Submitted:
02 February 2025
Posted:
03 February 2025
You are already at the latest version
Abstract
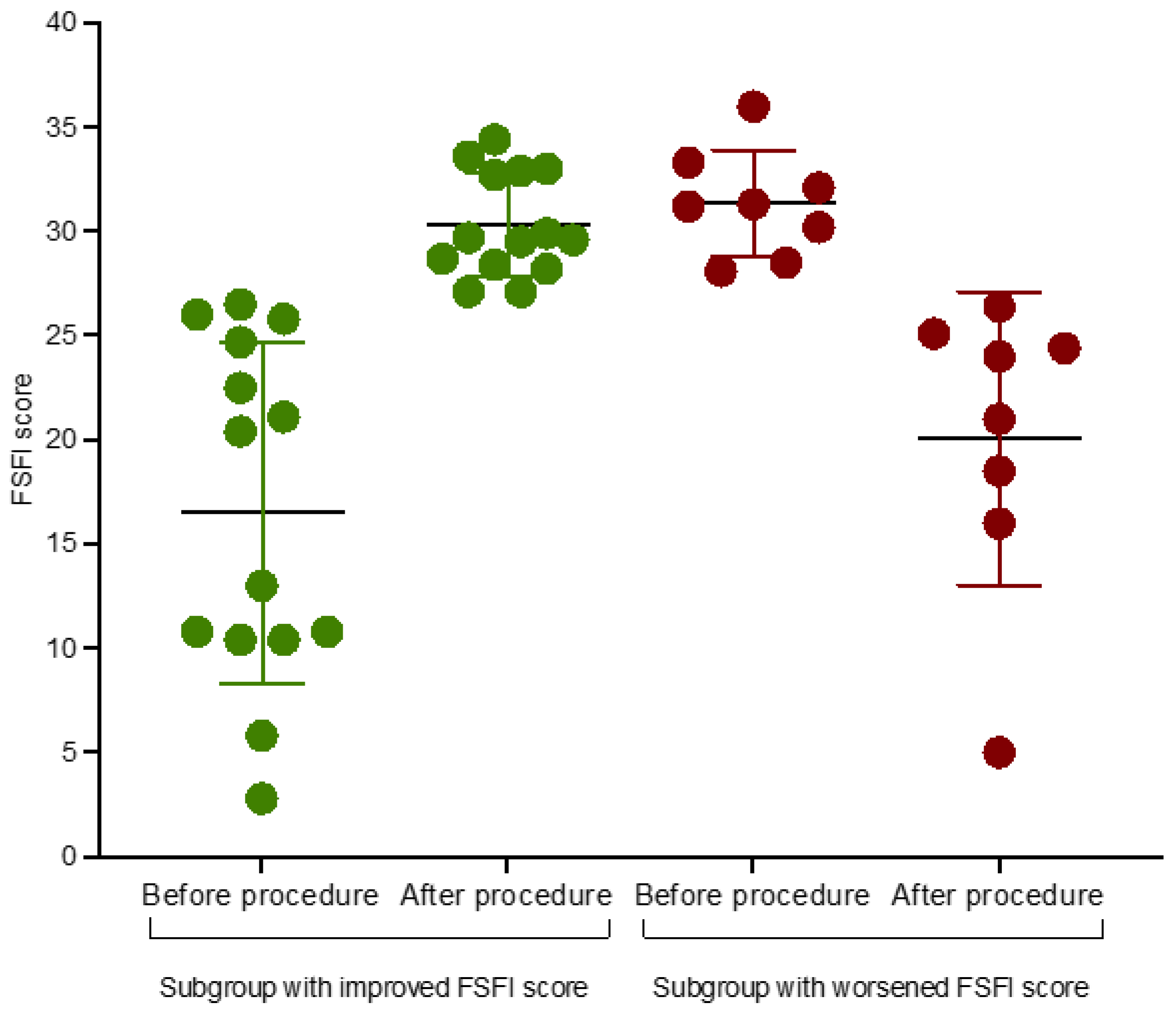
Background/Objectives: Cervical cancer is one of the most common cancers in women worldwide, with the leading risk factor being high-risk human papillomavirus (HR-HPV); persistent HR-HPV infection leads to cervical dysplasia [1,2,3,4]. With early screening and, if indicated, therapeutic strategies such as loop electrosurgical excision procedure (LEEP) and large loop excision of transformation zone (LLETZ), morbidity and mortality in this population is decreasing. However, it is suspected that these procedures may have an impact on sexual dysfunction. Methods: In this single-centre prospective longitudinal study, we recruited patients with high-grade squamous intraepithelial lesion (HSIL) and HR-HPV positive result and evaluated the impact of LEEP/LLETZ on their sexual life and psychological well-being. All participants received two questionnaires - the Female Sexual Function Index (FSFI) and the Brief Index of Sexual Function-Women (BISF-W) – after diagnosis, before treatment and three months after the procedure. Results: A total of 40 women aged 28 to 55 years were enrolled. The study showed no significant changes in both FSFI (F(1,39) = 0.774; p = 0.38) and BISF-W total scores (F(1,39) The study revealed that 32/40 (80%) of participants based on FSFI either exhibited no change or improved sexual function. Only 3/40 (7.5%) mentioned sexual dysfunction after procedures. The study also found that the mean score for sexual function based on the FSFI was 2.80; p = 0.102. Conclusions: The findings suggest that patients qualified for LEEP/LLETZ can be reassured that the anxiety they experience prior to treatment is not necessarily justified. This provides evidence on the safety of loop excision procedures in terms of sexual functioning after the procedure. Nevertheless, further studies are needed to analyse potential risk factors that may contribute to adverse sexual outcomes and to achieve a better understanding of this complex problem.
Keywords:
1. Introduction
2. Materials and Methods
2.1. FSFI
2.2. BISF-W
2.3. Statistical Analysis
3. Results
3.1. Primary Outcome
3.2. Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HSIL | high-grade squamous intraepithelial lesions |
| CC | cervical cancer |
| HR HPV | high-risk human papillomavirus |
| LEEP | loop electrosurgical excision procedure |
| LLETZ | large loop excision of transformation zone |
| HPV | human papillomavirus |
| FSFI | female sexual function index |
| BISF-W | brief index of sexual function-women |
| FSAD | function and sexual arousal disorders |
| IQR | interquartile range |
References
- Bhatla, N.; Aoki, D.; et al. Cancer of the cervix uteri: 2021 update. Int J Gynaecol Obstet. 2021, 155, 28–44. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Koshiol, J.; Lindsay, L. Persistent human papillomavirus infection and cervical neoplasia: a systematic review and meta- analysis. Am. J. Epidemiol 2008, 168, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Human Papillomavirus (HPV) Infection - STI Treatment Guidelines. Available online: https://www.cdc.gov/std/treatment-guidelines/hpv.htm (accessed on 8 December 2022).
- Kyrgiou, M.; Arbyn, M.; et al. Cervical screening: ESGO-EFC position paper of the European Society of Gynaecologic Oncology (ESGO) and the European Federation of Colposcopy (EFC). Br. J. Cancer 2020, 123, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Sharp, L.; Cotton, S; et al. Factors associated with psychological distress following colposcopy among women with low- grade abnormal cervical cytology: a prospective study within the Trial Of Management of Borderline and Other Low-grade Abnormal smears (TOMBOLA). Psychooncology 2013, 22, 368–380. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.S.; Kothali-Tarwar, S.; et al. Cross-sectional study estimating the psychosocial impact of genital warts and other anogenital diseases in South Korea. BMJ Open 2019, 9, e025035. [Google Scholar] [CrossRef]
- Sparić, R.; Papoutsis, D.; et al. Psychosexual outcomes in women of reproductive age at more than two-years from excisional cervical treatment - a cross-sectional study. J. Psychosom. Obstet. Gynecol 2019, 40, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Michaan, N.; Loboda, N.; et al. The Effect of Cervical Conization on Women’s’ Sexual Function and Psychological Health, A Prospective Observational Study. J Sex Med 2022, 19, 257–262. [Google Scholar] [CrossRef]
- Inna, N.; Phianmongkhol, Y.; et al. Sexual function after loop electrosurgical excision procedure for cervical dysplasia. J. Sex. Med 2010, 7, 1291–1297. [Google Scholar] [CrossRef]
- Giovannetti, O.D.; Tomalty, D.; et al. Self-Report Assessment of Sexual Function After LEEP in Women who Report Negative Outcomes. J. Sex. Med 2022, 19, S15–S16. [Google Scholar] [CrossRef]
- Gaurav, A.; Verma, P.; et al. Psychosexual Health After Loop Electrosurgical Excision Procedure (LEEP) among women with Cervical Intraepithelial Neoplasia in North Indian tertiary Centre: A Prospective Observational Study. Preprint, 2022. [CrossRef]
- Hellsten, C.; Lindqvist, P.G.; et, al. A longitudinal study of sexual functioning in women referred for colposcopy: a 2-year follow up. BJOG 2008, 115, 205–211. [Google Scholar] [CrossRef]
- Serati, M.; Salvatore, S.; et al. The impact of the loop electrosurgical excisional procedure for cervical intraepithelial lesions on female sexual function. J. Sex. Med 2010, 7, 2267–2272. [Google Scholar] [CrossRef]
- Rosen, R.; Brown, C.; et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J. Sex Marital Ther 2000, 26, 191–205. [Google Scholar] [CrossRef] [PubMed]
- Meston, C.M. Validation of the Female Sexual Function Index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J. Sex Marital Ther 2003, 29, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Munarriz, R.; Talacoub, L.; et al. Androgen replacement therapy with dehydroepiandrosterone for androgen insufficiency and female sexual dysfunction: androgen and questionnaire results. J. Sex Marital Ther 2002, 28, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.F.; Rosen, R.C.; et al. Self-report assessment of female sexual function: psychometric evaluation of the Brief Index of Sexual Functioning for Women. Arch. Sex. Beha. 1994, 23, 627–643. [Google Scholar] [CrossRef]
- Goldfarb, S.; Baron, S.R.; et al. Female Sexuality and Sexual Function. In Women Health, 2nd ed.; Goldman, M.B., Troisi, R., Eds.; Elsevier Inc.: Amsderdam, Netherlands, 2013; Volume 23, pp. 347–357. [Google Scholar] [CrossRef]
- Sikorska, M.; Pawłowska, A.; et al. The Impact of HPV Diagnosis and the Electrosurgical Excision Procedure (LEEP) on Mental Health and Sexual Functioning: A Systematic Review. Cancers, 2023, 15, 2226. [Google Scholar] [CrossRef] [PubMed]
- Bahadur, A.; Mahamood, M.; et al. Comparison of Sexual Function after Thermal Ablation Versus Loop Electrosurgical Excision Procedure (LEEP) for Cervical Intraepithelial Neoplasia (CIN 2 and 3): A Randomized Controlled Trial. Asian Pac J Cancer Prev 2024, 25, 1699–1705. [Google Scholar] [CrossRef]
- Drolet, M.; Brisson, M.; et al. The psychosocial impact of an abnormal cervical smear result. Psychooncology 2012, 21, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, A.; Tapper, A.M.; et al. Health-related quality of life and perception of anxiety in women with abnormal cervical cytology referred for colposcopy: An observational study. Eur. J. Obstet. Gynecol. Reprod. Biol 2013, 169, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Kwan, T.T.; Cheung, A.N.; et al. Psychological burden of testing positive for high-risk human papillomavirus on women with atypical cervical cytology: A prospective study. Acta Obstet. Gynecol. Scand 2011, 90, 445–451. [Google Scholar] [CrossRef] [PubMed]
- McBride, E.; Marlow, L.A.; Forster, A.S.; et al. Anxiety and distress following receipt of results from routine HPV primary testing in cervical screening: The psychological impact of primary screening (PIPS) study. Int. J. Cancer 2020, 146, 2113. [Google Scholar] [CrossRef] [PubMed]
- McCaffery, K.; Waller, J.; et al. Social and psychological impact of HPV testing in cervical screening: a qualitative study. Sex Transm Infect 2006, 82, 169–74. [Google Scholar] [CrossRef] [PubMed]
- Giannella, L.; Mfuta, K.; et al. Loop electrosurgical excision procedure as a life event that impacts on postmenopausal women. J. Obstet. Gynaecol 2013, 39, 842–848. [Google Scholar] [CrossRef]
- Lee Mortensen, G.; Adeler, A.L. Qualitative study of women’s anxiety and information needs after a diagnosis of cervical dysplasia. J. Public Health (Bangkok. 2010, 18, 473–482. [Google Scholar] [CrossRef]
- Marlow, L.A.V.; McBride, E.; et al. Patterns of anxiety and distress over 12 months following participation in HPV primary screening. Sex. Transm. Infect 2022, 98, 255–261. [Google Scholar] [CrossRef]
- McCaffery, K.; Irwig, L. Australian women’s needs and preferences for information about human papillomavirus in cervical screening. J. Med. Screen 2005, 12, 134–141. [Google Scholar] [CrossRef]
- Bennett, K.F.; Waller, J.; et al. The psychosexual impact of testing positive for high-risk cervical human papillomavirus (HPV): A systematic review. Psychooncology, 2019, 28, 1959–1970. [Google Scholar] [CrossRef] [PubMed]
- Caruso, S.; Bruno, M.T.; et al. Sexual Behavior of Women With Diagnosed HPV. J Sex Marital Ther, 2019, 45, 569–573. [Google Scholar] [CrossRef]
- Perrin, K.K.; Daley, E.M.; et al. Women’s reactions to HPV diagnosis: insights from in-depth interviews. Women Health, 2006, 43, 93–110. [Google Scholar] [CrossRef] [PubMed]
- Sellors, J.W.; Karwalajtys, T.L.; et al. Survey of HPV in Ontario Women Group. Incidence, clearance and predictors of human papillomavirus infection in women. CMAJ, 2003, 168, 421–5. [Google Scholar] [PubMed]
- Taberna, M.; Inglehart, R.C.; et al. Significant changes in sexual behavior after a diagnosis of human papillomavirus-positive and human papillomavirus-negative oral cancer. Cancer 2017, 123, 1156–1165. [Google Scholar] [CrossRef] [PubMed]
- Nagele, E.; Reich, O.; et al. Sexual Activity, Psychosexual Distress, and Fear of Progression in Women With Human Papillomavirus-Related Premalignant Genital Lesions. The Journal of Sexual Medicine 2016, 13, 253–259. [Google Scholar] [CrossRef] [PubMed]
| Dimension |
Before excision procedure (n= 40) |
After excision procedure (n=40) |
F | p-value |
| Desire (mean ± SD) Median |
3.8 ± 1.3 3.6 |
3.8 ± 1.2 4.2 |
F (1,39) = 0.003 | p=0.842 |
| Arousal (mean ± SD) Median |
4.0 ± 1.9 4.5 |
4.3 ± 1.5 4.7 |
F (1,39) = 0.611 | p=0.439 |
| Lubrication (mean ± SD) Median |
4.2 ± 2.1 4.9 |
4.7 ± 1.6 5.1 |
F (1,39) = 1.174 | P=0.285 |
| Orgasm (mean ± SD) Median |
4.0 ± 2.1 4.8 |
4.3 ± 1.7 4.8 |
F (1,39) = 0.509 | p = 0.479 |
| Satisfaction (mean ± SD) Median |
4.7 ± 1.2 5 |
4.7±1.4 5.2 |
F (1,39) = 0.004 | p = 0.948 |
| Dyspareunia (mean ± SD) Median |
4.5 ± 1.5 4.8 |
5.1 ± 1.4 5.6 |
F (1,39) = 2.459 | p = 0.124 |
| Total (mean ± SD) Median |
25.1 ± 8.8 28.0 |
26.8 ± 7.5 28.8 |
F (1,39) = 0.774 | p = 0.381 |
| Dimension | Before excision procedure (n= 40) |
After excision procedure (n=40) |
F | p-value |
| D1 Thoughts/Desire (mean ± SD) Median |
4.75 ± 2.7 4.14 |
5.31 ± 3.04 5.57 |
F (1,39) = 0.936 | p = 0.339 |
| D 2 Arousal (mean ± SD) Median |
6.97 ± 2.81 7.5 |
7.3 ± 3.13 8.25 |
F (1,39) = 0.253 | p = 0.617 |
| D3 Frequency of sexual activity (mean ± SD) Median |
4.18 ± 2.67 3.88 |
4.43 ± 2.82 4 |
F (1,39) = 0.163 | p = 0.688 |
| D4 Receptivity/initiation (mean ± SD) Median |
7.15 ± 4.11 8 |
7.9 ± 2.72 8 |
F (1,39) = 0.918 | p = 0.343 |
| D5 Pleasure/orgasm (mean ± SD) Median |
4.83 ± 3.07 5.13 |
5.97 ± 2.9 6.5 |
F (1,39) = 2.827 | p = 0.100 |
| D6 Relationship satisfaction (mean ± SD) Median |
8.55 ± 3.09 9 |
9.05 ± 2.96 10 |
F (1,39) = 0.627 |
p = 0.433 |
| D7 Problems affecting sexual functioning (mean ± SD) Median |
4.76 ± 2.63 4.71 |
4.54 ± 1.85 4.61 |
F (1,39) = 0.192 |
p = 0.663 |
| Composite score (mean ± SD) Median |
31.12 ± 13.89 31.75 |
35.62 ± 11.33 36.87 |
F (1,39) = 2.804 |
p = 0.102 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





