Submitted:
26 December 2024
Posted:
10 January 2025
You are already at the latest version
Abstract
Background: Culture-based caring in nursing is a crucial strategy for enhancing nurses’ performance by integrating cultural values into nursing practices. Objective: This literature aims to create more inclusive, meaningful, and culturally responsive healthcare services for both patients and nurses. Methods: Articles were obtained from several databases includes Scopus, Science Direct, ProQuest, PubMed, and CINAHL to identify articles published between 2019 - 2024. The review evaluated various literature on the development of culture-based caring models, focusing on cultural competence dimensions such as awareness, knowledge, skills, encounters, and desire. Result: The findings indicate that the success of this model heavily depends on continuous education, supportive and inclusive work environments, as well as nurses’ ability to adapt and communicate across cultures. This holistic approach does not only improve patients’ satisfaction but also strengthens interprofessional relationships, reduces miscommunication, and enhances overall healthcare service quality.

Keywords:
Introduction
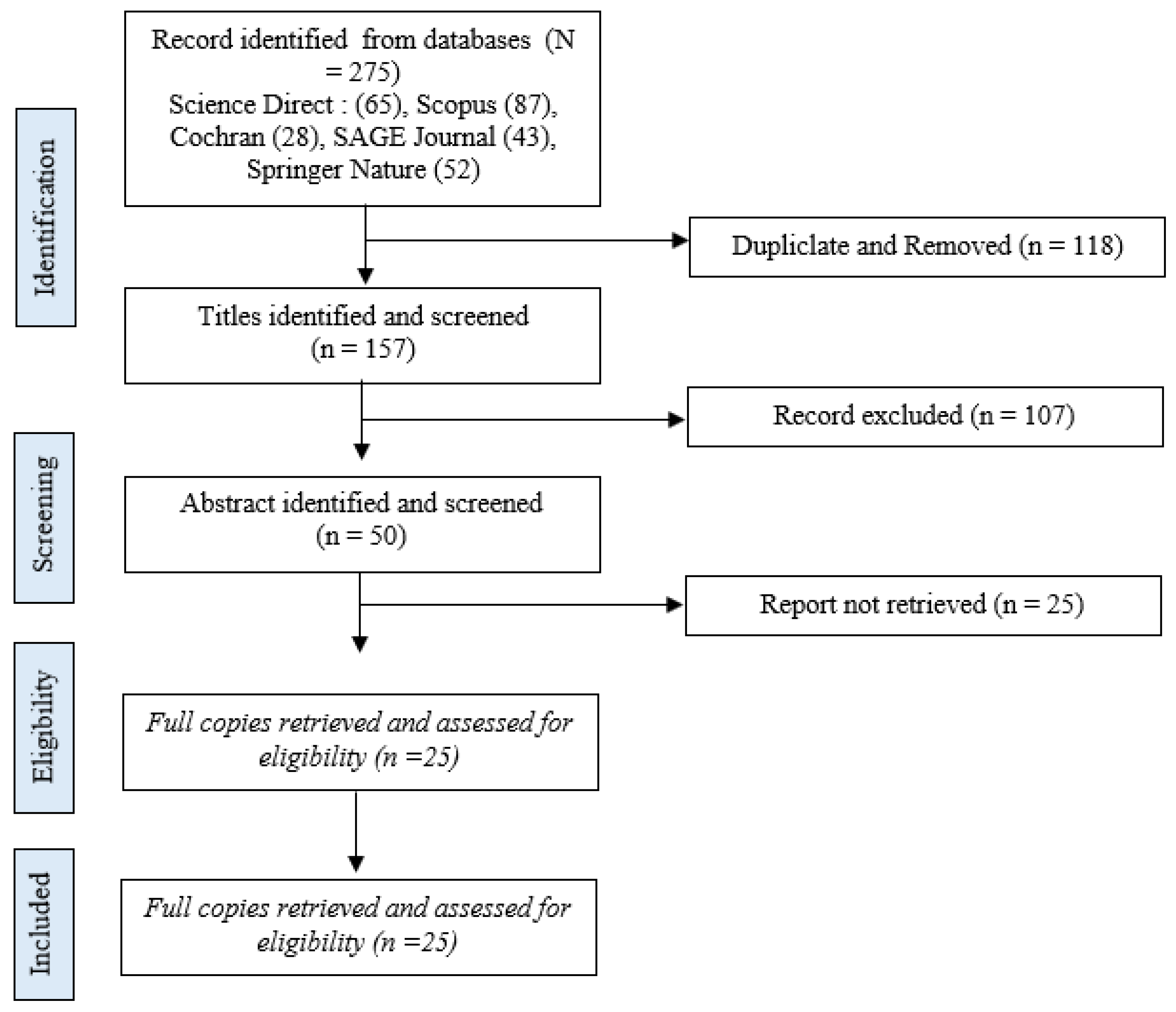
Method
Search Strategy
Inclusion Criteria
- Studies focusing on the development or implementation of culture-based caring models.
- Studies evaluating the impact of care models on nurse performance or job satisfaction.
- Quantitative, qualitative, or mixed-method studies.
- Articles published in peer-reviewed journals.
Exclusion Criteria
- Studies not available in full text.
- Articles not peer-reviewed, such as editorials, commentaries, and opinion pieces.
Data Extraction and Management
- Study Details: Author(s), year, and location of the study.
- Research Objectives and Design: Purpose and type of study design.
- Population and Sample Size: Description of the study population and sample size.
- Description of the Culture-Based Caring Model: Key features and implementation of the model.
- Outcomes Measured: Nurse performance and job satisfaction.
- Key Findings and Conclusions: Main results and implications of the study.
- The extracted data were organized into a spreadsheet for analysis.
Results
| No | Article Title | Author | Result |
| 1 | Exploring the integration of culturally and linguisticallydiverse nurses and nursing students in healthcare: A cross-sectional study | (Martikainen et al., 2024b) | Nurses and nursing students from diverse cultural and linguistic backgrounds often face challenges in adapting to their work environments. Some of the influencing factors include: 1) Unsupportive Work Environment, many respondents reported feeling insufficiently supported by colleagues and management, negatively impacting their motivation and performance, 2) Language Barriers, these barriers affect not only communication with patients but also interactions with colleagues and 3) Low Job Satisfaction, despite many respondents having strong communication skills, their job satisfaction tends to be low, especially in non-inclusive environments. |
| 2 | Patient experiences of nurse caring behaviors based on Swanson’s theory in Indonesian hospital | (Amalina et al., 2020) | All patients who participated in this study identified nurses’ communication skills as one of their most significant experiences regarding nurses’ caring behaviors toward patients. Several participants reported that nurses demonstrated humility and care toward patients. The majority of participants stated that nurses responded promptly to patients' needs or complaints. However, patients expressed dissatisfaction with the fulfillment of the maintaining belief dimension, particularly due to a lack of communication between nurses and patients in fostering trust-based relationships. |
| 3 | Cultural competency of Nurses in a Multi-Cultural Healthcare System in Two Regions of Ghana | (Abubakari et al., 2024) | The dimensions of cultural competence include cultural encounter, awareness, skill, knowledge, and desire. The cultural encounter dimension was rated at a moderate level, while the other dimensions were rated high. However, these results should be interpreted with caution as the assessments are subjective and not supported by a comprehensive transcultural curriculum. The development of a holistic transcultural nursing curriculum in Ghana is essential to comprehensively address the care needs of patients from diverse cultural backgrounds. |
| 4 | Ethnocaring Model in Predicting Patient Satisfaction: How Powerful Is It? | (Adiutama & Fauziah, 2022) | Swanson’s caring theory, including maintaining beliefs, culture care preservation, knowing, being with, negotiation, doing for, enabling, and restructuring, significantly influences patient satisfaction. Negotiation was the most impactful, as nurses assist clients while considering cultural phenomena. The study revealed that the majority of patients were fairly satisfied; however, many felt that nurses occasionally overlooked their preferences, and nearly half reported difficulties in scheduling appointments with nurses. |
| 5 | Challenges and approaches to transcultural care: An integrative review of nurses' and nursing students' experiences | (Sharoon et al., 2021) | Providing transcultural care is complex due to differing interpretations of personal and organizational factors. Healthcare institutions need to allocate resources to enhance nurses’ interpersonal and psychological skills. Theory-based strategies, self-awareness, reflection, and empathy can significantly improve transcultural care. This approach is essential to bridge gaps caused by differences in the social values, cultural norms, and beliefs of patients and healthcare providers. |
| 6 | Culturally Sensitive Care: Definitions, Perceptions, and Practices of Health Care Professionals | (Claeys et al., 2021) | Healthcare professionals (doctors, midwives, nurses) and students were interviewed to understand their perspectives on culturally sensitive care. The findings revealed that the definitions, perceptions, and practices of culturally sensitive care by current and future healthcare professionals were often narrow, focusing primarily on daily care practices with a specific emphasis on Islamic and/or Arab cultures. The analysis indicated that healthcare providers viewed culturally sensitive care as challenging—they felt uncertain and sought solutions within the domain of cultural knowledge to comfort themselves and establish boundaries. Additionally, healthcare providers frequently reported experiencing racism in their practice settings. |
| 7 | Interpersonal Communication in Transcultural Nursing Care in India: A Descriptive Qualitative Study | (Larsen et al., 2021) | Comprehensible communication between nurses and patients was considered fundamental for quality healthcare by all nurses interviewed in this study. Communication barriers arose when nurses did not share a common language with patients or lacked an understanding of their cultural background. All participating nurses identified these intercultural communication challenges as a primary cause of miscommunication or misunderstandings. The nurses provided examples of delayed treatments and medication errors linked to these communication barriers. They recommended the implementation of standardized documentation to enhance communication and improve care safety. Additionally, the provision of interpreters was deemed crucial for delivering better services. |
| 8 | Investigation for the transcultural self-efficacy of nurses in Guizhou, China | (Li et al., 2020) | This study revealed that nurses’ transcultural self-efficacy generally ranged at a moderate level, with some nurses scoring either high or low. TSET (Transcultural Self-Efficacy Tool) scores were influenced by factors such as age, marital status, job type, position, income, and work experience. Hospital nursing management is advised to provide continuous education on transcultural nursing tailored to nurses’ demographic characteristics and TSET scores. Nursing administrators can leverage these characteristics to enhance nurses’ cultural competence. Integrating transcultural skills and knowledge into continuing education and evaluation systems will help improve nurses’ transcultural self-efficacy and the quality of care provided to patients from diverse cultural backgrounds. |
| 9 | The associations among nurse work engagement, job satisfaction, quality of care, and intent to leave: A national survey in the United States | (Wei et al., 2023) | This study highlighted differences in job satisfaction between certified and non-certified nurses, with certified nurses who demonstrating higher professionalism and quality. Higher job satisfaction was associated with increased engagement, better quality of care, and reduced turnover intentions. Organizations should enhance support for male nurses, minority groups, and diploma-educated nurses, while also exploring strategies to improve job satisfaction to ensure better care quality. |
| 10 | Culturally and Linguistically Appropriate Hospital Services Reduce Medicare Length of Stay | (Schiaffino et al., 2020) | Culturally and linguistically appropriate services can reduce patients’ length of hospital stay. This is particularly important given the increasing diversity of patients in the U.S., although many hospitals are not yet equipped to provide such services. Policy support through education, accountability, and tools for integrating culturally and linguistically appropriate services is needed to establish them as a standard of care practice. |
| 11 | Strengthening Cultural Competence in Health Professionals Through Partnerships: A Case Study of a Health Collaborative Exchange Between Malawi and Norway in Trauma Care and Emergency Medicine | (Tanyanyiwa & Chimhutu, 2022) | Healthcare professionals from Malawi found it easier to interact with Norwegian patients, who were more participatory, whereas Norwegian participants were less accustomed to Malawian patients, who tended to be more passive and agreeable to professional advice. These differences reflect the social structures of the two countries: Norway’s individualistic culture values personal freedom, while Malawi’s egalitarian society emphasizes respect for authority. These cultural and hierarchical settings influence interactions with patients, colleagues, and the community. Awareness of external factors such as culture and governance are crucial in healthcare practice |
| 12 | Cultural competence in critical care nurses and its relationships with empathy, job conflict, and work engagement: a cross-sectional descriptive study | (Soleimani & Yarahmadi, 2023) | Nurses’ cultural competence was found to be significantly associated with age, marital status, academic degree, work experience, empathy, and workplace conflict. Academic degree and empathy were the primary predictors of cultural competence, with the greatest impact observed from academic qualifications. Workplace conflict had a negative correlation with cultural competence, highlighting the importance of reducing conflicts to enhance this competence. Identifying the causes of workplace conflict can help mitigate burnout and decrease turnover intentions. |
| 13 | Perceived transcultural self-efficacy and its associated factors among nurses in Ethiopia: A cross-sectional study | (Berhanu et al., 2021) | Research indicates that male nurses exhibit higher transcultural self-efficacy compared to female nurses. Longer work experience also enhances cross-cultural self-efficacy, aligning with social cognitive theory. Intercultural communication skills, cultural sensitivity, interpersonal communication, and cultural motivation were significantly associated with transcultural self-efficacy. Nurses with higher cultural sensitivity demonstrated greater confidence in handling clients from diverse cultural backgrounds. |
| 14 | A preliminary research on transcultural capacity in global public health: from the view of public health professionals | (Ning et al., 2023) | Interest in transcultural capacity has become a key focus for public health professionals due to its relevance to the Global Public Health Assistance Cooperation (GPHAC). Participants recommended initiatives to strengthen transcultural capacity in global public health practices. They also emphasized the importance of a macro perspective on transcultural capacity, encompassing health assistance, mutually beneficial cooperation, and the integration of local customs. These principles support global public health practices while ensuring individual skills in healthcare services are not constrained. |
| 15 | Organisational and staf-related efects on cultural competence in the hospital setting: a cross-sectional online survey of nursing and medical staf | (Schenk et al., 2022) | Sociocultural diversity adds challenges to nursing, both in patient care and staff collaboration. Cultural competence improves with intercultural experiences and relevant training. Individual factors, such as staff attentiveness to this topic and migration background, play a significant role. Overall, cultural competence is more influenced by individual factors than institutional structures. |
| 16 | The influence of cultural competence on healthcare outcomes | (Harita Nair et al., 2023) | Research indicates that nurses’ cultural competence is influenced by age, education, prior training, and self-perception of cultural competence. Additionally, nurses who participate in cultural training programs tend to have higher competence scores, particularly those who are older, more highly educated, and identify themselves as having good cultural competence. Interventions are needed to enhance culturally competent healthcare services, such as educational programs for nurses. Further research is required to explore additional factors affecting cultural competence. |
| 17 | competence perspectives from nurses in four Asian countries: A qualitative descriptive study | (Songwathana et al., 2021) | Asian nurses view cultural competence as a holistic, patient-centered approach that considers religious beliefs, social norms, and patient rights. This competence involves assessing patients’ cultural backgrounds and applying professional nursing knowledge and skills. There is a shared perspective among nurses from various countries, highlighting the need for developing a more comprehensive assessment scale that incorporates beliefs, norms, and holistic care, along with future psychometric evaluations. |
| 18 | Transcultural nursing leadership: A concept analysis | (Teixeira et al., 2023) | Transcultural nursing leadership is the process of transforming leaders, nurses, and organizations to meet the cultural needs of both nurses and patients, fostering team synergy and achieving optimal health outcomes. Its attributes include cultural sensitivity, transcultural competence, behavioral adaptation, and challenging conventional paradigms. This concept is rooted in nursing theory and has a significant impact on nursing management, education, research, and policy. |
| 19 | Culturally sensitive communication in healthcare: A concept analysis | (Brooks et al., 2019) | Three key aspects of culturally sensitive care were identified: understanding one’s own culture, open and sensitive communication, and strategies for collaborating with patients and their families to achieve optimal patient care. Awareness of one’s own beliefs, values, attitudes, and cultural practices was recognized as a critical first step before learning about other cultures. |
| 20 | Culturally competent nursing care as a promoter of parental empowerment in neonatal unit: A scoping review | (Guarda-Rodrigues et al., 2024) | This review identified gaps in cultural competence and supports research and decision-making for qualification strategies and cultural interventions, particularly for family support in neonatal care units. It is essential to identify parents’ cultural needs according to the cultural context of each country. Individualized care approaches and the establishment of cultural working groups or committees in care units can enhance cultural competence. |
| 21 | Transcultural Nurses’ Caring for Pilgrims for the First Time During Hajj Season in Saudi Arabia | (Falatah et al., 2021) | Nurses serving Hajj pilgrims for the first time described their experience as fulfilling and meaningful, despite significant challenges. Strong systemic support from the Saudi government, including free healthcare and collaboration among staff, facilitated their duties. However, barriers such as language difficulties, emotional challenges, and insufficient training posed major hurdles. The nurses demonstrated high empathy and reported spiritual growth from the experience, but recommended additional training, communication technology, and improved policies to enhance the quality of transcultural care. |
| 22 | Experience of transcultural nursing for migrant workers in covid-19 field hospitals: aqualitative study in Samut Sakhon Province, Thailand | (Bussarin Arayathanitku et al., 2024) | Nurses providing transcultural care for migrant workers in COVID-19 field hospitals in Samut Sakhon, Thailand, encountered significant challenges, including language barriers, cultural differences, and emotional strain due to patients' isolation and anxiety. Despite these hurdles, nurses emphasized the importance of empathy, adaptability, and culturally sensitive approaches to build trust and provide effective care. They recommended improved training in transcultural nursing, access to interpreters, and enhanced institutional support to overcome challenges and improve care quality in such diverse and high-stress environments. |
| 23 | Cultural sensitivity and associated factors among nurses in southwest Ethiopia: a cross-sectional study | (Berhanu et al., 2024) | Nurses in southwest Ethiopia were found to have low levels of cultural sensitivity, with only 40.3% scoring as culturally sensitive. Factors such as higher education levels, effective interpersonal communication, and intercultural communication skills were strongly associated with increased cultural sensitivity. The study emphasizes the importance of training in transcultural nursing theories and cultural understanding, recommending organized educational programs to enhance cultural sensitivity and ensure high-quality, patient-centered care in a multicultural healthcare setting. |
| 24 | Validation and cross-cultural adaptation of the six-dimension scale of nursing performance- Arabic version | (Ta’an et al., 2024) | The current study produced a culturally appropriate, valid, and reliable Arabic version of the six-dimensional nursing performance scale, which also supports the scale’s dimensions. The cross-cultural adaptation process resulted in a rigorous version of the previously mentioned tool, demonstrated by the excellent psychometric properties of the Arabic version. The development of a scale that broadly covers nursing leadership practices can significantly benefit researchers in the field. Future studies investigating nursing performance among nurses can be enhanced using the findings of the current research. Additionally, this study facilitates valid comparisons of cross-cultural study findings by employing robust methodological procedures for cross-cultural adaptation. |
| 25 | Increasing cultural awareness: Qualitative study of nurses’ perceptions about cultural competence training | (Kaihlanen et al., 2019) | The qualitative study explored nurses’ perceptions of cultural competence training conducted in southern Finland. The training emphasized raising awareness of nurses’ own cultural characteristics to improve cross-cultural care. Participants highlighted the training’s utility in fostering self-awareness, reshaping communication practices, and enhancing respect for patients from diverse cultural backgrounds. The inclusion of storytelling and real-life examples enriched the training experience, but nurses suggested integrating feedback from immigrant communities and adopting hybrid or condensed formats for broader accessibility. Overall, the training demonstrated potential to improve cultural competence but requires refinement for scalability and effectiveness in diverse healthcare settings. |
Discussion
The Importance of Cultural-Based Caring Competence
Implementation of Cultural-Based Caring
Strategic Recommendations
Conclusion
Funding
Acknowledgments
Conflicts of Interest
References
- Abubakari, A. K., Gross, J., Boateng, S. K., & Ansong, R. (2024). Cultural competency of Nurses in a Multi-Cultural Healthcare System in Two Regions of Ghana. International Journal of Africa Nursing Sciences, 20. [CrossRef]
- Adiutama, N. M., & Fauziah, W. (2022). Ethnocaring Model in Predicting Patient Satisfaction: How Powerful Is It? Babali Nursing Research, 3(3), 264–272. [CrossRef]
- Alikari, V., Gerogianni, G., Fradelos, E. C., Kelesi, M., Kaba, E., & Zyga, S. (2023). Perceptions of Caring Behaviors among Patients and Nurses. International Journal of Environmental Research and Public Health, 20(1). [CrossRef]
- Amalina, S. F., Rachmawaty, R., Ilkafah, I., & Erfina, E. (2020). Patient experiences of nurse caring behaviors based on Swanson’s theory in Indonesian hospital. Enfermeria Clinica, 30, 332–336. [CrossRef]
- Berhanu, R. D., Golja, E. A., Gudeta, T. A., Feyisa, J. W., Rikitu, D. H., & Bayane, Y. B. (2024). Cultural sensitivity and associated factors among nurses in southwest Ethiopia: a cross-sectional study. BMC Nursing, 23(1), 1–8.
- Berhanu, R. D., Tesema, A. A., Deme, M. B., & Kanfe, S. G. (2021). Perceived transcultural self-efficacy and its associated factors among nurses in Ethiopia: A cross-sectional study. PLoS ONE, 16(7 July). [CrossRef]
- Brooks, L. A., Manias, E., & Bloomer, M. J. (2019). Culturally sensitive communication in healthcare: A concept analysis. In Collegian (Vol. 26, Issue 3, pp. 383–391). Elsevier B.V. [CrossRef]
- Bussarin Arayathanitku, Jutarat Bandansin, Su-ari Lamtraku, Pacharaphorn Kwiensungnoen, & Suwaluck Eaksamai. (2024, August). View of Experience of transcultural nursing for migrant workers in covid-19 field hospitals: a qualitative study in Samut Sakhon Province, Thailand. Available online: https://e-journal.unair.ac.id/JNERS/article/view/48328/29741.
- Claeys, A., Berdai-Chaouni, S., Tricas-Sauras, S., & De Donder, L. (2021). Culturally Sensitive Care: Definitions, Perceptions, and Practices of Health Care Professionals. Journal of Transcultural Nursing, 32(5), 484–492. [CrossRef]
- Falatah, R., Almansour, L., Alsolami, A., Aljehani, A., Al Dhubayban, E., & Walker, R. K. (2021). Transcultural Nurses’ Caring for Pilgrims for the First Time During Hajj Season in Saudi Arabia. Journal of Religion and Health, 60(1), 232–245. [CrossRef]
- Guarda-Rodrigues, J., Ferreira Calado Dias, M. P., Rodrigues Fatela, M. M., Rosa Jeremias, C. J., Gonçalves Negreiro, M. P., & Lemos e Sousa, O. (2024). Culturally competent nursing care as a promoter of parental empowerment in neonatal unit: A scoping review. In Journal of Neonatal Nursing. Elsevier Ltd. [CrossRef]
- Harita Nair, M., Pandya, A., & Parveen, S. (2023). The influence of cultural competence on healthcare outcomes. Salud, Ciencia y Tecnologia, 3. [CrossRef]
- Kaihlanen, A.-M., Hietapakka, L., & Heponiemi, T. (2019). Increasing cultural awareness: Qualitative study of nurses’ perceptions about cultural competence training. BMC Nursing, 18(1). [CrossRef]
- Larsen, R., Mangrio, E., & Persson, K. (2021). Interpersonal Communication in Transcultural Nursing Care in India: A Descriptive Qualitative Study. Journal of Transcultural Nursing, 32(4), 310–317. [CrossRef]
- Li, J., Wu, B., He, Z., Liu, J., Xiao, R., & Luo, Y. (2020). Investigation for the transcultural self-efficacy of nurses in Guizhou, China. International Journal of Nursing Sciences, 7(2), 191–197. [CrossRef]
- Martikainen, R.-M., Kuivila, H.-M., Koskenranta, M., Kamau, S., Oikarainen, A., Matinlompolo, N., Juntunen, J., & Mikkonen, K. (2024a). Exploring the integration of culturally and linguistically diverse nurses and nursing students in healthcare: A cross-sectional study. Nurse Education in Practice, 80, 104129. [CrossRef]
- Martikainen, R.-M., Kuivila, H.-M., Koskenranta, M., Kamau, S., Oikarainen, A., Matinlompolo, N., Juntunen, J., & Mikkonen, K. (2024b). Exploring the integration of culturally and linguistically diverse nurses and nursing students in healthcare: A cross-sectional study. Nurse Education in Practice, 80, 104129. [CrossRef]
- Melody K. Schiaffino, Melissa Ruiz, Melissa Yakuta, Alejandro Contreras, Setareh Akhavan, Britney Prince, & Robert Weech-Maldonado. (2020). Culturally and Linguistically Appropriate Hospital Services Reduce Medicare Length of Stay. Ethnicity & Disease, Inc., 3(4), 603–610. Available online: https://www.jstor.org/stable/10.2307/48668032.
- Ning, F., Xin, L., Quan, W., Xiaohui, L., & Xiaoping, D. (2023). A preliminary research on transcultural capacity in global public health: from the view of public health professionals. BMC Public Health, 23(1). [CrossRef]
- Schenk, L., Sonntag, P. T., Beck, P., Khan, Z., Peppler, L., & Schouler-Ocak, M. (2022). Organisational and staff-related effects on cultural competence in the hospital setting: a cross-sectional online survey of nursing and medical staff. BMC Health Services Research, 22(1). [CrossRef]
- Schiaffino, M. K., Ruiz, M., Yakuta, M., Contreras, A., Akhavan, S., Prince, B., & Weech-Maldonado, R. (2020). Culturally and linguistically appropriate hospital services reduce medicare length of stay. Ethnicity and Disease, 30(4), 603–610. [CrossRef]
- Sharoon, S., Nizar, A., ude L. Tayaben, & Ahtisham, Y. (2021). Challenges and approaches to transcultural care: An integrative review of nurses’ and nursing students’ experiences. Journal of Professional Nursing, 37(6), 1119–1131.
- Soleimani, M., & Yarahmadi, S. (2023). Cultural competence in critical care nurses and its relationships with empathy, job conflict, and work engagement: a cross-sectional descriptive study. BMC Nursing, 22(1). [CrossRef]
- Songwathana, P., Chunuan, S., Balthip, K., Purinthrapibal, S., Hui, T., Ibrahim, K., & Thuy, L. T. (2021). Cultural competence perspectives from nurses in four Asian countries: A qualitative descriptive study. Journal of Health Science and Medical Research, 39(1), 57–66. [CrossRef]
- Stolt, M., Katajisto, J., Kottorp, A., & Leino-Kilpi, H. (2019). Measuring Quality of Care: A Rasch Validity Analysis of the Good Nursing Care Scale. Journal of Nursing Care Quality, 34(4), E1–E6. [CrossRef]
- Ta’an, W. F., Rababah, J. A., Al-Hammouri, M. M., Yousef, J., Mukattash, T. L., & Williams, B. (2024). Validation and cross-cultural adaptation of the six-dimension scale of nursing performance- arabic version. BMC Nursing, 23(1). [CrossRef]
- Tanyanyiwa, T. A., & Chimhutu, V. (2022). Strengthening Cultural Competence in Health Professionals Through Partnerships: A Case Study of a Health Collaborative Exchange Between Malawi and Norway in Trauma Care and Emergency Medicine. Inquiry (United States), 59. [CrossRef]
- Teixeira, G., Cruchinho, P., Lucas, P., & Gaspar, F. (2023). Transcultural nursing leadership: A concept analysis. International Journal of Nursing Studies Advances, 5. [CrossRef]
- Wei, H., Horsley, L., Cao, Y., Haddad, L. M., Hall, K. C., Robinson, R., Powers, M., & Anderson, D. G. (2023). The associations among nurse work engagement, job satisfaction, quality of care, and intent to leave: A national survey in the United States. International Journal of Nursing Sciences, 10(4), 476–484. [CrossRef]
- Wong, F. M. F. (2024). Job satisfaction in nursing: A qualitative inquiry into novice and experienced nurses’ perspectives. Nurse Education in Practice, 78, 104018. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




