Submitted:
30 January 2025
Posted:
31 January 2025
You are already at the latest version
Abstract
Keywords:
INTRODUCTION
Pediatric Stroke
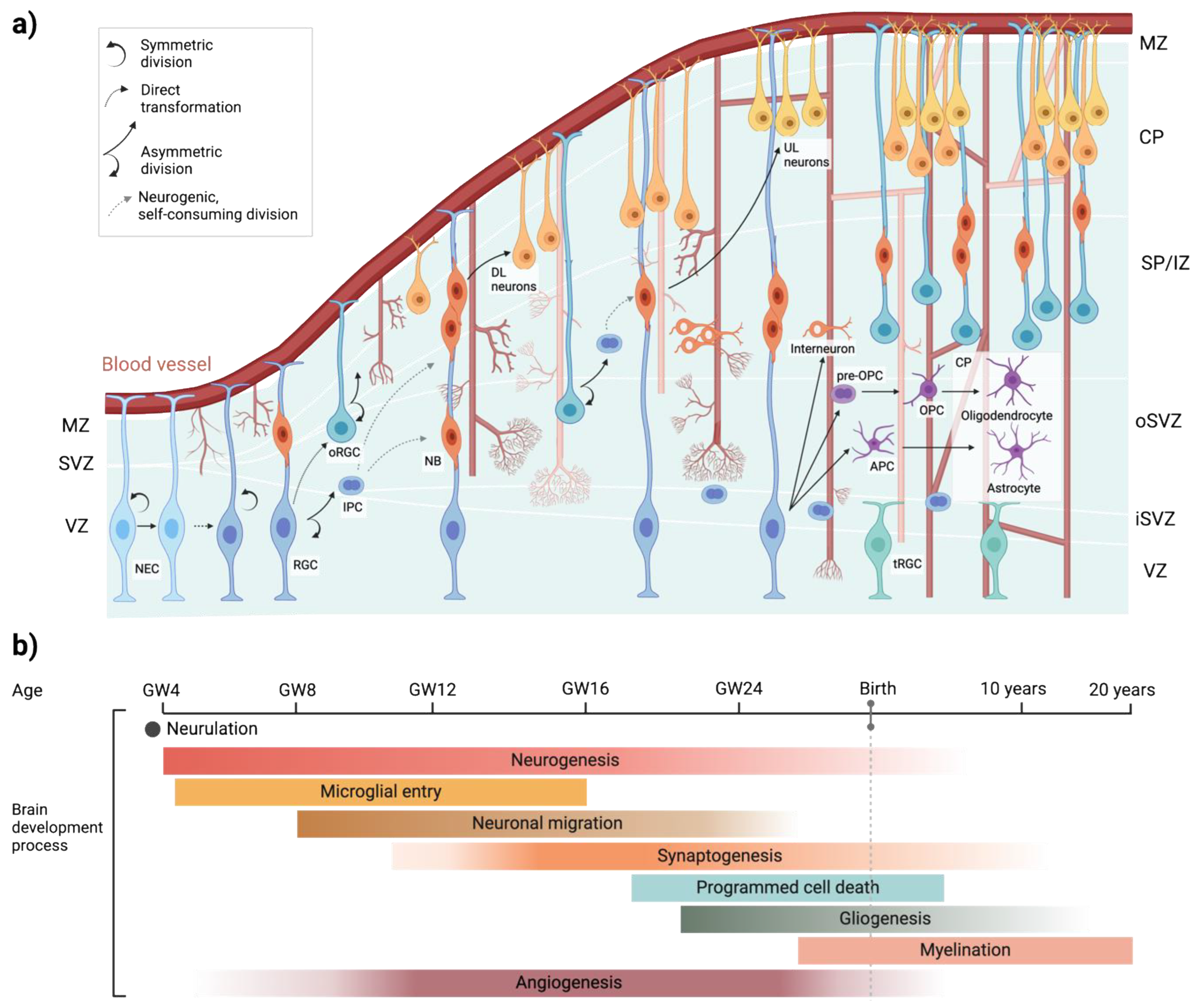
Human Brain Development
Human Vascular Development
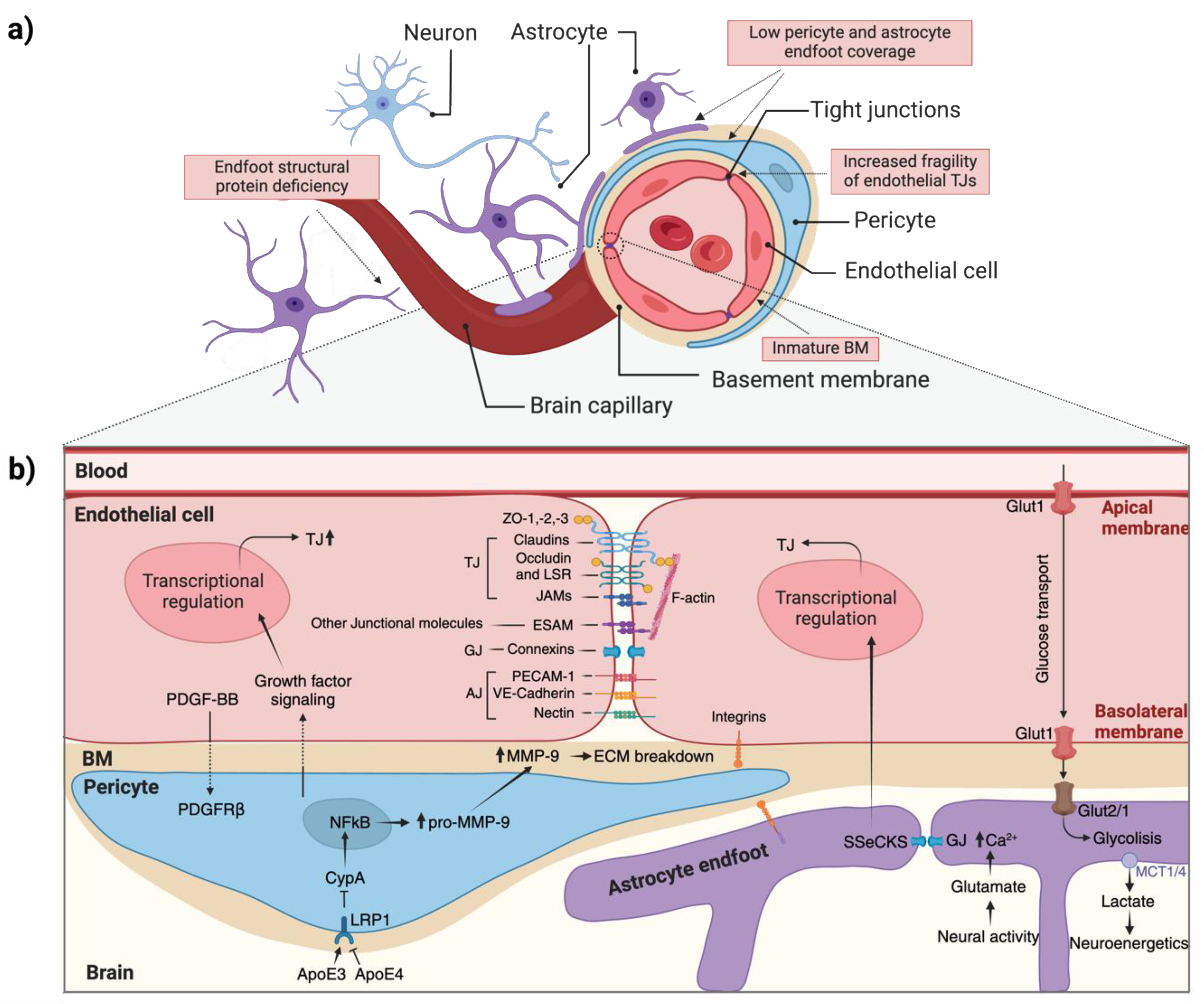
NEUROVASCULAR UNIT CELL-CELL INTERACTION
Astrocyte, pericytes and ECs interactions
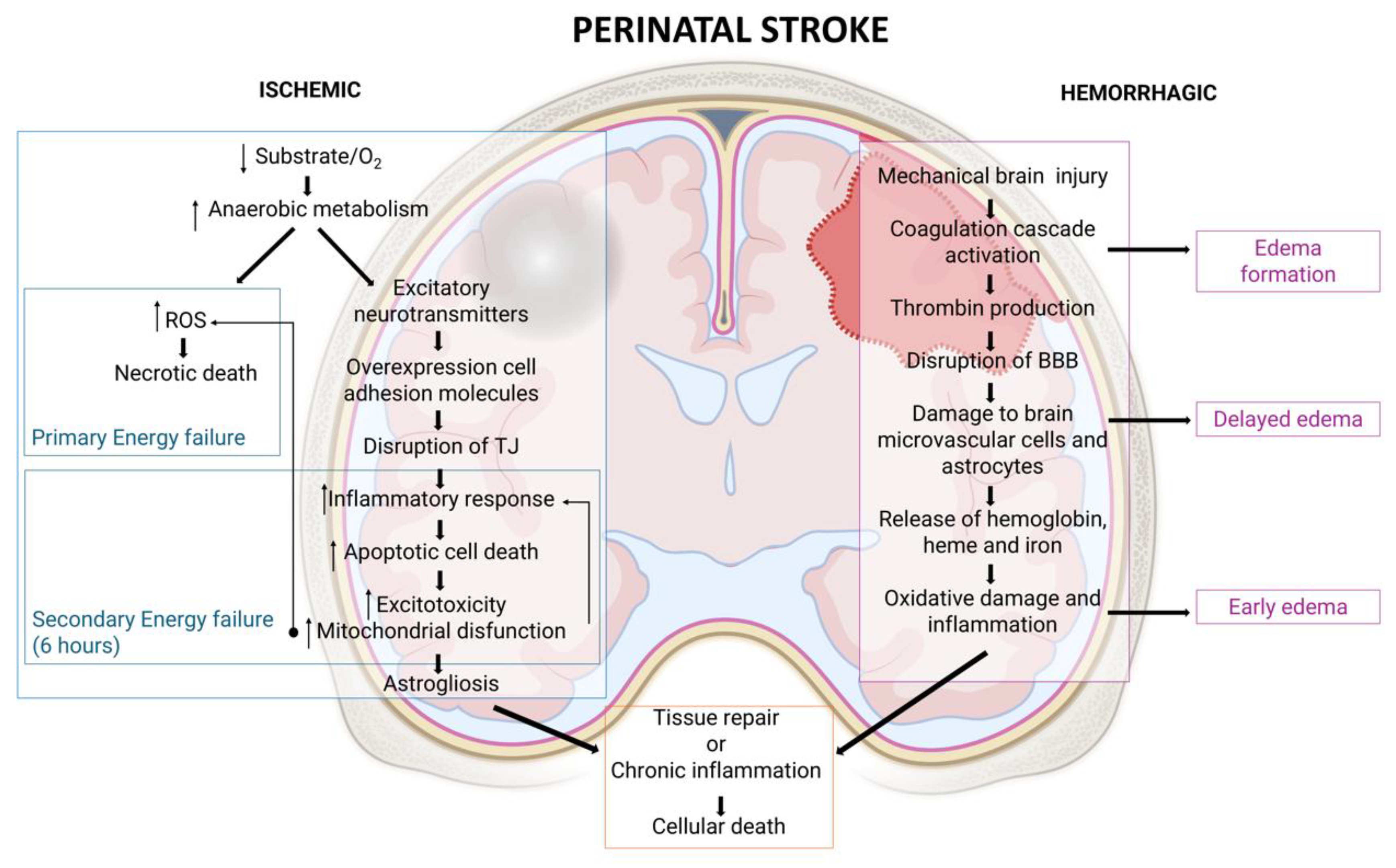
MECHANISMS OF BRAIN DAMAGE AFTER A PERINATAL STROKE
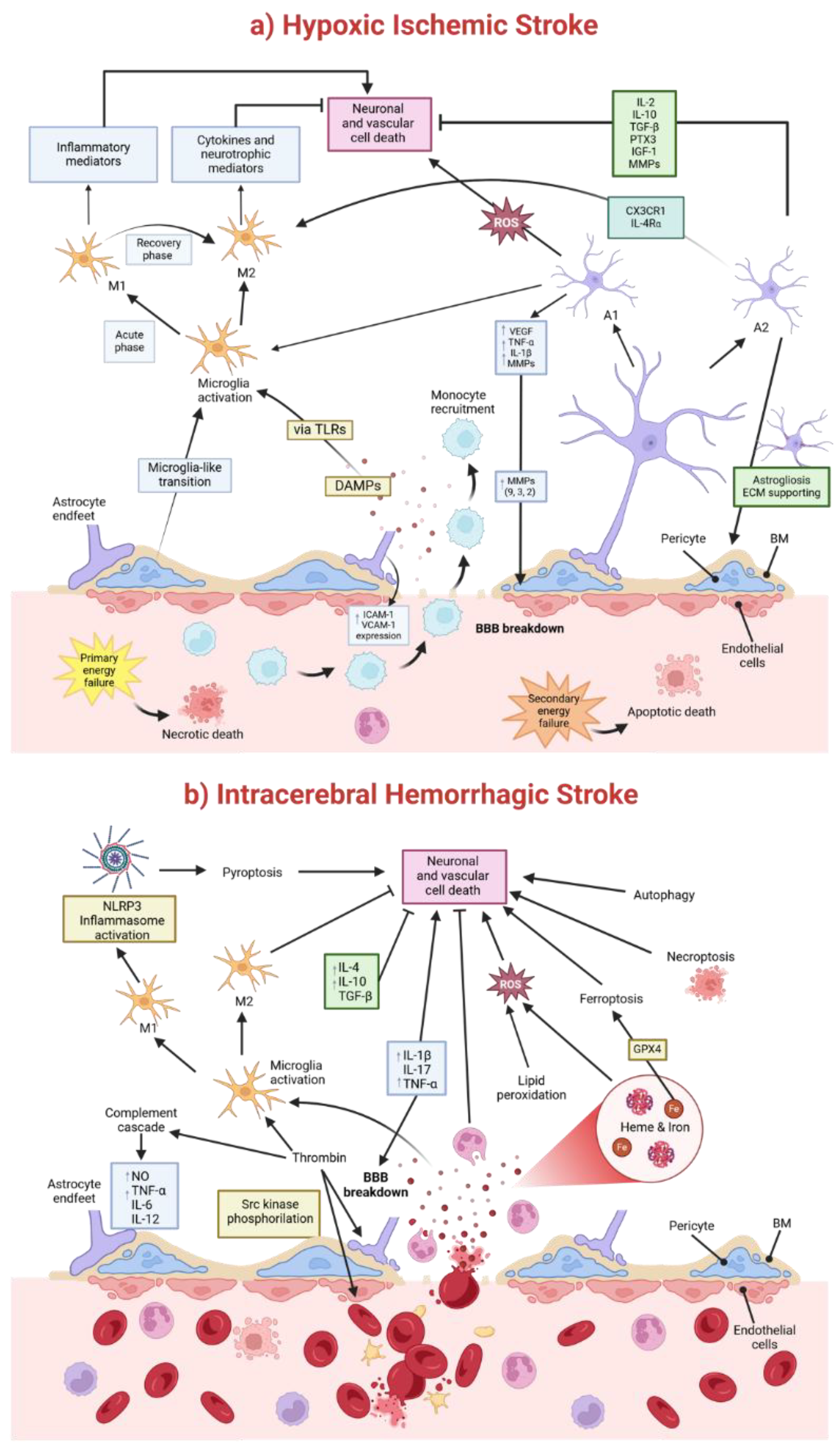
Pathophysiological Mechanisms of a Hypoxic-Ischemic Injury
Pathophysiological Mechanisms of Brain Damage after Intracerebral Hemorrhage (ICH)
NVU AND MONOGENIC NEUROLOGICAL DISORDERS
Pediatric stroke caused by mutations in genes expressed in ECs
Pediatric Stroke caused by mutations in genes expressed in Vascular Mural Cells and Pericytes
FUTURE PERSPECTIVES
Acknowledgements
References
- Zhou, Y.; Song, H.; Ming, G.L. Genetics of human brain development. Nat Rev Genet 2024, 25, 26–45. [Google Scholar] [CrossRef]
- Doi, M.; Usui, N.; Shimada, S. Prenatal Environment and Neurodevelopmental Disorders. Front Endocrinol (Lausanne) 2022, 13, 860110. [Google Scholar] [CrossRef]
- Quinn, J.A.; Munoz, F.M.; Gonik, B.; Frau, L.; Cutland, C.; Mallett-Moore, T.; Kissou, A.; Wittke, F.; Das, M.; Nunes, T.; et al. Preterm birth: Case definition & guidelines for data collection, analysis, and presentation of immunisation safety data. Vaccine 2016, 34, 6047–6056. [Google Scholar] [CrossRef]
- Purisch, S.E.; Gyamfi-Bannerman, C. Epidemiology of preterm birth. Semin Perinatol 2017, 41, 387–391. [Google Scholar] [CrossRef]
- Di Martino, E.; Rayasam, A.; Vexler, Z.S. Brain Maturation as a Fundamental Factor in Immune-Neurovascular Interactions in Stroke. Transl Stroke Res 2024, 15, 69–86. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.B. Perinatal ischemic stroke. Stroke 2007, 38, 742–745. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.M.; Malone, L.A.; Sun, L.R. Stroke in the Developing Brain: Neurophysiologic Implications of Stroke Timing, Location, and Comorbid Factors. Pediatr Neurol 2023, 148, 37–43. [Google Scholar] [CrossRef]
- Ferriero, D.M.; Fullerton, H.J.; Bernard, T.J.; Billinghurst, L.; Daniels, S.R.; DeBaun, M.R.; deVeber, G.; Ichord, R.N.; Jordan, L.C.; Massicotte, P.; et al. Management of Stroke in Neonates and Children: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke 2019, 50, e51–e96. [Google Scholar] [CrossRef]
- Jankovic, M.; Petrovic, B.; Novakovic, I.; Brankovic, S.; Radosavljevic, N.; Nikolic, D. The Genetic Basis of Strokes in Pediatric Populations and Insight into New Therapeutic Options. Int J Mol Sci 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, R.; Mailo, J.; Dunbar, M. Perinatal Stroke in Fetuses, Preterm and Term Infants. Semin Pediatr Neurol 2022, 43, 100988. [Google Scholar] [CrossRef] [PubMed]
- Dunbar, M.; Kirton, A. Perinatal stroke: mechanisms, management, and outcomes of early cerebrovascular brain injury. Lancet Child Adolesc Health 2018, 2, 666–676. [Google Scholar] [CrossRef]
- Lee, C.C.; Lin, J.J.; Lin, K.L.; Lim, W.H.; Hsu, K.H.; Hsu, J.F.; Fu, R.H.; Chiang, M.C.; Chu, S.M.; Lien, R. Clinical Manifestations, Outcomes, and Etiologies of Perinatal Stroke in Taiwan: Comparisons between Ischemic, and Hemorrhagic Stroke Based on 10-year Experience in A Single Institute. Pediatr Neonatol 2017, 58, 270–277. [Google Scholar] [CrossRef]
- Raju, T.N.; Nelson, K.B.; Ferriero, D.; Lynch, J.K. Ischemic perinatal stroke: summary of a workshop sponsored by the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke. Pediatrics 2007, 120, 609–616. [Google Scholar] [CrossRef]
- Govaert, P.; Ramenghi, L.; Taal, R.; de Vries, L.; Deveber, G. Diagnosis of perinatal stroke I: definitions, differential diagnosis and registration. Acta Paediatr 2009, 98, 1556–1567. [Google Scholar] [CrossRef] [PubMed]
- Bogousslavsky, J.; Regli, F.; Uské, A.; Maeder, P. Early spontaneous hematoma in cerebral infarct: is primary cerebral hemorrhage overdiagnosed? Neurology 1991, 41, 837–840. [Google Scholar] [CrossRef] [PubMed]
- Choi, P.M.; Ly, J.V.; Srikanth, V.; Ma, H.; Chong, W.; Holt, M.; Phan, T.G. Differentiating between Hemorrhagic Infarct and Parenchymal Intracerebral Hemorrhage. Radiol Res Pract 2012, 2012, 475497. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, H.J.; Wu, Y.W.; Zhao, S.; Johnston, S.C. Risk of stroke in children: ethnic and gender disparities. Neurology 2003, 61, 189–194. [Google Scholar] [CrossRef]
- Mallick, A.A.; Ganesan, V.; Kirkham, F.J.; Fallon, P.; Hedderly, T.; McShane, T.; Parker, A.P.; Wassmer, E.; Wraige, E.; Amin, S.; et al. Childhood arterial ischaemic stroke incidence, presenting features, and risk factors: a prospective population-based study. Lancet Neurol 2014, 13, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Malone, L.A.; Felling, R.J. Pediatric Stroke: Unique Implications of the Immature Brain on Injury and Recovery. Pediatr Neurol 2020, 102, 3–9. [Google Scholar] [CrossRef]
- Lynch, J.K.; Hirtz, D.G.; DeVeber, G.; Nelson, K.B. Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics 2002, 109, 116–123. [Google Scholar] [CrossRef]
- Budday, S.; Steinmann, P.; Kuhl, E. Physical biology of human brain development. Front Cell Neurosci 2015, 9, 257. [Google Scholar] [CrossRef] [PubMed]
- Degl'Innocenti, E.; Dell'Anno, M.T. Human and mouse cortical astrocytes: a comparative view from development to morphological and functional characterization. Front Neuroanat 2023, 17, 1130729. [Google Scholar] [CrossRef]
- O'Rahilly, R.; Müller, F. The Embryonic Human Brain: An Atlas of Developmental Stages, Third Edition. The Embryonic Human Brain: An Atlas of Developmental Stages, Third Edition 2005, 1–358. [Google Scholar] [CrossRef]
- Stiles, J.; Jernigan, T.L. The basics of brain development. Neuropsychol Rev 2010, 20, 327–348. [Google Scholar] [CrossRef] [PubMed]
- Baggiani, M.; Dell'Anno, M.T.; Pistello, M.; Conti, L.; Onorati, M. Human Neural Stem Cell Systems to Explore Pathogen-Related Neurodevelopmental and Neurodegenerative Disorders. Cells 2020, 9. [Google Scholar] [CrossRef]
- Gao, P.; Sultan, K.T.; Zhang, X.J.; Shi, S.H. Lineage-dependent circuit assembly in the neocortex. Development 2013, 140, 2645–2655. [Google Scholar] [CrossRef]
- Tau, G.Z.; Peterson, B.S. Normal development of brain circuits. Neuropsychopharmacology 2010, 35, 147–168. [Google Scholar] [CrossRef] [PubMed]
- Lanzone, A.; Ferrazzani, S.; Botta, A. Delivery and late preterm birth. Italian Journal of Pediatrics 2014, 40, A1. [Google Scholar] [CrossRef]
- Molliver, M.E.; Kostović, I.; van der Loos, H. The development of synapses in cerebral cortex of the human fetus. Brain Res 1973, 50, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Riccomagno, M.M.; Kolodkin, A.L. Sculpting neural circuits by axon and dendrite pruning. Annu Rev Cell Dev Biol 2015, 31, 779–805. [Google Scholar] [CrossRef]
- Jithoo, A.; Penny, T.R.; Pham, Y.; Sutherland, A.E.; Smith, M.J.; Petraki, M.; Fahey, M.C.; Jenkin, G.; Malhotra, A.; Miller, S.L.; et al. The Temporal Relationship between Blood-Brain Barrier Integrity and Microglial Response following Neonatal Hypoxia Ischemia. Cells 2024, 13. [Google Scholar] [CrossRef] [PubMed]
- Kierdorf, K.; Erny, D.; Goldmann, T.; Sander, V.; Schulz, C.; Perdiguero, E.G.; Wieghofer, P.; Heinrich, A.; Riemke, P.; Hölscher, C.; et al. Microglia emerge from erythromyeloid precursors via Pu.1- and Irf8-dependent pathways. Nat Neurosci 2013, 16, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Roessmann, U.; Gambetti, P. Astrocytes in the developing human brain. An immunohistochemical study. Acta Neuropathol 1986, 70, 308–313. [Google Scholar] [CrossRef]
- Yeung, M.S.; Zdunek, S.; Bergmann, O.; Bernard, S.; Salehpour, M.; Alkass, K.; Perl, S.; Tisdale, J.; Possnert, G.; Brundin, L.; et al. Dynamics of oligodendrocyte generation and myelination in the human brain. Cell 2014, 159, 766–774. [Google Scholar] [CrossRef] [PubMed]
- Raybaud, C. Normal and abnormal embryology and development of the intracranial vascular system. Neurosurg Clin N Am 2010, 21, 399–426. [Google Scholar] [CrossRef] [PubMed]
- Ballabh, P.; Hu, F.; Kumarasiri, M.; Braun, A.; Nedergaard, M. Development of tight junction molecules in blood vessels of germinal matrix, cerebral cortex, and white matter. Pediatr Res 2005, 58, 791–798. [Google Scholar] [CrossRef]
- Liebner, S.; Czupalla, C.J.; Wolburg, H. Current concepts of blood-brain barrier development. Int J Dev Biol 2011, 55, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.H. Vascular patterning by Eph receptor tyrosine kinases and ephrins. Semin Cell Dev Biol 2002, 13, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.I.; Dodelet-Devillers, A.; Kebir, H.; Ifergan, I.; Fabre, P.J.; Terouz, S.; Sabbagh, M.; Wosik, K.; Bourbonnière, L.; Bernard, M.; et al. The Hedgehog pathway promotes blood-brain barrier integrity and CNS immune quiescence. Science 2011, 334, 1727–1731. [Google Scholar] [CrossRef]
- Daneman, R.; Agalliu, D.; Zhou, L.; Kuhnert, F.; Kuo, C.J.; Barres, B.A. Wnt/beta-catenin signaling is required for CNS, but not non-CNS, angiogenesis. Proc Natl Acad Sci U S A 2009, 106, 641–646. [Google Scholar] [CrossRef]
- Liebner, S.; Corada, M.; Bangsow, T.; Babbage, J.; Taddei, A.; Czupalla, C.J.; Reis, M.; Felici, A.; Wolburg, H.; Fruttiger, M.; et al. Wnt/beta-catenin signaling controls development of the blood-brain barrier. J Cell Biol 2008, 183, 409–417. [Google Scholar] [CrossRef]
- Shawber, C.J.; Kitajewski, J. Notch function in the vasculature: insights from zebrafish, mouse and man. Bioessays 2004, 26, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.I.; Katayama, T.; Prat, A. Glial influence on the blood brain barrier. Glia 2013, 61, 1939–1958. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Han, J.; Bai, H.J.; Kim, K.W. Brain angiogenesis in developmental and pathological processes: regulation, molecular and cellular communication at the neurovascular interface. Febs j 2009, 276, 4622–4635. [Google Scholar] [CrossRef] [PubMed]
- Betz, C.; Lenard, A.; Belting, H.G.; Affolter, M. Cell behaviors and dynamics during angiogenesis. Development 2016, 143, 2249–2260. [Google Scholar] [CrossRef]
- Wacker, A.; Gerhardt, H. Endothelial development taking shape. Curr Opin Cell Biol 2011, 23, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Sauteur, L.; Affolter, M.; Belting, H.G. Distinct and redundant functions of Esama and VE-cadherin during vascular morphogenesis. Development 2017, 144, 1554–1565. [Google Scholar] [CrossRef]
- Bell, A.H.; Miller, S.L.; Castillo-Melendez, M.; Malhotra, A. The Neurovascular Unit: Effects of Brain Insults During the Perinatal Period. Front Neurosci 2019, 13, 1452. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.A.; Chand, K.K.; Bell, A.; Miller, S.L.; Colditz, P.B.; Malhotra, A.; Wixey, J.A. Effects of fetal growth restriction on the perinatal neurovascular unit and possible treatment targets. Pediatr Res 2024, 95, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Iadecola, C. Neurovascular regulation in the normal brain and in Alzheimer's disease. Nat Rev Neurosci 2004, 5, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Abbott, N.J.; Rönnbäck, L.; Hansson, E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci 2006, 7, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, S.; Iadecola, C. Revisiting the neurovascular unit. Nat Neurosci 2021, 24, 1198–1209. [Google Scholar] [CrossRef]
- Iadecola, C. The Neurovascular Unit Coming of Age: A Journey through Neurovascular Coupling in Health and Disease. Neuron 2017, 96, 17–42. [Google Scholar] [CrossRef]
- Rizzuti, M.; Melzi, V.; Brambilla, L.; Quetti, L.; Sali, L.; Ottoboni, L.; Meneri, M.; Ratti, A.; Verde, F.; Ticozzi, N.; et al. Shaping the Neurovascular Unit Exploiting Human Brain Organoids. Mol Neurobiol 2024, 61, 6642–6657. [Google Scholar] [CrossRef] [PubMed]
- Manu, D.R.; Slevin, M.; Barcutean, L.; Forro, T.; Boghitoiu, T.; Balasa, R. Astrocyte Involvement in Blood-Brain Barrier Function: A Critical Update Highlighting Novel, Complex, Neurovascular Interactions. Int J Mol Sci 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- Disdier, C.; Stonestreet, B.S. Hypoxic-ischemic-related cerebrovascular changes and potential therapeutic strategies in the neonatal brain. J Neurosci Res 2020, 98, 1468–1484. [Google Scholar] [CrossRef] [PubMed]
- Langen, U.H.; Ayloo, S.; Gu, C. Development and Cell Biology of the Blood-Brain Barrier. Annu Rev Cell Dev Biol 2019, 35, 591–613. [Google Scholar] [CrossRef]
- Wolburg, H.; Lippoldt, A. Tight junctions of the blood–brain barrier: development, composition and regulation. Vascular Pharmacology 2002, 38, 323–337. [Google Scholar] [CrossRef]
- Zhao, Z.; Nelson, A.R.; Betsholtz, C.; Zlokovic, B.V. Establishment and Dysfunction of the Blood-Brain Barrier. Cell 2015, 163, 1064–1078. [Google Scholar] [CrossRef]
- Nico, B.; Quondamatteo, F.; Herken, R.; Marzullo, A.; Corsi, P.; Bertossi, M.; Russo, G.; Ribatti, D.; Roncali, L. Developmental expression of ZO-1 antigen in the mouse blood-brain barrier. Brain Res Dev Brain Res 1999, 114, 161–169. [Google Scholar] [CrossRef]
- Daneman, R.; Zhou, L.; Kebede, A.A.; Barres, B.A. Pericytes are required for blood-brain barrier integrity during embryogenesis. Nature 2010, 468, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Armulik, A.; Genové, G.; Betsholtz, C. Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell 2011, 21, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Shen, Q.; Goderie, S.K.; He, W.; Capela, A.; Davis, A.A.; Temple, S. Timing of CNS cell generation: a programmed sequence of neuron and glial cell production from isolated murine cortical stem cells. Neuron 2000, 28, 69–80. [Google Scholar] [CrossRef]
- Dore-Duffy, P.; Cleary, K. Morphology and properties of pericytes. Methods Mol Biol 2011, 686, 49–68. [Google Scholar] [CrossRef] [PubMed]
- Dalkara, T.; Gursoy-Ozdemir, Y.; Yemisci, M. Brain microvascular pericytes in health and disease. Acta Neuropathol 2011, 122, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Armulik, A.; Abramsson, A.; Betsholtz, C. Endothelial/pericyte interactions. Circ Res 2005, 97, 512–523. [Google Scholar] [CrossRef]
- Kemp, S.S.; Aguera, K.N.; Cha, B.; Davis, G.E. Defining Endothelial Cell-Derived Factors That Promote Pericyte Recruitment and Capillary Network Assembly. Arterioscler Thromb Vasc Biol 2020, 40, 2632–2648. [Google Scholar] [CrossRef]
- Lee, S.W.; Kim, W.J.; Choi, Y.K.; Song, H.S.; Son, M.J.; Gelman, I.H.; Kim, Y.J.; Kim, K.W. SSeCKS regulates angiogenesis and tight junction formation in blood-brain barrier. Nat Med 2003, 9, 900–906. [Google Scholar] [CrossRef]
- Bell, R.D.; Winkler, E.A.; Singh, I.; Sagare, A.P.; Deane, R.; Wu, Z.; Holtzman, D.M.; Betsholtz, C.; Armulik, A.; Sallstrom, J.; et al. Apolipoprotein E controls cerebrovascular integrity via cyclophilin A. Nature 2012, 485, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Paz, A.A.; González-Candia, A. Potential pharmacological target of tight junctions to improve the BBB permeability in neonatal Hypoxic-Ischemic encephalopathy Diseases. Biochem Pharmacol 2023, 207, 115356. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Chen, Z.L.; Norris, E.H.; Strickland, S. Astrocytic laminin regulates pericyte differentiation and maintains blood brain barrier integrity. Nat Commun 2014, 5, 3413. [Google Scholar] [CrossRef] [PubMed]
- Saunders, N.R.; Dziegielewska, K.M.; Mollgard, K.; Habgood, M.D. Physiology and molecular biology of barrier mechanisms in the fetal and neonatal brain. J Physiol 2018, 596, 5723–5756. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Biarge, M.; Ferriero, D.M.; Cowan, F.M. Perinatal arterial ischemic stroke. Handb Clin Neurol 2019, 162, 239–266. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Concepcion, K.; Meng, X.; Zhang, L. Brain-immune interactions in perinatal hypoxic-ischemic brain injury. Prog Neurobiol 2017, 159, 50–68. [Google Scholar] [CrossRef]
- Greco, P.; Nencini, G.; Piva, I.; Scioscia, M.; Volta, C.A.; Spadaro, S.; Neri, M.; Bonaccorsi, G.; Greco, F.; Cocco, I.; et al. Pathophysiology of hypoxic-ischemic encephalopathy: a review of the past and a view on the future. Acta Neurol Belg 2020, 120, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Fernández-López, D.; Natarajan, N.; Ashwal, S.; Vexler, Z.S. Mechanisms of perinatal arterial ischemic stroke. J Cereb Blood Flow Metab 2014, 34, 921–932. [Google Scholar] [CrossRef]
- Zhang, G.; Zhao, A.; Zhang, X.; Zeng, M.; Wei, H.; Yan, X.; Wang, J.; Jiang, X.; Dai, Y. Glycolytic reprogramming in microglia: A potential therapeutic target for ischemic stroke. Cell Signal 2024, 124, 111466. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Wen, J. Crosstalk Among Glial Cells in the Blood-Brain Barrier Injury After Ischemic Stroke. Mol Neurobiol 2024, 61, 6161–6174. [Google Scholar] [CrossRef] [PubMed]
- Gidday, J.M.; Gasche, Y.G.; Copin, J.C.; Shah, A.R.; Perez, R.S.; Shapiro, S.D.; Chan, P.H.; Park, T.S. Leukocyte-derived matrix metalloproteinase-9 mediates blood-brain barrier breakdown and is proinflammatory after transient focal cerebral ischemia. Am J Physiol Heart Circ Physiol 2005, 289, H558–568. [Google Scholar] [CrossRef]
- McColl, B.W.; Rothwell, N.J.; Allan, S.M. Systemic inflammation alters the kinetics of cerebrovascular tight junction disruption after experimental stroke in mice. J Neurosci 2008, 28, 9451–9462. [Google Scholar] [CrossRef]
- Asahi, M.; Asahi, K.; Jung, J.C.; del Zoppo, G.J.; Fini, M.E.; Lo, E.H. Role for matrix metalloproteinase 9 after focal cerebral ischemia: effects of gene knockout and enzyme inhibition with BB-94. J Cereb Blood Flow Metab 2000, 20, 1681–1689. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, G.A.; Estrada, E.Y.; Dencoff, J.E. Matrix metalloproteinases and TIMPs are associated with blood-brain barrier opening after reperfusion in rat brain. Stroke 1998, 29, 2189–2195. [Google Scholar] [CrossRef] [PubMed]
- Asahi, M.; Sumii, T.; Fini, M.E.; Itohara, S.; Lo, E.H. Matrix metalloproteinase 2 gene knockout has no effect on acute brain injury after focal ischemia. Neuroreport 2001, 12, 3003–3007. [Google Scholar] [CrossRef] [PubMed]
- Lo, E.H.; Dalkara, T.; Moskowitz, M.A. Mechanisms, challenges and opportunities in stroke. Nat Rev Neurosci 2003, 4, 399–415. [Google Scholar] [CrossRef]
- Tong, W.; Zhang, L. Fetal hypoxia and programming of matrix metalloproteinases. Drug Discov Today 2012, 17, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Borjini, N.; Sivilia, S.; Giuliani, A.; Fernandez, M.; Giardino, L.; Facchinetti, F.; Calzà, L. Potential biomarkers for neuroinflammation and neurodegeneration at short and long term after neonatal hypoxic-ischemic insult in rat. J Neuroinflammation 2019, 16, 194. [Google Scholar] [CrossRef]
- Lai, J.C.Y.; Rocha-Ferreira, E.; Ek, C.J.; Wang, X.; Hagberg, H.; Mallard, C. Immune responses in perinatal brain injury. Brain Behav Immun 2017, 63, 210–223. [Google Scholar] [CrossRef] [PubMed]
- Zonneveld, R.; Martinelli, R.; Shapiro, N.I.; Kuijpers, T.W.; Plötz, F.B.; Carman, C.V. Soluble adhesion molecules as markers for sepsis and the potential pathophysiological discrepancy in neonates, children and adults. Crit Care 2014, 18, 204. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.Q.; Wang, S.; Kim, H.Y.; Storrie, H.; Rosen, B.R.; Mooney, D.J.; Wang, X.; Lo, E.H. Role of matrix metalloproteinases in delayed cortical responses after stroke. Nat Med 2006, 12, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Vaillant, C.; Didier-Bazès, M.; Hutter, A.; Belin, M.F.; Thomasset, N. Spatiotemporal expression patterns of metalloproteinases and their inhibitors in the postnatal developing rat cerebellum. J Neurosci 1999, 19, 4994–5004. [Google Scholar] [CrossRef]
- Norden, D.M.; Fenn, A.M.; Dugan, A.; Godbout, J.P. TGFbeta produced by IL-10 redirected astrocytes attenuates microglial activation. Glia 2014, 62, 881–895. [Google Scholar] [CrossRef] [PubMed]
- Rakers, C.; Schleif, M.; Blank, N.; Matuskova, H.; Ulas, T.; Handler, K.; Torres, S.V.; Schumacher, T.; Tai, K.; Schultze, J.L.; et al. Stroke target identification guided by astrocyte transcriptome analysis. Glia 2019, 67, 619–633. [Google Scholar] [CrossRef] [PubMed]
- Nakagomi, T.; Kubo, S.; Nakano-Doi, A.; Sakuma, R.; Lu, S.; Narita, A.; Kawahara, M.; Taguchi, A.; Matsuyama, T. Brain vascular pericytes following ischemia have multipotential stem cell activity to differentiate into neural and vascular lineage cells. Stem Cells 2015, 33, 1962–1974. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, R.; Kawahara, M.; Nakano-Doi, A.; Takahashi, A.; Tanaka, Y.; Narita, A.; Kuwahara-Otani, S.; Hayakawa, T.; Yagi, H.; Matsuyama, T.; et al. Brain pericytes serve as microglia-generating multipotent vascular stem cells following ischemic stroke. J Neuroinflammation 2016, 13, 57. [Google Scholar] [CrossRef]
- Nirwane, A.; Yao, Y. SMA(low/undetectable) pericytes differentiate into microglia- and macrophage-like cells in ischemic brain. Cell Mol Life Sci 2022, 79, 264. [Google Scholar] [CrossRef] [PubMed]
- Bai, Q.; Sheng, Z.; Liu, Y.; Zhang, R.; Yong, V.W.; Xue, M. Intracerebral haemorrhage: from clinical settings to animal models. Stroke Vasc Neurol 2020, 5, 388–395. [Google Scholar] [CrossRef]
- Xi, G.; Keep, R.F.; Hoff, J.T. Pathophysiology of brain edema formation. Neurosurg Clin N Am 2002, 13, 371–383. [Google Scholar] [CrossRef]
- Zheng, H.; Chen, C.; Zhang, J.; Hu, Z. Mechanism and Therapy of Brain Edema after Intracerebral Hemorrhage. Cerebrovasc Dis 2016, 42, 155–169. [Google Scholar] [CrossRef]
- Wilkinson, D.A.; Pandey, A.S.; Thompson, B.G.; Keep, R.F.; Hua, Y.; Xi, G. Injury mechanisms in acute intracerebral hemorrhage. Neuropharmacology 2018, 134, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Wang, Z.; Yu, J.; Yang, X.; He, F.; Liu, Z.; Che, F.; Chen, X.; Ren, H.; Hong, M.; et al. Role and mechanisms of cytokines in the secondary brain injury after intracerebral hemorrhage. Prog Neurobiol 2019, 178, 101610. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Dai, W.; Zheng, Y.; Qiao, W.; Chen, W.; Peng, L.; Zhou, H.; Zhao, T.; Liu, H.; Zheng, F.; et al. Mechanism and Regulation of Microglia Polarization in Intracerebral Hemorrhage. Molecules 2022, 27. [Google Scholar] [CrossRef]
- Simard, J.M.; Geng, Z.; Woo, S.K.; Ivanova, S.; Tosun, C.; Melnichenko, L.; Gerzanich, V. Glibenclamide reduces inflammation, vasogenic edema, and caspase-3 activation after subarachnoid hemorrhage. J Cereb Blood Flow Metab 2009, 29, 317–330. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.Y.; Cui, G.Z.; Yan, X.L.; Wang, X.; Qu, Y.; Guo, Z.N.; Jin, H. Mechanism of Ferroptosis and Its Relationships With Other Types of Programmed Cell Death: Insights for Potential Interventions After Intracerebral Hemorrhage. Front Neurosci 2020, 14, 589042. [Google Scholar] [CrossRef] [PubMed]
- Fernández-López, D.; Faustino, J.; Daneman, R.; Zhou, L.; Lee, S.Y.; Derugin, N.; Wendland, M.F.; Vexler, Z.S. Blood-brain barrier permeability is increased after acute adult stroke but not neonatal stroke in the rat. J Neurosci 2012, 32, 9588–9600. [Google Scholar] [CrossRef]
- Abdel-Hamid, M.S.; Abdel-Salam, G.M.H.; Issa, M.Y.; Emam, B.A.; Zaki, M.S. Band-like calcification with simplified gyration and polymicrogyria: report of 10 new families and identification of five novel OCLN mutations. J Hum Genet 2017, 62, 553–559. [Google Scholar] [CrossRef] [PubMed]
- O'Driscoll, M.C.; Daly, S.B.; Urquhart, J.E.; Black, G.C.; Pilz, D.T.; Brockmann, K.; McEntagart, M.; Abdel-Salam, G.; Zaki, M.; Wolf, N.I.; et al. Recessive mutations in the gene encoding the tight junction protein occludin cause band-like calcification with simplified gyration and polymicrogyria. Am J Hum Genet 2010, 87, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Cen, Z.; Chen, Y.; Chen, S.; Wang, H.; Yang, D.; Zhang, H.; Wu, H.; Wang, L.; Tang, S.; Ye, J.; et al. Biallelic loss-of-function mutations in JAM2 cause primary familial brain calcification. Brain 2020, 143, 491–502. [Google Scholar] [CrossRef]
- Schottlaender, L.V.; Abeti, R.; Jaunmuktane, Z.; Macmillan, C.; Chelban, V.; O'Callaghan, B.; McKinley, J.; Maroofian, R.; Efthymiou, S.; Athanasiou-Fragkouli, A.; et al. Bi-allelic JAM2 Variants Lead to Early-Onset Recessive Primary Familial Brain Calcification. Am J Hum Genet 2020, 106, 412–421. [Google Scholar] [CrossRef]
- Lamagna, C.; Meda, P.; Mandicourt, G.; Brown, J.; Gilbert, R.J.; Jones, E.Y.; Kiefer, F.; Ruga, P.; Imhof, B.A.; Aurrand-Lions, M. Dual interaction of JAM-C with JAM-B and alpha(M)beta2 integrin: function in junctional complexes and leukocyte adhesion. Mol Biol Cell 2005, 16, 4992–5003. [Google Scholar] [CrossRef] [PubMed]
- Stamatovic, S.M.; Johnson, A.M.; Keep, R.F.; Andjelkovic, A.V. Junctional proteins of the blood-brain barrier: New insights into function and dysfunction. Tissue Barriers 2016, 4, e1154641. [Google Scholar] [CrossRef]
- Lecca, M.; Pehlivan, D.; Suner, D.H.; Weiss, K.; Coste, T.; Zweier, M.; Oktay, Y.; Danial-Farran, N.; Rosti, V.; Bonasoni, M.P.; et al. Bi-allelic variants in the ESAM tight-junction gene cause a neurodevelopmental disorder associated with fetal intracranial hemorrhage. Am J Hum Genet 2023, 110, 681–690. [Google Scholar] [CrossRef]
- Gould, D.B.; Phalan, F.C.; Breedveld, G.J.; van Mil, S.E.; Smith, R.S.; Schimenti, J.C.; Aguglia, U.; van der Knaap, M.S.; Heutink, P.; John, S.W. Mutations in Col4a1 cause perinatal cerebral hemorrhage and porencephaly. Science 2005, 308, 1167–1171. [Google Scholar] [CrossRef] [PubMed]
- Durrani-Kolarik, S.; Manickam, K.; Chen, B. COL4A1 Mutation in a Neonate With Intrauterine Stroke and Anterior Segment Dysgenesis. Pediatr Neurol 2017, 66, 100–103. [Google Scholar] [CrossRef]
- Garvey, A.A.; Walsh, B.H.; Inder, T.E. Pathogenesis and prevention of intraventricular hemorrhage. Semin Perinatol 2022, 46, 151592. [Google Scholar] [CrossRef]
- Abdel-Salam, G.M.H.; Esmail, A.; Nagy, D.; Abdel-Ghafar, S.F.; Abdel-Hamid, M.S. Novel homozygous ESAM variants in two families with perinatal strokes showing variable neuroradiologic and clinical findings. J Hum Genet 2024. [Google Scholar] [CrossRef] [PubMed]
- Mochida, G.H.; Ganesh, V.S.; Felie, J.M.; Gleason, D.; Hill, R.S.; Clapham, K.R.; Rakiec, D.; Tan, W.H.; Akawi, N.; Al-Saffar, M.; et al. A homozygous mutation in the tight-junction protein JAM3 causes hemorrhagic destruction of the brain, subependymal calcification, and congenital cataracts. Am J Hum Genet 2010, 87, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Duong, C.N.; Nottebaum, A.F.; Butz, S.; Volkery, S.; Zeuschner, D.; Stehling, M.; Vestweber, D. Interference With ESAM (Endothelial Cell-Selective Adhesion Molecule) Plus Vascular Endothelial-Cadherin Causes Immediate Lethality and Lung-Specific Blood Coagulation. Arterioscler Thromb Vasc Biol 2020, 40, 378–393. [Google Scholar] [CrossRef] [PubMed]
- Stahl, S.; Gaetzner, S.; Voss, K.; Brackertz, B.; Schleider, E.; Surucu, O.; Kunze, E.; Netzer, C.; Korenke, C.; Finckh, U.; et al. Novel CCM1, CCM2, and CCM3 mutations in patients with cerebral cavernous malformations: in-frame deletion in CCM2 prevents formation of a CCM1/CCM2/CCM3 protein complex. Hum Mutat 2008, 29, 709–717. [Google Scholar] [CrossRef]
- McDonald, J.; Wooderchak-Donahue, W.; VanSant Webb, C.; Whitehead, K.; Stevenson, D.A.; Bayrak-Toydemir, P. Hereditary hemorrhagic telangiectasia: genetics and molecular diagnostics in a new era. Front Genet 2015, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Wooderchak-Donahue, W.L.; Johnson, P.; McDonald, J.; Blei, F.; Berenstein, A.; Sorscher, M.; Mayer, J.; Scheuerle, A.E.; Lewis, T.; Grimmer, J.F.; et al. Expanding the clinical and molecular findings in RASA1 capillary malformation-arteriovenous malformation. Eur J Hum Genet 2018, 26, 1521–1536. [Google Scholar] [CrossRef] [PubMed]
- Amyere, M.; Revencu, N.; Helaers, R.; Pairet, E.; Baselga, E.; Cordisco, M.; Chung, W.; Dubois, J.; Lacour, J.P.; Martorell, L.; et al. Germline Loss-of-Function Mutations in EPHB4 Cause a Second Form of Capillary Malformation-Arteriovenous Malformation (CM-AVM2) Deregulating RAS-MAPK Signaling. Circulation 2017, 136, 1037–1048. [Google Scholar] [CrossRef]
- Shirley, M.D.; Tang, H.; Gallione, C.J.; Baugher, J.D.; Frelin, L.P.; Cohen, B.; North, P.E.; Marchuk, D.A.; Comi, A.M.; Pevsner, J. Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. N Engl J Med 2013, 368, 1971–1979. [Google Scholar] [CrossRef]
- Nasim, S.; Bichsel, C.; Pinto, A.; Alexandrescu, S.; Kozakewich, H.; Bischoff, J. Similarities and differences between brain and skin GNAQ p.R183Q driven capillary malformations. Angiogenesis 2024, 27, 931–941. [Google Scholar] [CrossRef] [PubMed]
- Di Donato, I.; Bianchi, S.; De Stefano, N.; Dichgans, M.; Dotti, M.T.; Duering, M.; Jouvent, E.; Korczyn, A.D.; Lesnik-Oberstein, S.A.; Malandrini, A.; et al. Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL) as a model of small vessel disease: update on clinical, diagnostic, and management aspects. BMC Med 2017, 15, 41. [Google Scholar] [CrossRef] [PubMed]
- Henshall, T.L.; Keller, A.; He, L.; Johansson, B.R.; Wallgard, E.; Raschperger, E.; Mae, M.A.; Jin, S.; Betsholtz, C.; Lendahl, U. Notch3 is necessary for blood vessel integrity in the central nervous system. Arterioscler Thromb Vasc Biol 2015, 35, 409–420. [Google Scholar] [CrossRef]
- Wang, Y.; Pan, L.; Moens, C.B.; Appel, B. Notch3 establishes brain vascular integrity by regulating pericyte number. Development 2014, 141, 307–317. [Google Scholar] [CrossRef]
- Jin, S.; Hansson, E.M.; Tikka, S.; Lanner, F.; Sahlgren, C.; Farnebo, F.; Baumann, M.; Kalimo, H.; Lendahl, U. Notch signaling regulates platelet-derived growth factor receptor-beta expression in vascular smooth muscle cells. Circ Res 2008, 102, 1483–1491. [Google Scholar] [CrossRef] [PubMed]
- Nadeem, T.; Bogue, W.; Bigit, B.; Cuervo, H. Deficiency of Notch signaling in pericytes results in arteriovenous malformations. JCI Insight 2020, 5. [Google Scholar] [CrossRef]
- Lindahl, P.; Johansson, B.R.; Leveen, P.; Betsholtz, C. Pericyte loss and microaneurysm formation in PDGF-B-deficient mice. Science 1997, 277, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Tallquist, M.D.; French, W.J.; Soriano, P. Additive effects of PDGF receptor beta signaling pathways in vascular smooth muscle cell development. PLoS Biol 2003, 1, E52. [Google Scholar] [CrossRef] [PubMed]
- Kundishora, A.J.; Peters, S.T.; Pinard, A.; Duran, D.; Panchagnula, S.; Barak, T.; Miyagishima, D.F.; Dong, W.; Smith, H.; Ocken, J.; et al. DIAPH1 Variants in Non-East Asian Patients With Sporadic Moyamoya Disease. JAMA Neurol 2021, 78, 993–1003. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.C.; Papke, C.L.; Tran-Fadulu, V.; Regalado, E.S.; Avidan, N.; Johnson, R.J.; Kim, D.H.; Pannu, H.; Willing, M.C.; Sparks, E.; et al. Mutations in smooth muscle alpha-actin (ACTA2) cause coronary artery disease, stroke, and Moyamoya disease, along with thoracic aortic disease. Am J Hum Genet 2009, 84, 617–627. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




