Introduction
Heart failure (HF) has reached epidemic proportion, resulting a major contributor to population health and health expenditure [
1]. The growing number of HF patients reflects a better management of CV disease (including decreased CV mortality) together with aging population [
1]. HF prevalence increases with age [
2]. Due to increasing age, the number of HF patients with multiple comorbidities is increasing. In a real-world US study, hospitalized HF patients with ≥3 comorbidities increased from 18% to 29% from 2005 to 2014 [
3].
The number of comorbidities of older and older HF patients determines the complexity of patients’ management and significantly will contribute to a greater number of hospitalizations in the years to come [
4]. The increasing age of HF patients has been accompanied by an increasing number of non-cardiac comorbidities, that have been associated with increased mortality and poorer prognosis in chronic and acute hospitalized HF patients [
5,
6].
Recurrent hospitalization in HF patients represents a change in the trajectory of the disease and its progression and a major contributor to HF costs. Hospitalization also represents an outcome of HF care. In fact, it reflects and is defined by the complex interplay between quality and continuity of care, the underlying cardiac function, and patient cardiac and non-cardiac comorbidities. In general, short-term readmissions are largely attributable to decompensation and congestion [
7]. However, only about fifty percent of long-term readmissions are attributable to hemodynamic factors and associated cardiovascular comorbidities (also impacting on optimal innovative medication titration) [
7,
8]; the remaining fifty percent is attributable to non-cardiac comorbidity and (preventable?) precipitating factors [
7].
In other terms, if it stays true that about half of hospitalizations occur because of HF, it is also true that hospitalizations occur in patients with HF.
The purpose of the present study was to describe the prevalence of comorbidities in HF patients hospitalized in Internal Medicine wards; the prevalence of cardiac and non-cardiac comorbidity and their clustering; the impact of pattern of comorbidities of in-hospital outcomes (length of stay and mortality).
Methods
Study Design and Data Collection
A retrospective observational study based on administrative sources was conducted. We used data from Hospital Discharge Record (SDO) of patients admitted to the Internal Medicine Unit of University Hospital “Duilio Casula” in Cagliari (Italy) between January 1st, 2017 and December 31st, 2022.
SDO allows maximum six diagnoses. Primary and secondary diagnoses were identified according to the “International Statistical Classification of Diseases and Related Health Problems” Ninth Edition (ICD9 ) code.
Heart failure (HF) was identified by the following ICD9 codes: 428, 402.01, 402.11, 402.91, 404.11, 404.13, 404.91, 404.93. It was further classified whether it was the primary diagnosis (HFp) (people hospitalized because of acute episode of HF decompensation) or a secondary diagnosis (HFs) (people hospitalized with HF) diagnosis.
The study complies with the Declaration of Helsinki and the research protocol was approved by the locally appointed Ethics Committee (PROT.. NP/2023/949).
Comorbidities
The ICD9 codes were also used to assess cardiac and non-cardiac comorbidities. For the purposes of the present analyses. The following cardiac and non-cardiac comorbidities were retained because of their higher prevalence ( ≥ 4%).
Four cardiac (atrial fibrillation, hypertension, diabetes mellitus, coronary artery disease - CHD) and five non-cardiac (respiratory failure and pneumonia, kidney disease, anaemia, sepsis, dementia) comorbidities were retained.
In-Hospital Outcomes: Length of Stay and Mortality
Length of stay (days) was calculated from SDO. Additionally, we identified patients deceased during the hospitalization.
Statistical Analysis
Data were analysed with Statistical Package for the Social Sciences SPSS® 20.0 (IBM Corp., Armonk, NY).
Categorical variables were presented as frequencies and percentages, while continuous variables as means with standard deviations.
Differences in mean values between groups were compared by Wilcoxon rank-sum test or Mann-Whitney U test non-parametric Wilcoxon test.
We assessed the association between Comorbidities and duration of hospitalization (length of stay) via a multivariable regression analysis model
Multivariate logistic regression was used to assess the association between comorbidities and tin-hospital mortality. Zero non-cardiac comorbidities also served as the reference group for these analyses.
All statistical tests were two-sided. P-values<0.05 were considered significant.
Results
Cohort Characteristics
Over the six-year observation time, a total of 12435 hospitalizations (6146 female, 6289 male) occurred in the Internal Medicine Unit. Of those, 1481 (or 11.9%) patients presented a diagnosis of HF. More specifically, 610 patients (41.2% of those with HF) had HF as the primary diagnosis (HFp) (people hospitalized because of HF) and 871 (58.8%) had HF among the secondary diagnoses (HFs) (people hospitalized with HF).
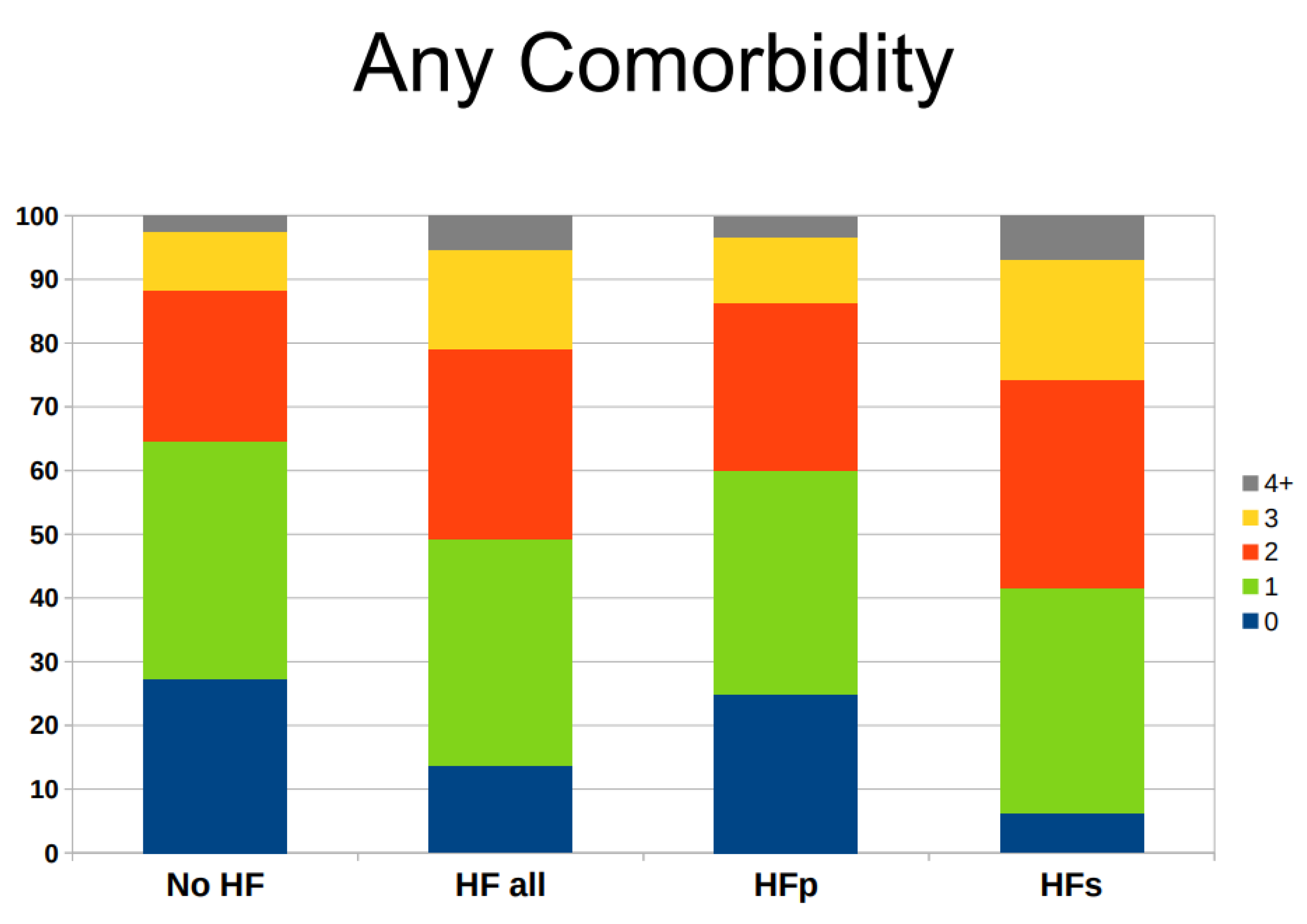
Patients with zero comorbidities comprised 27.2% of hospitalized patients without HF, followed by 37.5% with one comorbidity, 23.7% with two comorbidities, 9.0% with three comorbidities, and 2.6% with four or more comorbidities . The corresponding picture for patients with HF was 13.7% with zero comorbidities, followed by 35.5% with one comorbidity, 30.0% with two comorbidities, 15.4% with three comorbidities, and 5.4% with four or more comorbidities (
Figure 1).
A greater prevalence of multiple comorbidities was observable in patients with HFs as compared to those with HFp : for example, 25.8% of HFs patients had three or more comorbidity as compared to 13.7% of HFp patients (
Figure 1).
Occurrence of Cardiac and Non-Cardiac Comorbidity
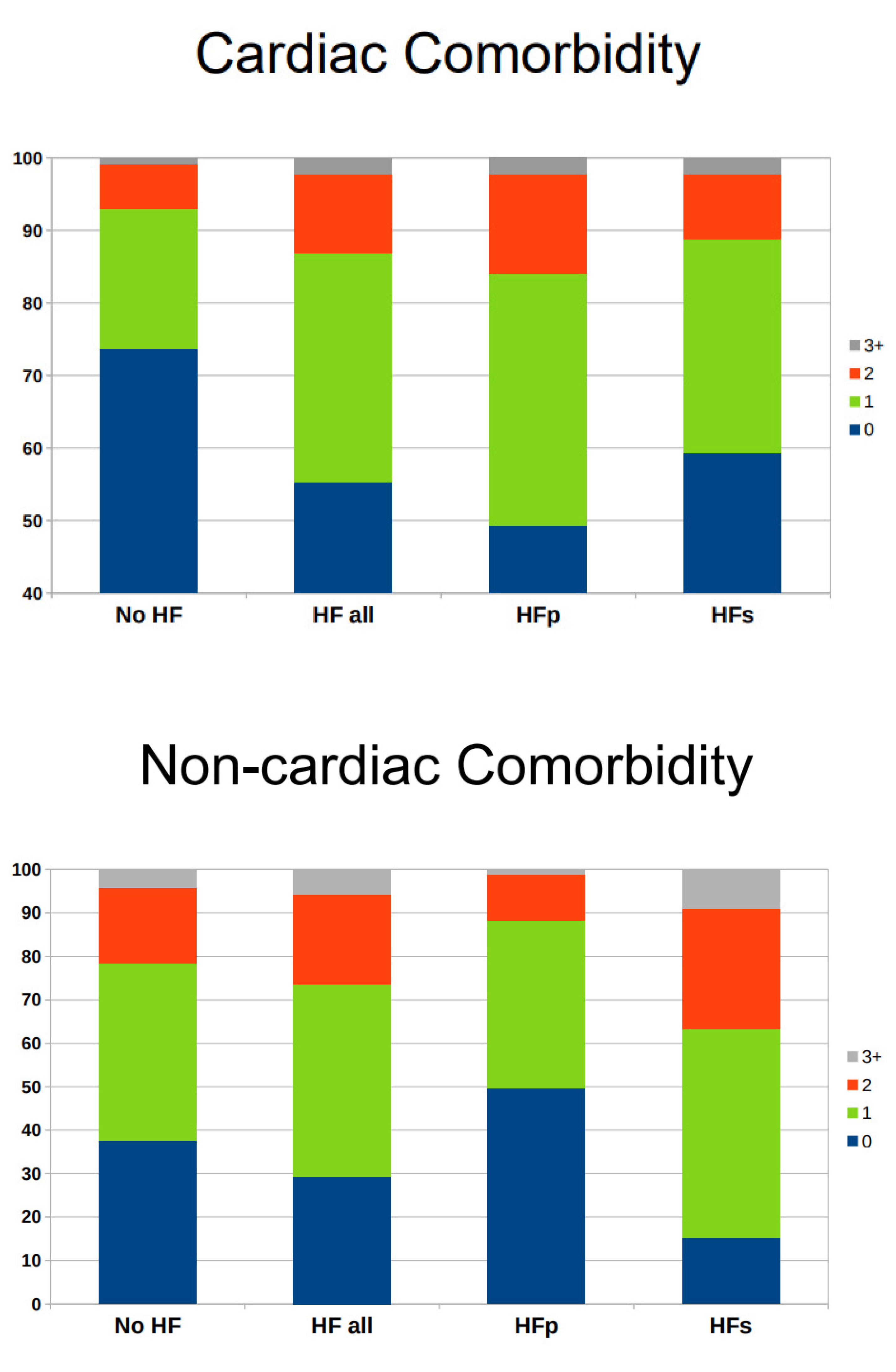
HF hospitalized patients with zero cardiac comorbidities were 55.2%, followed by 31.7% with one cardiac comorbidity, 10.9% with two cardiac comorbidities, and 2.2% with three or more cardiac comorbidities (
Figure 2).
The corresponding picture for non-cardiac comorbidity was 23.4% with zero non-cardiac comorbidities, followed by 44.1% with one non-cardiac comorbidity, 20.6% with two non-cardiac comorbidities, and 5.9% with three or more non-cardiac comorbidities (
Figure 2).
Patients with HFp had more cardiac comorbidities than those with HFs, who had at least one non-cardiac comorbidity in 84.7% of cases as compared to 50.3% in HFp.
Atrial fibrillation was the most prevalent cardiac comorbidity (25.6%) in HF patients, followed by hypertension (17.0%), diabetes mellitus (9.9%), and prevalent coronary heart disease (7.9%) (
Table 1). Respiratory failure and pneumonia represented the most prevalent non-cardiac comorbidity within HF population (38.9%), followed by kidney disease (27.9%), anemia (15.5%), sepsis (8.7%), and dementia (4.7%) (
Table 1).
Atrial fibrillation was more common in HFp (31.0% versus 21.7%), while respiratory failure or pneumonia (55.0% versus 15.9%) and sepsis (14.0% versus 1.2%) were more common in Hfs.
Association Between the Burden of Cardiac and Non-Cardiac Comorbidities on Length of Stay
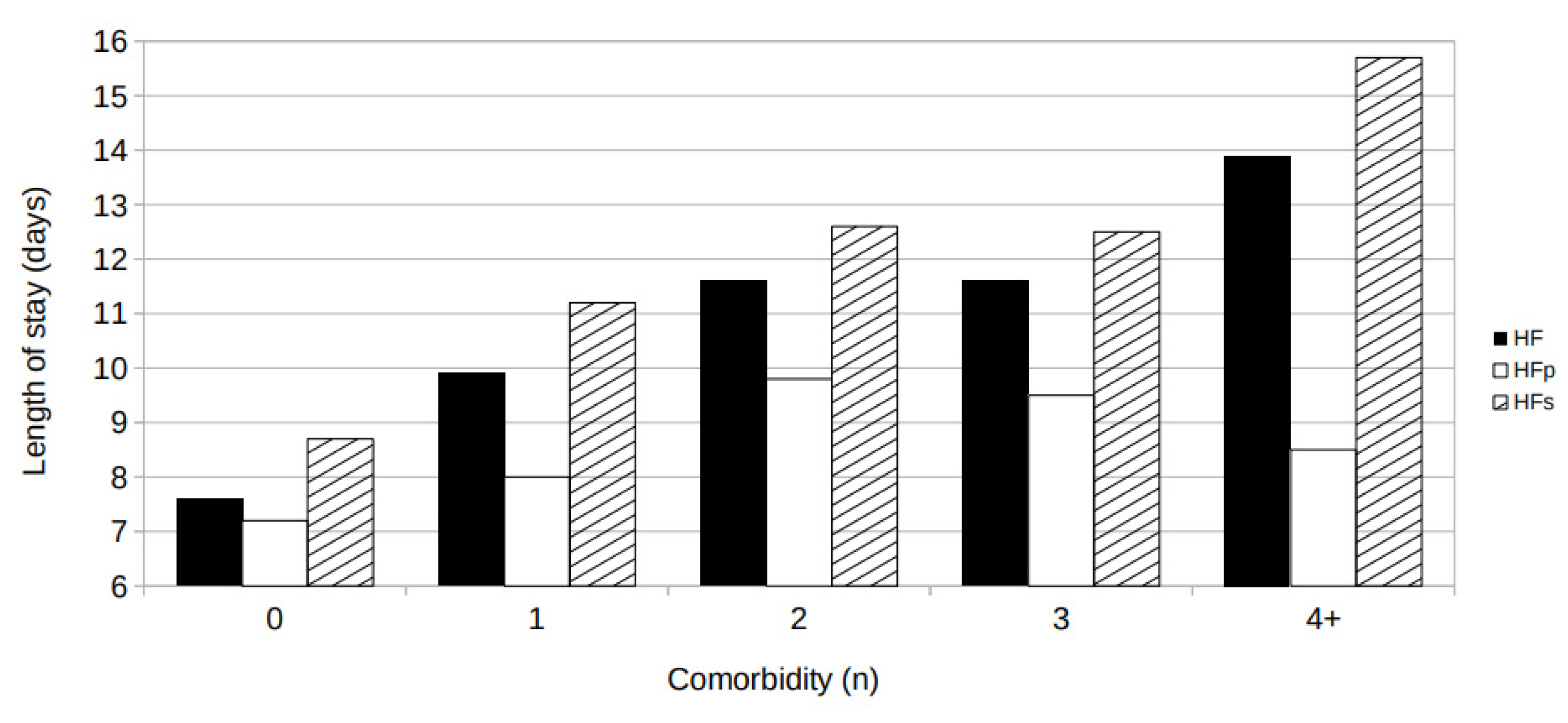
The number of comorbidities was associated with the length of stay in hospital. As illustrated in
Figure 3, average length of stay progressively increased in association with the number of comorbidities from 7.6 ± 0.5 days in subjects with no comorbidity to 13.9 ± 1.5 days in subjects with 4+ comorbidities (p< 0.0001).
Interestingly, the length of stay was greater in patients hospitalized with HF (HFs) than in patients hospitalized because of HF (HFp) at any level of comorbidity.
Multiple regression analyses, controlling for age and sex, confirmed this observation (number of comorbidities: beta coefficient 1.41 ± 0.22, p< 0.0001). It is noteworthy that, after controlling for age and sex, only non-cardiac comorbidities remained significantly associated with an increased duration of hospitalization (number of non-cardiac comorbidity: beta coefficient 2.86 ± 0.27, p< 0.0001) .
Association Between the Burden of Cardiac and Non-Cardiac Comorbidities on In-Hospital Mortality
No significant linear relationship between in-hospital mortality and length of stay was observed. Rather, the association between in-hospital mortality and length of stay showed a tendency toward a J-shaped relationship (Supplemental
Figure S1).
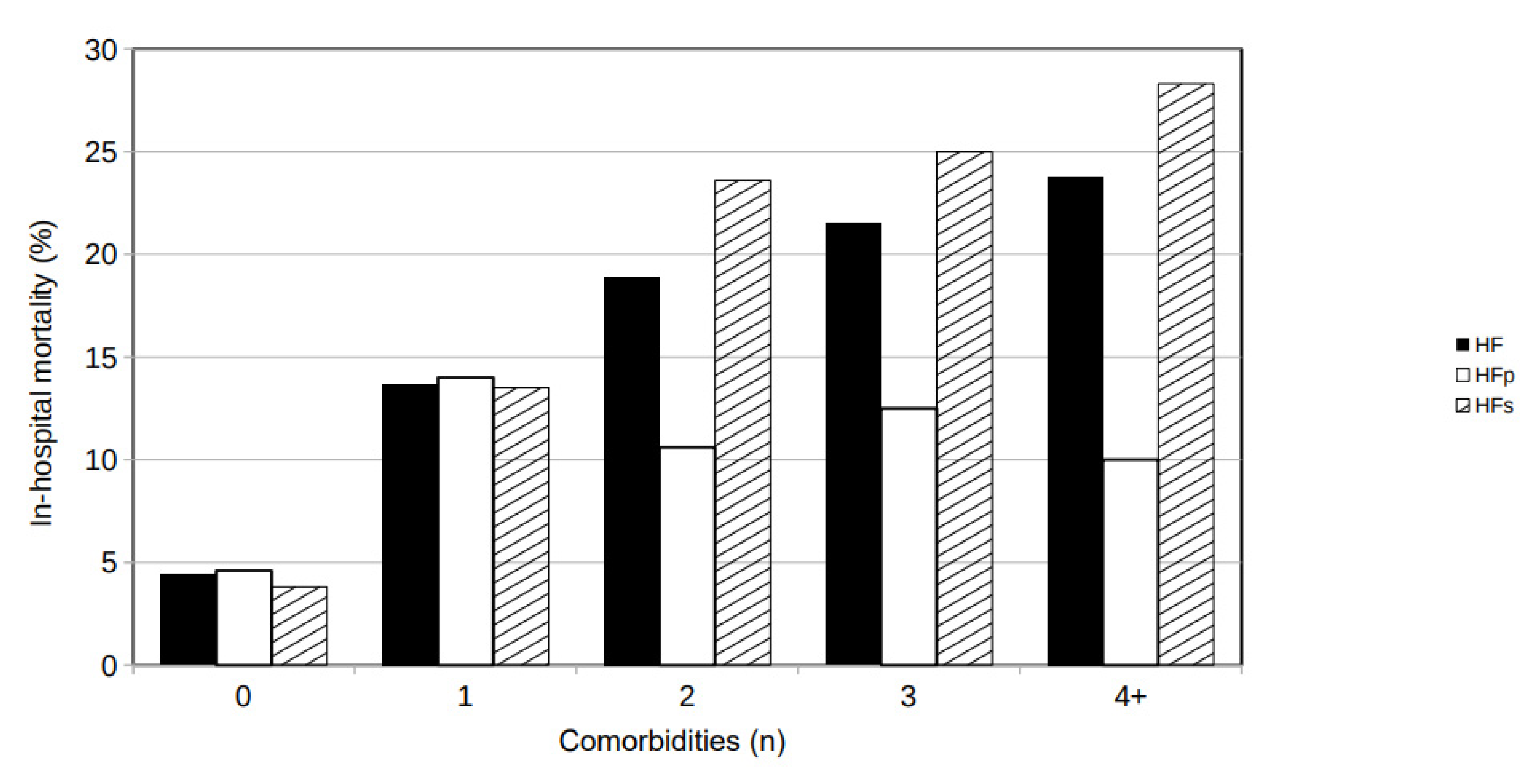
In-hospital mortality was associated with the number of comorbidities: it was 4.4% in HF patients with zero comorbidities, increased to 13.7% in HF patients with one comorbidity, 18.9% with two comorbidities, 21.5% with three comorbidities, and 23.8% with four or more comorbidities (
Figure 4). In-hospital mortality was similar in patients hospitalized with HF (HFs) than in patients hospitalized because of HF (HFp) if they presented zero or one comorbidity but was dramatically greater in HFs than in HFp patients with two or more comorbidities (
Figure 4).
Multivariable logistic regression analyses, controlling for age, sex, and length of stay, revealed that the number of comorbidities is associated with significantly greater odds of in-hospital mortality (adjusted OR 1.42, 95% CI 1.25–1.62; p <0.0001). The impact of comorbidity on in-hospital mortality appeared attributable to non-cardiac (adjusted OR 1.90, 95% CI 1.60–2.23; p <0.0001) but not to cardiac comorbidity in HF patients (adjusted OR 0.97, 95% CI 0.80–1.18; p= 0.76) .
Table 2 illustrates the growing burden on mortality with increasing number of overall and non-cardiac comorbidities. Of note, having two comorbidities was associated with six-fold higher odds of in-hospital mortality; the odds did not further increase with a greater number of comorbidities. When focusing on the specific contribution of cardiac and non-cardiac comorbidities in HF patients, no significant increase in the odds for in-hospital mortality were observed with growing number of cardiac comorbidities. Conversely, a sort of dose-response effect on mortality was observable with increasing number of non-cardiac comorbidities.
Discussion
The main findings of the present study were as follows: (i) HF represents a common condition (12%) in patients hospitalized in Internal Medicine wards; (ii) only 44% of HF patients are hospitalized because of acute decompensation; (iii) in HF patients, the prevalence of 0, 1, 2, 3, ≥4 comorbidities was 13.7%, 35.5%, 30.0%, 15.4%, 5.4%, respectively; (iv) the presence of ≥2 non-cardiac comorbidities was twice the presence of cardiac comorbidities;; (v) non-cardiac comorbidities were associated with longer duration of hospitalization and with higher rates of in-hospital mortality, independently of duration of hospitalization.
HF prevalence is increasing, both in general population and among hospitalized patients, as a facet of improved survival to acute coronary syndrome and better treatments contributing to the general greater life-expectancy [
1,
9]. Accordingly, older subjects present a greater prevalence of HF (7%−11%) than younger population (1-2). Therefore, although most studies describe HF patients admitted to and followed by Cardiology units, in the real-world a considerable proportion of HF patients are admitted to and followed-up by Internal Medicine and Geriatrics units [
10].
The impact of comorbidities on HF patients is such that ESC 2021 Guidelines encompassed a large section on both cardiac and non-cardiac comorbidities, highlighting their prevalence and their impact on specific dilemmas in treatment [
11]. In these regards, our observation of a greater burden of comorbidities on in-hospital outcomes was expected and has already been reported [
6,
11].
However, in the real world, a growing older population of HF patients faces multimorbidity, the simultaneous occurrence of several comorbidities reported in ESC Guidelines. We observed that multiple comorbidities are far more common in HF than in non-HF patients (twice concerning the presence of ≥3 comorbidities). Additionally, the presence of ≥2 non -cardiac comorbidities is two-fold more common than the presence ≥2 cardiac comorbidities in older HF patients.
Non-cardiac comorbidities have been associated with a greater risk of hospitalization in chronic HF patients with reduced ejection fraction (18-19) as well as with increased mortality [
12,
13]. Our study adds to these observations that non-cardiac – but not cardiac - comorbidities were associated with 2-fold greater odds of in-hospital mortality and longer hospitalization.
All together, these findings underline once more that about half of hospitalizations occur in patients with HF rather than because of HF, i.e. because of acute HF decompensation. Additionally, the length of stay was greater in patients hospitalized with HF (HFs) than in patients hospitalized because of an acute hemodynamic decompensation, at any level of comorbidity.
This phenomenon may reflect a growing tendency towards optimal management of cardiac conditions leading to an adequate control of cardiac comorbidities. It should be better characterized if and how the simultaneous occurrence of nan-cardiac comorbidities impacts on optimal innovative medication titration) (7-8) as well as whether the lack of appropriate guideline-directed medical therapy (GDMT) titration occurs because of ageism prejudice or rather because of a greater occurrence of side effects impacting on quality of life of older HF patients (particularly hypotension, and medication-medication or medication-disease interactions) [
14].
Limitations and Strengths
The present study has a major strength: it reports data from hospitalized HF patients in Internal Medicine Unit. This a growing proportion of HF patients, often older and more complex as compared to HF patients admitted to Cardiology Units [
15] commonly included in current registries.
The present study also presents several limitations that should be acknowledged. First, it is a retrospective study including patients admitted to internal medicine units, which introduces a selection bias. Second, cardiac and non-cardiac comorbidities had been defined on data readily obtained from Hospital Discharge Records, which reflects conditions more relevant for each hospitalization and may not adequately reflect common and prevalent conditions. In fact, the reported occurrence of atrial fibrillation or hypertension is much lower than commonly reported in HF patients from registries and/or clinical trials. Third, the use of so called “administrative data” does not allow access to clinical profiles of included patients (ejection fraction category, treatment and its adherence to Guidelines, severity of comorbidities).
Conclusions
The present study recalls the attention on the role of non-cardiac comorbidities in predicting in-hospital outcome in HF patients admitted to an internal medicine unit – where HF is present in 11% of hospitalized patients.
Since the hospital admission of these very old HF patients with several non-cardiac comorbidities will continue to increase, it is imperative that we optimize the management of non-CV conditions to improve outcomes and reduce early in-hospital mortality – accomplishing the recommendation of ESC Guidelines “In addition to optimizing medical and device therapies for HF, attention should also be given to how HF care is delivered”, i.e. implementing the models of care and disseminating a multidisciplinary management of older HF patients.
Improved management of HF patients in the pre-discharge and early post-discharge phase after hospitalization will be critical to reduce the burden of re-hospitalization and increase the time spent at home [
16].
Future studies are encouraged to adopt a multidisciplinary approach to the growing older HF patients, which will simplify the identification of more risky phenotypes [
17] and the early identification of preventable factors precipitating hospitalization.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, AScuteri; Methodology, VM, EB, AS, AScuteri; Formal Analysis, EB, AScuteri; Data Curation, AC; Writing – Original Draft Preparation, VM, Ascuteri; Writing – Review & Editing, VM, EB, AS, AC.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of University Hospital of Cagliari (Azienda Ospedaliera Universitaria Cagliari) (PROT.. NP/2023/949 on March 1st, 2023).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study and the large number of subjects involved makes not feasible to contact them all to get consent. Additionally, mostly data had been anonymized prior to data analysis.
Data Availability Statement
The datasets presented in this article are not readily available because their include patient sensitive data.
Conflicts of Interest
No Author has any conflict of interest to disclose.
References
- Conrad, N.; Judge, A.; Tran, J.; Mohseni, H.; Hedgecott, D.; Crespillo, A.P.; et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 2018, 391, 572–580. [Google Scholar] [CrossRef]
- Bui, A.L.; Horwich, T.B.; Fonarow, G.C. Epidemiology and risk profile of heart failure. Nat Rev Cardiol 2011, 8, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Zhao, X.; Hammill, B.G.; Hernandez, A.F.; Fonarow, G.C.; Felker, G.M.; et al. Trends in non cardiovascular comorbidities among patients hospitalized for heart failure: insights from the Get With The Guidelines-Heart Failure Registry. Circ Heart Fail 2018, 11, e004646. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; Settergren, C.; Schrage, B.; Thorvaldsen, T.; Löfman, I.; Sartipy, U.; et al. Comorbidities and cause-specific outcomes in heart failure across the ejection fraction spectrum: a blueprint for clinical trial design. Int J Cardiol 2020, 313, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Chioncel, O.; Benson, L.; Crespo-Leiro, M.G.; Anker, S.D.; Coats, A.J.S.; Filippatos, G.; et al. Comprehensive characterization of non-cardiac comorbidities in acute heart failure: an analysis of ESC-HFA EURObservational Research Programme Heart Failure Long-Term Registry. Eur J Prev Cardiol. 2023, 30, 1346–1358. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, A.S.; Ambrosy, A.P.; Dunning, A.; DeVore, A.D.; Butler, J.; Reed, S.; et al. The burden of non-cardiac comorbidities association with clinical outcomes in an acute heart failure trial—insights from, A. S.C.E.N.D.-H.F. Eur J Heart Fail 2020, 22, 1022–1031. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.S.; Stevenson, L.W. Rehospitalization for heart failure: predict or prevent? Circulation. 2012, 126, 501–6. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; Vaduganathan, M.; Fonarow, G.C.; Bonow, R.O. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol 2013, 61, 391–403. [Google Scholar] [CrossRef] [PubMed]
- Dharmarajan, K.; Rich, M.W. Epidemiology, pathophysiology, and prognosis of heart failure in older adults. Heart Fail Clin 2017, 13, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Maggioni, A.P.; Orso, F.; Calabria, S.; Rossi, E.; Cinconze, E.; Baldasseroni, S.; et al. The real-world evidence of heart failure: findings from 41,413 patients of the ARNO database. Eur J Heart Fail 2016, 18, 402–410. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Smith, D.H.; Thorp, M.L.; Gurwitz, J.H.; McManus, D.D.; Goldberg, R.J.; Allen, L.A.; et al. Chronic kidney disease and outcomes in heart failure with preserved versus reduced ejection fraction: the Cardiovascular Research Network PRESERVE study. Circ Cardiovasc Qual Outcomes 2013, 6, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Streng, K.W.; Nauta, J.F.; Hillege, H.L.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; et al. Non-cardiac comorbidities in heart failure with reduced, mid-range and preserved ejection fraction. Int J Cardiol 2018, 271, 132–139. [Google Scholar] [CrossRef] [PubMed]
- McAlister, F.A.; Savu, A.; Ezekowitz, J.A.; Armstrong, P.W.; Kaul, P. The hospital frailty risk score in patients with heart failure is strongly associated with outcomes but less so with pharmacotherapy. Brunner-La Rocca HP, Linssen GC, Smeele FJ, van Drimmelen AA, Schaafsma HJ, Westendorp PH et al. Contemporary drug treatment of chronic heart failure with reduced ejection fraction. The CHECK-HF Registry. JACC: Heart Fail 2019, 7, 13–21. [Google Scholar] [CrossRef]
- Orso, F.; Pratesi, A.; Herbst, A.; Baroncini, A.C.; Bacci, F.; Ciuti, G. , et al. . Acute heart failure in the elderly: setting related differences in clinical features and management. J Geriatr Cardiol. 2021, 18, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Metra, M.; Adamo, M.; Tomasoni, D.; Mebazaa, A.; Bayes-Genis, A.; Abdelhamid, M.; et al. Pre-discharge early post-discharge management of patients hospitalized for acute heart failure: A scientific statement by the Heart Failure Association of the, E. S.C. Eur J Heart Fail. 2023, 25, 1115–1131. [Google Scholar] [CrossRef]
- Musella, F.; Rosano, G.M.C.; Hage, C.; Benson, L.; Guidetti, F.; Moura, B.; et al. Patient profiles in heart failure with reduced ejection fraction: Prevalence, characteristics, treatments and outcomes in a real-world heart failure population. Eur J Heart Fail. 2023, 25, 1246–1253. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).