1. Introduction
Increased detection of non-palpable tumors emphasizes the need for precise preoperative marking and accurate specimen orientation for effective evaluation [
1]. Accurate specimen orientation during breast cancer surgery is crucial for proper pathological evaluation and ensuring complete tumor resection [
1]. Intraoperative misorientation of resected tissue can lead to errors in margin assessment, potentially misorienting re-excisions, and increasing the risk of local recurrence. Traditionally, surgeons rely on suture or clip marking techniques to orient specimens by indicating anatomical directions [
2]. However, these methods are prone to variability, primarily due to the mobility and torsion of excised breast tissue during surgery and transportation to pathology.
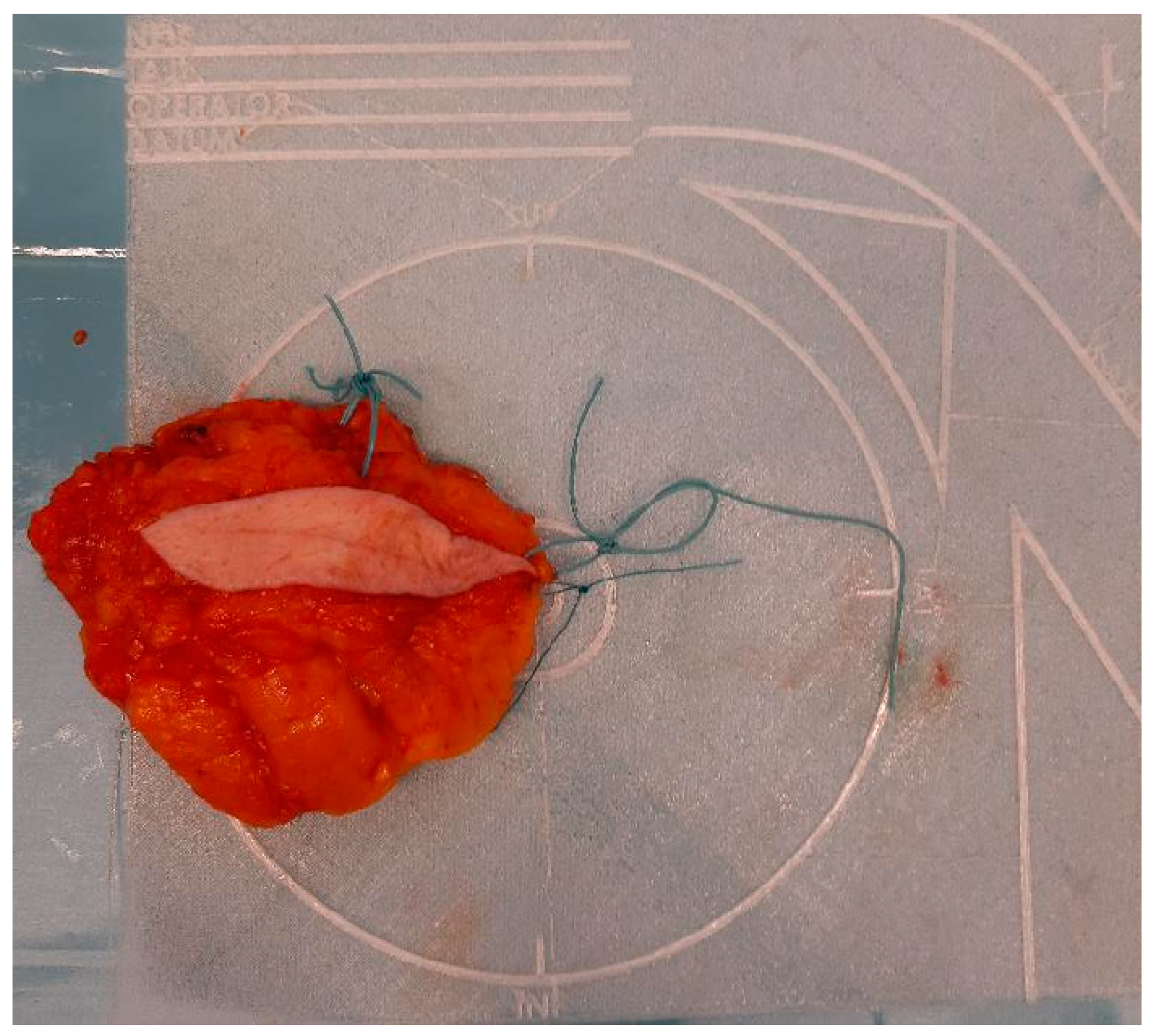
To address the limitations of current practices, a novel specimen plate was previously developed and introduced to mitigate [
3] the risk of misorientation (
Figure 1).
The specimen plate design was based on the feedback from a nationwide, structured, formal survey conducted via an online questionnaire among Hungarian breast cancer centers. This survey systematically assessed current challenges in specimen orientation, the limitations of traditional marking techniques, and the specific needs of surgeons and pathologists. The collected data provided objective insights into the variability in orientation practices and the demand for a standardized, reproducible method to improve pathological accuracy [
4].
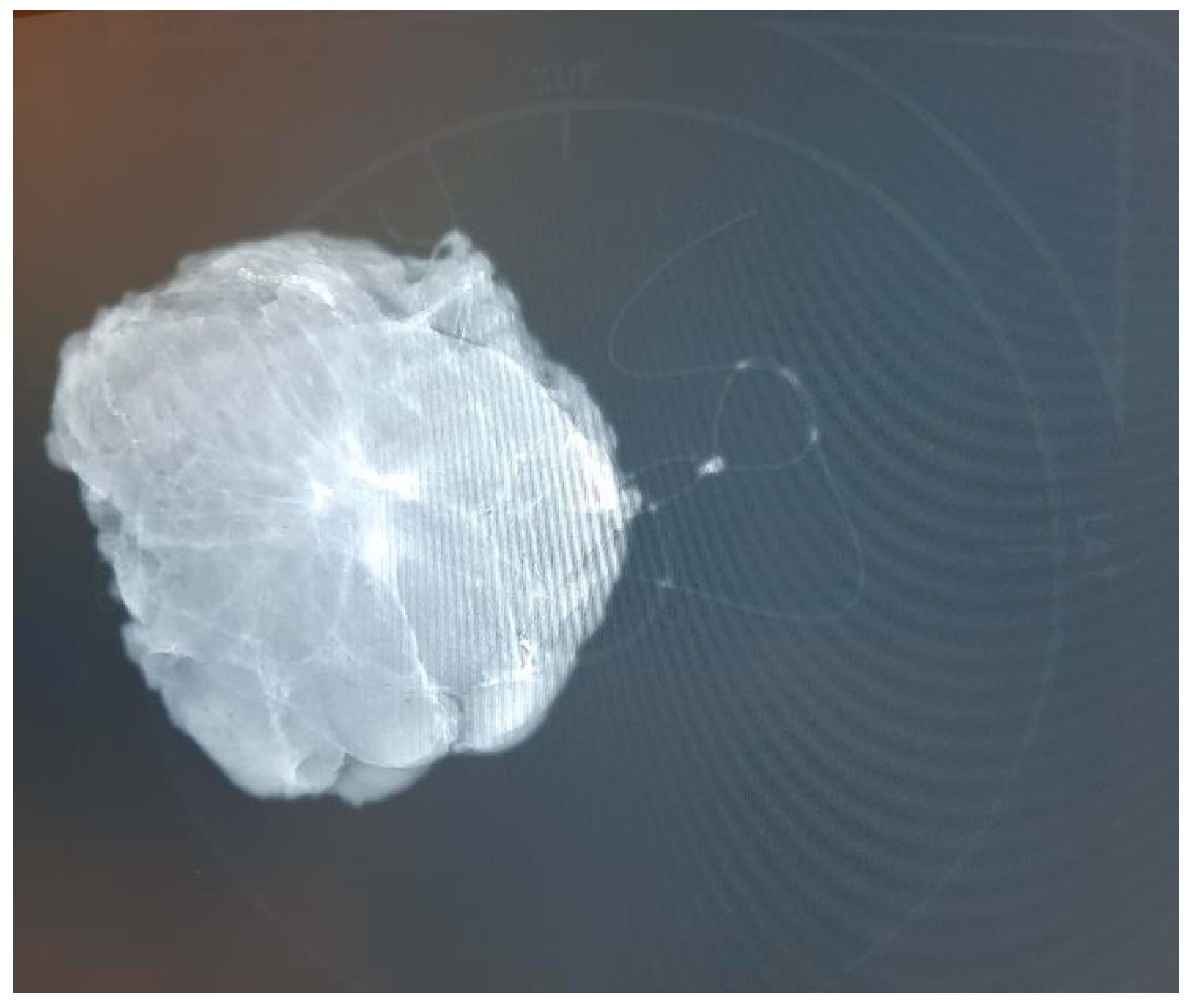
Based on survey data, we developed a specimen plate that securely anchors excised breast tissue on a reproducible coronal plane, thereby enhancing orientation accuracy for both surgeons and pathologists. Additionally, the breast scheme on the plate is clearly visible in the frontal plane, facilitating the visualization of the excised tissue and tumor’s in vivo position in this orientation. The plate enables specimen mammography without causing a disruptive X-ray shadow, as the material is radiolucent. This ensures that the plate does not interfere with standard imaging orientations. Radiologists typically rely on craniocaudal (CC) and mediolateral oblique (MLO) views when assessing breast lesions in mammographic imaging. However, surgeons usually conceptualize the tumor’s position within the breast in the coronal or frontal plane, which aligns more closely with their intraoperative perspective. A coronal plane image, supplemented by the breast scheme on the specimen plate, not only aids in avoiding misinterpretations but also enhances precision in margin assessment. By integrating this additional imaging perspective, the specimen plate facilitates a clearer understanding of the tumor’s in vivo location and improves the accuracy of pathological evaluation. (
Figure 2).
Despite its theoretical promise, the efficacy and real value of the specimen plate relative to traditional suture marking techniques required objective comparative investigation. A single-center, prospective, randomized comparative study was conducted to evaluate the scalable differences between traditional suture marking and the novel specimen plate in orienting resected breast tissue.
2. Patients and Methods
2.1. Study Design
A single-center, prospective, randomized, non-blinded comparative intervention study was conducted at the Surgical Department our high-volume cancer-center university teaching hospital.
2.2. Patient Selection and Randomization
A total of 110 consecutive female patients, aged 29 to 86 years (mean age: 60.63 ± 11.82 years), diagnosed with malignant breast lesions and undergoing breast-conserving surgery, were enrolled in the study. Patients were randomly assigned to two groups based on the resected breast tissue marking methods used during their surgery. Randomization was carried out using a random number generator. 56 patients were allocated into the Specimen Plate group, while the traditional suture marking group consisted of 54 patients. Specimens in the latter group were transported to the pathology department in standard pathological specimen containers. Patient safety was maintained by additional (standard) suture markings in the Specimen Plate group meaning that in this group both techniques were used simultaneously.
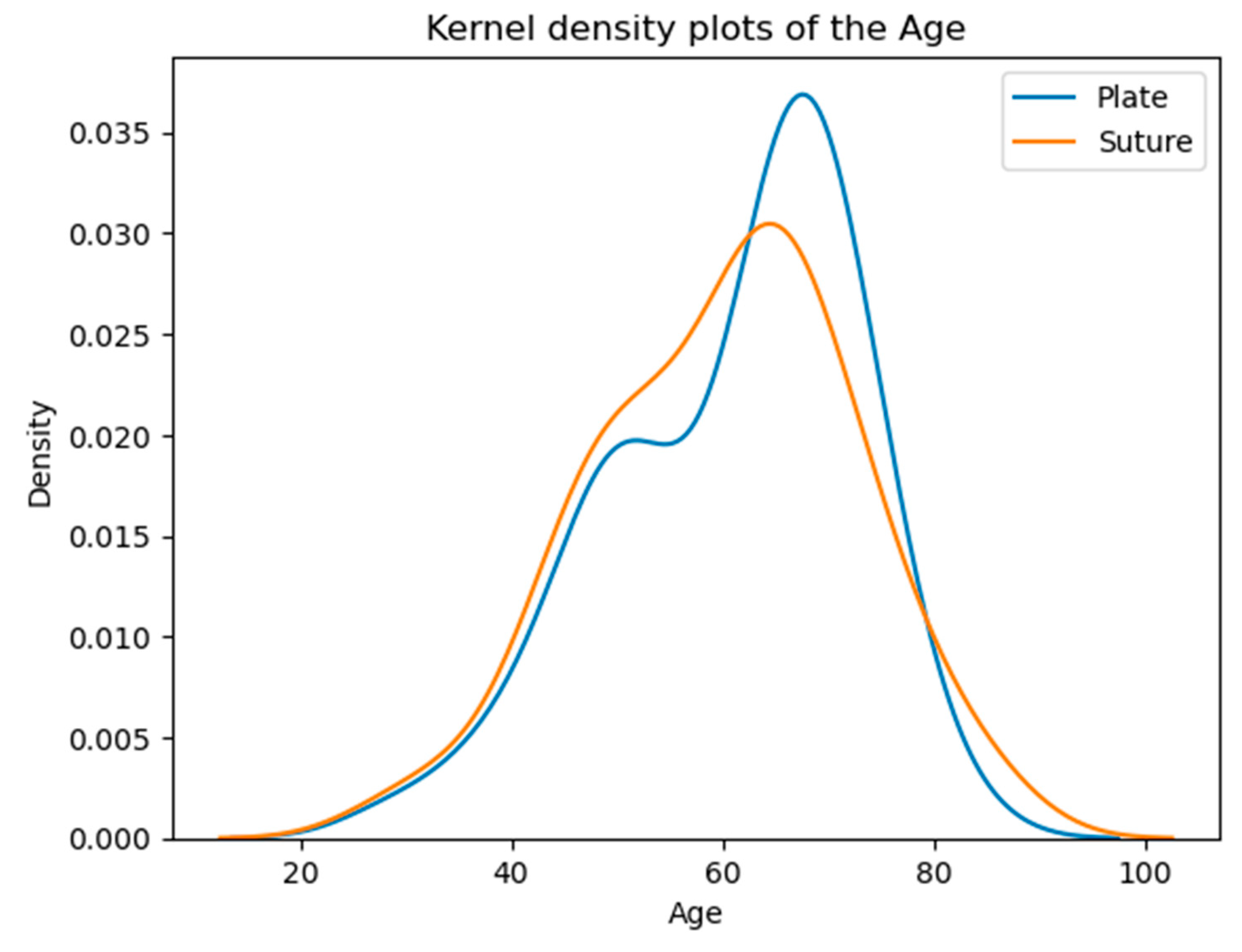
2.3. Ages of Patients in the Examined Groups at the Time of the Operation
The majority of patients fall within the 50-70 age range, with a noticeable peak around the 60s. The overall similarity in average and median ages suggests comparable age demographics across both groups (
Table 1,
Figure 3).
2.4. Specimen Orientation Assessment
Specimen orientation was assessed based on predefined criteria, including clarity of orientation upon arrival at pathology, tumor localization within the specimen (both macroscopically and based on the mammogram), and side-specific clarity.
2.5. Statistical Analyses
For statistical analysis, we utilized Python 3.11.5 along with the following packages: Pandas 2.0.3, Scipy 1.11.1, Seaborn 0.12.2, and Matplotlib 3.7.2. The statistical methods included the z-test (u-test) for proportions, using a significance level of 5% (0.05), with results deemed significant if p<0.05. Additionally, confidence intervals were calculated for specific analyses using multiple methods, including normal approximation, Agresti-Coull, beta, Wilson, and binomial tests.
2.5. Criteria for Assessing Specimen Orientation
Specimen orientation was assessed using the following questions:
A: Was the orientation clearly maintained upon arrival at pathology?
B: Was tumor localization clearly identifiable on the mammogram?
C: Were the specimen’s sides clearly identifiable?
D: Was tumor localization clearly evident on macroscopic examination?
E: Was neoadjuvant therapy performed?
F: Was there complete radiologic or pathologic regression, or no regression?
G: Could the specimen be rotated 180 degrees?
3. Results
3.1. Specimen Orientation and Tumor Localization
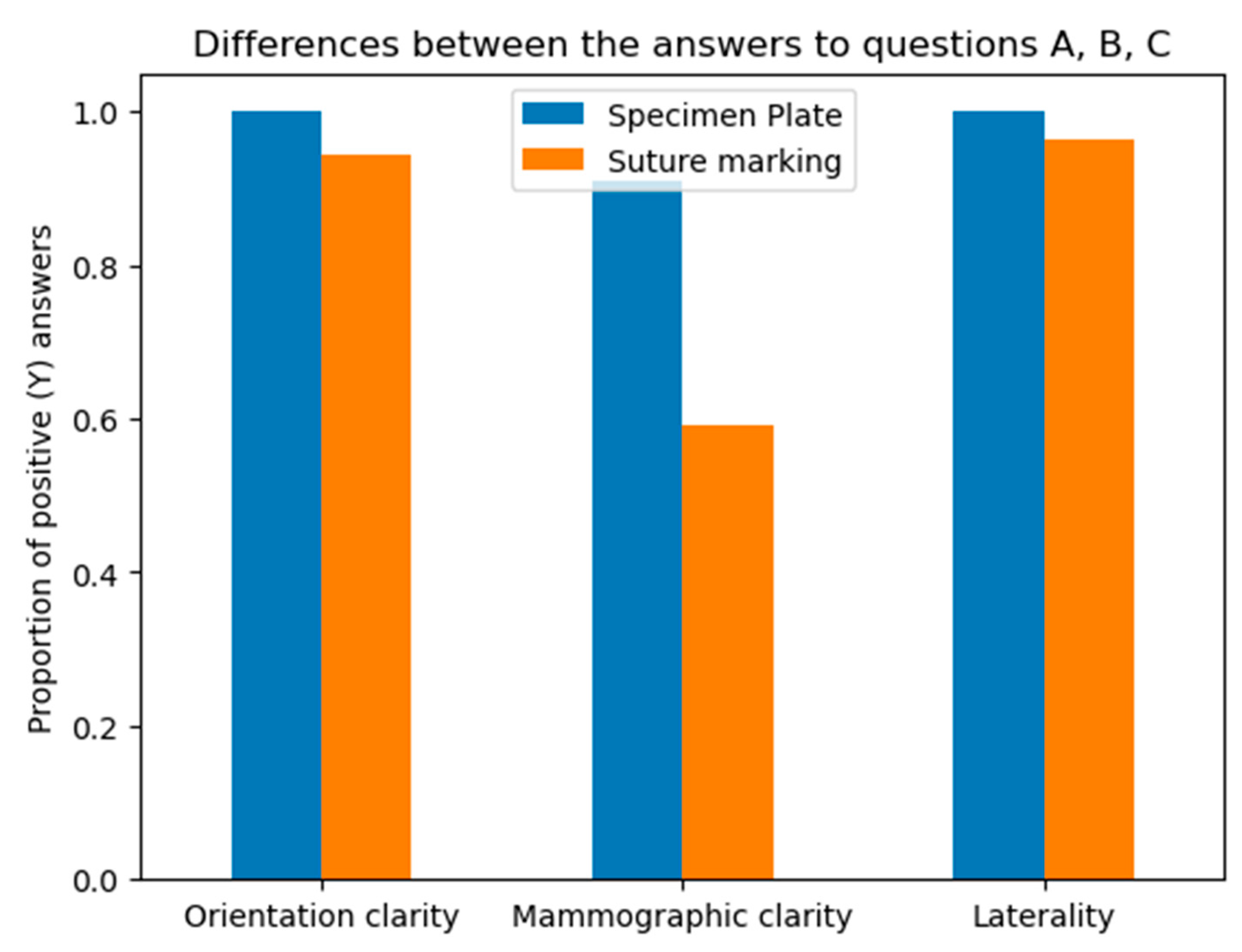
The results of the comparative analysis are summarized as follows:
A: Orientation clarity upon arrival at pathology was comparable between the two groups (p=0.0737).
B: Mammographic clarity of tumor localization was significantly less clear in the Suture Marking Group (p=0.0001).
C: Clarity of specimen laterality (left/right) was not significantly different (p=0.1461).
D: Macroscopic clarity of tumor localization within the specimen showed no significant difference (p=0.5834).
E: Neoadjuvant therapy usage was similar between the groups (p=0.7555).
F: Complete radiologic or pathologic regression rates showed no significant difference (p=0.5252).
G: Potential for 180-degree rotation of the specimen was identical across all cases in both groups.
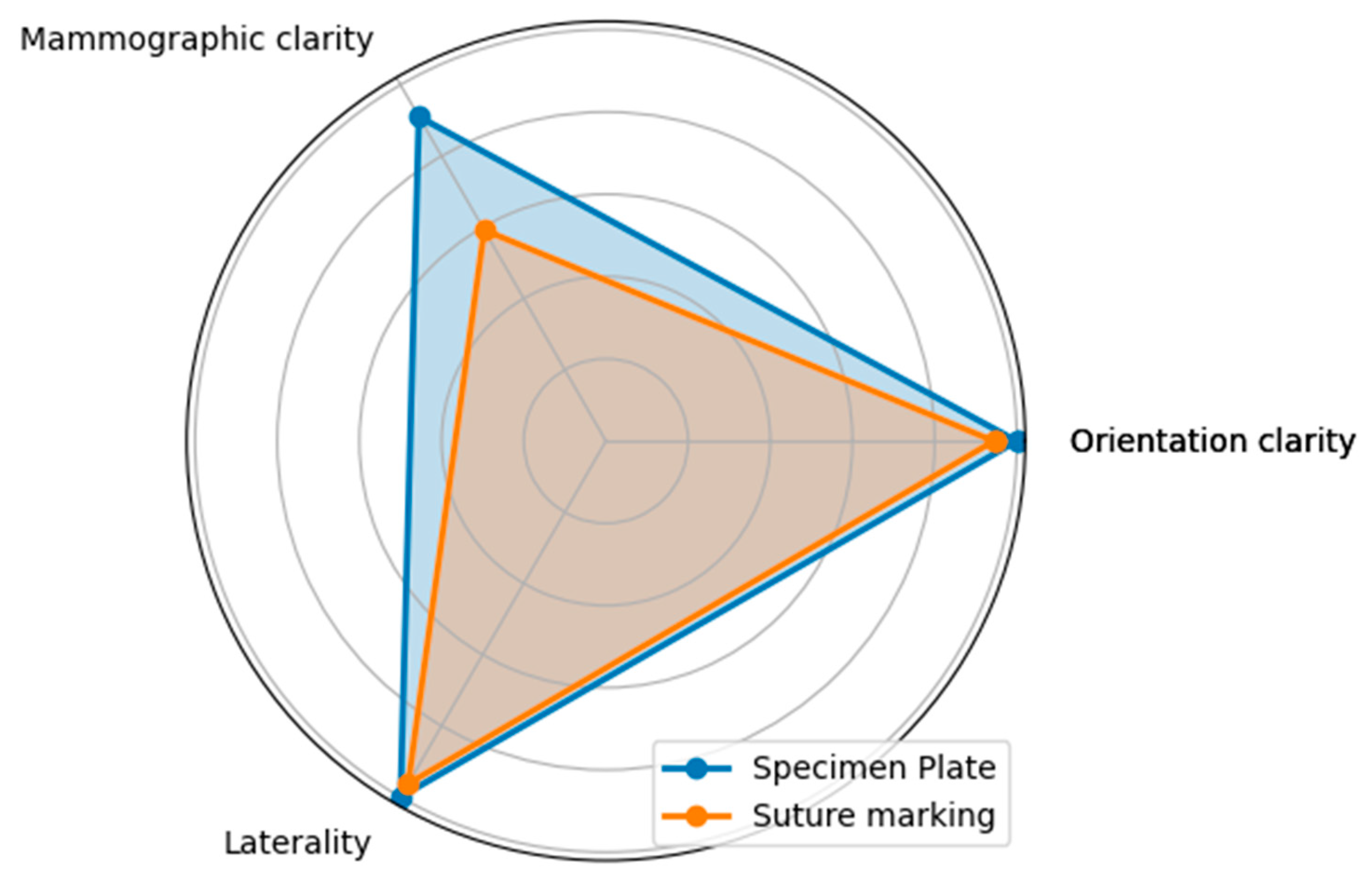
Questions A, B and C focused on the differences between the specimen plate and the traditional method, specifically evaluating whether the orientation of the breast specimen was improved when using the specimen plate. The results showed that the specimen plate provided more accurate orientation compared to the traditional method (
Figure 4 and
Figure 5).
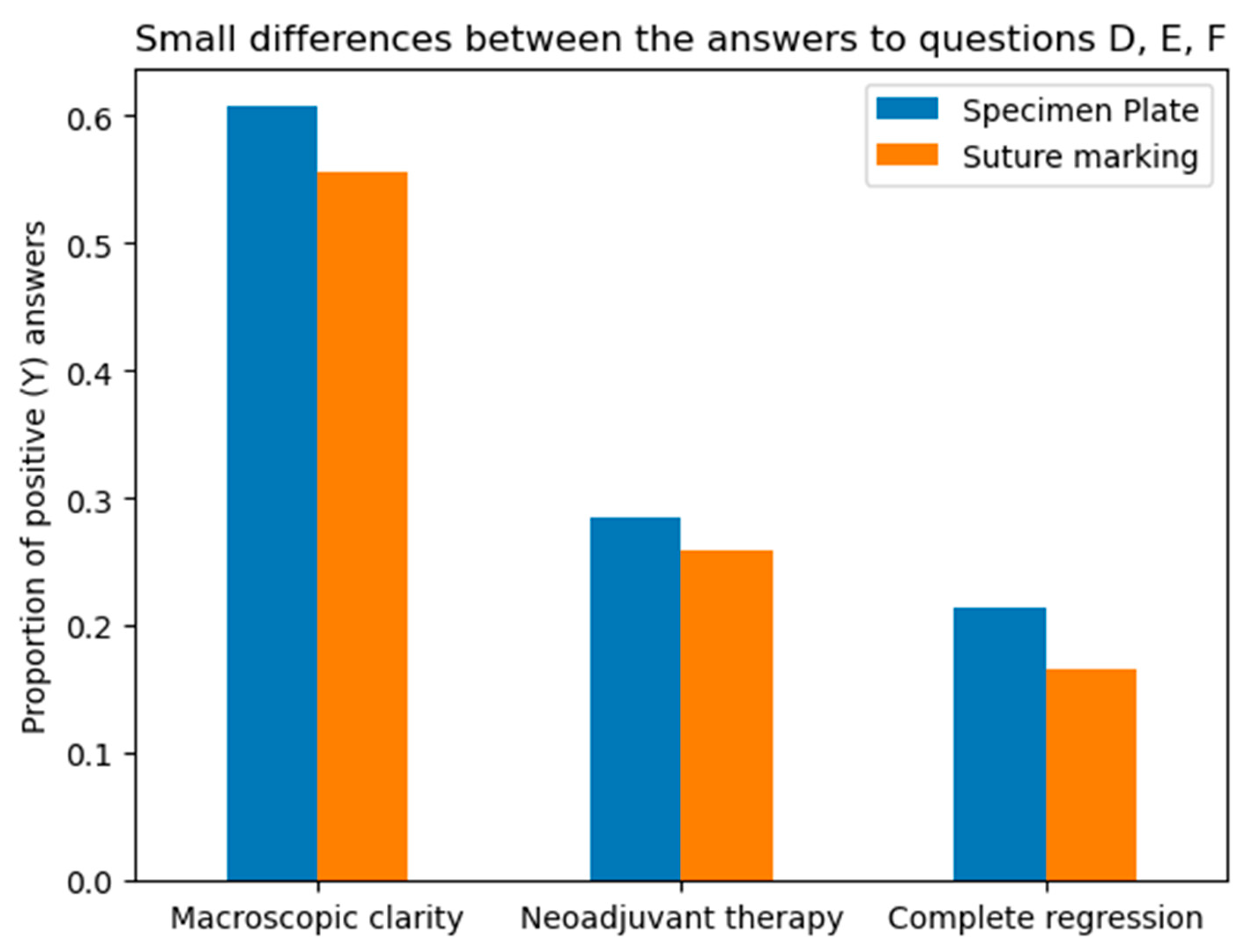
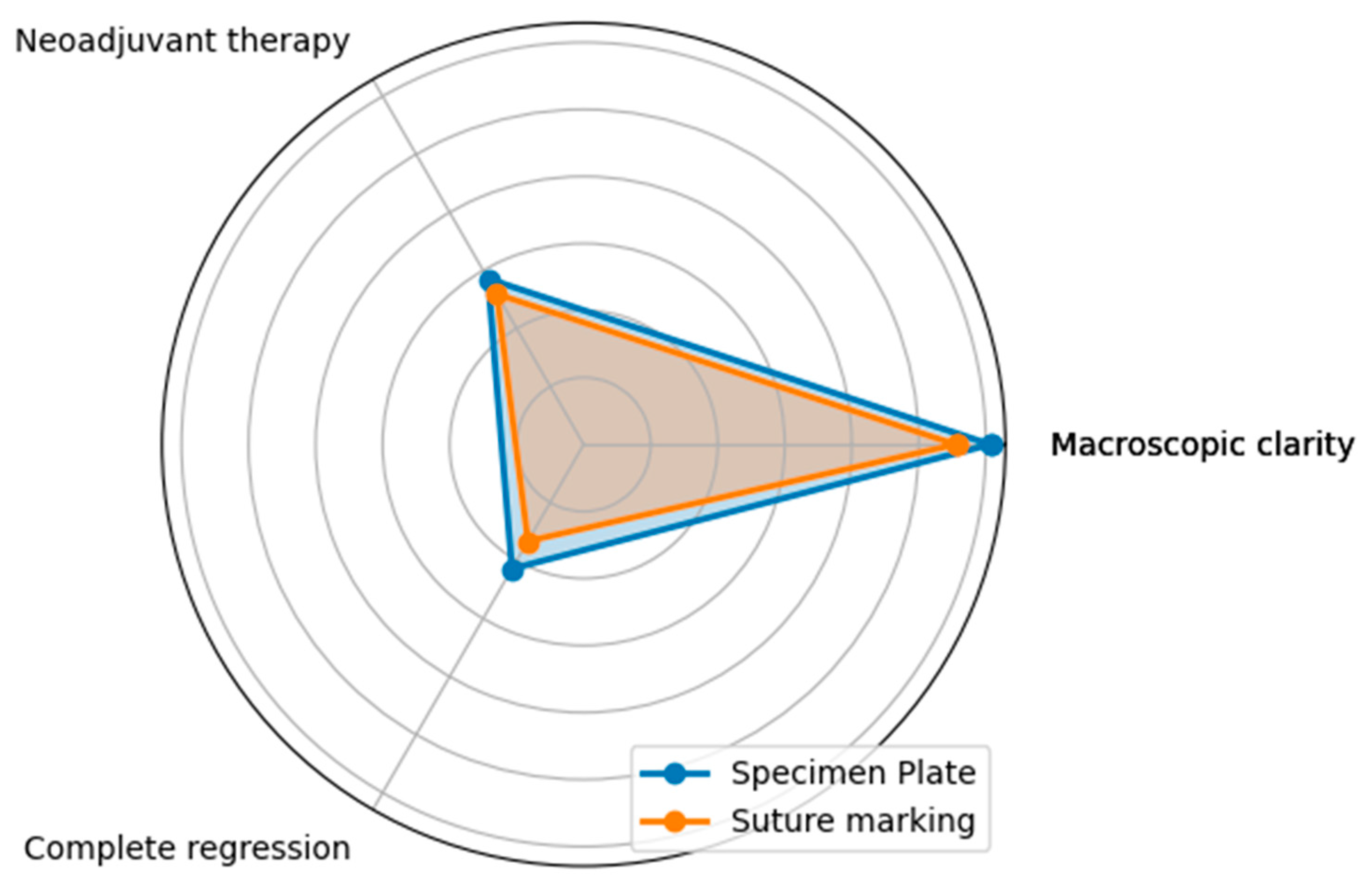
Questions D, E and F assessed whether the two groups in the study were properly randomized and ensured there were no statistical differences between the groups that could bias the results. Statistical analysis confirmed that the groups were comparable, supporting the validity of the study’s findings (
Figure 6 and
Figure 7).
The macroscopic tumor localization results underscore the proper randomization of the two groups, as they demonstrate that non-palpable or poorly palpable tumors became macroscopically identifiable for the pathologist after resection. This outcome reflects the even distribution of tumor characteristics between the groups, ensuring unbiased comparisons. Furthermore, the similar rates of neoadjuvant therapy usage and the resulting tumor regressions in both groups highlight the effectiveness of randomization in achieving comparable cohorts. These findings confirm that the observed outcomes are not influenced by baseline differences, supporting the validity of the study’s conclusions.
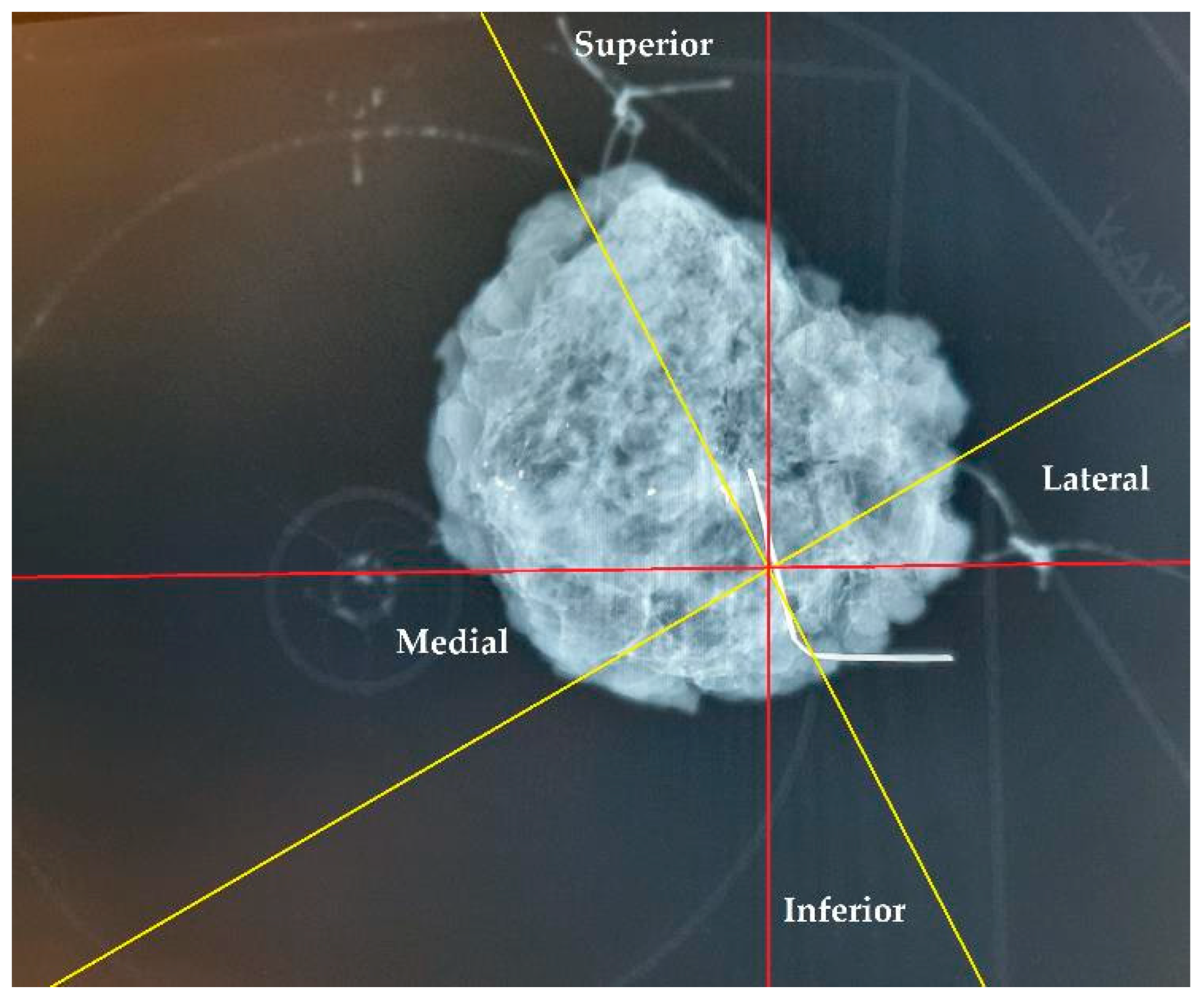
3.2. Orientation Accuracy and Reliability – Comparison of Specimen Plate and Suture Marking Methods
The specimen plate design offers enhanced stabilization of excised breast tissue compared to traditional suture marking. Rather than relying solely on sutures attached to sides of the tissue for orientation, the plate secures the tissue at its basal surface, thereby reducing torsion and mobility and ensuring more accurate preservation of the anatomical localization. In cases where both the specimen plate and suture markings were used (n = 56), 11 cases (19.64%) demonstrated an angular deviation of ≥20° between the two methods. This discrepancy highlights the potential for misleading pathological evaluations and incorrect re-excision directions, especially when relying solely on text descriptions. As demonstrated in
Figure 8, a comparison of suture marking with specimen plate orientation revealed angular deviations of up to 30° (even with accurate suture markings, due to tissue torsion), underscoring the limitations of suture markings alone.
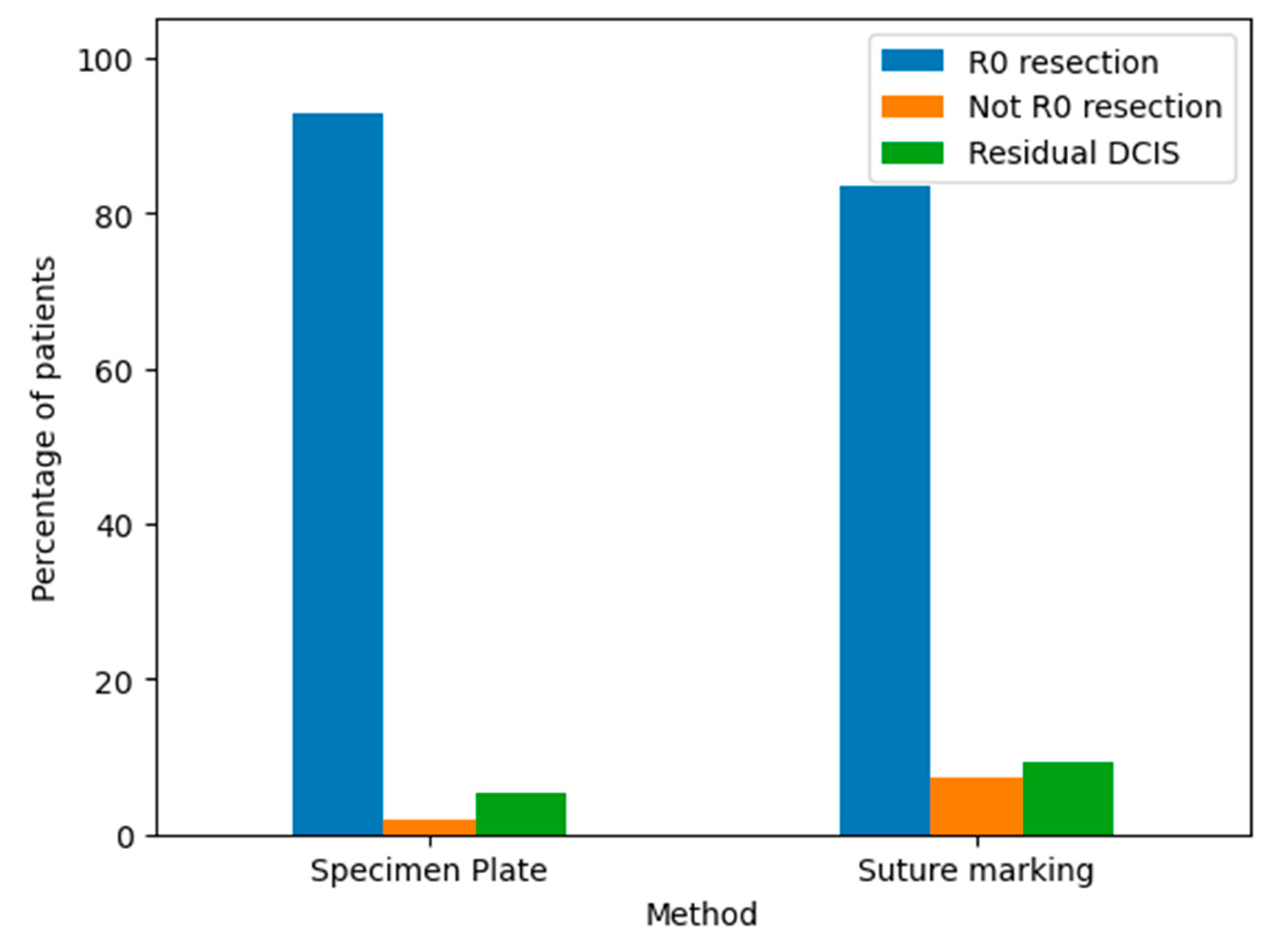
The pathological outcomes of resected breast specimens using the Specimen Plate and Suture Marking methods are illustrated in the corresponding bar chart (
Figure 9).
R0 resection: Indicates a complete tumor removal with negative margins. This was the most common outcome for both methods.
Not R0 resection: Indicates incomplete tumor removal with positive margins. This was infrequent for both techniques.
Residual DCIS: Indicates the presence of residual ductal carcinoma in situ. The frequency of this outcome was comparable between the two groups.
Both the Specimen Plate and Suture Marking methods predominantly achieved R0 resections, with minimal differences in pathological outcomes, underscoring their similar effectiveness in ensuring clear surgical margins. However, a detailed comparison (
Table 1) reveals notable differences in orientation reliability and tumor localization. All specimens in the Specimen Plate Group maintained their intended orientation upon arrival at pathology, with no instances of 180-degree rotation. In contrast, the Suture Marking Group exhibited slightly lower orientation reliability (96.3%). Furthermore, the Specimen Plate Group demonstrated superior performance in macroscopic tumor localization (60.71% vs. 44.44%) and mammographic orientation (80.4% vs. 13%). Detailed results are presented in
Table 2.
4. Discussion
Current studies indicate that re-excision rates after breast-conserving surgery vary significantly, reaching up to 30%, with many re-operations performed even when margins are negative [
4,
5,
6]. Advances in oncoplastic techniques and neoadjuvant treatments have reduced these rates, but challenges remain [
7,
8]. Margin assessment depends on multiple factors, including pathological sectioning techniques, tumor characteristics, and specimen handling. The irregular edges of tumors and compression of specimens during mammography further complicate accurate margin evaluation [
9]. Although consensus guidelines recommend a negative margin of ’no tumor on ink’ to achieve R0 resection, practice variability remains widespread, highlighting the importance of establishing standardized approaches [
10].
Increased detection of non-palpable tumors has underscored the importance of precise preoperative marking and intraoperative radiological evaluation. Techniques like wire-guided and radio-guided localization are widely used, with emerging technologies such as magnetic and radar localization showing promise [
11,
12,
13].
Techniques for localizing non-palpable breast tumors enable precise excision, helping surgeons achieve safe resection margins while preserving maximum volume of healthy tissue [
14]. The specimen plate radically improves orientation reliability, enhancing the efficacy of tumor localization and guiding accurate tumor removal, which in turn reduces re-excision rates and supports both oncologic control and cosmetic results. The specimen plate contributes to fewer re-excisions by providing clearer intraoperative mammograms for the surgeon and more precise radiologic evaluation of the specimen.
In our previous work, the specimen plate concept was introduced to address significant challenges – that were assessed by a nationwide questionnaire for the main breast cancer centers in Hungary - in breast specimen orientation during breast cancer surgery [
4]. That study focused on the design and development of the plate, emphasizing its potential to improve orientation accuracy and reduce misinterpretation in the surgeon-pathologist-radiologist workflow. This prospective randomized study provides compelling evidence demonstrating the superiority of the specimen plate over traditional suture marking methods.
The results from this randomized trial clearly demonstrate that the specimen plate not only enhances intraoperative handling but also provides superior mammographic images for assessing margins. Unlike suture marking, which can sometimes be ambiguous due to torsion or displacement of the specimen, the specimen plate offers consistent and noise-free safe orientation. The coronal plane images generated using the tool in question have proven to be easier for both surgeons and pathologists to interpret, as the breast scheme marked on the plate creates a visible X-ray shadow without obstructing the view, thanks to the plate’s radiolucent material.
Our findings also highlight a reduction in the rate of re-excisions when the specimen plate is used. Literature reports re-excision rates in breast-conserving surgery of 4-30%, largely due to uncertainty about margin status. The superior accuracy of the specimen plate allows for clearer identification of margins, contributing to fewer cases of ambiguous or positive margins. This not only benefits patient outcomes but also reduces the need for repeat surgeries, thus improving overall patient safety and satisfaction.
The randomized study revealed that the additional time required for using the specimen plate was minimal, with only a few minutes added to the procedure, while the benefits in terms of improved orientation accuracy outweighed this minor inconvenience. Furthermore, informal feedback from participating surgeons and pathologists indicated a preference for the specimen plate over traditional suture marking, citing enhanced clarity in specimen orientation.
While this study is a significant step forward, some limitations should be acknowledged. The trial was conducted at a single institution, and while the results are promising, a multicentric study would further validate the findings. To address this, we are currently organizing a multicenter study to assess the applicability and effectiveness of the specimen plate across different institutions and clinical settings.
5. Conclusions
The findings of this study highlight the significant advantages of the Specimen Plate in breast cancer surgery. While its use requires a few additional minutes during specimen preparation, this effort is justified by its benefits. The Specimen Plate improves specimen orientation, enhances mammographic clarity (80.4% vs. 13%), and increases successful R0 resection rates (91.1% vs. 77.8%), ultimately simplifying pathological assessment and improving efficiency. Furthermore, by providing surgeons with more interpretable specimen mammograms, it has the potential to enhance surgical precision and reduce re-excision rates. As surgical techniques and patient care advance, innovations like the Specimen Plate are vital for improving procedural accuracy and patient outcomes.
6. Patents
The process of obtaining design protection for the specimen plate described in this manuscript is currently underway.
Author Contributions
Conceptualization, A.D. and T.F.M.; methodology, A.D., I.Á.H. and T.S.; software, I.Á.H. and R.R..; validation, A.D. and T.F.M.; formal analysis, A.D., I.Á.H. and D.K.; investigation, A.D. and T.S.; investigation, resources A.D.; data curation, A.D., I.Á.H., R.R. and T.F.M.; writing—original draft preparation, A.D.; writing—review and editing, A.D. and D.K.; visualization, I.Á.H., R.R..; supervision, T.F.M.; project administration, AD, TFM; All authors have read and agreed to the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.”
Funding
This research received no external funding.
Institutional Review Board Statement
The study adhered to the principles of the Declaration of Helsinki and received approval from the Regional Science and Research Ethics Committee (protocol number 76-1-19/2021, dated 24 June 2021).
Informed Consent Statement
Consent from patients was not required, as the study involved anonymized data and presented no risk to participants, owing to the simultaneous application of the traditional specimen orientation technique.
Data Availability Statement
Data is contained within the article.
Acknowledgments
We sincerely thank the Pathology and the Radiology Department of the Petz Aladár University Teaching Hospital for their essential support and cooperation.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Specimen Plate Manufacturing
The specimen plate is produced using 3D printing technology (e.g., a Creality Ender 5 printer) with TPU A95 synthetic resin. This material provides the necessary stability for secure specimen fixation via specialized suture anchoring, while its radiotranslucent properties ensure minimal interference with radiographic imaging. The manufacturing process is straightforward and cost-effective, with precise printing parameters—such as a layer thickness of 0.1 mm and a printing temperature of 240 °C—ensuring a high-quality final product.
References
- Burstein, H.J.; Curigliano, G.; Loibl, S.; Dubsky, P.; Gnant, M.; Poortmans, P.; Colleoni, M.; Denkert, C.; Piccart-Gebhart, M.; Regan, M.; et al. Estimating the benefits of therapy for early-stage breast cancer: The St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019. Ann. Oncol. 2019, 30, 1541–1557. [Google Scholar] [CrossRef] [PubMed]
- Volleamere, A.J.; Kirwan, C.C. National survey of breast cancer specimen orientation marking systems. Eur. J. Surg. Oncol. 2013, 39, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Drozgyik, A.; Szabó, T.; Kovács, G.; Kollár, D.; Molnár, T.F. A New Approach to Breast Specimen Orientation: Avoiding Pitfalls with the Specimen Plate Concept. Curr. Oncol. 2024, 31, 4589–4598. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, M.A.; Sinnott, C.; Bawa, S.; Kaufman, D.I.; Guarino, K.; Addona, T. Re-excision rate after partial mastectomy in oncoplastic breast-conserving surgery: A single-institutional experience and review of the literature. Ann. Plast. Surg. 2019, 82, S170–S172. [Google Scholar] [CrossRef] [PubMed]
- McCahill, L.E.; Single, R.M.; Aiello Bowles, E.J.; Feigelson, H.S.; James, T.A.; Barney, T.; Engel, J.M.; Onitilo, A.A. Variability in reexcision following breast conservation surgery. JAMA 2012, 307, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.S.; Kaptanis, S.; Haddow, J.B.; Mondani, G.; Elsberger, B.; Tasoulis, M.K.; Obondo, C.; Johns, N.; Ismail, W.; Syed, A.; et al. Current margin practice and effect on re-excision rates following the publication of the SSO-ASTRO consensus and ABS consensus guidelines: A national prospective study of 2858 women undergoing breast-conserving therapy in the UK and Ireland. Eur. J. Cancer 2017, 84, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.A.; Baron, D.H.; Agrawal, A. Oncologic and cosmetic outcomes of oncoplastic breast-conserving surgery after neoadjuvant systemic therapy: Systematic review and meta-analysis. Breast Cancer Res. Treat. 2024. [Google Scholar] [CrossRef]
- Benjamin, M.A.; Sinnott, C.; Bawa, S.; Kaufman, D.I.; Guarino, K.; Addona, T. Re-excision rate after partial mastectomy in oncoplastic breast-conserving surgery: A single-institutional experience and review of the literature. Ann. Plast. Surg. 2019, 82, S170–S172. [Google Scholar] [CrossRef] [PubMed]
- Fregatti, P.; Gipponi, M.; Atzori, G.; De Rosa, R.; Diaz, R.; Cornacchia, C.; Sparavigna, M.; Garlaschi, A.; Belgioia, L.; Fozza, A.; et al. The margins’ challenge: Risk factors of residual disease after breast-conserving surgery in early-stage breast cancer. In Vivo 2022, 36, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Schulman, A.M.; Mirrielees, J.A.; Leverson, G.; Landercasper, J.; Greenberg, C.; Wilke, L.G. Reexcision surgery for breast cancer: An analysis of the American Society of Breast Surgeons (ASBrS) MasterySM database following the SSO-ASTRO “no ink on tumor” guidelines. Ann. Surg. Oncol. 2017, 24, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Banys-Paluchowski, M.; Kühn, T.; Masannat, Y.; Rubio, I.; de Boniface, J.; Ditsch, N.; Karadeniz Cakmak, G.; Karakatsanis, A.; Dave, R.; Hahn, M.; et al. Localization techniques for non-palpable breast lesions: Current status, knowledge gaps, and rationale for the MELODY study (EUBREAST-4/iBRA-NET, NCT 05559411). Cancers 2023, 15, 1173. [Google Scholar] [CrossRef]
- Zacharioudakis, K.; Down, S.; Bholah, Z.; Lee, S.; Khan, T.; Maxwell, A.J.; Douek, M. Is the future magnetic?—Magseed localization for non-palpable breast cancer: A multicenter nonrandomized control study. Eur. J. Surg. Oncol. 2019, 45, 2016–2021. [Google Scholar] [CrossRef] [PubMed]
- Di Leone, A.; Franceschini, G.; Mason, E.J.; D’Archi, S.; D’Angelo, A.; Scardina, L.; Sanchez, A.M.; Conti, M.; Trombadori, C.; Terribile, D.A.; et al. Image-guided localization techniques for surgical excision of non-palpable breast lesions: An overview of current literature and our experience with preoperative skin tattoo. J. Pers. Med. 2021, 11, 99. [Google Scholar] [CrossRef] [PubMed]
- Cheung, B.H.H.; Co, M.; Lui, T.T.N.; Kwong, A. Evolution of localization methods for non-palpable breast lesions: A literature review from a translational medicine perspective. Transl. Breast Cancer Res. 2024, 5, 12. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Properly oriented breast tissue specimen placed on the specimen plate used during the radio-guided removal of an occult lesion. This form of presentation allows the intuitive evaluation of the mammogram in the coronal plane and optimizes slicing for pathological processing.
Figure 1.
Properly oriented breast tissue specimen placed on the specimen plate used during the radio-guided removal of an occult lesion. This form of presentation allows the intuitive evaluation of the mammogram in the coronal plane and optimizes slicing for pathological processing.
Figure 2.
The mammographic image of the oriented breast tissue specimen with wire-guided tumor localization on the specimen plate. The specimen plate provides high-fidelity localization, accurately reflecting the specimen’s position within the breast. Traditional suture marking (single, long = lateral; double, short = superior) is also applied, using a thick yarn that creates an X-ray shadow.
Figure 2.
The mammographic image of the oriented breast tissue specimen with wire-guided tumor localization on the specimen plate. The specimen plate provides high-fidelity localization, accurately reflecting the specimen’s position within the breast. Traditional suture marking (single, long = lateral; double, short = superior) is also applied, using a thick yarn that creates an X-ray shadow.
Figure 3.
Age distribution of the patients. According to the Kolmogorov-Smirnov test, no significant difference is detected (p=0.5373) between the two distributions.
Figure 3.
Age distribution of the patients. According to the Kolmogorov-Smirnov test, no significant difference is detected (p=0.5373) between the two distributions.
Figure 4.
Differences in responses to questions A (Orientation clarity), B (Mammographic clarity) and C (Clarity of specimen laterality), comparing the specimen plate technique to traditional suture marking.
Figure 4.
Differences in responses to questions A (Orientation clarity), B (Mammographic clarity) and C (Clarity of specimen laterality), comparing the specimen plate technique to traditional suture marking.
Figure 5.
The radar diagram compares the performance of the Specimen Plate and traditional Suture Marking techniques across key parameters related to breast specimen orientation (Questions A - Orientation clarity, B - Mammographic clarity, and C - Clarity of specimen laterality). The shaded areas highlight the differences in performance between the two methods.
Figure 5.
The radar diagram compares the performance of the Specimen Plate and traditional Suture Marking techniques across key parameters related to breast specimen orientation (Questions A - Orientation clarity, B - Mammographic clarity, and C - Clarity of specimen laterality). The shaded areas highlight the differences in performance between the two methods.
Figure 6.
There are small differences between the Specimen Plate and traditional Suture Marking methods in responses to Questions D, E, and F. While small variations exist, none of the differences for these parameters were statistically significant, indicating comparable numbers of the two methods for the evaluated factors.
Figure 6.
There are small differences between the Specimen Plate and traditional Suture Marking methods in responses to Questions D, E, and F. While small variations exist, none of the differences for these parameters were statistically significant, indicating comparable numbers of the two methods for the evaluated factors.
Figure 7.
The radar diagram visualizes the performance of the Specimen Plate and traditional Suture Marking techniques for Questions D, E, and F, highlighting their similarities. The overlapping areas in the radar plot emphasize the minimal differences between the two groups for these parameters, reinforcing their comparable results in these aspects.
Figure 7.
The radar diagram visualizes the performance of the Specimen Plate and traditional Suture Marking techniques for Questions D, E, and F, highlighting their similarities. The overlapping areas in the radar plot emphasize the minimal differences between the two groups for these parameters, reinforcing their comparable results in these aspects.
Figure 8.
Orientation of a breast specimen using both suture marking and the specimen plate. The coronally positioned specimen is secured on the specimen plate, with additional suture markings: a longer thread marking on the lateral side and double shorter threads on the cranial side. A deviation of 30° is observed when comparing suture markings with the specimen plate orientation. The yellow lines represent the potential superior-inferior and lateral-medial axes based on suture markings, while the red lines denote the actual orientations established using the specimen plate.
Figure 8.
Orientation of a breast specimen using both suture marking and the specimen plate. The coronally positioned specimen is secured on the specimen plate, with additional suture markings: a longer thread marking on the lateral side and double shorter threads on the cranial side. A deviation of 30° is observed when comparing suture markings with the specimen plate orientation. The yellow lines represent the potential superior-inferior and lateral-medial axes based on suture markings, while the red lines denote the actual orientations established using the specimen plate.
Figure 9.
Pathological findings of resected breast specimens for the Specimen Plate and Suture Marking methods. The results are categorized as follows:.
Figure 9.
Pathological findings of resected breast specimens for the Specimen Plate and Suture Marking methods. The results are categorized as follows:.
Table 1.
Comparison of Mean and Median Ages Between Groups.
Table 1.
Comparison of Mean and Median Ages Between Groups.
| Group |
Mean Age (years) |
Median Age (years) |
| Specimen Plate Group |
61.1 |
64.0 |
| Suture Marking Group |
60.2 |
62.5 |
Table 2.
Comparison of Specimen Plate Group and Suture Marking Group.
Table 2.
Comparison of Specimen Plate Group and Suture Marking Group.
| Criteria |
Specimen Plate Group (n=56) |
Suture Marking Group (n=54) |
| Clear orientation upon arrival to Pathology |
100% |
96.3% (52 cases) |
| Clear tumor localization (macroscopic) |
60.71% (34 cases) |
44.44% (24 cases) |
| Clear laterality |
100% |
96.3%(52 cases) |
| Possibility of 180-degree rotation |
0 |
0 |
| Clear mammographic orientation |
80.4% (45 cases) |
13% (7 cases) |
| Successful R0 resection |
91.1% (51 cases) |
77.8% (42 cases) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).