1. Introduction
Advances in imaging technology and the widespread implementation of screening mammography have significantly improved the early detection of non-palpable breast lesions, leading to increased diagnosis rates of early-stage breast cancer [
1]. The ability to detect these lesions before they become clinically evident has contributed to a shift in breast cancer management, with a strong emphasis on breast-conserving surgery (BCS) as the preferred treatment approach when oncologically appropriate [
2,
3,
4]. Multiple randomized controlled trials have demonstrated that BCS, when combined with appropriate adjuvant therapy, provides equivalent survival outcomes to mastectomy while preserving the natural breast contour, thereby improving patient satisfaction and quality of life [
2,
3,
4].
Given the widespread adoption of BCS, precise preoperative localization techniques are essential to ensure complete tumor removal while minimizing excision of healthy breast tissue and optimizing cosmetic outcomes [
1]. Wire-guided localization (WL) has long been the gold standard for marking non-palpable breast lesions prior to surgical excision [
5]. However, despite its efficacy, WL presents several logistical and technical challenges, including patient discomfort, risk of wire migration or dislodgement, and the necessity for same-day wire placement, which imposes significant strain on healthcare resources by requiring close coordination between radiology and surgery teams [
1].
To overcome these limitations, various wire-free localization techniques have emerged, offering increased flexibility in scheduling and improved patient comfort. These include radioactive seed localization (RSL), non-radioactive radar localization (SAVI SCOUT), magnetic seed localization (Magseed), and radiofrequency identification (RFID) [
1].
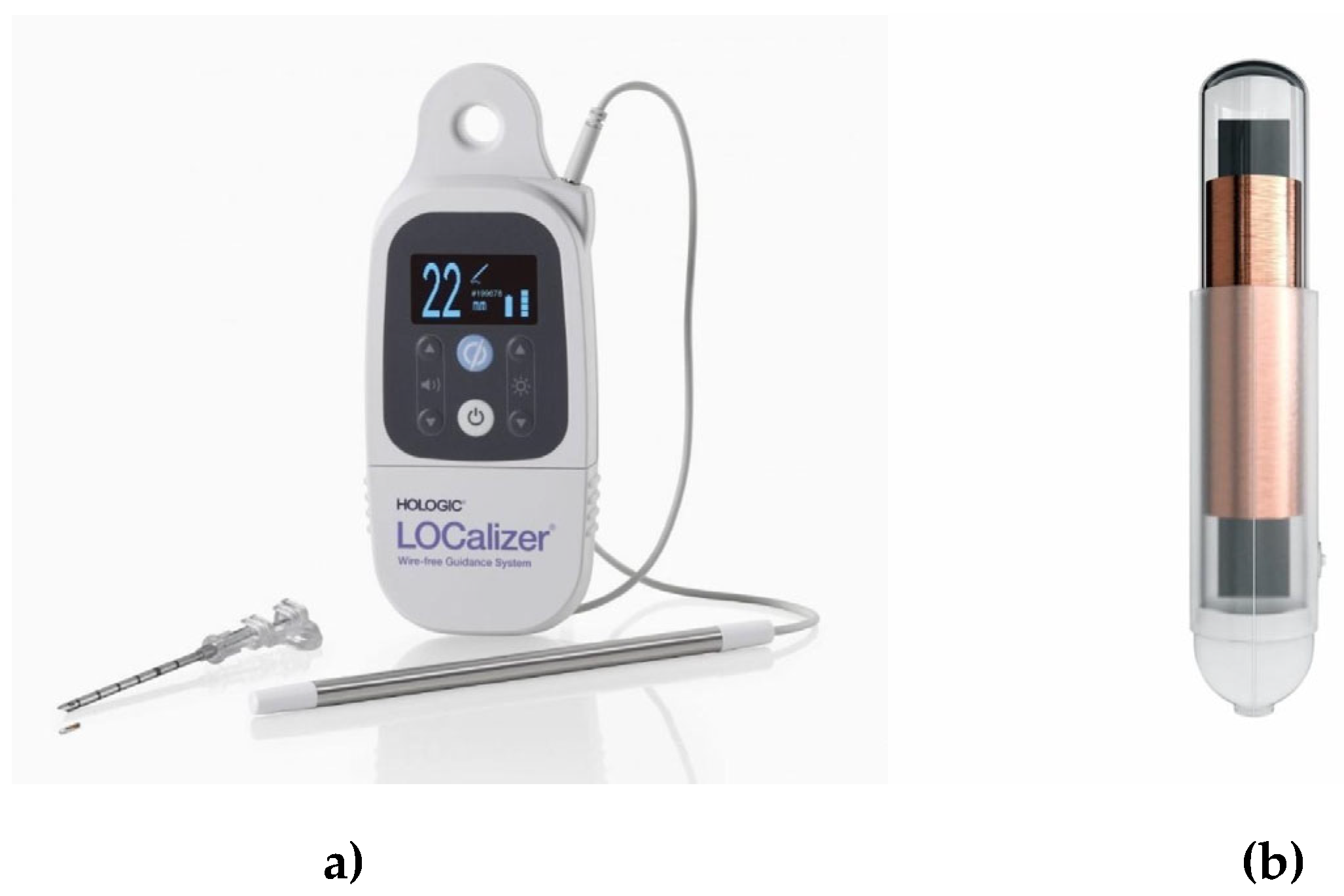
The LOCalizer™ system (Hologic, Marlborough, Massachusetts, USA) is based on ubiquitous RFID technology, offering a wire-free alternative for preoperative localization of non-palpable breast lesions. It consists of an RFID tag with a unique identification number preloaded in a needle applicator, a surgical probe with an 8 mm tip, and a portable handheld reader. The RFID tag itself is small, measuring approximately 11 mm in length and 2 mm in diameter, allowing for minimal tissue disruption upon placement. Notably, the tag includes a polypropylene cap designed to prevent migration within the breast tissue, ensuring stable localization until and during surgery. The tracer chip is deployed using a 12 G introducer, ensuring precise placement within the breast tissue. Once implanted, the tag emits a radiofrequency signal that is detected by the surgical probe, which is roughly the size of a pencil. The reader, which is lightweight and portable, displays real-time feedback on the distance to the tag in millimeters, while no along with the tag’s unique ID number, enabling accurate localization. Unlike some other localization methods, the LOCalizer™ tag does not require radiation or an external energy source to function, enhancing safety and logistical flexibility. The device is certified for long-term implantation, allowing for placement days or even weeks before surgery without compromising accuracy. Arguably, utilizing a widespread and well-understood technology such as RFID makes LOCalizer™ a robust and reliable choice for breast lesion localization, streamlining surgical workflows and improving patient comfort. [
5].
The purpose of this retrospective study was to assess the accuracy of preoperative RFID tag localization using the LOCalizer™ system and to document our initial experience with this technique in our breast unit. RFID tag placement accuracy was defined as being within 10 mm of the edge of the target lesion. Our benchmark of >95% of RFID tags being within 10 mm of the lesion was modeled on the NHS Breast Screening Programme’s standard, which considers >95% of localization wires within this range as acceptable [
6].
2. Materials and Methods
The cohort for this retrospective study included the first consecutive patients undergoing image-guided localization with radiofrequency identification (RFID) tags (LOCalizer™, Hologic, USA) prior to surgical excision from March 2021 to February 2023, comprising a total of 258 patients. Imaging and medical records were reviewed to evaluate the number of tags placed and the tag placement accuracy rate, defined as within 10 mm of the edge of the target lesion. Data collected also included patient age, the type of lesion/abnormality being targeted (e.g., impalpable lesions, masses, asymmetric densities, distortions, and microcalcifications [MCC]), lesion size (if applicable), and localization indication. The postoperative specimen pathology radiograph was reviewed to confirm the presence of the RFID tag. Post-surgical histopathology reports were assessed to calculate the number of patients requiring re-excision.
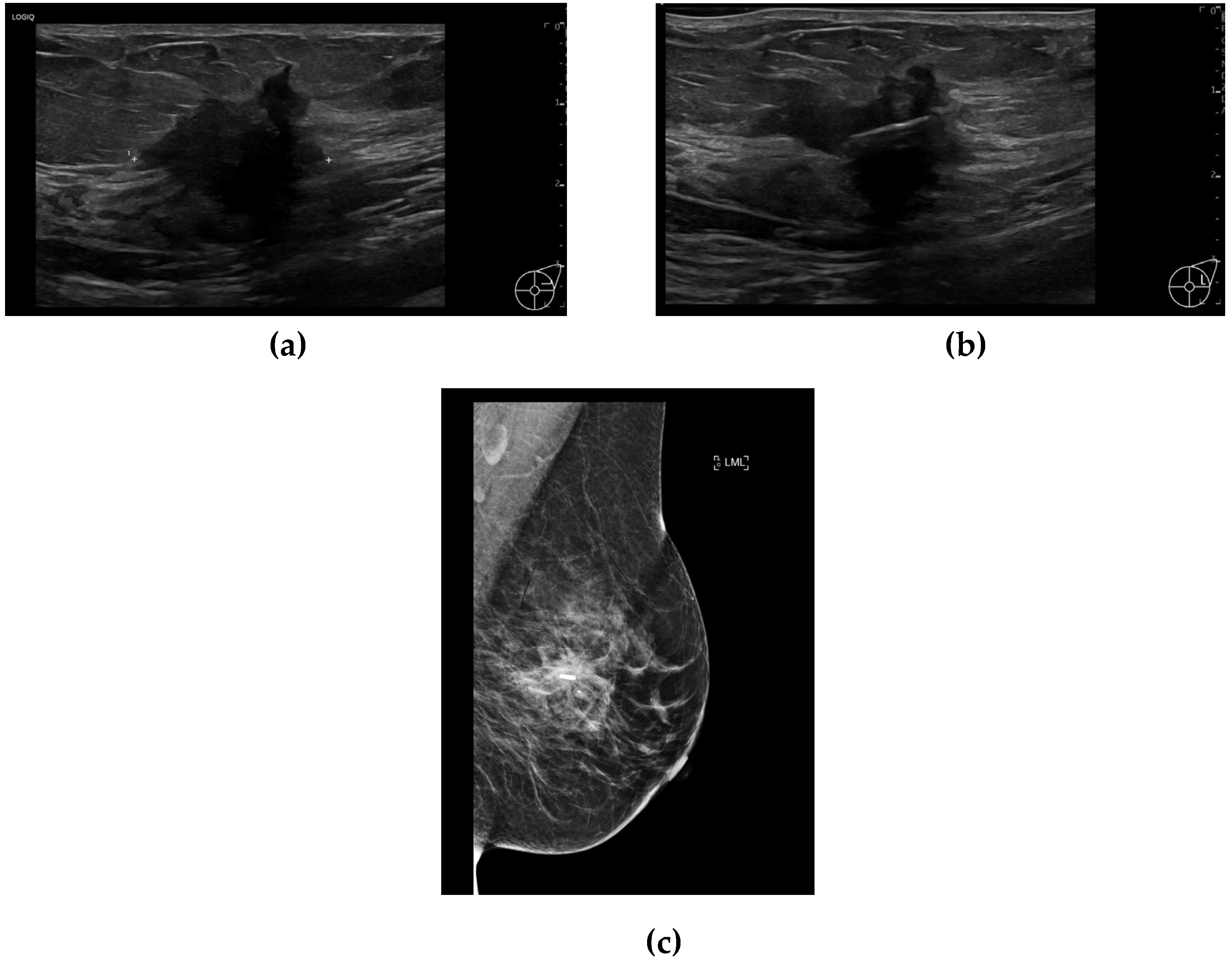
The RFID tags were inserted by either a consultant breast radiologist or a breast radiology trainee under ultrasound or mammographic guidance (
Figure 1a, 1b, and 1c). Tag insertion was performed during a dedicated appointment prior to surgery, allowing for preoperative planning and minimizing logistical challenges on the day of surgery. The LOCalizer system comprises a unique RFID tag, which measures approximately 11 mm in length and 2 mm in diameter, deployed using a 12-gauge introducer. Each tag includes a polypropylene cap designed to prevent migration within the breast tissue, ensuring stability throughout the preoperative period. After tag insertion, a handheld portable reader displays the distance to the tag in millimeters, which is particularly valuable when deploying more than one tag (e.g., in cases of bracketing or multifocal disease). The system also assigns an individual ID tag number, which is recorded in the patient’s medical notes (
Figure 2a and 2b), facilitating accurate intraoperative retrieval.
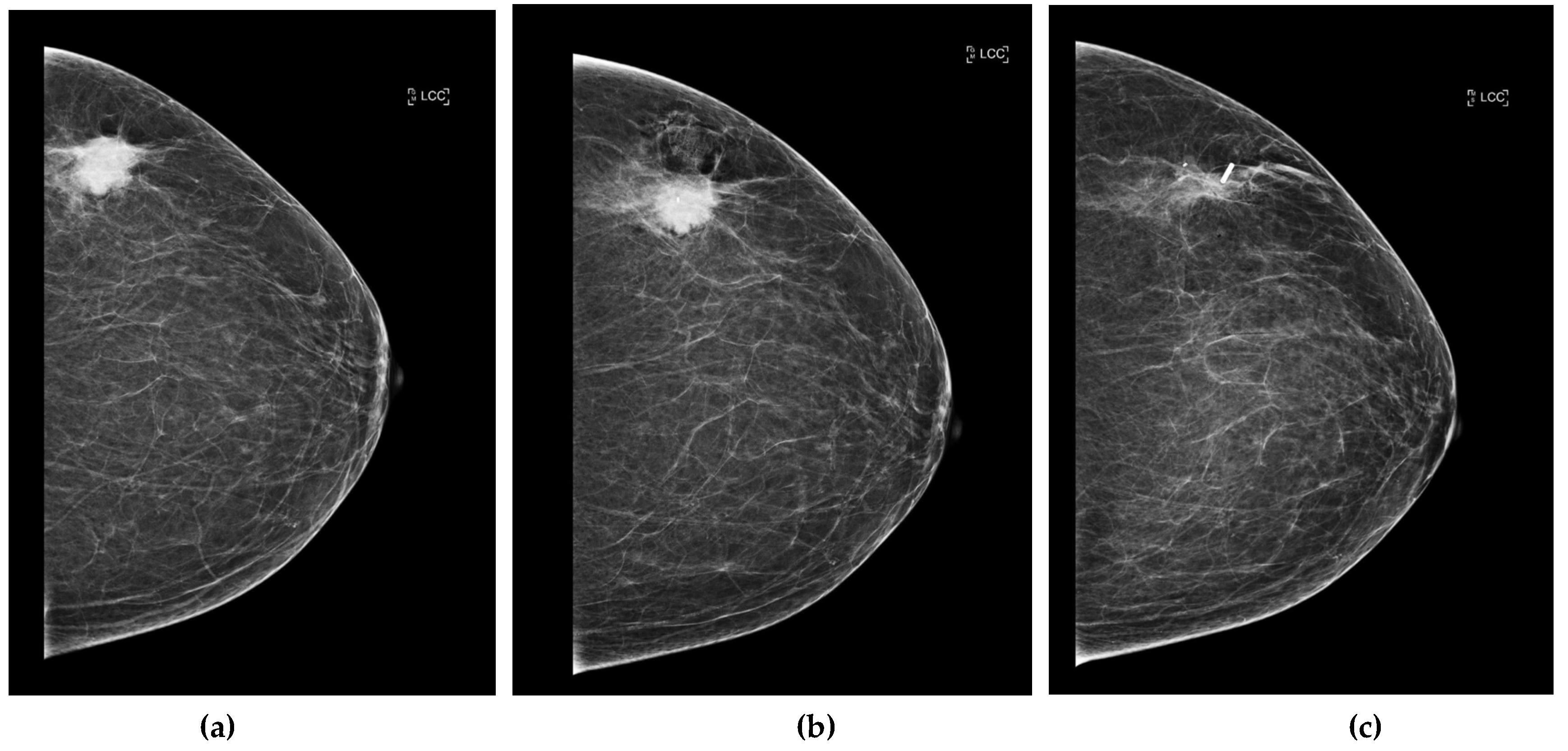
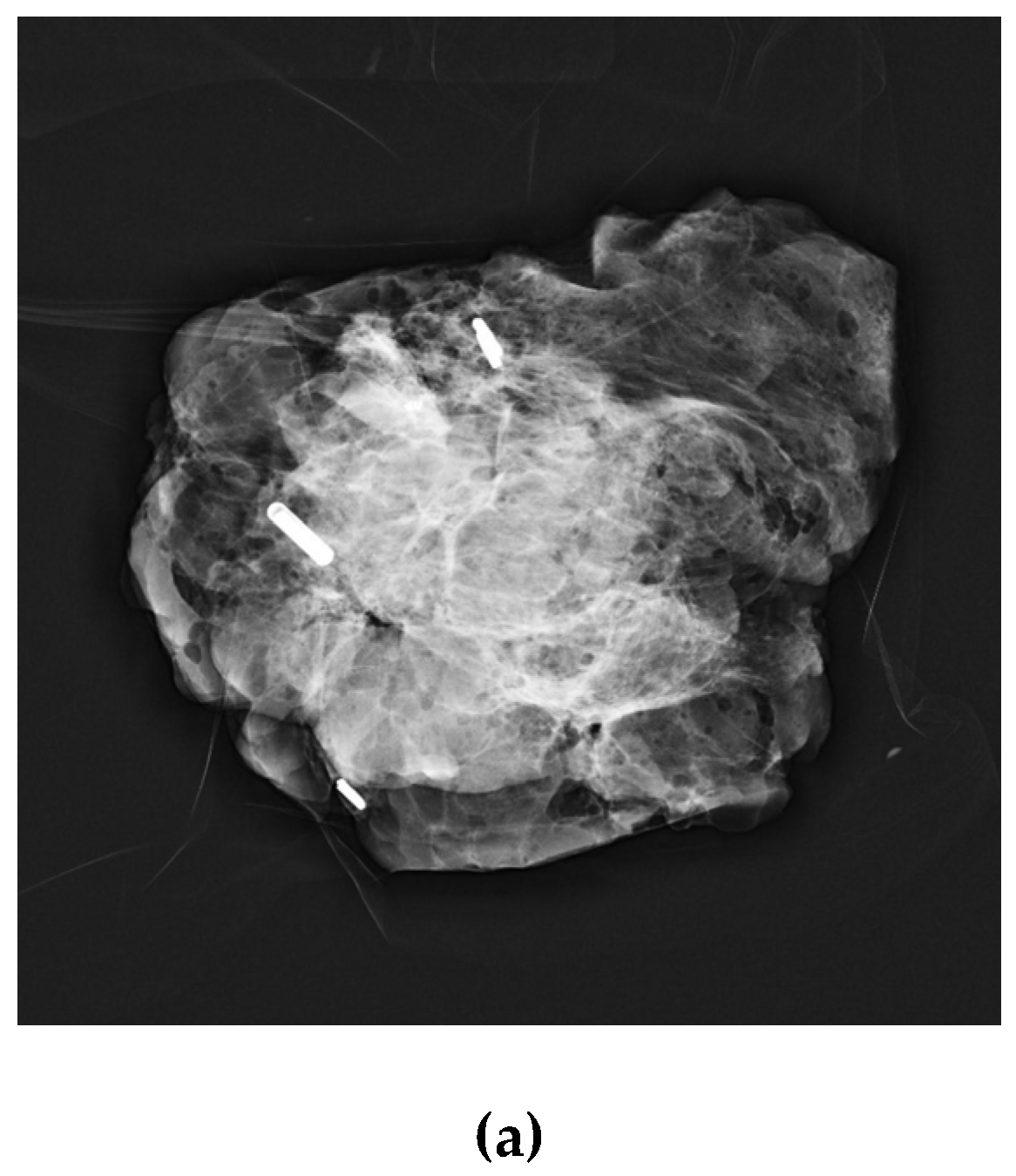
Post-placement, standard two-view mammograms were obtained to confirm tag placement. Placement accuracy was recorded by measuring the shortest distance, on either the mediolateral oblique (MLO) or craniocaudal (CC) view, from the tag to the intended target (e.g., target lesion, distortion, MCC) on the post-clip mammograms. Following surgical excision, a specimen radiograph was performed to confirm tag presence and location (
Figure 3a, 3b, 3c, and 4). Additionally, any cases of tag migration were documented, along with factors such as hematoma formation or lesion characteristics that may have influenced tag positioning. Data collection was conducted in compliance with institutional ethical guidelines, ensuring patient confidentiality and adherence to research standards.
Statistics
Confidence intervals (CIs) for proportions were calculated using the Wilson score method without continuity correction, which provides a reliable estimate for small sample sizes. Continuous variables, such as lesion size and patient age, were summarized using medians and interquartile ranges (IQR) due to the non-normal distribution of data. The accuracy of RFID placement was analyzed using descriptive statistics, with categorical variables compared using the chi-square test or Fisher’s exact test as appropriate. For cases requiring re-excision, logistic regression was considered to explore potential predictors, but the sample size was insufficient for robust multivariate modelling.
3. Results
During the study period, a total of 258 patients (mean age 61 years; range 17–91 years) underwent image-guided RFID tag localization. The median number of tags placed per patient was 1 (range 1–3). A single tag was placed in 223 patients (86.4%, 95% CI: 81.8%–90.1%), while 35 patients (13.6%, 95% CI: 9.9%–18.2%) had more than one tag inserted, resulting in a total of 297 tags placed. Among the 35 patients with multiple tags, 4 patients had 3 tags inserted, and 31 patients had 2 tags inserted, totaling 74 tags. Of these, 44 tags were used for bracketing, and 30 were used for targeting multiple breast lesions (e.g., multifocal or bilateral breast cancers).
The median size of the target lesion was 29 mm (range 0–57 mm). The distribution of target abnormalities and their size ranges are summarized in
Table 1. The types of targeted abnormalities are described in
Table 1. Mammographically occult lesions included MRI-detected abnormalities or lesions that demonstrated interval resolution/response to neoadjuvant chemotherapy, where marker clips were subsequently targeted for RFID placement. In cases of microcalcifications (MCC), lesion sizes ranged from single MCC clusters to the full anterior-to-posterior extent of multifocal pathological MCC.
Technical accuracy of RFID tag placement was achieved in 284/297 tags (95.6%, 95% CI: 92.5%–97.7%), defined as being within 10 mm of the target/lesion on post-clip mammograms. Of the 13 tags (4.4%, 95% CI: 2.3%–7.5%) inaccurately placed, 9 were inserted under ultrasound guidance, and 4 under stereotactic guidance. Among the 9 inaccurately placed tags under ultrasound guidance, 3 were affected by hematoma formation, impacting tag positioning, and 4 tags demonstrated migration. As this was a new technique at our institution, it is possible that inexperience contributed to the incorrect placement of the remaining 2 tags.
The 4 tags inaccurately placed under stereotactic guidance showed migration of up to 35 mm from the target. All cases of inaccurately placed tags were identified prior to surgery and discussed with the breast surgeons or during the regional MDT meeting. Two patients required additional wire placements on the day of surgery due to small, focal MCC.
A total of 273/297 tags (92%, 95% CI: 88.4%–94.7%) were present in the specimen radiograph, while 24/297 tags (8%, 95% CI: 5.3%–11.6%) were absent. Of the absent tags, 5/24 were placed in patients with more than one tag. Four of these 5 tags were placed in patients undergoing bracketing (2 tags), where the remaining tag was present in the specimen radiograph. The fifth tag was from a patient with multifocal disease where 3 tags were placed; the other 2 tags were present in the specimen radiograph.
Four patients with absent tags in the specimen radiograph required surgical re-excision, and all tags were retrieved. Overall, 21/258 patients (8%, 95% CI: 5.0%–11.9%) had positive or close surgical margins necessitating re-excision. Of these, 8 patients had more than one tag placed during localization (2 patients had 3 tags, and 6 patients had 2 tags). The need for re-excision was higher in patients with extensive microcalcifications or multifocal disease, where multiple tags were used to guide surgery.
4. Discussion
This study evaluates the use of the LOCalizer™ system for the localisation of non-palpable breast lesions, highlighting its accuracy, feasibility, and potential advantages over traditional wire-guided localisation (WL). To our knowledge, this is the second largest reported study assessing this technology in a cohort of 258 patients with 297 tags deployed.
The LOCalizer™ demonstrated a high technical accuracy rate of 95.6%, comparable to the standards set by WL and consistent with previously published data on RFID localisation [
5,
7]. Importantly, the decoupling of radiological and surgical scheduling offers significant logistical benefits, addressing a key limitation of WL, which requires same-day placement. This scheduling flexibility can improve patient experience and reduce the strain on healthcare systems. Furthermore, the Localizer reflector’s unique identification number facilitates precise bracketing of large nonpalpable breast lesions, enabling accurate surgical targeting.
However, our findings also reveal some limitations of the LOCalizer™ system. Migration accounted for the majority of inaccurate placements (8/13 cases), likely due to its smooth casing, learning curve effects, the wide tract created by the 12-gauge introducer needle, and limited anchoring within soft tissue [
5,
8]. While migration rates were low overall, this highlights the importance of operator experience and meticulous insertion technique to minimise complications. Additionally, the MRI void artifacts (2 cm), although smaller than those caused by Magseed (4 cm), may limit its use in certain patients, particularly those undergoing neoadjuvant systemic therapy and MRI surveillance [
5,
9]. These void signals are notably larger than those produced by radioactive seed localization (RSL) and SAVI SCOUT (less than 5 mm) [
10]. Finally the LOCalizer™ system is not currently licensed for deployment within axillary lymph nodes to facilitate targeted axillary dissection following neoadjuvant systemic therapy (NST).
Alternative wire-free localization techniques, such as RSL, Magseed, and SAVI SCOUT, offer the advantage of being deployed through narrower introducer needles (16-18 gauge), enhancing precision and facilitating easier insertion, particularly in dense breast tissue [
8,
9,
10].
However, the complex regulatory and safety requirements represent a significant limitation for the widespread adoption of radioactive seed localization (RSL) [
10]. Additionally, the use of Magseed necessitates the removal of all metal instruments from the surgical field during dissection [
9]. Direct comparisons between these wire-free localization technologies and the LOCalizer™ system, however, remain limited.
Our study’s findings are consistent with those of Malik et al., [
11] supporting the effectiveness of RFID technology in localizing non-palpable breast lesions. Malik et al. observed a re-excision rate of 17.27%, with higher rates when the RFID tags were placed outside the lesion (28.94%). We identified a re-excision rate of 8% in our cohort, with technical accuracy in 95.6% of RFID placements. Accurate tag placement within 10 mm of the lesion, achieved in the majority of cases, minimized positive margins and the need for re-excision. While migration of RFID tags or hematoma formation affected placement in a small subset of patients (4.4%), these challenges highlight the importance of operator experience and precision in tag placement. In the largest study reported in the literature, Lamb et al. detailed their experience with 1,013 RFID tags placed under imaging guidance in 848 patients, achieving a 98.4% successful localization rate and a 15.1% positive surgical margin rate.[
12]. Additionally, our findings demonstrated the utility of RFID tags in more complex scenarios, such as multifocal disease and bracketing, further underscoring the versatility of this technology as a reliable alternative to wire localization. Our re-excision rate is comparable to that reported for other wire-free localization technologies and appears lower than the rates associated with wire localization (WL) [
8,
9,
10].
A recent study found that RFID tag localization for nonpalpable breast lesions resulted in higher patient satisfaction compared to WL, attributed to greater comfort and reduced anxiety. [
13].
The limitations of our study include its retrospective design, which may introduce selection bias, and the single-center setting, which could limit the generalizability of our findings. Further analysis comparing RF tag insertion modalities (ultrasound vs. stereotactic) could provide insights into which techniques are more prone to inaccurate placement. The absence of a direct comparison with wire localization in a controlled setting further limits the ability to comprehensively assess the advantages of RFID technology.
A recent meta-analysis [
14] assessing the effectiveness of non-wired non-ionizing (NWNI) techniques in preoperative localization of non-palpable breast lesions, compared to traditional wire-guided localization (WGL), spanned 27 studies and encompassed 2,103 procedures. NWNI methods, including magnetic seeds (Magseed, MaMaLoc, MOLLI), radiofrequency tags (LOCalizer), and infrared tags (SAVI SCOUT), demonstrated excellent performance in lesion localization. The overall positive margin rate for NWNI techniques was 12%, indicating their potential to reduce re-excision rates, which were observed at 14%. Compared to WGL, NWNI techniques exhibited a lower positive margin rate (12% vs. 17%) and slightly reduced re-excision rates, though the difference was not statistically significant. An additional advantage of NWNI methods is the ability to place reflectors days in advance, enhancing scheduling flexibility and improving patient comfort. No serious complications were reported, and improved cosmetic outcomes were noted due to more precise lesion localization and minimized removal of healthy tissue. Despite these promising findings, further randomized trials are needed to confirm their long-term clinical benefits, cost-effectiveness, and overall impact on breast-conserving surgery outcomes.
The use of NWNI localization technologies has been increasing due to a global shift away from WL. Furthermore, the indications for preoperative localization of non-palpable breast lesions and axillary lymph nodes have expanded, driven not only by the rising incidence of screening-detected breast cancer but also by the de-escalation of breast cancer surgery after neoadjuvant NST and the need for localization in cases of ipsilateral in-breast tumor recurrence following previous BCS [
15,
16]. Recently, a new paradigm known as extreme oncoplastic BCS has been introduced for mastectomy candidates with large multifocal and multicentric tumors or extensive DCIS. This approach has expanded the eligibility for BCS by enabling the application of advanced surgical techniques to tumors that would have previously required mastectomy. Such procedures often necessitate bracketing, utilizing a minimum of two localization active markers to ensure precise tumor excision while preserving breast aesthetics. [
17].
Several barriers however hinder the universal adoption of NWNI localization technologies for breast cancer surgery. The high cost of devices, specialized equipment, and training limits accessibility, particularly in resource-limited settings. Implementing NWNI techniques also requires training for surgeons, radiologists, and operating room staff, with resistance to change and workflow adjustments posing challenges. Regulatory approvals and reimbursement issues further impact adoption, as some NWNI devices may not yet be widely approved or covered by healthcare systems and insurers. Additionally, the need for specialized detection systems and probes can create logistical barriers, particularly in centers lacking the necessary infrastructure. While NWNI technologies offer greater scheduling flexibility, integrating them into existing surgical and radiology workflows requires coordination. Surgeon and radiologist preferences also play a role, as many clinicians have extensive experience with WL and may be reluctant to transition unless clear advantages in efficiency and outcomes are demonstrated. Overcoming these barriers will require cost reduction, expanded training programs, regulatory support, and streamlined workflow integration to facilitate the broader adoption of NWNI localization methods.
Several advancements could enhance the performance and versatility of the LOCalizer™ system. One key area for improvement is the reduction of MRI-related voice signals, which can interfere with imaging quality. Optimizing the tag’s material composition or adjusting its resonance frequency could help minimize MRI artifacts, improving its compatibility for preoperative planning in patients requiring MRI-guided localization. Additionally, refining the tag design to make it even smaller could enhance patient comfort and further reduce the risk of migration, particularly in dense breast tissue. Another potential modification involves using a broader gauge needle for deployment, which could facilitate smoother insertion while minimizing tissue disruption. The development of an MRI-compatible deployment system would also expand the clinical utility of the LOCalizer™ in settings where MRI is the preferred imaging modality. Furthermore, obtaining regulatory approval for using RFID technology in axillary lymph node localization could significantly improve surgical precision in patients with node-positive breast cancer, providing a wire-free alternative to current localization techniques. These innovations could enhance the accuracy, usability, and scope of the LOCalizer™, making it a more adaptable tool for breast cancer surgery. To address migration, modifications to the tag’s surface texture or the addition of bioresorbable anchoring elements could enhance tissue integration and stability. The current polypropylene cap could be redesigned with microbarbs or a porous structure to encourage fibrosis around the tag, securing it more effectively in place. Another potential approach is the use of a hydrogel coating that expands slightly upon implantation, providing additional resistance to displacement. Additionally, a broader gauge needle for deployment could minimize tissue trauma at insertion, reducing the likelihood of tag movement.
5. Conclusions
The LOCalizer RFID system demonstrated a high accuracy rate for preoperative localization of breast lesions, presenting a viable alternative to WL. This technique improves surgical scheduling flexibility and enhances patient comfort. Comparative studies with other wire-free localization technologies, such as magnetic seeds and radar reflectors, are needed to determine the optimal approach for clinical practice.
Author Contributions
Conceptualisation, A. Malhotra., K.M.; methodology, C.M., A. Malhotra., and K.M.; validation, C.M., S.T., A. Menon; A.O.; and A. Malhotra; formal analysis, C.M.; investigation, C.M., S.T., A. Menon; A.O.; and A. Malhotra; resources, A. Malhotra; data curation, C.M., S.T., A. Menon; A.O.; and A. Malhotra; writing—original draft preparation, C.M.; A. Malhotra and K.M.; writing—review and editing, data extraction, C.M.; A. Malhotra; K.M.; S.T., A. Menon; and A.O.; supervision, K.M. and A. Malhotra. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed patient consent was waived for this de-identified retrospective review of existing data.
Data Availability Statement
Datasets generated during this study are publicly available in this open access publication without any restrictions.
Conflict of Interest
K.M. has received honoraria for offering academic and clinical advice to Merit Medical. The other authors declare no conflict of interest.
Ethics Statement
This retrospective audit study was approved by the radiology department, the clinical audit lead and registered with the quality improvement team.
References
- Cheang E, Ha R, Thornton CM, Mango VL. Innovations in image-guided preoperative breast lesion localization. The British journal of radiology. 2018 May;91(1085):20170740. [CrossRef]
- Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. New England Journal of Medicine. 2002 Oct 17;347(16):1233-41. [CrossRef]
- Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. New England Journal of Medicine. 2002 Oct 17;347(16):1227-32. [CrossRef]
- Houssami N, Macaskill P, Marinovich ML, Dixon JM, Irwig L, Brennan ME, Solin LJ. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. European journal of cancer. 2010 Dec 1;46(18):3219-32. [CrossRef]
- Tayeh S, Wazir U, Mokbel K. The evolving role of radiofrequency guided localisation in breast surgery: a systematic review. Cancers. 2021 Oct 5;13(19):4996. [CrossRef]
- National Breast Screening Program. Breast Screening Program: Standards [Internet]. NHS England: November 2023 [Published Nov 2023, cited 2024 January 12] Available from: https://www.gov.uk/government/collections/nhs-breast-screening-bsp-programme.
- Wazir U, Tayeh S, Perry N, Michell M, Malhotra A, Mokbel K. Wireless Breast Localization Using Radio-frequency Identification Tags: The First Reported European Experience in Breast Cancer. In Vivo. 2020 Jan-Feb;34(1):233-238. PMID: 31882483; PMCID: PMC6984090. [CrossRef]
- Hayes MK. Update on Preoperative Breast Localization. Radiol Clin North Am. 2017 May;55(3):591-603. PMID: 28411682. [CrossRef]
- Kasem I, Mokbel K. Savi Scout® Radar Localisation of Non-palpable Breast Lesions: Systematic Review and Pooled Analysis of 842 Cases. Anticancer Res. 2020 Jul;40(7):3633-3643. PMID: 32620602. [CrossRef]
- Ferreira HHJ, de Souza CD, Pozzo L, Ribeiro MS, Rostelato MECM. Radioactive Seed Localization for Nonpalpable Breast Lesions: Systematic Review and Meta-Analysis. Diagnostics (Basel). 2024 Feb 17;14(4):441. PMID: 38396480; PMCID: PMC10887864. [CrossRef]
- Malik M, Brookes P, Kasana MI, Tromans L, Audrey Chew WY, Green MJ. Radiofrequency as a method of localizing impalpable breast lesions. Surgeon. 2024 Oct;22(5):296-300. Epub 2024 Aug 23. PMID: 39179450. [CrossRef]
- Lamb LR, Gilman L, Specht M, D'Alessandro HA, Miles RC, Lehman CD. Retrospective review of preoperative radiofrequency tag localization of breast lesions in 848 patients. American Journal of Roentgenology. 2021 Sep 21;217(3):605-. [CrossRef]
- Pete R, Pinard C, Sirodot F, Molnar I, Dressaire M, Ginzac A, Abrial C, Durando X, Tekath M. Patient satisfaction with radio-frequency identification (RFID) tag localization compared with wire localization for nonpalpable breast lesions: the RFID trial. BMC Cancer. 2025 Jan 22;25(1):123. PMID: 39844175; PMCID: PMC11753160. [CrossRef]
- Garzotto F, Comoretto RI, Michieletto S, Franzoso G, Lo Mele M, Gregori D, Bonavina MG, Bozza F, Caumo F, Saibene T. Preoperative non-palpable breast lesion localization, innovative techniques and clinical outcomes in surgical practice: A systematic review and meta-analysis. Breast. 2021 Aug;58:93-105. Epub 2021 Apr 22. PMID: 33991806; PMC8481910
. [CrossRef]
- Shubeck SP, Morrow M, Dossett LA. De-escalation in breast cancer surgery. NPJ Breast Cancer. 2022 Feb 23;8(1):25. PMID: 35197478; PMCID: PMC8866473. [CrossRef]
- Tollan CJ, Pantiora E, Valachis A, Karakatsanis A, Tasoulis MK. A Systematic Review and Meta-Analysis on the Role of Repeat Breast-Conserving Surgery for the Management of Ipsilateral Breast Cancer Recurrence. Ann Surg Oncol. 2022 Oct;29(10):6440-6453. Epub 2022 Jul 18. PMID: 35849299
. [CrossRef]
- Vieira RADC, Paulinelli RR, de Oliveira-Junior I. Extreme oncoplasty: past, present and future. Front Oncol. 2024 Jan 30;13:1215284. PMID: 38352300; PMCID: PMC10862476
. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).