Submitted:
22 January 2025
Posted:
24 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. OCD: Definition, Diagnostic Criteria, and Prevalence
1.2. Treatment
1.3. OCD In Childhood and Adolescence
1.4. The Role of the Teacher
1.5. Barriers to Early Detection
1.6. Are Teachers Educated About OCD?
1.7. Research Aim
2. Method
2.1. Participants and Procedures
2.2. Materials
2.3. Data Analysis
2.3.1. Reflexivity
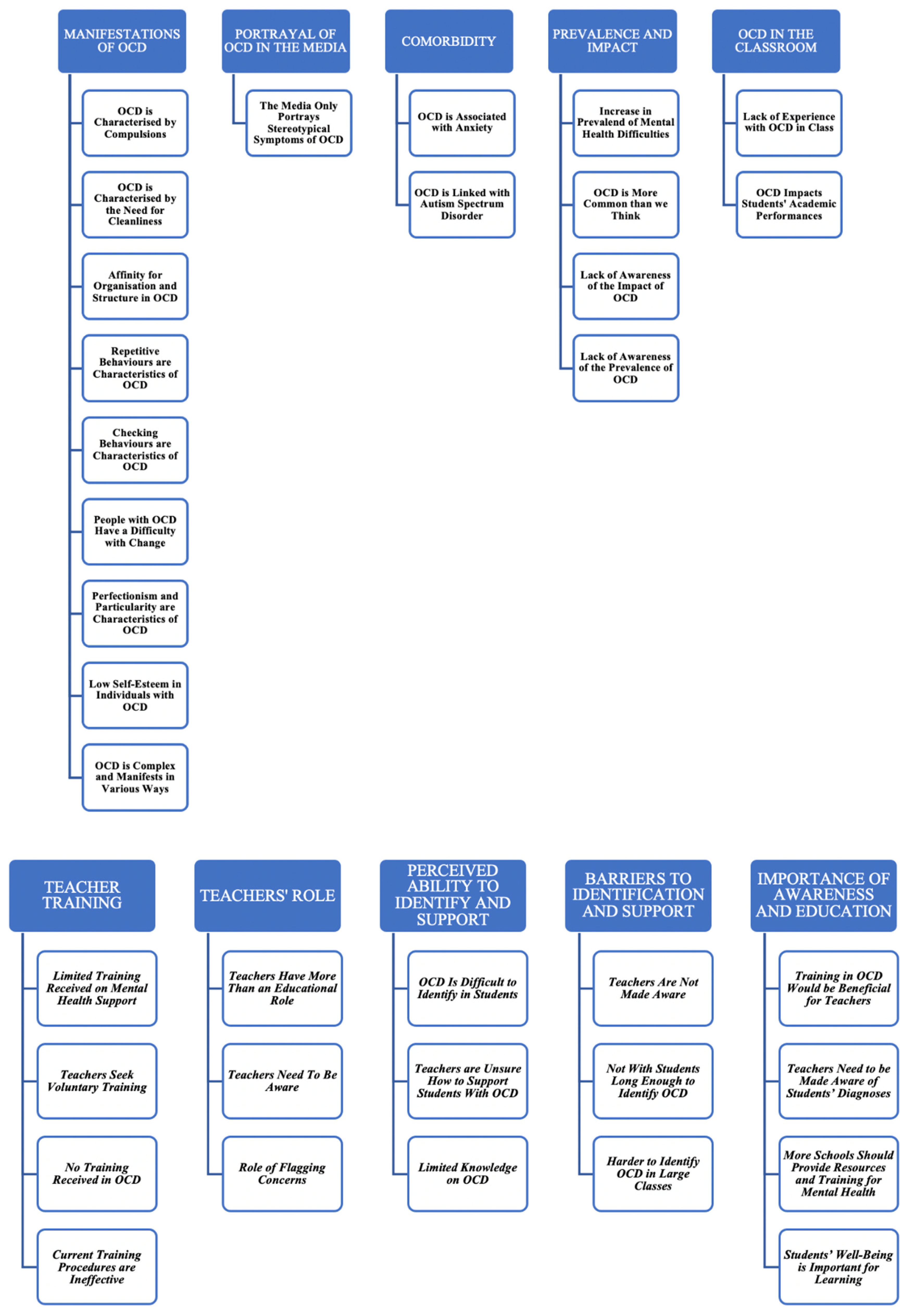
3. Results
3.1. Manifestations of OCD
3.1.1. OCD is Characterised by Compulsions
3.1.2. OCD is Characterised by the Need for Cleanliness
3.1.3. Affinity for Organisation and Structure in OCD
3.1.4. Repetitive Behaviours are Characteristics of OCD
3.1.5. Checking Behaviours are Characteristics of OCD
3.1.6. People with OCD have a Difficulty with Change
3.1.7. Perfectionism and Particularity are Characteristics of OCD
3.1.8. Low Self-Esteem in Individuals with OCD
3.1.9. OCD is Complex and Manifests in Various Ways
3.2. Portrayal of OCD in the Media
3.2.1. The Media Only Portrays Stereotypical Symptoms of OCD
3.3. Comorbidity
3.3.1. OCD is Associated with Anxiety
3.3.2. OCD is Linked with Autism Spectrum Disorder
3.4. Prevalence and Impact
3.4.1. Increase in Prevalence of Mental Health Difficulties
3.4.2. OCD is More Common than we Think
3.4.3. Lack of Awareness of the Impact of OCD
3.4.4. Lack of Awareness of the Prevalence of OCD
3.5. OCD in the Classroom
3.5.1. Lack of Experience with OCD in Class
3.5.2. OCD Impacts Students’ Academic Performance
3.6. Teacher Training
3.6.1. Limited Training Received on Mental Health Support
3.6.2. Teachers Seek Voluntary Training
3.6.3. No Training Received on OCD
3.6.4. Current Training Procedures are Ineffective
3.7. Teachers’ Role
3.7.1. Teachers Have More than an Educational Role
3.7.2. Teachers Need to Be Aware
3.7.3. Role of Flagging Concerns
3.8. Perceived Ability to Identify and Support
3.8.1. OCD is Difficult to Identify in Students
3.8.2. Teachers are Unsure How to Support Students with OCD
3.8.3. Limited Knowledge on OCD
3.9. Barriers to Identification and Support
3.9.1. Teachers Are Not Made Aware
3.9.2. Not with Students Long Enough to Identify OCD
3.9.3. Harder to Identify OCD in Large Classes
3.10. Importance of Awareness and Education
3.10.1. Training in OCD Would be Beneficial for Teachers
3.10.2. Teachers Need to be Made Aware of Students’ Diagnoses
3.10.3. More Schools Should Provide Resources and Training for Mental Health
3.10.4. Students’ Well-Being is Important for Learning
4. Discussion
4.1. Limited Understanding of OCD
4.2. Need for Targeted Education and Training
4.3. Limitations
4.4. Recommendations
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Interview Schedule
- Opening Questions:
- 1.
- How long have you been a secondary school teacher?
- 2.
- Which county do you currently work in?
- 3.
- What is your age?
- 4.
- What gender do you identify with?
- Understanding of OCD:
- 5.
- What is your understanding of OCD?
- 6.
- If you have heard of OCD before, how would you define it in your own words?
- 7.
- Can you name some symptoms of OCD? Please name as many as you know.
- Identifying OCD in Students:
- 8.
- What do you see as the role of teachers in relation to students with mental health problems?
- 9.
- What do you see as the role of teachers in relation to students with OCD?
- 10.
- As a secondary school teacher, have you ever received any training or information regarding how to support students with any form of mental health problem? If yes, please provide some detail on the nature of this training or information (the source of the training/information, the duration of the training, the content etc.)
- 11.
- As a secondary school teacher, have you ever received any training or information regarding how to support students with obsessive-compulsive disorder? If yes, please provide some detail on the nature of this training (the source of the training/information, the duration, the content etc.)
- 12.
- Do you feel that you could identify obsessive-compulsive disorder in your students?
- 13.
- Can you share any experiences you’ve had regarding OCD among your students?
- 14.
- In your opinion, how common do you think OCD is among students in the secondary school system in Ireland?
- Closing Questions:
- I am now going to read you a short paragraph which details the ways in which obsessive-compulsive disorder may affect students’ lives and their academic performance. Please identify any information that you were unaware of, prior to hearing this segment.
- Research in the area of mental health has identified OCD as one of the most common disorders in childhood and adolescence (Helbig & Ficca, 2009) and studies have indicated that it can cause serious academic and psychosocial impairment (Dyches et al., 2010). It has been suggested that individuals diagnosed with OCD are 55-62% less likely to progress beyond compulsory education (Negreiros et al., 2023). Studies have identified some of the ways in which students’ academic performance may be affected by OCD. For example; students may spend long periods of time in the bathroom washing their hands and missing class. They may avoid touching sports equipment or books used by other students, causing them to miss out on certain aspects of their learning. They may avoid certain people and/or socially isolate themselves. They may have a fear of bringing home “contaminated” schoolbooks, making it difficult for them to complete their homework (Ledley & Pasapuleti, 2007).
- 15.
- What information is new to you in this paragraph or is there anything in this paragraph that you maybe had not realised or thought about before in relation to the potential effect of OCD on academic performance?
- 16.
- Do you feel that it would be beneficial for teachers to receive more information or training on how to support students with obsessive-compulsive disorder or that teachers already have a sufficient level of training and information in this area?
- 17.
- Are there events that have happened in the last 3 months that have influenced your thinking or understanding about students with mental health problems including OCD and how they are supported in schools? If yes, please explain your answer.
- 18.
- Is there anything else that you’d like to say or wish that I had asked?
References
- Abramowitz, J. S., Tolin, D. F., & Diefenbach, G. J. (2005). Measuring change in OCD: sensitivity of the Obsessive-Compulsive Inventory-Revised. Journal of Psychopathology and Behavioral Assessment, 27, 317-324. [CrossRef]
- Adam, J., Goletz, H., Dengs, S., Klingenberger, N., Könnecke, S., Vonderbank, C.,... & Döpfner, M. (2022). Extended treatment of multimodal cognitive behavioral therapy in children and adolescents with obsessive–compulsive disorder improves symptom reduction: a within-subject design. Child and adolescent psychiatry and mental health, 16(1), 99. [CrossRef]
- Akkerman, S., Admiraal, W., Brekelmans, M., & Oost, H. (2008). Auditing quality of research in social sciences. Quality & quantity, 42, 257-274. [CrossRef]
- Albert, U., Manchia, M., Tortorella, A., Volpe, U., Rosso, G., Carpiniello, B., & Maina, G. (2015). Admixture analysis of age at symptom onset and age at disorder onset in a large sample of patients with obsessive–compulsive disorder. Journal of affective disorders, 187, 188-196. [CrossRef]
- American Psychiatric Association, D. S. M. T. F., & American Psychiatric Association, D. S. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5, No. 5). Washington, DC: American psychiatric association.
- Aymerich, C., Pacho, M., Catalan, A., Yousaf, N., Pérez-Rodríguez, V., Hollocks, M. J.,... & Salazar de Pablo, G. (2024). Prevalence and Correlates of the Concurrence of Autism Spectrum Disorder and Obsessive Compulsive Disorder in Children and Adolescents: A Systematic Review and Meta-Analysis. Brain Sciences, 14(4), 379. [CrossRef]
- Barrett, P. M., & Healy, L. J. (2003). An examination of the cognitive processes involved inchildhood obsessive–compulsive disorder. Behaviour Research and Therapy, 41(3), 285-299. [CrossRef]
- Baxter, A. J., Vos, T., Scott, K. M., Ferrari, A. J., & Whiteford, H. A. (2014). The global burden of anxiety disorders in 2010. Psychological medicine, 44(11), 2363-2374. [CrossRef]
- Blanco-Vieira, T., Radua, J., Marcelino, L., Bloch, M., Mataix-Cols, D., & do Rosário, M. C. (2023). The genetic epidemiology of obsessive-compulsive disorder: a systematic review and meta-analysis. Translational psychiatry, 13(1), 230. [CrossRef]
- Brar, J., Sidana, A., Chauhan, N., & Bajaj, M. K. (2022). Early improvement as a predictor oftreatment response in patients with obsessive-compulsive disorder: A 12-week randomized trial of sertraline and fluvoxamine. The Primary Care Companion for CNS Disorders, 24(2), 40361.
- Carcary, M. (2009). The research audit trial—enhancing trustworthiness in qualitative inquiry. Electronic journal of business research methods, 7(1), pp11-24.
- Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative analysis. sage.
- Chaturvedi, A., Murdick, N. L., & Gartin, B. C. (2014). Obsessive Compulsive Disorder: What an Educator Needs to Know. Physical Disabilities: Education and Related Services, 33(2), 71-83. [CrossRef]
- Chaves, A., Arnáez, S., Roncero, M., & García-Soriano, G. (2021). Teachers' knowledge and stigmatizing attitudes associated with obsessive-compulsive disorder: effectiveness ofa brief educational intervention. Frontiers in psychiatry, 12, 677567. [CrossRef]
- Coluccia, A., Fagiolini, A., Ferretti, F., Pozza, A., Costoloni, G., Bolognesi, S., & Goracci, A. (2016). Adult obsessive–compulsive disorder and quality of life outcomes: a systematic review and meta-analysis. Asian Journal of Psychiatry, 22, 41-52. [CrossRef]
- Crino, R., Slade, T., & Andrews, G. (2005). The changing prevalence and severity of obsessive-compulsive disorder criteria from DSM-III to DSM-IV. American Journal of Psychiatry, 162(5), 876-882. [CrossRef]
- Dyches, T. T., Leininger, M., Heath, M. A., & Prater, M. A. (2010). Understanding obsessive-compulsive disorder in students: symptoms and school-based interventions.School Social Work Journal, 34(2), 35-55.
- Elliott, R., & Timulak, L. (2005). Descriptive and interpretive approaches to qualitative research. A handbook of research methods for clinical and health psychology, 1(7), 147-159.
- Fawcett, E. J., Power, H., & Fawcett, J. M. (2020). Women are at greater risk of OCD than men: a meta-analytic review of OCD prevalence worldwide. The Journal of clinical psychiatry, 81(4), 13075.
- Fennell, D., & Boyd, M. (2014). Obsessive-compulsive disorder in the media. Deviant Behavior, 35(9), 669-686. [CrossRef]
- Fennell, D., & Liberato, A. S. (2007). Learning to live with OCD: Labeling, the self, and stigma. Deviant Behavior, 28(4), 305-331. [CrossRef]
- Ferrando, C., & Selai, C. (2021). A systematic review and meta-analysis on the effectiveness of exposure and response prevention therapy in the treatment of obsessive-compulsivedisorder. Journal of Obsessive-Compulsive and Related Disorders, 31, 100684. [CrossRef]
- Fineberg, N. A., Brown, A., Reghunandanan, S., & Pampaloni, I. (2012). Evidence-based pharmacotherapy of obsessive-compulsive disorder. International Journal of Neuropsychopharmacology, 15(8), 1173-1191. [CrossRef]
- Flick, U. (2022). The SAGE handbook of qualitative research design. [CrossRef]
- Foa, E. B., Liebowitz, M. R., Kozak, M. J., Davies, S., Campeas, R., Franklin, M. E.,... & Tu, X. (2005). Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of psychiatry, 162(1), 151-161.
- Fontenelle, L. F., Mendlowicz, M. V., & Versiani, M. (2006). The descriptive epidemiology of obsessive–compulsive disorder. Progress in Neuro-Psychopharmacology andBiological Psychiatry, 30(3), 327-337. [CrossRef]
- Fontenelle, L. F., Nicolini, H., & Brakoulias, V. (2022). Early intervention in obsessive-compulsive disorder: From theory to practice. Comprehensive Psychiatry, 119, 152353. [CrossRef]
- Frances, A. (2013). The past, present and future of psychiatric diagnosis. World Psychiatry, 12(2), 111. [CrossRef]
- Franklin, M. E., Sapyta, J., Freeman, J. B., Khanna, M., Compton, S., Almirall, D.,... & March, J. S. (2011). Cognitive behavior therapy augmentation of pharmacotherapy inpediatric obsessive-compulsive disorder: the Pediatric OCD Treatment Study II (POTS II) randomized controlled trial. Jama, 306(11), 1224-1232.
- Froese-Germain, B., & Riel, R. (2012). Understanding Teachers' Perspectives on Student Mental Health: Findings from a National Survey. Canadian Teachers' Federation. 2490 Don Reid Drive, Ottawa, ON K1H 1E1, Canada.
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field methods, 18(1), 59-82.
- Helbing, M. L. C., & Ficca, M. (2009). Obsessive-compulsive disorder in school-age children. The Journal of school nursing, 25(1), 15-26. [CrossRef]
- Henin, A., & Kendall, P. C. (1997). Obsessive—Compulsive Disorder in Childhood and Adolescence. In Advances in clinical child psychology (pp. 75-131). Boston, MA: Springer US.
- Horwath, E., & Weissman, M. M. (2022). The epidemiology and cross-national presentation of obsessive-compulsive disorder. Obsessive-Compulsive Disorder and Tourette's Syndrome, 35-49.
- Karno, M., Golding, J. M., Sorenson, S. B., & Burnam, M. A. (1988). The epidemiology of obsessive-compulsive disorder in five US communities. Archives of general psychiatry, 45(12), 1094-1099. [CrossRef]
- Kim, A. J. (2021). The metanarrative of OCD: Deconstructing positive stereotypes in mediaand popular nomenclature. In Metanarratives of Disability (pp. 61-76). Routledge.
- Koch, T. (1994). Establishing rigour in qualitative research: the decision trail. Journal of advanced nursing, 19(5), 976-986. [CrossRef]
- Kratt, D. (2018). Teachers’ perspectives on educator mental health competencies: A qualitative case study. American Journal of Qualitative Research, 2(1), 22-40. [CrossRef]
- Lewis, A. (1936). Problems of obsessional illness. [CrossRef]
- Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Sage.
- Mahjani, B., Bey, K., Boberg, J., & Burton, C. (2021). Genetics of obsessive-compulsive disorder. Psychological Medicine, 51(13), 2247-2259. [CrossRef]
- Mandelli, L., Draghetti, S., Albert, U., De Ronchi, D., & Atti, A. R. (2020). Rates of comorbid obsessive-compulsive disorder in eating disorders: a meta-analysis of the literature. Journal of affective disorders, 277, 927-939. [CrossRef]
- Mao, L., Hu, M., Luo, L., Wu, Y., Lu, Z., & Zou, J. (2022). The effectiveness of exposure and response prevention combined with pharmacotherapy for obsessive-compulsive disorder: A systematic review and meta-analysis. Frontiers in psychiatry, 13, 973838. [CrossRef]
- Martin, S. (2017). Madness in the Media: Demystifying the Emergence of an OCD Trope in Television.
- Mcgrath, K., Riegel, C., & Mete, R. (2023). Teacher Perceptions of Obsessive-Compulsive Disorder. AILACTE Journal, 20, 1-29.
- Murphy, D. L., Timpano, K. R., Wheaton, M. G., Greenberg, B. D., & Miguel, E. C. (2010). Obsessive-compulsive disorder and its related disorders: a reappraisal of obsessive-compulsive spectrum concepts. Dialogues in clinical neuroscience, 12(2), 131-148. [CrossRef]
- Nakatani, E., Krebs, G., Micali, N., Turner, C., Heyman, I., & Mataix-Cols, D. (2011). Children with very early onset obsessive-compulsive disorder: Clinical features and treatment outcome. Journal of Child Psychology and Psychiatry, 52(12), 1261-1268. [CrossRef]
- Nazeer, A., Latif, F., Mondal, A., Azeem, M. W., & Greydanus, D. E. (2020). Obsessive-compulsive disorder in children and adolescents: epidemiology, diagnosis, and management. Translational pediatrics, 9(Suppl 1), S76.
- Negreiros, J., Best, J. R., Vallani, T., Belschner, L., Szymanski, J., & Stewart, S. E. (2023). Obsessive-compulsive disorder (OCD) in the school: Parental experiences regarding impacts and disclosure. Journal of Child and Family Studies, 32(9), 2848-2857. [CrossRef]
- Nicolini, H., Arnold, P., Nestadt, G., Lanzagorta, N., & Kennedy, J. L. (2009). Overview of genetics and obsessive–compulsive disorder. Psychiatry research, 170(1), 7-14. [CrossRef]
- Oliveira, M., Slezakova, K., Delerue-Matos, C., Pereira, M. C., & Morais, S. (2019). Children environmental exposure to particulate matter and polycyclic aromatic hydrocarbons and biomonitoring in school environments: A review on indoor and outdoor exposure levels, major sources and health impacts. Environment international, 124, 180-204. [CrossRef]
- Parker, C., Scott, S., & Geddes, A. (2019). Snowball sampling. SAGE research methods foundations.
- Pérez-Vigil, A., de la Cruz, L. F., Brander, G., Isomura, K., Jangmo, A., Feldman, I.,... & Mataix-Cols, D. (2018). Association of obsessive-compulsive disorder with objective indicators of educational attainment: a nationwide register-based sibling control study. JAMA psychiatry, 75(1), 47-55. [CrossRef]
- Presta, S., Marazziti, D., Dell’Osso, L., Pfanner, C., Pfanner, P., Marcheschi, M.,... & Cassano, G. B. (2003). Obsessive-compulsive disorder in childhood and adolescence. Psychopathology, 36(2), 55-64. [CrossRef]
- Quarantini, L. C., Torres, A. R., Sampaio, A. S., Fossaluza, V., de Mathis, M. A., Do Rosário, M. C.,... & Koenen, K. C. (2011). Comorbid major depression in obsessive-compulsive disorder patients. Comprehensive psychiatry, 52(4), 386-393. [CrossRef]
- Reid, J. E., Laws, K. R., Drummond, L., Vismara, M., Grancini, B., Mpavaenda, D., & Fineberg, N. A. (2021). Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive-compulsive disorder: A systematic review and meta-analysis of randomised controlled trials. Comprehensive psychiatry, 106, 152223. [CrossRef]
- Remmerswaal, K. C., Batelaan, N. M., Hoogendoorn, A. W., van der Wee, N. J., van Oppen, P., & van Balkom, A. J. (2020). Four-year course of quality of life and obsessive–compulsive disorder. Social Psychiatry and Psychiatric Epidemiology, 55, 989-1000.
- Roh, D., Jang, K. W., & Kim, C. H. (2023). Clinical Advances in Treatment Strategies for Obsessive-compulsive Disorder in Adults. Clinical Psychopharmacology and Neuroscience, 21(4), 676. [CrossRef]
- Rosa-Alcázar, A. I., Sánchez-Meca, J., Gómez-Conesa, A., & Marín-Martínez, F. (2008). Psychological treatment of obsessive–compulsive disorder: A meta-analysis. Clinical psychology review, 28(8), 1310-1325.
- Ruscio, A. M., Stein, D. J., Chiu, W. T., & Kessler, R. C. (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular psychiatry, 15(1), 53-63. [CrossRef]
- Sabol, T. J., & Pianta, R. C. (2012). Recent trends in research on teacher–child relationships. Attachment & human development, 14(3), 213-231. [CrossRef]
- Shafran, R. (2001). Obsessive-compulsive disorder in children and adolescents. Child Psychology and Psychiatry Review, 6(2), 50-58.
- Sharma, E., Sharma, L. P., Balachander, S., Lin, B., Manohar, H., Khanna, P.,... & Stewart, S. E. (2021). Comorbidities in obsessive-compulsive disorder across the lifespan: a systematic review and meta-analysis. Frontiers in psychiatry, 12, 703701. [CrossRef]
- Sharma, E., Thennarasu, K., & Reddy, Y. J. (2014). Long-term outcome of obsessive-compulsive disorder in adults: a meta-analysis. The Journal of clinical psychiatry, 75(9), 10746.
- Singh, A., Anjankar, V. P., & Sapkale, B. (2023). Obsessive-compulsive disorder (OCD): a comprehensive review of diagnosis, comorbidities, and treatment approaches. Cureus, 15(11).
- Skapinakis, P., Caldwell, D. M., Hollingworth, W., Bryden, P., Fineberg, N. A., Salkovskis, P.,... & Lewis, G. (2020). Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: A systematic review and network meta-analysis. Focus, 19(4), 457-467. [CrossRef]
- Stahnke, B. (2021). A systematic review of misdiagnosis in those with obsessive-compulsive disorder. Journal of affective disorders reports, 6, 100231. [CrossRef]
- Stein, D. J., Costa, D. L., Lochner, C., Miguel, E. C., Reddy, Y. J., Shavitt, R. G.,... & Simpson, H. B. (2019). Obsessive–compulsive disorder. Nature reviews Disease primers, 5(1), 52.
- Stewart, S. E., Geller, D. A., Jenike, M., Pauls, D., Shaw, D., Mullin, B., & Faraone, S. V. (2004). Long-term outcome of pediatric obsessive–compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatrica Scandinavica, 110(1), 4-13.
- Storch, E. A., Ledley, D. R., Lewin, A. B., Murphy, T. K., Johns, N. B., Goodman, W. K., & Geffken, G. R. (2006). Peer victimization in children with obsessive–compulsive disorder: relations with symptoms of psychopathology. Journal of Clinical Child and Adolescent Psychology, 35(3), 446-455. [CrossRef]
- Taylor, S. (2011). Early versus late onset obsessive–compulsive disorder: evidence for distinct subtypes. Clinical psychology review, 31(7), 1083-1100. [CrossRef]
- Thompson, E. M., Torres, A. R., Albertella, L., Ferrão, Y. A., Tiego, J., Shavitt, R. G.,... & Fontenelle, L. F. (2020). The speed of progression towards obsessive-compulsive disorder. Journal of affective disorders, 264, 181-186. [CrossRef]
- Tini, E., Smigielski, L., Romanos, M., Wewetzer, C., Karwautz, A., Reitzle, K.,... & Walitza, S. (2022). Therapeutic drug monitoring of sertraline in children and adolescents: A naturalistic study with insights into the clinical response and treatment of obsessive-compulsive disorder. Comprehensive psychiatry, 115, 152301. [CrossRef]
- Tolin, D. F., & Worden, B. L. (2012). Combining pharmacotherapy and psychological treatments for OCD. Oxford handbook of obsessive compulsive and spectrum disorders, 365-375.
- Tollefson, G. D., Rampey, A. H., Potvin, J. H., Jenike, M. A., Rush, A. J., Dominguez, R. A.,... & Genduso, L. A. (2022). A multicenter investigation of fixed-dose fluoxetine in the treatment of obsessive-compulsive disorder. In Obsessive-Compulsive Disorder and Tourette's Syndrome (pp. 237-245). Routledge.
- Van Manen, M. (2023). Phenomenology of practice: Meaning-giving methods in phenomenological research and writing. Routledge.
- Vickers, A. J., & Altman, D. G. (2001). Analysing controlled trials with baseline and follow up measurements. Bmj, 323(7321), 1123-1124.
- Walitza, S., Melfsen, S., Jans, T., Zellmann, H., Wewetzer, C., & Warnke, A. (2011). Obsessive-compulsive disorder in children and adolescents. Deutsches Ärzteblatt International, 108(11), 173.
- World Health Organisation. (2023). Obsessive- compulsive disorder (OCD). https://applications.emro.who.int/docs/WHOEMMNH232E-eng.pdf?ua=1.
- Woolcock, E., & Campbell, M. A. (2005). The role of teachers in the support of students with obsessive-compulsive disorder. The Australian Educational and Developmental Psychologist, 22(1), 54-64. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




