapse: A Systematic Review and Meta-Analysis. ijph 2024. [Google Scholar] [CrossRef] [PubMed]
- Schulten, S.F.M.; Claas-Quax, M.J.; Weemhoff, M.; Van Eijndhoven, H.W.; Van Leijsen, S.A.; Vergeldt, T.F.; IntHout, J.; Kluivers, K.B. Risk Factors for Primary Pelvic Organ Prolapse and Prolapse Recurrence: An Updated Systematic Review and Meta-Analysis. American Journal of Obstetrics and Gynecology 2022, 227, 192–208. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, S.L.; Clark, A.; Nygaard, I.; Aragaki, A.; Barnabei, V.; McTiernan, A. Pelvic Organ Prolapse in the Women’s Health Initiative: Gravity and Gravidity. American Journal of Obstetrics and Gynecology 2002, 186, 1160–1166. [Google Scholar] [CrossRef]
- Maher, C.; Feiner, B.; Baessler, K.; Schmid, C. Surgical Management of Pelvic Organ Prolapse in Women. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd: Chichester, UK, 2013; p. 004014. [Google Scholar]
- Health, C. for D. and R. Pelvic Organ Prolapse (POP): Surgical Mesh Considerations and Recommendations. FDA 2021.
- Dällenbach, P. To Mesh or Not to Mesh: A Review of Pelvic Organ Reconstructive Surgery. IJWH 2015, 331. [Google Scholar] [CrossRef]
- Barber, M.D.; Walters, M.D.; Bump, R.C. Short Forms of Two Condition-Specific Quality-of-Life Questionnaires for Women with Pelvic Floor Disorders (PFDI-20 and PFIQ-7). American Journal of Obstetrics and Gynecology 2005, 193, 103–113. [Google Scholar] [CrossRef]
- Shatkin-Margolis, A.; Pauls, R.N. Sexual Function after Prolapse Repair. Current Opinion in Obstetrics & Gynecology 2017, 29, 343–348. [Google Scholar] [CrossRef]
- Sharami, A.N.; Feiring, M.H.; Eide, E.N.; Thornhill, H.; Trovik, J. Long-Term Patient-Reported Outcome for Surgical Management of Pelvic Organ Prolapse: A Retrospective Cohort Study. Journal of Gynecology Obstetrics and Human Reproduction 2024, 102895. [Google Scholar] [CrossRef]
- De Tayrac, R.; Cornille, A.; Eglin, G.; Guilbaud, O.; Mansoor, A.; Alonso, S.; Fernandez, H. Comparison between Trans-Obturator Trans-Vaginal Mesh and Traditional Anterior Colporrhaphy in the Treatment of Anterior Vaginal Wall Prolapse: Results of a French RCT. Int Urogynecol J 2013, 24, 1651–1661. [Google Scholar] [CrossRef]
- Delroy, C.A.; Castro, R.D.A.; Dias, M.M.; Feldner, P.C.; Bortolini, M.A.T.; Girão, M.J.B.C.; Sartori, M.G.F. The Use of Transvaginal Synthetic Mesh for Anterior Vaginal Wall Prolapse Repair: A Randomized Controlled Trial. Int Urogynecol J 2013, 24, 1899–1907. [Google Scholar] [CrossRef]
- Dias, M.M.; Castro, R.D.A.; Bortolini, M.A.T.; Delroy, C.A.; Martins, P.C.F.; Girão, M.J.B.C.; Sartori, M.G.F. Two-years Results of Native Tissue versus Vaginal Mesh Repair in the Treatment of Anterior Prolapse According to Different Success Criteria: A Randomized Controlled Trial. Neurourology and Urodynamics 2016, 35, 509–514. [Google Scholar] [CrossRef]
- Menefee, S.A.; Dyer, K.Y.; Lukacz, E.S.; Simsiman, A.J.; Luber, K.M.; Nguyen, J.N. Colporrhaphy Compared With Mesh or Graft-Reinforced Vaginal Paravaginal Repair for Anterior Vaginal Wall Prolapse: A Randomized Controlled Trial. Obstetrics & Gynecology 2011, 118, 1337–1344. [Google Scholar] [CrossRef]
- Nguyen, J.N.; Burchette, R.J. Outcome After Anterior Vaginal Prolapse Repair: A Randomized Controlled Trial. Obstetrics & Gynecology 2008, 111, 891–898. [Google Scholar] [CrossRef]
- Rudnicki, M.; Laurikainen, E.; Pogosean, R.; Kinne, I.; Jakobsson, U.; Teleman, P. Anterior Colporrhaphy Compared with Collagen-coated Transvaginal Mesh for Anterior Vaginal Wall Prolapse: A Randomised Controlled Trial. BJOG 2014, 121, 102–111. [Google Scholar] [CrossRef]
- Rudnicki, M.; Laurikainen, E.; Pogosean, R.; Kinne, I.; Jakobsson, U.; Teleman, P. A 3–Year Follow-up after Anterior Colporrhaphy Compared with Collagen-coated Transvaginal Mesh for Anterior Vaginal Wall Prolapse: A Randomised Controlled Trial. BJOG 2016, 123, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Tamanini, J.T.N.; Castro, R.C.D.O.S.; Tamanini, J.M.; Feldner Jr, P.C.; Castro, R.D.A.; Sartori, M.G.F.; Girao, M.J.B.C. Treatment of Anterior Vaginal Wall Prolapse with and without Polypropylene Mesh: A Prospective, Randomized and Controlled Trial - Part II. Int. braz j urol. 2013, 39, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Tamanini, J.T.N.; De Oliveira Souza Castro, R.C.; Tamanini, J.M.; Castro, R.A.; Sartori, M.G.F.; Girão, M.J.B.C. A Prospective, Randomized, Controlled Trial of the Treatment of Anterior Vaginal Wall Prolapse: Medium Term Followup. Journal of Urology 2015, 193, 1298–1304. [Google Scholar] [CrossRef]
- Tamanini, J.T.N.; Reis, L.O.; Da Mota Tamanini, M.M.; Aquino Castro, R.; Sartori, M.G.F.; Girão, M.J.B.C. No Mesh versus Mesh in the Treatment of Anterior Vaginal Wall Prolapse: Prospective, Randomised, Controlled Trial, Long-Term Follow-Up. Int Urol Nephrol 2020, 52, 1839–1844. [Google Scholar] [CrossRef]
- Vollebregt, A.; Fischer, K.; Gietelink, D.; Van Der Vaart, C. Primary Surgical Repair of Anterior Vaginal Prolapse: A Randomised Trial Comparing Anatomical and Functional Outcome between Anterior Colporrhaphy and Trocar-guided Transobturator Anterior Mesh. BJOG 2011, 118, 1518–1527. [Google Scholar] [CrossRef]
- Lamblin, G.; Van-Nieuwenhuyse, A.; Chabert, P.; Lebail-Carval, K.; Moret, S.; Mellier, G. A Randomized Controlled Trial Comparing Anatomical and Functional Outcome between Vaginal Colposuspension and Transvaginal Mesh. Int Urogynecol J 2014, 25, 961–970. [Google Scholar] [CrossRef]
- Lucot, J.; Cosson, M.; Verdun, S.; Debodinance, P.; Bader, G.; Campagne-Loiseau, S.; Salet-Lizee, D.; Akladios, C.; Ferry, P.; De Tayrac, R.; et al. Long-term Outcomes of Primary Cystocele Repair by Transvaginal Mesh Surgery versus Laparoscopic Mesh Sacropexy: Extended Follow up of the PROSPERE Multicentre Randomised Trial. BJOG 2022, 129, 127–137. [Google Scholar] [CrossRef]
- Minassian, V.A.; Parekh, M.; Poplawsky, D.; Gorman, J.; Litzy, L. Randomized Controlled Trial Comparing Two Procedures for Anterior Vaginal Wall Prolapse. Neurourology and Urodynamics 2014, 33, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Sivaslioglu, A.A.; Unlubilgin, E.; Dolen, I. A Randomized Comparison of Polypropylene Mesh Surgery with Site-Specific Surgery in the Treatment of Cystocoele. Int Urogynecol J 2008, 19, 467–471. [Google Scholar] [CrossRef]
- Daneshpajooh, A.; Pakmanesh, H.; Sohbati, S.; Mirzaei, M.; Zemanati, E.; Dehesh, T. Comparing Laparoscopic Sacrocolpopexy with Vaginal Sacrospinous Ligament Fixation in the Treatment of Vaginal Apical Prolapse; the First Randomized Clinical Trial: A Pilot Study. Urology Journal 2022, 7039. [Google Scholar] [CrossRef]
- Van IJsselmuiden, M.; Van Oudheusden, A.; Veen, J.; Van De Pol, G.; Vollebregt, A.; Radder, C.; Housmans, S.; Van Kuijk, S.; Deprest, J.; Bongers, M.; et al. Hysteropexy in the Treatment of Uterine Prolapse Stage 2 or Higher: Laparoscopic Sacrohysteropexy versus Sacrospinous Hysteropexy—A Multicentre Randomised Controlled Trial (LAVA Trial). BJOG 2020, 127, 1284–1293. [Google Scholar] [CrossRef]
- Juliato, C.R.T.; Santos-Junior, L.C.; De Castro, E.B.; Dertkigil, S.S.; Brito, L.G.O. Vaginal Axis after Abdominal Sacrocolpopexy versus Vaginal Sacrospinous Fixation—A Randomized Trial. Neurourology and Urodynamics 2019, 38, 1142–1151. [Google Scholar] [CrossRef]
- Maher, C.F.; Qatawneh, A.M.; Dwyer, P.L.; Carey, M.P.; Cornish, A.; Schluter, P.J. Abdominal Sacral Colpopexy or Vaginal Sacrospinous Colpopexy for Vaginal Vault Prolapse: A Prospective Randomized Study. American Journal of Obstetrics and Gynecology 2004, 190, 20–26. [Google Scholar] [CrossRef]
- Halaska, M.; Maxova, K.; Sottner, O.; Svabik, K.; Mlcoch, M.; Kolarik, D.; Mala, I.; Krofta, L.; Halaska, M.J. A Multicenter, Randomized, Prospective, Controlled Study Comparing Sacrospinous Fixation and Transvaginal Mesh in the Treatment of Posthysterectomy Vaginal Vault Prolapse. American Journal of Obstetrics and Gynecology 2012, 207, 301.e1–301.e7. [Google Scholar] [CrossRef] [PubMed]
- Lopes, E.D.; De Barros Moreira Lemos, N.L.; Da Silva Carramão, S.; Lunardelli, J.L.; Ruano, J.M.C.; Aoki, T.; Auge, A.P.F. Transvaginal Polypropylene Mesh versus Sacrospinous Ligament Fixation for the Treatment of Uterine Prolapse: 1-Year Follow-up of a Randomized Controlled Trial. Int Urogynecol J 2010, 21, 389–394. [Google Scholar] [CrossRef]
- Rondini, C.; Braun, H.; Alvarez, J.; Urzúa, M.J.; Villegas, R.; Wenzel, C.; Descouvieres, C. High Uterosacral Vault Suspension vs Sacrocolpopexy for Treating Apical Defects: A Randomized Controlled Trial with Twelve Months Follow-Up. Int Urogynecol J 2015, 26, 1131–1138. [Google Scholar] [CrossRef]
- Allahdin, S.; Glazener, C.; Bain, C. A Randomised Controlled Trial Evaluating the Use of Polyglactin Mesh, Polydioxanone and Polyglactin Sutures for Pelvic Organ Prolapse Surgery. Journal of Obstetrics and Gynaecology 2008, 28, 427–431. [Google Scholar] [CrossRef]
- Carey, M.; Higgs, P.; Goh, J.; Lim, J.; Leong, A.; Krause, H.; Cornish, A. Vaginal Repair with Mesh versus Colporrhaphy for Prolapse: A Randomised Controlled Trial. BJOG 2009, 116, 1380–1386. [Google Scholar] [CrossRef] [PubMed]
- Glazener, C.M.; Breeman, S.; Elders, A.; Hemming, C.; Cooper, K.G.; Freeman, R.M.; Smith, A.R.; Reid, F.; Hagen, S.; Montgomery, I.; et al. Mesh, Graft, or Standard Repair for Women Having Primary Transvaginal Anterior or Posterior Compartment Prolapse Surgery: Two Parallel-Group, Multicentre, Randomised, Controlled Trials (PROSPECT). The Lancet 2017, 389, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Glazener, C.; Breeman, S.; Elders, A.; Hemming, C.; Cooper, K.; Freeman, R.; Smith, A.; Hagen, S.; Montgomery, I.; Kilonzo, M.; et al. Mesh Inlay, Mesh Kit or Native Tissue Repair for Women Having Repeat Anterior or Posterior Prolapse Surgery: Randomised Controlled Trial (PROSPECT). BJOG 2020, 127, 1002–1013. [Google Scholar] [CrossRef]
- Madhuvrata, P.; Glazener, C.; Boachie, C.; Allahdin, S.; Bain, C. A Randomised Controlled Trial Evaluating the Use of Polyglactin (Vicryl) Mesh, Polydioxanone (PDS) or Polyglactin (Vicryl) Sutures for Pelvic Organ Prolapse Surgery: Outcomes at 2 Years. Journal of Obstetrics and Gynaecology 2011, 31, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Withagen, M.I.; Milani, A.L.; Den Boon, J.; Vervest, H.A.; Vierhout, M.E. Trocar-Guided Mesh Compared With Conventional Vaginal Repair in Recurrent Prolapse: A Randomized Controlled Trial. Obstetrics & Gynecology 2011, 117, 242–250. [Google Scholar] [CrossRef]
- Galad, J.; Papcun, P.; Dudic, R.; Urdzik, P. Single-incision Mesh vs Sacrospinous Ligament Fixationin Posthysterectomy Women at a Three-Year Follow-up:A Randomized Trial. BLL 2020, 121, 640–647. [Google Scholar] [CrossRef]
- Iglesia, C.B.; Sokol, A.I.; Sokol, E.R.; Kudish, B.I.; Gutman, R.E.; Peterson, J.L.; Shott, S. Vaginal Mesh for Prolapse. 2010, 116.
- Nager, C.W.; Visco, A.G.; Richter, H.E.; Rardin, C.R.; Komesu, Y.; Harvie, H.S.; Zyczynski, H.M.; Paraiso, M.F.R.; Mazloomdoost, D.; Sridhar, A.; et al. Effect of Sacrospinous Hysteropexy with Graft vs Vaginal Hysterectomy with Uterosacral Ligament Suspension on Treatment Failure in Women with Uterovaginal Prolapse: 5-Year Results of a Randomized Clinical Trial. American Journal of Obstetrics and Gynecology 2021, 225, 153.e1–153.e31. [Google Scholar] [CrossRef]
- Dos Reis Brandão Da Silveira, S.; Haddad, J.M.; De Jármy-Di Bella, Z.I.K.; Nastri, F.; Kawabata, M.G.M.; Da Silva Carramão, S.; Rodrigues, C.A.; Baracat, E.C.; Auge, A.P.F. Multicenter, Randomized Trial Comparing Native Vaginal Tissue Repair and Synthetic Mesh Repair for Genital Prolapse Surgical Treatment. Int Urogynecol J 2015, 26, 335–342. [Google Scholar] [CrossRef]
- Da Silveira, S.D.R.B.; Auge, A.P.; Jarmy-Dibella, Z.I.; Margarido, P.F.; Carramao, S.; Alves Rodrigues, C.; Doumouchtsis, S.K.; Chada Baracat, E.; Milhem Haddad, J. A Multicenter, Randomized Trial Comparing Pelvic Organ Prolapse Surgical Treatment with Native Tissue and Synthetic Mesh: A 5-year Follow-up Study. Neurourology and Urodynamics 2020, 39, 1002–1011. [Google Scholar] [CrossRef]
- Gutman, R.E.; Nosti, P.A.; Sokol, A.I.; Sokol, E.R.; Peterson, J.L.; Wang, H.; Iglesia, C.B. Three-Year Outcomes of Vaginal Mesh for Prolapse: A Randomized Controlled Trial. Obstetrics & Gynecology 2013, 122, 770–777. [Google Scholar] [CrossRef]
- Sokol, A.I.; Iglesia, C.B.; Kudish, B.I.; Gutman, R.E.; Shveiky, D.; Bercik, R.; Sokol, E.R. One-Year Objective and Functional Outcomes of a Randomized Clinical Trial of Vaginal Mesh for Prolapse. American Journal of Obstetrics and Gynecology 2012, 206, 86.e1–86.e9. [Google Scholar] [CrossRef]
- Ruseckaite, R.; Jayasinghe, R.; Bavor, C.; Dean, J.; Daly, O.; Ahern, S. Evaluation and Acceptability of Patient-Reported Outcome Measures in Women Following Pelvic Organ Prolapse Procedures. BMC Health Serv Res 2023, 23, 624. [Google Scholar] [CrossRef]
- Barber, M.D.; Kuchibhatla, M.N.; Pieper, C.F.; Bump, R.C. Psychometric Evaluation of 2 Comprehensive Condition-Specific Quality of Life Instruments for Women with Pelvic Floor Disorders. American Journal of Obstetrics and Gynecology 2001, 185, 1388–1395. [Google Scholar] [CrossRef]
- Rogers, R.G.; Kammerer-Doak, D.; Villarreal, A.; Coates, K.; Qualls, C. A New Instrument to Measure Sexual Function in Women with Urinary Incontinence or Pelvic Organ Prolapse. American Journal of Obstetrics and Gynecology 2001, 184, 552–558. [Google Scholar] [CrossRef]
- Rogers, R.G.; Coates, K.W.; Kammerer-Doak, D.; Khalsa, S.; Qualls, C. A Short Form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). International Urogynecology Journal and Pelvic Floor Dysfunction 2003, 14, 164–168. [Google Scholar] [CrossRef]
- Rogers, R.G.; Pauls, R.N.; Thakar, R.; Morin, M.; Kuhn, A.; Petri, E.; Fatton, B.; Whitmore, K.; Kinsberg, S.; Lee, J. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for the Assessment of Sexual Health of Women with Pelvic Floor Dysfunction. Neurourology and Urodynamics 2018, 37, 1220–1240. [Google Scholar] [CrossRef]
- Digesu, G.A.; Khullar, V.; Cardozo, L.; Robinson, D.; Salvatore, S. P-QOL: A Validated Questionnaire to Assess the Symptoms and Quality of Life of Women with Urogenital Prolapse. Int Urogynecol J 2005, 16, 176–181. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, B.; Yuste-Sánchez, M.J.; Arranz-Martín, B.; Navarro-Brazález, B.; Romay-Barrero, H.; Torres-Lacomba, M. Quality of Life in POP: Validity, Reliability and Responsiveness of the Prolapse Quality of Life Questionnaire (P-QoL) in Spanish Women. IJERPH 2020, 17, 1690. [Google Scholar] [CrossRef]
- Ismail, S.; Duckett, J.; Rizk, D.; Sorinola, O.; Kammerer-Doak, D.; Contreras-Ortiz, O.; Al-Mandeel, H.; Svabik, K.; Parekh, M.; Phillips, C. Recurrent Pelvic Organ Prolapse: International Urogynecological Association Research and Development Committee Opinion. Int Urogynecol J 2016, 27, 1619–1632. [Google Scholar] [CrossRef]
- Geoffrion, R.; Larouche, M. Guideline No. 413: Surgical Management of Apical Pelvic Organ Prolapse in Women. Journal of Obstetrics and Gynaecology Canada 2021, 43, 511–523.e1. [Google Scholar] [CrossRef]
- Maher, C.F.; Feiner, B.; DeCuyper, E.M.; Nichlos, C.J.; Hickey, K.V.; O’Rourke, P. Laparoscopic Sacral Colpopexy versus Total Vaginal Mesh for Vaginal Vault Prolapse: A Randomized Trial. American Journal of Obstetrics and Gynecology 2011, 204, 360.e1–360.e7. [Google Scholar] [CrossRef]
- Devan, W.J.; Rodriguez, D.; Munarriz, R.; Ng, L.; Bose, S. Would Surgeons Opt for Polypropylene Mesh If They Hypothetically Had Stress Urinary Incontinence or Pelvic Organ Prolapse? Urology Practice 2022, 9, 306–313. [Google Scholar] [CrossRef]
- Dabica, A.; Balint, O.; Olaru, F.; Secosan, C.; Balulescu, L.; Brasoveanu, S.; Pirtea, M.; Popin, D.; Bacila, I.F.; Pirtea, L. Complications of Pelvic Prolapse Surgery Using Mesh: A Systematic Review. JPM 2024, 14, 622. [Google Scholar] [CrossRef]
- Chughtai, B.; Mao, J.; Buck, J.; Kaplan, S.; Sedrakyan, A. Use and Risks of Surgical Mesh for Pelvic Organ Prolapse Surgery in Women in New York State: Population Based Cohort Study. BMJ 2015, 350, h2685. [Google Scholar] [CrossRef]
- Kenton, K.; Mueller, E.R.; Tarney, C.; Bresee, C.; Anger, J.T. One-Year Outcomes After Minimally Invasive Sacrocolpopexy. Female Pelvic Med Reconstr Surg 2016, 22, 382–384. [Google Scholar] [CrossRef]
- Mereu, L.; Tateo, S.; D’Alterio, M.N.; Russo, E.; Giannini, A.; Mannella, P.; Pertile, R.; Cai, T.; Simoncini, T. Laparoscopic Lateral Suspension with Mesh for Apical and Anterior Pelvic Organ Prolapse: A Prospective Double Center Study. European Journal of Obstetrics & Gynecology and Reproductive Biology 2020, 244, 16–20. [Google Scholar] [CrossRef]
- Van Oudheusden, A.M.J.; Eissing, J.; Terink, I.M.; Vink, M.D.H.; Van Kuijk, S.M.J.; Bongers, M.Y.; Coolen, A.-L.W.M. Laparoscopic Sacrocolpopexy versus Abdominal Sacrocolpopexy for Vaginal Vault Prolapse: Long-Term Follow-up of a Randomized Controlled Trial. Int Urogynecol J 2023, 34, 93–104. [Google Scholar] [CrossRef]
- Ghanbari, Z.; Ghaemi, M.; Shafiee, A.; Jelodarian, P.; Hosseini, R.S.; Pouyamoghaddam, S.; Montazeri, A. Quality of Life Following Pelvic Organ Prolapse Treatments in Women: A Systematic Review and Meta-Analysis. JCM 2022, 11, 7166. [Google Scholar] [CrossRef]
- Guan, Y.; Han, J. Quality-of-Life Improvements in Patients after Various Surgical Treatments for Pelvic Organ Prolapse. Arch Gynecol Obstet 2023, 309, 813–820. [Google Scholar] [CrossRef]
| Compartment | Surgical Techniques | Studies | |
|---|---|---|---|
| Single | Anterior | Anterior colporraphy vs. transvaginal mesh | [10,11,12,13,14,15,16,17,18,19,20]; |
| Vaginal colposuspension vs. transvaginal mesh | [21]; | ||
| Laparoscopic sacropexy vs. transvaginal mesh | [22]; | ||
| Abdominal paravaginal repair vs. anterior colporraphy with mesh | [23]; | ||
| Multiple native tissue techniques vs transvaginal mesh | [24]; | ||
| Apical | Sacrospinous fixation vs. laparoscopic sacropexy | [25,26]; | |
| Sacrospinous fixation vs. abdominal sacropexy | [27,28]; | ||
| Sacrospinous fixation vs. mesh; | [29,30]; | ||
| Uterosacral suspension vs. abdominal sacropexy | [31]; | ||
| Multiple | Anterior/posterior | Native tissue techniques vs. transvaginal mesh | [32,33,34,35,36,37] |
| Anterior/apical | Sacrospinous fixation vs mesh; | [38] | |
| Uterosacral fixation vs. mesh; | [39] | ||
| Any/Not specified | Uterosacral suspension vs sacrospinous suspension with mesh; | [40] | |
| Multiple native tissue techniques vs. transvaginal mesh | [41,42,43,44]; | ||
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





