Submitted:
05 March 2025
Posted:
05 March 2025
You are already at the latest version
Abstract
Background: Optimal radiotherapy doses for Merkel cell carcinoma are unknown. Methods: After a PubMed literature search, we analyzed data by Equivalent Dose in 2-Gy fractions (EQD2). Results: 939/949 data were evaluable: 728/939 (77.5%) presented with localized disease, of which 171 were irradiated alone, with a median primary EQD2 of 50 (14.0-72.0) Gy2. Local recurrence (LR) was 23.4% (40/171). The remaining patients were controlled with a median EQD2 of 50 (23.3-72.0) Gy2. Thirteen patients were given definitive radiotherapy EQD2<50 vs >50 Gy2 to gross primaries: LR were 23.1% (3/13) vs 12.5% (1/8)(P=0.0004). Few patients received >60 Gy2. After adjuvant radiotherapy <50 vs >50 Gy2 to 156 primaries, LR were 18.8% (6/32) vs 12.8% (12/124); for <60 vs >60 Gy2, 15.5% (16/103) vs 8.7% (2/23)(P=0.52). LR after <50 Gy2 was 25% (3/12) for positive margins versus 17.4% (4/23) for negative margins; for >50 Gy2: 15% (3/20) versus 4.8% (3/62), respectively (P=0.36). Conclusions: For definitive radiotherapy, EQD2<50 Gy2 demonstrates significant higher LR than >50 Gy2 (P=0.0004). For adjuvant radiotherapy, a trend of higher LR with < 50 Gy2 was seen. Large prospective multicenter studies are required to define the optimal doses for definitive and adjuvant MCC treatment.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADMEC-O | Adjuvant immunotherapy with nivolumab versus observation |
| ADT | Androgen deprivation therapy |
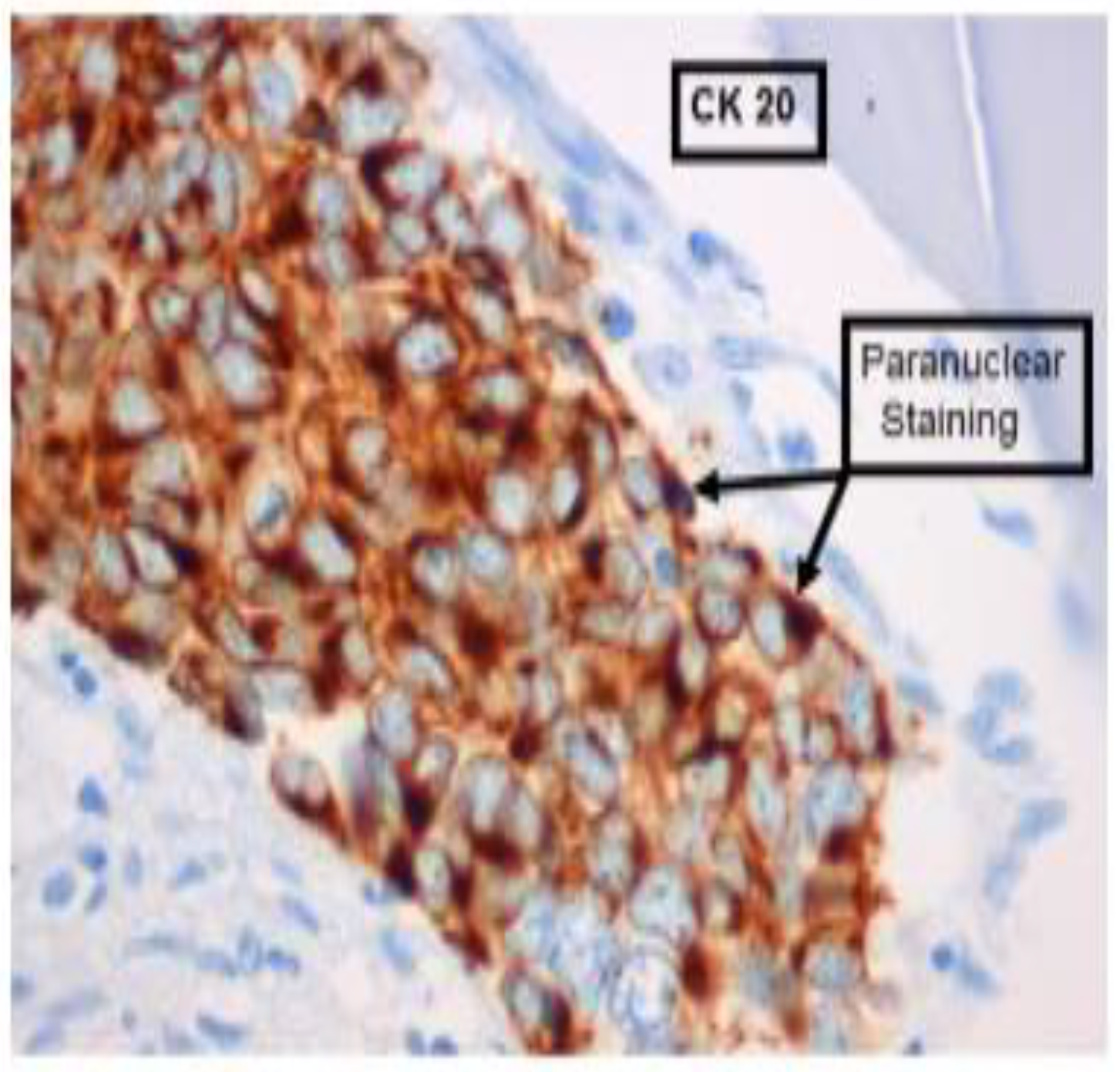
| CK | Cytokeratin |
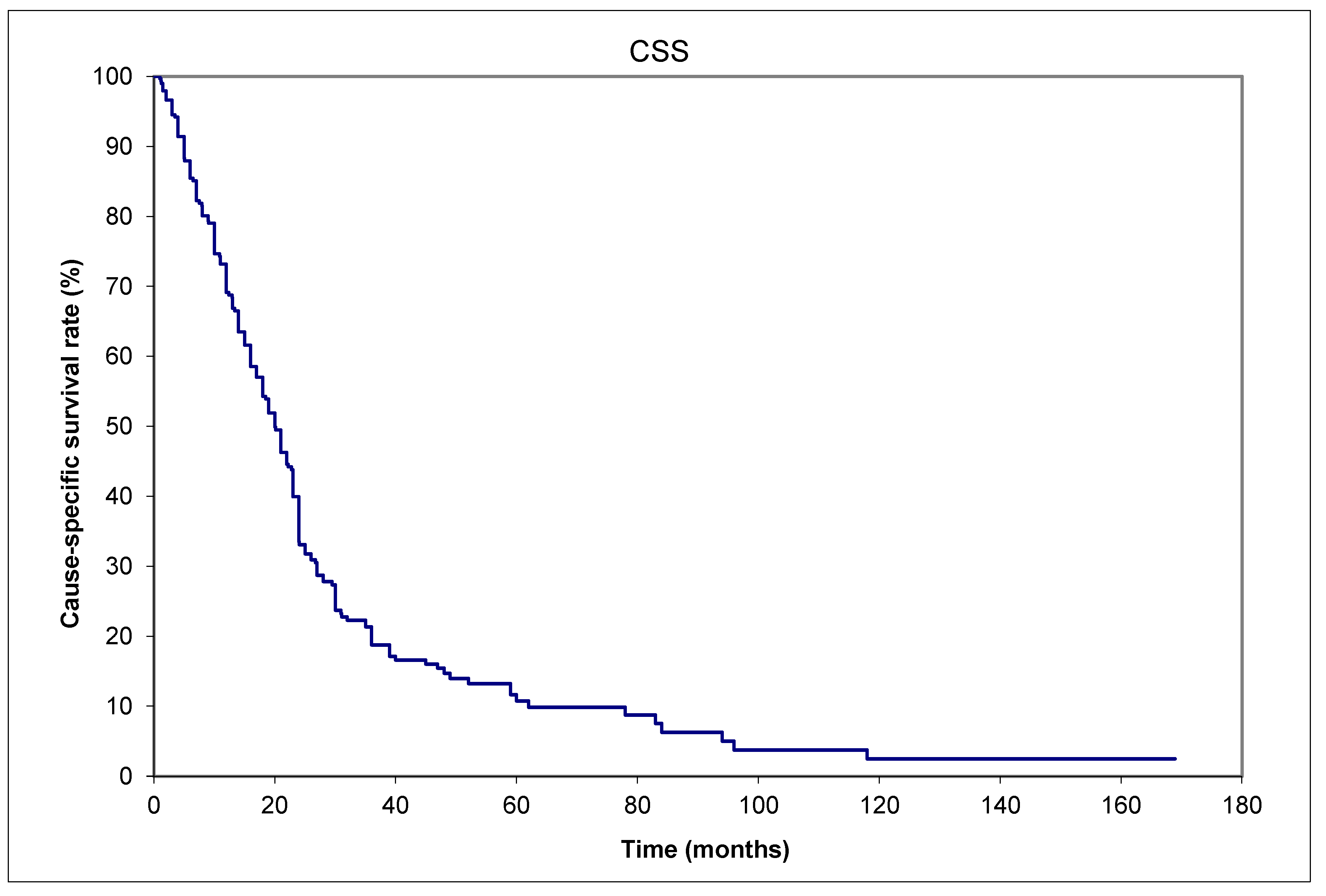
| CSS | Cause-specific survival |
| CT | Computerized tomography |
| DFS | Disease-free survival |
| DM | Distant metastases |
| LNM | Lymph node metastases |
| LRR | Locoregional recurrence |
| MCC | Merkel cell carcinoma |
| NCDB | National Cancer Database |
| OS | National Comprehensive Cancer Network |
| NCCN | Overall survival |
| PD-L1 | Programmed death-ligand 1 |
| PET | Positron emission tomography |
| PFS | Progression-free survival |
| SEER | Surveillance, Epidemiology, and End Results (SEER) program |
| SLNB | Sentinel lymph node biopsy |
| STING | Stimulator of interferon genes |
| TAM | Tumor-associated macrophages |
| ttPORT | Time to initiate postoperative radiotherapy |
References
- Tai, P.; Park, S.Y.; Nghiem, P.T. Pathogenesis, clinical features, and diagnosis of Merkel cell (neuroendocrine) carcinoma. In UpToDat; Canellos, G.P., Schnipper, L., Eds.; UpToDate: Waltham, MA, USA, 2025; www.uptodate.com (accessed on 1 March 2025).
- Tilling, T.; Moll, I. Which are the cells of origin in Merkel cell carcinoma? J Skin Cancer 2012, 2012, 680410. [Google Scholar] [CrossRef] [PubMed]
- Tai, P.; Au, J. Skin cancer management – updates on Merkel cell carcinoma. Ann Transl Med 2018, 6, 282. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.K.; Toker, C.; Nedwich, A.; Zaman, A.N. Unusual cutaneous carcinoma with features of small cell (oat cell-like) and squamous cell carcinomas. A variant of malignant Merkel cell neoplasm. Am J Dermatopathol 1982, 4, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Raaf, J.H.; Urmacher, C.; Knapper, W.K.; Shiu, M.H.; Cheng, E.W. Trabecular (Merkel cell) carcinoma of the skin. Treatment of primary, recurrent, and metastatic disease. Cancer 1986, 57, 178–182. [Google Scholar] [CrossRef]
- Ratner, D.; Nelson, B.R.; Brown, M.D.; Johnson, T.M. Merkel cell carcinoma. J Am Acad Dermatol 1993, 29 (2 Pt 1), 143–156. [Google Scholar] [CrossRef] [PubMed]
- Sunshine, J.C.; Jahchan, N.S.; Sage, J.; Choi, J. Are there multiple cells of origin of Merkel cell carcinoma? Oncogene 2018, 37, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Nirenberg, A.; Steinman, H.; Dixon, J.; Dixon, A. Merkel cell carcinoma update: the case for two tumours. J Eur Acad Dermatol Venereol 2020, 34, 1425–1431. [Google Scholar] [CrossRef] [PubMed]
- Yiengpruksawan, A.; Coit, D.G.; Thaler, H.T.; Urmacher, C.; Knapper, W.K. Merkel cell carcinoma. Prognosis and management. Arch Surg 1991, 126, 1514–1519. [Google Scholar] [CrossRef] [PubMed]
- Victor, N.S.; Morton, B.; Smith, J.W. Merkel cell cancer: is prophylactic lymph node dissection indicated? Am Surg 1996, 62, 879–882. [Google Scholar] [PubMed]
- Queirolo, P.; Gipponi, M.; Peressini, A.; Raposio, E.; Vecchio, S.; Guenzi, M.; Sertoli, M.R.; Santi, P.; Cafiero, F. Merkel cell carcinoma of the skin. Treatment of primary, recurrent and metastatic disease: review of clinical cases. Anticancer Res 1997, 17, 2339–2342. [Google Scholar] [PubMed]
- Gillenwater, A.M.; Hessel, A.C.; Morrison, W.H.; Burgess, M.; Silva, E.G.; Roberts, D.; Goepfert, H. Merkel cell carcinoma of the head and neck: effect of surgical excision and radiation on recurrence and survival. Arch Otolaryngol Head Neck Surg 2001, 127, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Gunaratne, D.A.; Howle, J.R.; Veness, M.J. Sentinel lymph node biopsy in Merkel cell carcinoma: a 15-year institutional experience and statistical analysis of 721 reported cases. Br J Dermatol 2016, 174, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Santamaria-Barria, J.A.; Boland, G.M.; Yeap, B.Y.; Nardi, V.; Dias-Santagata, D.; Cusack, J.C., Jr. Merkel cell carcinoma: 30-year experience from a single institution. Ann Surg Oncol 2013, 20, 1365–1373. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.C.; Ugurel, S.; Leiter, U.; Meier, F.; Gutzmer, R.; Haferkamp, S.; Zimmer, L.; Livingstone, E.; Eigentler, T.K.; Hauschild, A.; et al. DeCOG: Adjuvant immunotherapy with nivolumab versus observation in completely resected Merkel cell carcinoma (ADMEC-O): disease-free survival results from a randomised, open-label, phase 2 trial. Lancet 2023, 402, 798–808. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, E.L.; Meier, P. Non-parametric estimation from incomplete observations. J Am Stat Assoc 1958, 53, 457–482. [Google Scholar] [CrossRef]
- Cox, D.R. Regression Models and Life-Tables. J Royal Statistical Soc 1972, 34, 187–220. [Google Scholar] [CrossRef]
- Coggshall, K.; Tello, T.L.; North, J.P.; Yu, S.S. Merkel cell carcinoma: An update and review: Pathogenesis, diagnosis, and staging. J Am Acad Dermatol 2018, 78, 433–442. [Google Scholar] [CrossRef]
- Tai, P.; Park, S.Y.; Nghiem, P.T.; Silk, A. Staging and treatment, and surveillance of locoregional Merkel cell carcinoma. In UpToDate; Canellos, G.P., Schnipper, L., Eds.; UpToDate: Waltham, MA, USA, 2024; www.uptodate.com (accessed on 15 May 2024).
- Park, S.Y.; Nghiem, P.T.; Tai, P.; Silk, A. Treatment of recurrent and metastatic Merkel cell carcinoma. In UpToDate; Canellos, G.P., Schnipper, L., Eds.; UpToDate: Waltham, MA, USA, 15 May 2024; www.uptodate.com (accessed on 14 March 2025).
- National Comprehensive Cancer Network (NCCN) guideline. www.nccn.org (accessed on 15 January 2025).
- Ginsburg, K.B.; Bell, S.; Bukavina, L.; Schober, J.P.; Magee, D.; Kutikov, A. The Phenomenon of “Therapeutic” Nodal Yield at Cystectomy for Bladder Cancer: Do Not Discount the Will Rogers Effect. Eur Urol Open Sci 2022, 47, 43–47. [Google Scholar] [CrossRef] [PubMed]
- CASCADE | English meaning - Cambridge Dictionary.
- Miranda, I.; Jahan, N.; Shevde, L.A. The metastatic cascade through the lens of therapeutic inhibition. Cell Rep Med 2025, 6, 1101872. [Google Scholar] [CrossRef]
- Kaufman, H.L.; Russell, J.S.; Hamid, O.; Bhatia, S.; Terheyden, P.; D’Angelo, S.P.; Shih, K.C.; Lebbé, C.; Milella, M.; Brownell, I.; et al. Updated efficacy of avelumab in patients with previously treated metastatic Merkel cell carcinoma after ≥1 year of follow-up: JAVELIN Merkel 200, a phase 2 clinical trial. J Immunother Cancer 2018, 6, 7. [Google Scholar] [CrossRef]
- Kaufman, H.L.; Russell, J.; Hamid, O.; Bhatia, S.; Terheyden, P.; D’Angelo, S.P.; Shih, K.C.; Lebbé, C.; Linette, G.P.; Milella, M.; et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multi-center, single-group, open-label, phase 2 trial. Lancet Oncol 2016, 17, 1374–1385. [Google Scholar] [CrossRef] [PubMed]
- Tai, P.T.H.; Yu, E.; Winquist, E.; Hammond, A.; Stitt, L.; Tonita, J.; Gilchrist, J. Chemotherapy in neuroendocrine / Merkel cell carcinoma of the skin [MCC]: case series and review of 204 cases. J Clin Oncol 2000, 18, 2493–2499. [Google Scholar] [CrossRef] [PubMed]
- Nayak, A.L.; Pickett, A.T.; Delisle, M.; Dingley, B.; Mallick, R.; Hamilton, T.; Stuart, H.; Talbot, M.; McKinnon, G.; Jost, E.; et al. Survival of Patients With Head and Neck Merkel Cell Cancer: Findings From the Pan-Canadian Merkel Cell Cancer Collaborative. JAMA Netw Open 2023, 6, e2344127. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, M.B.; Gaskins, J.; Wall, W.; Tennant, P.; Bumpous, J.; Dunlap, N. Immune status and the efficacy of radiotherapy on overall survival for patients with localized Merkel cell carcinoma: An analysis of the National Cancer Database. J Med Imaging Radiat Oncol 2020, 64, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Nudelman, N.T.; Ekhator, N.; Rothschild, M.; Wladis, E.J. A SEER program study of survival trends in Merkel cell carcinoma of the eyelid: 2000-2019. Orbit 2024, 43, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Alexander, N.A.; Schaub, S.K.; Goff, P.H.; Hippe, D.S.; Park, S.Y.; Lachance, K.; Bierma, M.; Liao, J.J.; Apisarnthanarax, S.; Bhatia, S.; et al. Increased risk of recurrence and disease-specific death following delayed postoperative radiation for Merkel cell carcinoma. J Am Acad Dermatol 2024, 90, 261–268. [Google Scholar] [CrossRef]
- Desai, A.D.; Behbahani, S.; Samie, F.H. Predictors of time to definitive surgery and survival in Merkel cell carcinoma: analysis of the US National Cancer Database. Clin Exp Dermatol 2022, 47, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Alexander, N.A.; Schaub, S.K.; Goff, P.H.; Hippe, D.S.; Park, S.Y.; Lachance, K.; Bierma, M.; Liao, J.J.; Apisarnthanarax, S.; Bhatia, S.; et al. Increased risk of recurrence and disease-specific death following delayed postoperative radiation for Merkel cell carcinoma. J Am Acad Dermatol 2024, 90, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Clinical trials for Merkel Cell Carcinoma.
- https://www.fredhutch.org.
- https://www.mskcc.org.
- https://my.clevelandclinic.org.
- https://www.mayoclinic.org.
- https://www.skincancer.org.
- touchONCOLOGY-D-23-00021.pdf.
- 1146P Updated results from POD1UM-201: A phase II study of retifanlimab in patients with advanced or metastatic Merkel cell carcinoma (MCC) - Annals of Oncology.
- Treatment Clinical Trials for Merkel Cell Cancer - NCI.
- Silk, A.W.; Davar, D. Tumor-Associated Macrophages in Merkel Cell Carcinoma: Old Balances, New Checks. Clin Cancer Res 2024, OF1–OF3. [Google Scholar] [CrossRef] [PubMed]
- Pulliam, T.; Jani, S.; Goff, P.H.; Bhakuni, R.; Tabachnick-Cherny, S.; Smythe, K.; Seaton, B.W.; Tachiki, L.; Kulikauskas, R.; Church, C.; et al. Intratumoral STING agonist reverses immune evasion in PD-(L)1-refractory Merkel cell carcinoma: mechanistic insights from detailed biomarker analyses. J Immunother Cancer 2024, 12, e009803. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick-Cherny, S.; Pulliam, T.; Church, C.; Koelle, D.M.; Nghiem, P. Polyomavirus-driven Merkel cell carcinoma: Prospects for therapeutic vaccine development. Mol Carcinog 2020, 59, 807–821. [Google Scholar] [CrossRef] [PubMed]
- Joseph, K.; Wong, J.; Abraham, A.; Zebak, J.; Patel, A.; Jones Thachuthara, A.; Iqbal, U.; Pham, T.M.; Menon, A.; Ghosh, S.; et al. Patterns and predictors of relapse in Merkel cell carcinoma: Results from a population-based study. Radiother Oncol 2022, 166, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Tai, P.; Assouline, A.; Koul, R.; Dubey, A.; Lian, J.; Yu, E.; Veness, M.; Joseph, K. Merkel cell carcinoma (MCC) of the skin: comprehensive analysis of radiation (RT) doses of aggregate patient data from literature. Radiother Oncol 2024, 198, 74–75. [Google Scholar]
- Joseph, K.; Tai, P.; Veness, M.; Lian, J.; Assouline, A.; Koul, R.; Dubey, A.; Park, S.Y.; Yu, E. Merkel cell carcinoma (MCC) of the skin: when is local radiotherapy (RT) without nodal coverage adequate? Comprehensive analysis of aggregate patient data from literature. Radiother Oncol 2024, 198, 75. [Google Scholar]
| Aggregated data from | Saskatchewan (Canada) | 13 (16%) | |||
| Alberta (Canada) | 17 (22%) | ||||
| London, Ontario (Canada) | 15 (19%) | ||||
| Windsor/Ontario, Canada | 5 (6%) | ||||
| Amiens (France) | 9 (11%) | ||||
| Westmead, New South Wales (Australia) | 20 (25%) | ||||
| Baseline characteristics | Age: | median 78 (range: 47-95) years | |||
| Sex: | 29 males & 50 females | ||||
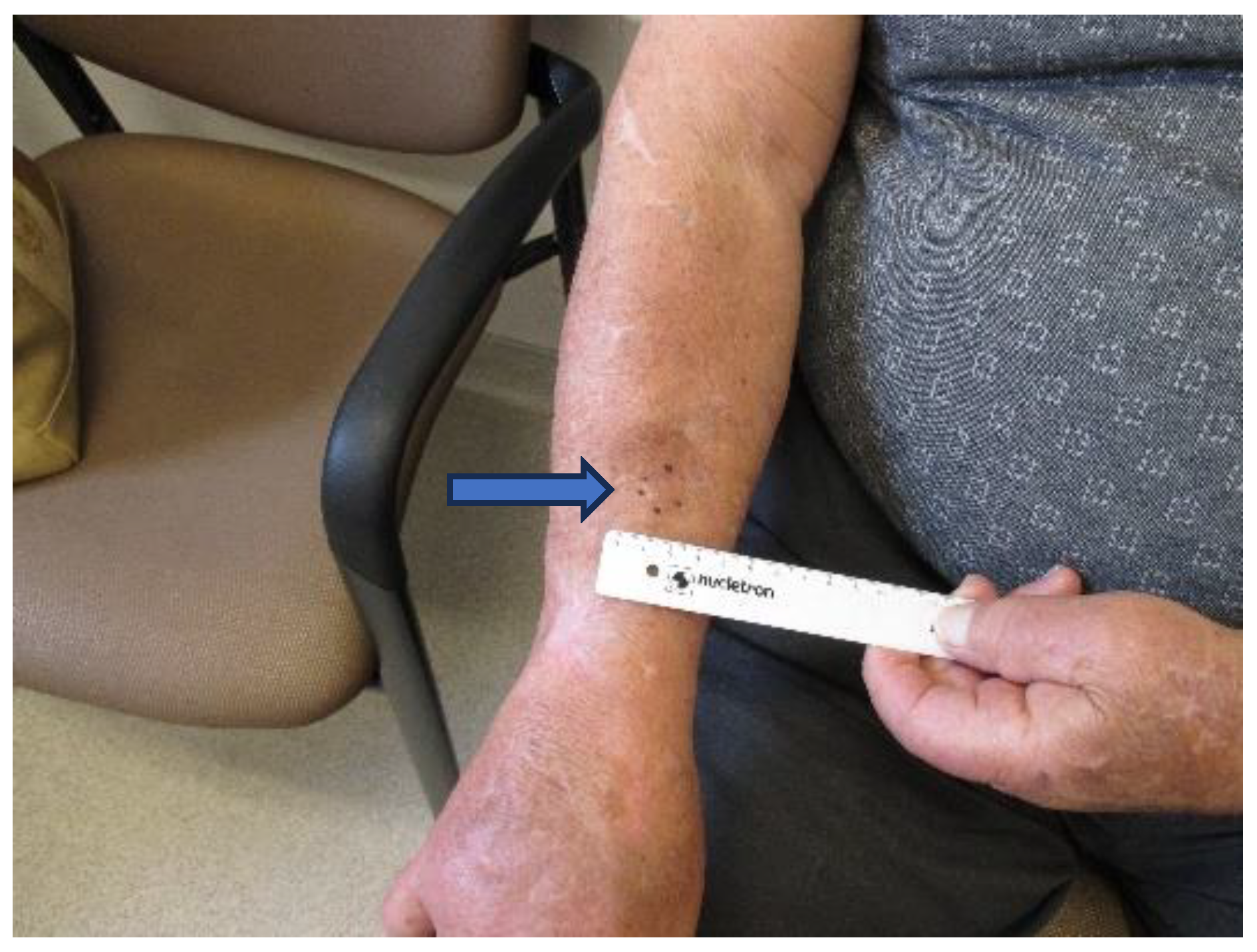
| Size of primary tumor: | median 2.5 (range: 0.2-17) cm | ||||
| Initial stages | Local | Nodal | Distant metastases | Unknown | |
| Clinical | 42 (53%) | 28 (35%) | 8 (10%) | 1 (1%) | |
| Pathological | 35 (44%) | 35 (44%) | 8 (10%) | 1 (1%) | |
| Primary site | Head and neck | 35 (44%) | |||
| Limb (upper or lower) | 23 (29%) | ||||
| Trunk | 13 (16%) | ||||
| Unknown primary, presented with nodes only | 8 (10%) | ||||
| Timing of nodal metastases (patient number = 47) | Before distant metastases diagnosis | 31/47 (66%) | |||
| Within 1 month of distant metastases diagnosis | 10/47 (21%) | ||||
| After distant metastases diagnosis | 1/47 (2%) | ||||
| Unknown time relative to distant metastases | 5/47 (11%) | ||||
| Treatment of localized disease at presentation (patient number = 43) | Surgery | 24/43 (56%) | |||
| Surgery+Radiotherapy | 11/43 (26%) | ||||
| Surgery+Chemotherapy | 1/43 (2%) | ||||
| Radiotherapy alone | 4/43 (9%) | ||||
| Radiotherapy+Chemotherapy | 1/43 (2%) | ||||
| None | 2/43 (5%) | ||||
| Treatment of nodal metastases at presentation (patient number = 28) | Surgery | 6/28 (21%) | |||
| Surgery+Radiotherapy | 7/28 (25%) | ||||
| Surgery+Radiotherapy+Chemotherapy | 2/28 (7%) | ||||
| Radiotherapy alone | 13/28 (46%) | ||||
| Treatment of distant metastases at presentation (patient number = 8) | Radiotherapy+Chemotherapy | 3/8 (38%) | |||
| Chemotherapy alone | 2/8 (25%) | ||||
| None | 3/8 (38%) | ||||
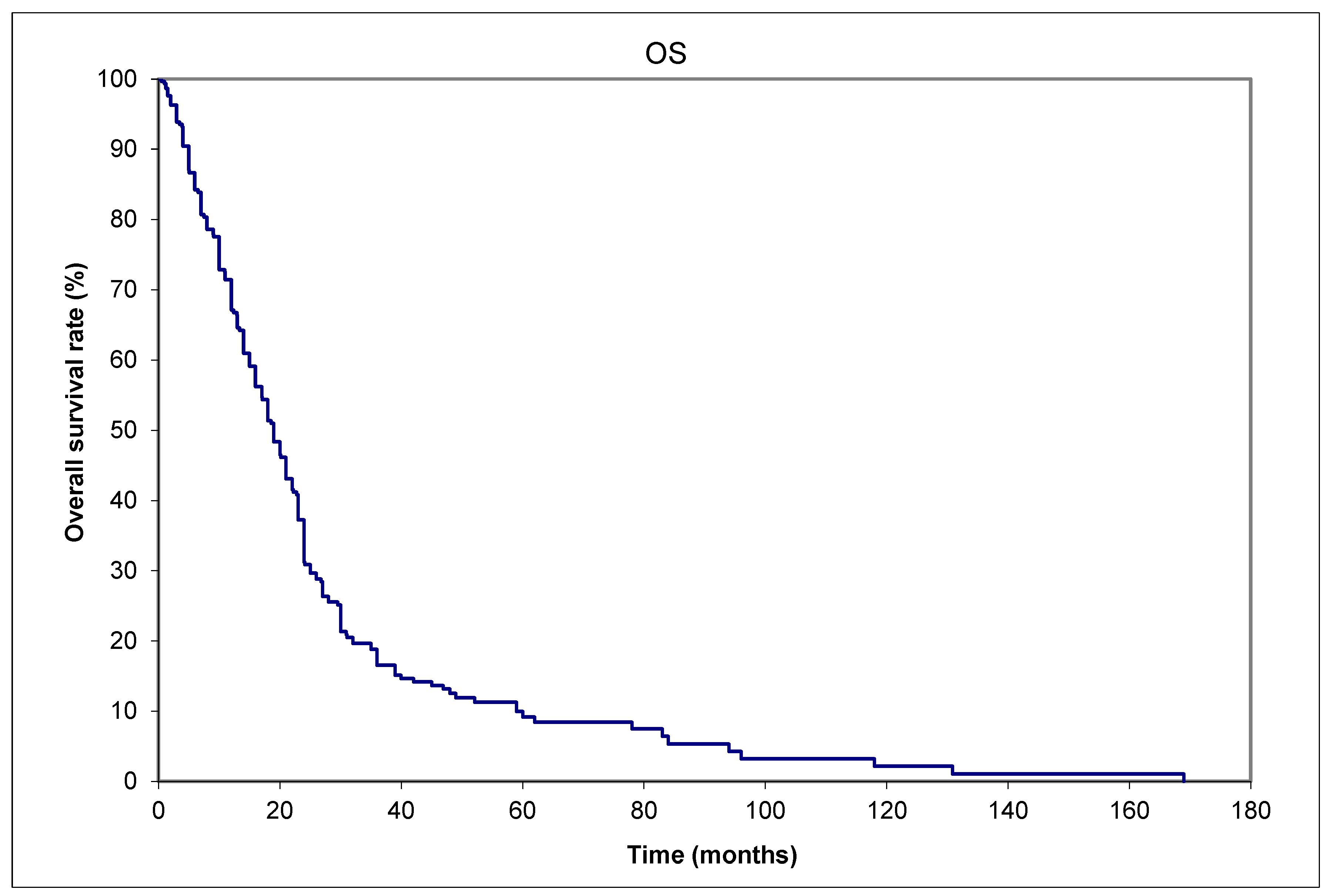
| Final vital status | Alive | 8/79 (10%) | |||
| Dead | 71/79 (90%) | ||||
| Cause of death among those expired (patient number = 71) | Merkel cell carcinoma | 65/71 (92%) | |||
| Intercurrent disease | 6/71 (8%) | ||||
| Variable | Hazard Ratio | (95% Confidence interval) | P values | |
| Age: | 60 | Reference variable | ||
| 70 | 0.90 | (0.64-1.26) | 0.50 | |
| 80 | 1.06 | (0.66-1.68) | 0.82 | |
| 90 | 1.75 | (0.89-3.46) | 0.11 | |
| Sex: | Male | 0.87 | (0.54-1.42) | 0.59 |
| Female | Reference variable | |||
| Chemotherapy: | Yes | 0.56 | (0.19-1.62) | 0.29 |
| No | Reference variable | |||
| Clinical stage: | Localized disease | 2.53 | (1.21-5.28) | 0.013 |
| Primary ≤1 cm | Reference variable | |||
| Primary >1 cm | 1.32 | (0.61-2.89) | 0.49 | |
| Nodal metastases | 3.27 | (1.85-5.78) | <0.001 | |
| Distant metastases | 21.42 | (7.15-64.21) | <0.001 | |
| Previous irradiation: | Yes | 2.95 | (0.90-9.61) | 0.073 |
| No | Reference variable | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





