1. Introduction
Colorectal cancer represents the third most common disease in terms of morbidity as well as mortality worldwide, and it can be anticipated that the prevalence of this disease will continue to rise in the future. What is alarming, however, is the decreasing age threshold for the incidence of the disease. Therefore, screening for the disease is essential, and optimizing patient management is crucial. Currently, tumor resection is considered the curative option for colorectal lesions. In the case of rectal tumors, the treatment is multimodal, ranging from primary resection to neoadjuvant therapy, total neoadjuvant therapy, and adjuvant therapy.
Rectal surgery has rapidly developed in recent decades, with significant improvements in surgical techniques, instrumentation, and patient management in oncological treatment. These advances have substantially improved patient prognosis in the perioperative and postoperative periods. One of the cornerstones of rectal surgery is the introduction of total mesorectal excision (TME), which is the gold standard for rectal cancer surgery. There is widespread consensus on the importance of achieving an intact excision of the mesorectum with adequate clear circumferential and longitudinal margins [
1]. However, there remains ongoing debate about the height of ligation of the inferior mesenteric artery (IMA) during rectal resection. The IMA can be ligated either proximal or distal to the left colic artery. High-tie (HT) ligation is achieved by transecting the IMA 1 cm distally from the aorta. Low-tie (LT) ligation, on the other hand, is achieved by transecting the IMA 1 cm distally to the origin of the left colic artery (LCA) However, it is unclear whether the height of ligation affects postoperative complications and oncological outcomes [
2].
The primary hypothesis is that higher ligation leads to the removal of a greater number of lymph nodes, which may improve prognosis. Conversely, low ligation is thought to result in fewer postoperative and functional injuries, with a lower risk of injury to the autonomic innervation and vascular supply and thus a lower risk of anastomotic dehiscence [
3]. This dilemma has led to the creation of numerous surgical protocols and recommendations for the management of rectal cancer patients [
4,
5,
6].
Many systematic reviews and meta-analyses have been published on this topic in the last five years, and a recent randomized controlled trial (RCT) provided new data [
7] (
Table 1).
Our study focuses on the analysis of postoperative complications associated with low ligation of the IMA after resection of the upper and middle rectum. We primarily monitored the local recurrence and overall survival in patients – 96 patients, over a seven-year follow-up period, comparing these results with the recent literature. The primary aim of the study was to assess the oncological outcomes of patients with low tie ligation of the inferior mesenteric artery in comparison with the literature.
2. Materials and Methods
This prospective study exclusively included patients with upper and middle rectal cancer treated at the 3rd Surgical Clinic, Faculty of Medicine, Comenius University in Bratislava, Slovakia, between September 2013 and September 2017. Patients were informed about the procedures and treatment, with which they agreed and confirmed by signing the informed consent.. A total of 96 patients who underwent primary surgical resection were included, consisting of 44 females and 52 males. The patients were subdivided into two groups based on the tumor's distance from the anus: the first group included upper rectal tumors (12-16 cm from the anus), and the second group included middle rectal tumors (6-12 cm from the anus). The inclusion criteria were upper or middle rectal tumors with indications for primary surgical resection, based on MR staging (T1-T3b, CRM negative, EMVI negative), and no evidence of disease dissemination.
Exclusion criteria included patients with metastatic disease, prior surgery on the left-sided colon, local excision of the rectum, Hartmann’s procedure, or severe atherosclerosis. The primary aim of the study was to assess the oncological outcomes of patients with low tie ligation of the inferior mesenteric artery in comparison with the literature.
All the included patients had indications for primary rectal resection without neoadjuvant therapy. Presurgical tumor evaluation included a physical examination with a digital rectal exam and anoscopy, serum CEA and CA19-9, total colonoscopy with biopsy, pelvic MRI, and CT.
The surgical procedure was performed laparoscopically by three colorectal surgeons, with laparotomy used only in exceptional cases. In all cases, a latero-medial approach was used for dissection. The specimen was then removed through a small abdominal incision, and the proximal colon was transected approximately 10 cm above the lesion [
8].
In all the laparoscopically performed surgeries, distal resection was performed using a laparoscopic linear stapler (Endo Gia), while the laparotomy cases used Contour staplers. The proximal stump was treated using tabular forceps. An end-to-end circular stapler anastomosis was performed.
Data were evaluated statistically using Fisher’s exact test, and differences between two groups were evaluated using the Chi-square test. A p-value of < 0.05 was considered statistically significant (tab2).
3. Results
A total of 96 patients were included in the study (44 females and 52 males). The inclusion criteria were upper or middle rectal tumors with indications for primary surgical resection, based on MR staging (T1-T3b, CRM negative, EMVI negative), and no evidence of disease dissemination. Of the 96 patients, 36 had upper rectal tumors and 60 had middle rectal tumors. The average age of the patients was 68.4 years, with ASA scores ranging from I to III and a BMI 27,2±4 (
Table 2).
A laparoscopic approach was performed in 83 patients (86.46%), with 35 patients (97.22%) in the upper rectum group and 48 patients (80%) in the middle rectum group. In 10 patients (10.42%), laparoscopic surgery was converted to laparotomy, and 3 patients (3,12%) had primary laparotomy due to comorbidities. Mobilization of the splenic flexure was performed in 16 cases (16.67%), particularly in the middle rectal tumor group.
In all the laparoscopically performed surgeries, distal resection was performed using a laparoscopic linear stapler (Endo Gia), while the laparotomy cases used Contour staplers. The proximal stump was treated using tabular forceps. An end-to-end circular stapler anastomosis was performed. A protective stoma was created in four cases. The average length of hospital stay was 5.8 days, with the first peristalsis occurring on the second postoperative day and first passage of gas on the third postoperative day.
The minimum number of lymph nodes harvested was 12, with an average of 17. No suspicion of positive apical lymph nodes was found in the preoperative imaging. Postoperative complications included one death on the second postoperative day due to a massive myocardial infarction. Five cases of anastomotic dehiscence were recorded, of which three were asymptomatic (two in middle rectum group, one in upper rectum group) and managed conservatively, and two required revision and a temporary stoma (one patient in both groups) (
Table 3).
Long-term follow-up (7 years) showed six deaths: three patients died due to the dissemination of the disease, and three patients died from other causes, two of them because of cardiovascular disease and one because of acute leukemia. Two patients were lost to follow-up due to non-compliance – they came not to oncological checks. Two patients in the definitive histopathological examination had a benign tumor. Of the 94 patients with confirmed rectal adenocarcinoma, local recurrence occurred in 5 patients (5.81%) at least 7 years after surgery. All five patients had R0 resections, and recurrence was identified within two years post-surgery. One of the five patients had a preoperative N+ status, while the other patients had an N- status. Just one patient in group of middle rectum tumor had a positive postoperative lymph status.
4. Discussion
Rectal cancer remains one of the most common gastrointestinal malignancies, and its prevalence is likely to increase in the near future [
9]. The five-year overall survival (OS) for non-metastatic colorectal cancer is directly correlated to the pTNM classification and is 95% for stage I, 76% for stage II, and 64% for stage III disease [
10,
11]. Although the prognosis is relatively favorable for patients with stage I and II colon cancer, 30% of patients will experience a systemic disease recurrence [
12].
The question of managing patients with rectal cancer remains highly relevant. Despite significant advancements in this area, there are still many unanswered or controversial debates regarding the treatment approaches for patients with rectal cancer. One such debate concerns the implementation of high versus low ligation of the inferior mesenteric artery (IMA) and its oncological impact on the patient. High-tie (HT) ligation is achieved by transecting the IMA 1 cm distally from the aorta. Low-tie (LT) ligation, on the other hand, is achieved by transecting the IMA 1 cm distally to the origin of the left colic artery (LCA) to allow for the preservation of the LCA [
13]. The primary assumption of high ligation of the IMA is to obtain a larger number of lymph nodes, which should positively influence the patient's prognosis. Furthermore, the HT ligation approach would lead to an additional gain in the length of the lowered colon [
14]. Conversely, proponents of low ligation argue for a lower risk of damaging autonomic innervation, thereby reducing the risk of sexual dysfunction, dysfunction of the urinary tract, or defecation disorders. Fuji and colleagues published a study where they essentially found no significant difference in the number of lymph nodes retrieved between high and low IMA ligation [
15]. However, a much more fundamental issue seems to be the extirpation of apical lymph nodes in patients with suspected metastatic involvement of these nodes [
16]. The presence of positive apical nodes is a negative prognostic factor, but positive apical nodes are only found in 1.7% of cases [
17,
18]. A tailored approach was suggested by the American Society of Colon and Rectal Surgeons (ASCRS) in the practice parameters for the management of rectal cancer. High ligation of the IMA at its origin is not associated with any survival advantage [
19], but it is still recommended when clinically enlarged lymph nodes are visible up to the root of the IMA [
20]. Ultimately, while Japanese clinicians prefer more extensive lymph node dissection for tumors larger than T2 in the belief that this is associated with better overall survival (OS) and disease-free survival (DFS) [
21] (
Table 4), American guidelines favor less extensive node dissection, as positive apical nodes are rare.
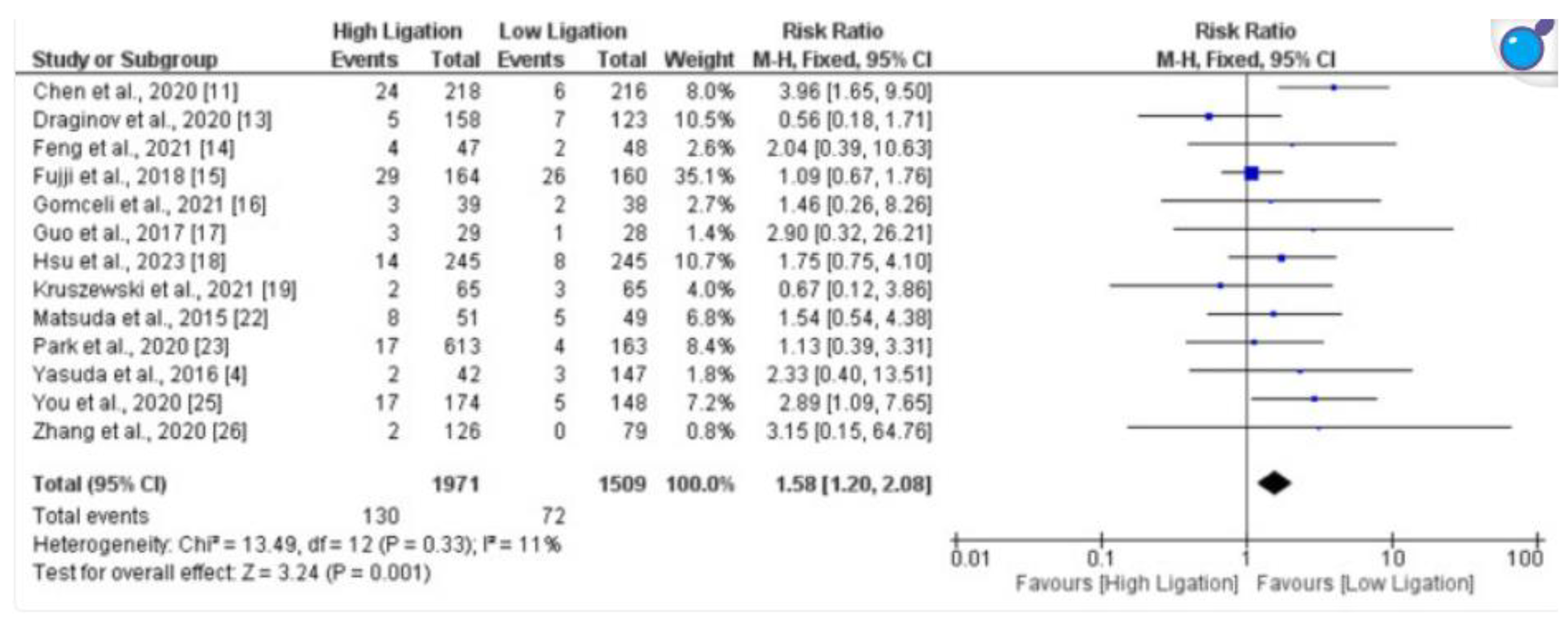
Another important question regarding the height of IMA ligation is the risk of anastomotic dehiscence, which may be influenced by poor blood supply or anastomosis under tension. Proponents of low ligation believe that performing low ligation maintains a better blood supply to the proximal colonic limb (3). Even in this question, we find ambiguous answers. While a meta-analysis by Reyaz and colleagues describes a lower risk of anastomotic dehiscence (risk ratio, 1.58; 95% confidence interval, 1.20–2.08) and an earlier onset of flatulence in patients with low ligation [
22], this difference was not confirmed in other studies by Lee and colleagues or Fuji and colleagues [
23,
24]. In our study we found 5 anastomotic leaks(AL), but in comparison to the literature is it not worse than in group with high ligation (
Table 5).
An often-underestimated fact is the postoperative condition of the patient. High IMA ligation is associated with a higher risk of damage to autonomic innervation, leading to dysfunction of the urinary tract, defecation mechanism, or sexual dysfunction. Lee et al. [
23] explored the impact on defecatory function and found that the Fecal Incontinence Severity Index scores were better in the group that underwent low ligation. Similarly, Koda et al. [
25] examined the effects of high versus low IMA ligation on defecatory disorders following low anterior resection for rectal cancer. Their study observed spastic waves in the neorectum of the high ligation group, which they suggested could lead to incomplete fecal evacuation and subsequent defecatory dysfunction.
A possible diagnostic techniques is the use of indocyanine green (ICG) in the staging of lymph nodes, which could provide more insight into the extent of lymph node dissection perioperatively and could help to determine the height of the necessary ligation. ICG-FI for SLN detection in patients treated for primary colorectal cancer has been clearly demonstrated to be a safe and feasible technique with a detection rate of 65.5%–100% for colon cancer and 28%–92% for rectal cancer [
26].
It is therefore essential to standardize procedures in the treatment of rectal cancers, primarily considering the benefit to the patient; however, it seems that the question of the height of IMA ligation should remain at the discretion of the surgeon based on anatomical conditions. Rather, it has been demonstrated that the quality of the mesorectal excision and the biology of the tumor are much more critical than the height of IMA ligation [
20].
In our study, we also demonstrated that low IMA ligation during resection of the rectum in the upper and middle thirds does not worsen patient survival compared to the literature, even at 7 years’ follow-up. We can already state that well-performed surgical resection, the stage of the disease, and the biology of the tumor are decisive for the patient's prognosis. Because studies do not confirm the oncological significance of IMA ligation during the resection of the upper and middle rectum, this choice should be left to the surgeon and the anatomical conditions of the patient.
References
- West NP, Quirke P. Colon cancer surgery: pathological quality control is essential for optimal outcomes. Colorectal Dis. 2018, 20, 34–35. [Google Scholar] [CrossRef] [PubMed]
- Cirocchi R, Trastulli S, Farinella E, Desiderio J, Vettoretto N, Parisi A et al High tie versus low tie of the inferior mesenteric artery in colorectal cancer: a RCT is needed. Surg Oncol 2012, 21, e111–e123. [CrossRef] [PubMed]
- Kim, K.; An, S.; Kim, M.H.; Jung, J.H.; Kim, Y. High Versus Low Ligation of the Inferior Mesenteric Artery in Colorectal Cancer Surgery: A Systematic Review and Meta-Analysis. Medicina 2022, 58, 1143. [Google Scholar] [CrossRef] [PubMed]
- Cirocchi R, Farinella E, Trastulli S, Desiderio J, Di Rocco G, Covarelli P, et al. High tie versus low tie of the inferior mesenteric artery: a protocol for a systematic review. World J Surg Oncol. 2011, 9, 147. [Google Scholar] [CrossRef] [PubMed]
- Bridoux V, de Chaisemartin C, Beyer L, et al. Recommandations pour la pratique clinique Cancer du rectum. Colon Rectum. 2016, 10, 12–27. [Google Scholar] [CrossRef]
- You YN, Hardiman KM, Bafford A, Poylin V, Francone TD, Davis K, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of rectal cancer. Dis Colon Rectum. 2020, 63, 1191–1222. [Google Scholar] [CrossRef]
- Cirocchi R, Marchetti F, Mari G, Bagolini F, Cavaliere D, Avenia S, Anania G, Tebala G, Donini A, Davies RJ, Fingerhut A. Inferior mesenteric artery ligation level in rectal cancer surgery: still no answer-a systematic review and meta-analysis. Langenbecks Arch Surg. 2023, 408, 286. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carmichael JC, Keller DS, Baldini G, et al. , Clinical practice guideline for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgeons (ASCRS) and Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Surg Endosc 2017, 31, 3412–3436. [Google Scholar] [CrossRef] [PubMed]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Andre, T. , Boni C, Navarro M, et al. , Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial, J Clin Oncol. 2009, 27, 3109–3116. [Google Scholar] [CrossRef]
- Siegel R, Ma J, Zou Z, et al. , Cancer Statistics. CA Cancer J Clin. 2014, 64, 9–29. [Google Scholar]
- Andre T, Boni C, Mounedji – Boudiaf L, et al. , Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004, 350, 2343–2351. [Google Scholar] [CrossRef] [PubMed]
- Nayeri M, Iskander O, Tabchouri N, et al. , Low Tie Compared to High Tie Vascular Ligation of the Inferior Mesenteric Artery in Rectal Cancer Surgery Decreases Postoperative Complications Without Affecting Overall Survival. Anticancer Research August 2019, 39, 4363–4370. [Google Scholar] [CrossRef]
- Bonnet S, Berger A, Hentati N, et al. , High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses., Dis Colon Rectum 2012, 55, 515–521. [CrossRef] [PubMed]
- Fujii, S.; Ishibe, A.; Ota, M.; Watanabe, K.; Watanabe, J.; Kunisaki, C.; Endo, I. Randomized clinical trial of high versus low inferior mesenteric artery ligation during anterior resection for rectal cancer. BJS Open 2018, 2, 195–202. [Google Scholar] [CrossRef]
- Jonnada, P.K.; Karunakaran, M.; Rao, D. Outcomes of level of ligation of inferior mesenteric artery in colorectal cancer: A systematic review and meta-analysis. Future Oncol. 2021, 17, 3645–3661. [Google Scholar] [CrossRef] [PubMed]
- Kang J, Hur H, Min BS, et al. , Prognostic impact of inferior mesenteric artery lymph node metastasis in colorectal cancer. Ann Surg Oncol 2011, 18, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Kanemitsu Y, Hirai T, Komori K, et al. , Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg 2006, 93, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Rouffet F, Hay JM, Vacher B, Fingerhut A, Elhadad A, Flamant Y, Mathon C, Gainant A Curative resection for left colonic carcinoma: hemicolectomy vs segmental colectomy. A prospective, controlled, multicenter trial avec The French Association for Surgical Research. Dis Colon Rectum 1994, 37, 651–659. [Google Scholar]
- Tjandra JJ, Kilkenny JW, Buie WD, Hyman N, Simmang C, Anthony T, et al. Practice parameters for the management of rectal cancer (revised). Dis Colon Rectum. 2005, 48, 411–423. [Google Scholar] [CrossRef] [PubMed]
- Matsuda K, Yokoyama S, Hotta T, Takifuji K, Watanabe T, Tamura K, et al. Oncological outcomes following rectal cancer surgery with high or low ligation of the inferior mesenteric artery. Gastrointest Tumors. 2017, 4, 45–52. [Google Scholar] [CrossRef]
- Reyaz I, Reyaz N, Salah QM, Nagi TK, Mian AR, Bhatti AH, et al. Comparison of high ligation versus low ligation of the inferior mesenteric artery (IMA) on short-term and long-term outcomes in sigmoid colon and rectal cancer surgery: a meta-analysis. Cureus 2023, 15, e39406. [Google Scholar]
- Lee MW, Park SS, You K, Lee DE, Lee DW, Park SC, et al. Longterm clinical outcomes after high and low ligations with lymph node dissection around the root of the inferior mesenteric artery in patients with rectal cancer. Ann Coloproctol 2024, 40. [Google Scholar]
- Fujii S, Ishibe A, Ota M, Suwa H, Watanabe J, Kunisaki C, et al. Short-term and long-term results of a randomized study comparing high tie and low tie inferior mesenteric artery ligation in laparoscopic rectal anterior resection: subanalysis of the HTLT (high tie vs. low tie) study. Surg Endosc 2019, 33, 1100–10. [Google Scholar] [CrossRef]
- Koda K, Saito N, Seike K, Shimizu K, Kosugi C, Miyazaki M. Denervation of the neorectum as a potential cause of defecatory disorder following low anterior resection for rectal cancer. Dis Colon Rectum 2005, 48, 210–7. [Google Scholar] [CrossRef] [PubMed]
- Currie AC, Brigic A, Thomas-Gibson S, et al. , A pilot study to assess near infrared laparoscopy with indocyanine green (ICG) for intraoperative sentinel lymph node mapping in early colon cancer. Eur J Surg Oncol. 2017, 43, 2044–2051. [Google Scholar] [CrossRef] [PubMed]
Table 1.
RCT, randomized control study;
CCT, clinical control study, Systematic reviews and meta-analysis published in the last 5 years [
7].
Table 1.
RCT, randomized control study;
CCT, clinical control study, Systematic reviews and meta-analysis published in the last 5 years [
7].
| Authors |
RCTs included |
CCTs included |
Functional outcomes |
Short term outcomes |
Long term outcomes |
| Tryliskyy et al. (2022) |
3 |
0 |
x |
|
|
| Kim et al. (2022) |
12 |
0 |
x |
x |
x |
| Kong et al. (2021) |
5 |
0 |
|
x |
x |
| Bai et al. (2021) |
5 |
9 |
x |
x |
x |
| Jonnada et al. (2021) |
31 |
0 |
x |
x |
x |
| Yin et al. (2021) |
4 |
17 |
x |
x |
x |
Table 2.
Patients characteristics.
Table 2.
Patients characteristics.
| N |
96 |
| Male |
52 |
| Female |
44 |
| ASA 1 |
16 |
| ASA 2 |
63 |
| ASA 3 |
17 |
| BMI |
27,2±4 |
| Age |
68,4 average |
| Upper rectum |
36 |
| Middle rectum |
60 |
| Stage I |
34 |
| Stage II |
41 |
| Stage III |
21 |
| Adenocarcinoma |
94 |
Table 3.
perioperative characteristics.
Table 3.
perioperative characteristics.
| Laparoscopic |
83 |
| Conversion |
10 |
| Laparotomy |
3 |
| Operation time |
170±60 |
| Blood loss (ml) |
80±40 |
| Harvested lymph nodes |
17±4 |
| TME – total mesorectal excision |
82 |
| Complete |
71 |
| Near complete |
11 |
| PME – partial mesorectal excision |
14 |
Table 5.
:
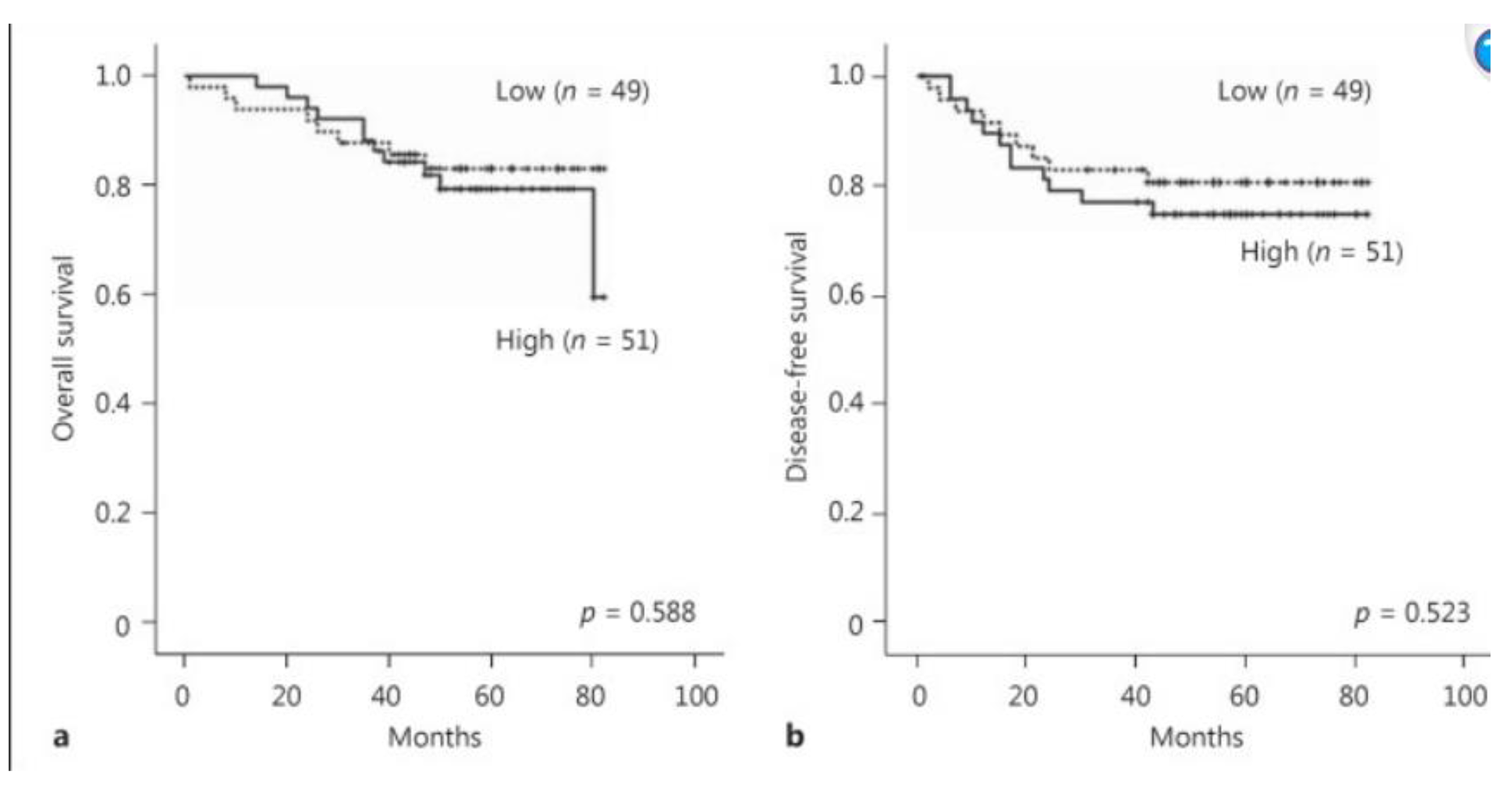
a Cumulative overall survival rates in patients with high ligation (solid line) and low ligation (dotted
line). There is no difference between the two groups (
p = 0.588).
b Cumulative disease-free survival rates in patients with high ligation (solid line) and low ligation (dotted line). There is no difference between the two
groups (
p = 0.523) [
21].
Table 5.
:
a Cumulative overall survival rates in patients with high ligation (solid line) and low ligation (dotted
line). There is no difference between the two groups (
p = 0.588).
b Cumulative disease-free survival rates in patients with high ligation (solid line) and low ligation (dotted line). There is no difference between the two
groups (
p = 0.523) [
21].
Table 5.
Anostomic leaks studies [
22].
Table 5.
Anostomic leaks studies [
22].
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).