1. Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive, fibrotic interstitial lung disease. In untreated patients who are not candidates for lung transplantation, the average life expectancy is 2–3 years [
1]. The clinical course of IPF is unpredictable and varies among patients [
2]. While most patients are managed in outpatient care settings, approximately 10% experience acute exacerbations (AEs) within the first two years following diagnosis [
3]. Acute exacerbation of idiopathic pulmonary fibrosis (IPF-AE) is typically characterized as clinically significant respiratory deterioration developing within less than a month, associated with new diffuse alveolar damage. The annual incidence of IPF-AE is estimated to be 4.1%. Acute exacerbations are the leading cause of mortality in IPF patients. Despite advances in medical therapies, in-hospital mortality rates exceed 50% [
4]. Furthermore, post-discharge mortality within the first six months remains notably high. Identifying prognostic factors in these patients is critical for effective patient management.
Complete blood count (CBC) is a routine laboratory test with prognostic significance in many diseases. A recent study on IPF patients evaluated CBC parameters, highlighting the prognostic value of red cell distribution width and the neutrophil-to-lymphocyte ratio [
5]. CBC includes mean platelet volume (MPV) and platelet count (PC). Platelets have been shown to play a significant role in the immune response to inflammation [
6]. MPV reflects platelet size and activity and has been evaluated in diseases with intense inflammation, being reported as an important biomarker for predicting survival [
7,
8]. A strong negative correlation exists between MPV and PC. The mean platelet volume-to-platelet count ratio (MPR) was first proposed as a survival marker in pancreatic cancer [
9] and has since been identified as a predictive biomarker for prognosis in various diseases [
10,
11]. Considering the role of platelets in IPF, the heightened inflammation observed during acute exacerbations could make MPR even more significant. However, the relationship between MPR and IPF-AE has not yet been reported in the literature. Therefore, this study aimed to evaluate MPR and other factors affecting mortality in patients with IPF-AE monitored in the intensive care unit.
2. Materials and Methods
This study was retrospectively designed to include patients diagnosed with IPF-AE who were monitored in the intensive care unit (ICU) of our hospital between January 1, 2017, and November 15, 2023. IPF diagnosis date, treatments used for IPF with computed tomography, and demographic characteristics were examined Vital findings at the time of admission to intensive care, blood tests taken within the first 24 hours, treatments applied, respiratory support, and outcome status were recorded.
The diagnosis of IPF-AE was based on the following criteria:
A prior or current diagnosis of IPF.
Acute worsening of dyspnea within less than one month.
Presence of new bilateral ground-glass opacities and/or consolidations superimposed on an underlying usual interstitial pneumonia (UIP) pattern on thoracic CT.
Worsening not fully explained by heart failure or fluid overload.
Patients meeting these criteria were classified as having IPF-AE after excluding alternative diagnoses such as pneumonia, pulmonary embolism, and pneumothorax.
The extent of radiological involvement in patients was assessed using high-resolution computed tomography (HRCT). HRCT was performed in the supine position during inspiration and expiration, with 1.0 mm thick sections covering the entire lungs. The imaging evaluations included assessment of upper lobe involvement and the extent of disease involvement.
In our research, CBC analyses were performed using the Mindray BC 6800 automated complete blood count analyzer (Shenzhen Mindray Bio-medical Electronics Co., Ltd., China). PC were determined using the impedance method, which involves directly counting the platelets passing through the aperture, with results expressed in units of 103/µL. MPV was simultaneously derived from the platelet histogram.
MPV and PC were obtained from the complete blood count performed within the first 24 hours of ICU admission. The MPR was calculated by dividing the MPV by the PC.
2.1. Patient Selection
Patients monitored in the ICU for IPF-AE during the specified dates were included in the study. Exclusion criteria were as follows: patients with any history of platelet or hematopoietic abnormalities related to MPV or platelet , patients under 18 years of age, those monitored for less than 24 hours, patients with IPF who were admitted for reasons other than acute exacerbation, patients electively admitted to the ICU for postoperative monitoring, patients with interstitial lung diseases other than IPF, patients diagnosed with disseminated intravascular coagulation (DIC), and those with incomplete data.
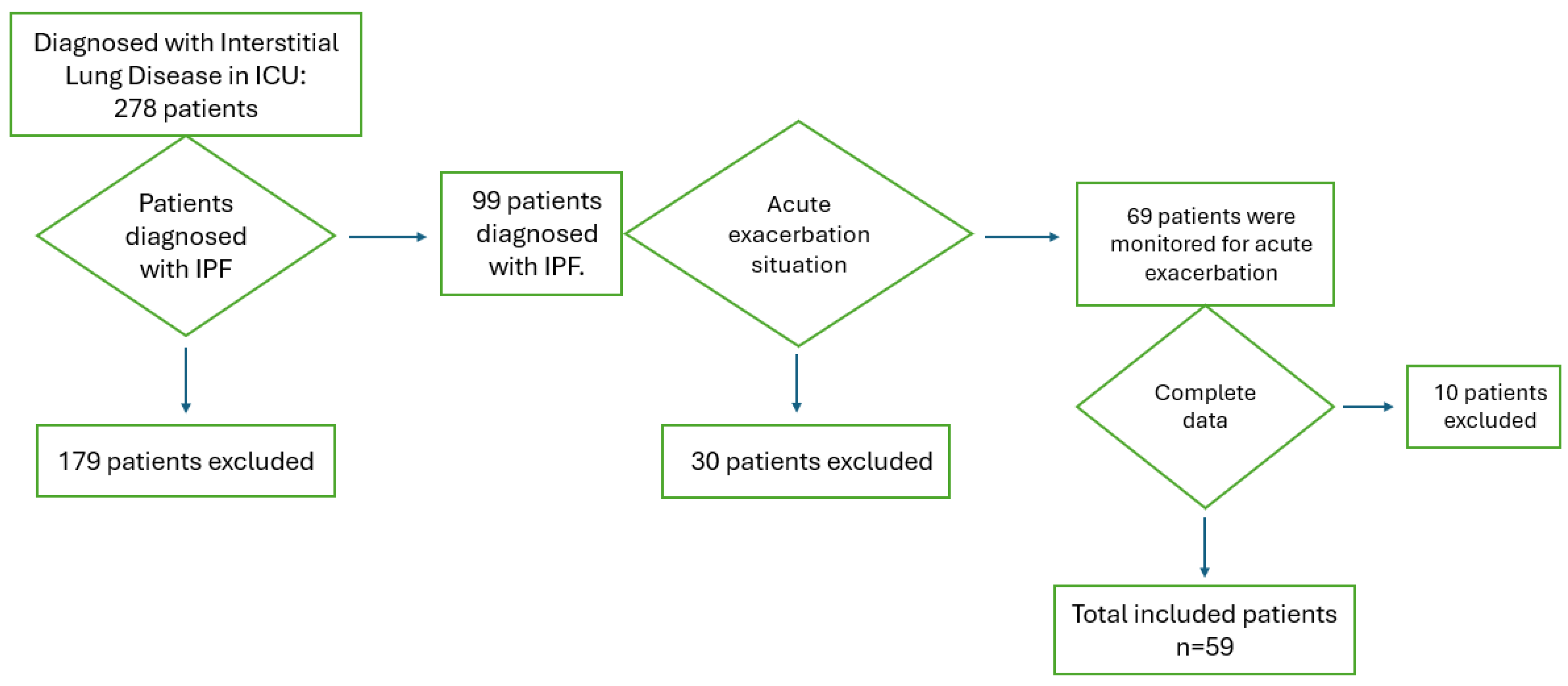
Figure 1 shows a flowchart detailing the patients included in and excluded from this study.
In the presence of appropriate findings for the diagnosis of DIC, the DIC scoring system developed by the International Society on Thrombosis and Haemostasis was used. The total score was calculated by combining platelet count, fibrinogen levels, prolongation of prothrombin time (PT), and D-dimer levels. A score greater than 5 was considered indicative of a high likelihood of DIC, and consultation with the hematology department was obtained. Patients suspected of having DIC were excluded from the study. Ethical approval for the study was obtained from the Clinical Research Ethics Committee of our hospital, with decision number 2840, dated November 22, 2023. Ethical principles outlined in the Declaration of Helsinki were adhered to throughout the study.
2.2. Statistical Analysis
The statistical analysis of the collected data was performed using IBM SPSS Statistics version 27.0. The normality of the distribution of continuous variables was evaluated using the Kolmogorov-Smirnov test. Data following a normal distribution were presented as mean ± standard deviation (Mean ± SD), while data not following a normal distribution were presented as median (min-max). Categorical variables were expressed as frequencies and percentages (%), and continuous variables were reported as Mean ± SD or median (min-max), depending on their distribution. Categorical variables between groups were compared using the Chi-square test, and continuous variables were compared using the Independent T Test (for normally distributed data) or the Mann-Whitney U test (for non-normally distributed data) depending on the distribution of the data.
A ROC (Receiver Operating Characteristic) analysis was performed for the MPR laboratory parameter. The analysis determined the optimal cut-off point for predicting mortality, and the associated Area Under the Curve (AUC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), as well as positive and negative likelihood ratios (LR+ and LR−) were calculated.
Univariate Cox Regression Analysis was used to evaluate the relationship between clinical, radiological and laboratory parameters and mortality. Results of the univariate analysis were reported as Hazard Ratios (HR), 95% Confidence Intervals (CI), and p-values. Parameters found to be significant in the univariate analysis were included in the Multivariate Cox Regression Analysis to control for the effects of other factors. In the multivariate analysis, the independent effects of these parameters on mortality were evaluated as independent risk factors, and the results were presented with HR, 95% CI, and p-values. Comparisons with a p-value below 0.05 were considered statistically significant.
3. Results
Among the patients monitored in the intensive care unit, 278 were diagnosed with interstitial lung disease. Of these, 99 patients had a diagnosis of IPF. Thirty patients who were monitored for reasons unrelated to an acute exacerbation and 10 patients with incomplete data were excluded from the study. A total of 59 patients were included in the analysis. The demographic characteristics of the included patients are presented in
Table 1.
A total of 45 patients included in the study were using antifibrotic therapy. The clinical characteristics of IPF and treatments administered to the patients are presented in
Table 2.
When examining clinical factors associated with mortality in the included patients, the need for invasive mechanical ventilation was found to be significantly associated with increased mortality (p<0.001). Mortality was also higher in patients with upper lobe involvement observed on computed tomography (p=0.043) (
Table 3).
Table 4 presents the evaluation of laboratory findings at the time of admission, providing a comprehensive overview of key parameters assessed during the initial examination.
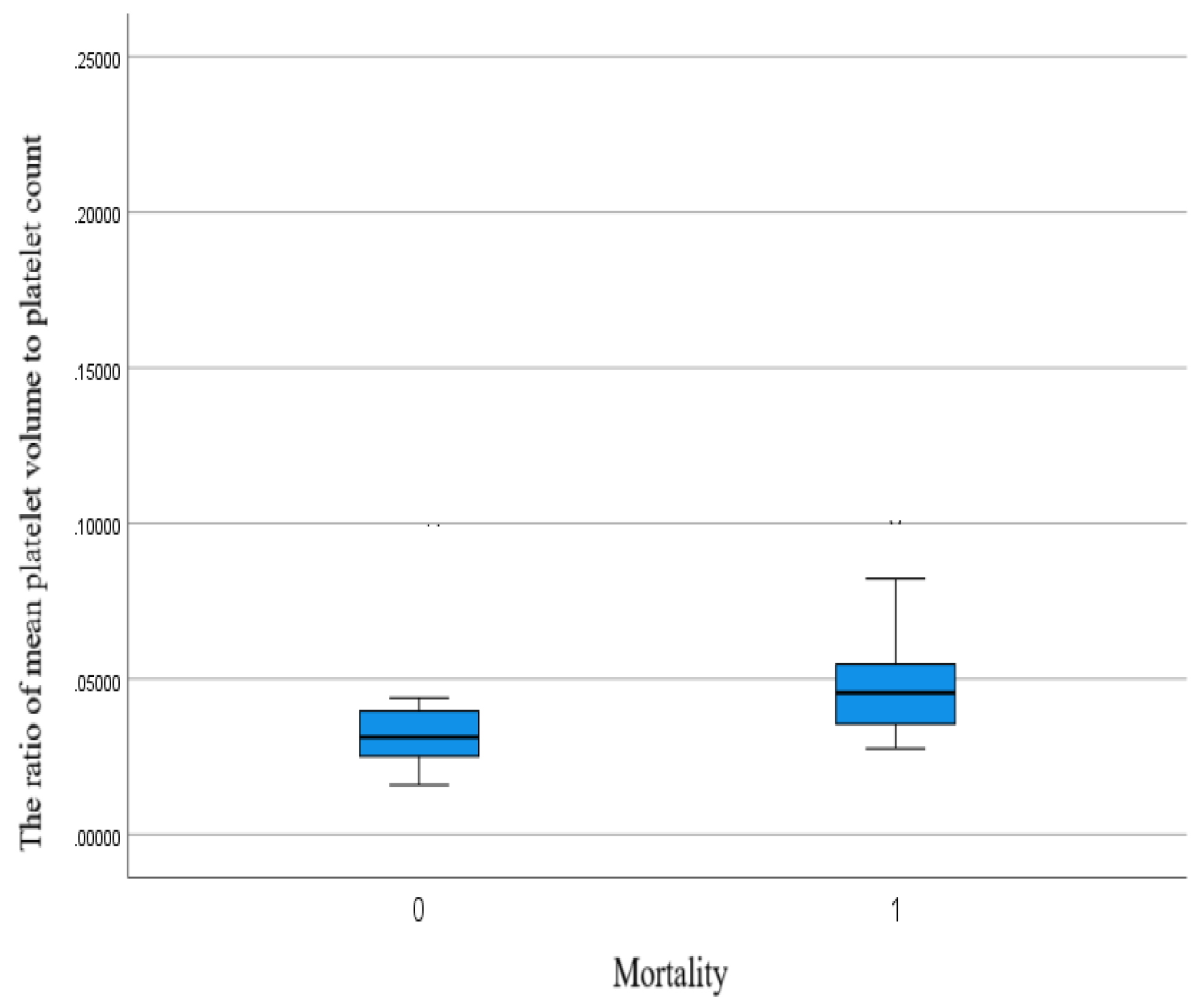
MPR was found to be 0.043 in surviving patients and 0.048 in deceased patients. A significant difference was observed between the groups (p<0.001) (
Figure 2).
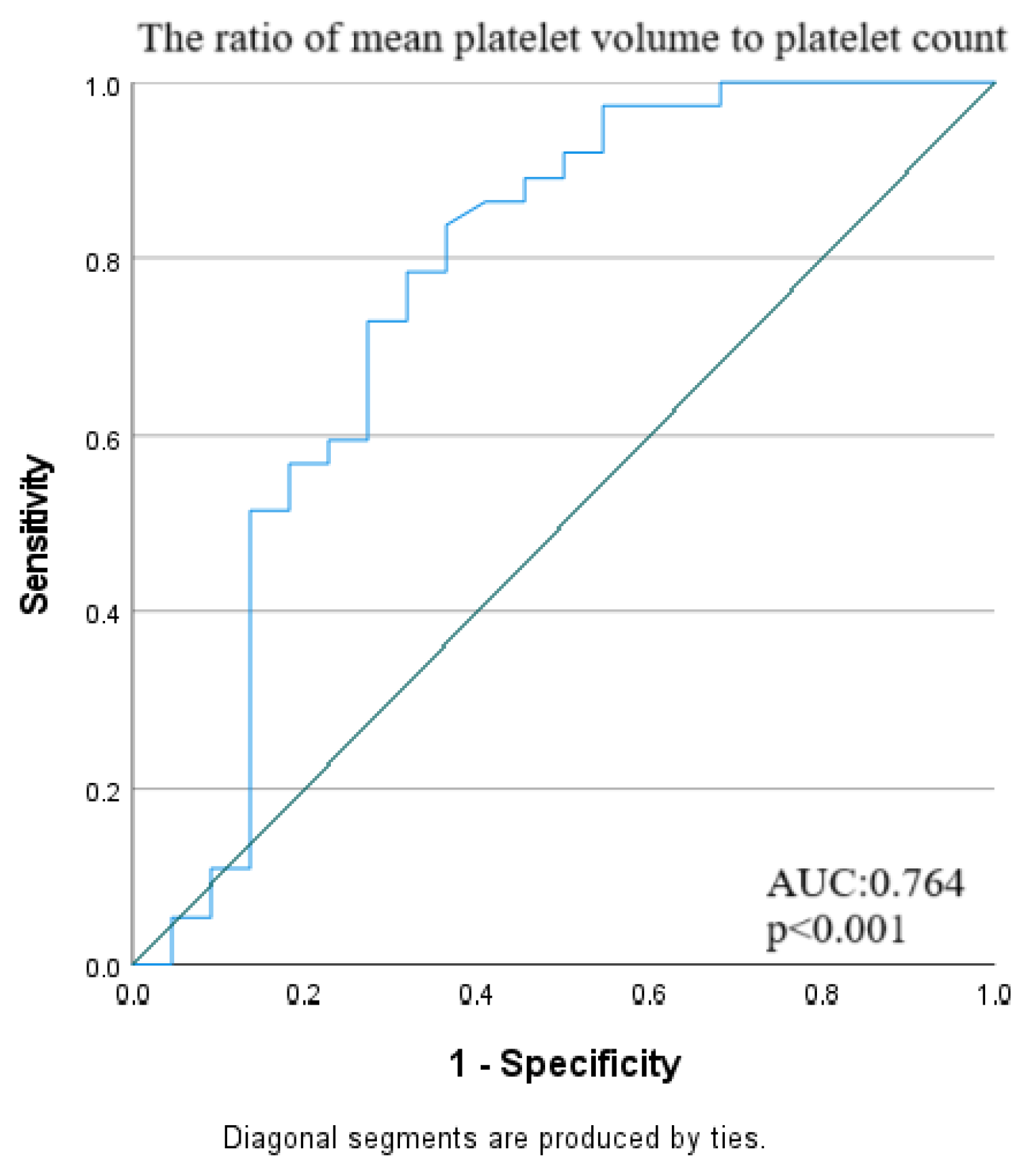
The cut-off value for MPR was determined to be 0.033, with a sensitivity of 83.7% and a specificity of 63.64%, and it was identified as a significant predictor of mortality (AUC: 0.764, 95% CI: 0.635–0.864; p<0.001) (
Table 5). The ROC curve for MPR in predicting mortality is shown in
Figure 3.
To assess the independent effects of clinical, radiological, and laboratory parameters on mortality, the impact of dependent variables and MPR was initially examined. During this process, the two most significant parameters were identified. Using these parameters, a multivariate Cox regression model was developed to provide a more comprehensive evaluation of the independent effect of MPR on mortality alongside other variables. The results are presented in
Table 6.
In univariate analysis, upper lobe involvement on computed tomography was significantly associated with mortality (HR:2.13, 95%CI:1.06-4.27, p=0.032). Additionally, platelet count (HR:0.996, 95%CI:0.002-0.999, p=0.010) and MPV (HR:1.44, 95%CI:1.05-1.96, p=0.022) were also significantly associated with mortality.
A MPR>0.033 was identified as a significant risk factor in univariate analysis (HR:4.55, 95%CI:1.76-11.78, p=0.002). However, it did not reach statistical significance in the multivariate analysis (HR:2.17, 95%CI:0.79-5.92, p=0.130).
Invasive mechanical ventilation support was identified as the strongest independent risk factor for mortality in both univariate (HR:13.23, 95%CI:4.01-43.64, p<0.001) and multivariate analysis (HR: 9.98, 95% CI: 2.92–34.12, p<0.001).
4. Discussion
This study presents an evaluation of 59 patients diagnosed with IPF who were monitored in the ICU. The factors affecting mortality were investigated in light of the patients' clinical, radiological, and laboratory findings. The results obtained through Cox regression analysis demonstrated that certain clinical parameters, particularly the need for invasive mechanical ventilation (IMV), significantly increased the mortality risk of the patients. Additionally, radiological findings such as upper lobe involvement on computed tomography, as well as laboratory parameters including PC, MPV, and the MPR, were identified as valuable prognostic indicators for predicting mortality. Our study highlights the potential clinical utility of MPR, which could be validated further through larger cohort studies and prospective research.
Mortality is high in IPF-AE cases requiring ICU admission due to acute respiratory failure (ARF). However, reported mortality rates vary across studies. In general, mortality is influenced by the subtype of interstitial lung disease (ILD), with IPF being associated with worse outcomes compared to other ILD subtypes [
12]. In a study by Ba et al. on patients with ILD monitored for respiratory failure, mortality was reported to be higher in IPF compared to other subtypes, with in-hospital mortality exceeding 50% [
13]. In our study, in-hospital mortality was found to be 67.4%.
In our study, 81.4% of the included patients were male. The most common comorbidities were cardiovascular diseases. It was observed that the majority of patients (76.2%) were on antifibrotic therapy. A recent review examining the clinical characteristics and treatment strategies of IPF-AE highlighted that the pathogenesis of IPF-AE remains unclear and that multiple mechanisms may be involved simultaneously. Corticosteroids were reported to remain the mainstay of treatment for IPF-AE [
14]. Similarly, in our study, all patients received corticosteroid therapy.
In IPF, the development of ARF requiring IMV is associated with poor prognosis. The literature reports that mortality is very high in acute exacerbations associated with ILD requiring intensive care [
15]. A recent study also demonstrated that in fibrosis-dominant ILD patients, mortality reaches up to 75% in cases requiring mechanical ventilation [
16]. In our study, the majority of patients (67.8%) required invasive mechanical ventilation. The analysis showed a strong association between the need for IMV and mortality (p<0.001).
The course of IPF is unpredictable; however, given its potentially aggressive progression, radiological extent is of great importance in predicting mortality. In IPF, the honeycombing pattern typically has a basal and peripheral predominance. Upper lobe involvement may be observed in the advanced stages of the disease. Another significant finding in our study was that patients with upper lobe involvement on computed tomography had higher mortality rates (p=0.043). This finding is meaningful as it may be associated with more advanced disease. The impact of upper lobe involvement on mortality was demonstrated in univariate regression analysis. However, in multivariate regression, its significance appeared to diminish, likely due to the dominant effect of other factors, such as the need for invasive mechanical ventilation support.
In IPF, increased platelet activation and accumulation in the lung fields have been demonstrated in animal studies [
17]. MPV has been reported to be elevated in IPF patients compared to healthy controls and may serve as a marker of platelet activation [
18]. However, no direct causal relationship between platelets or platelet-derived products and IPF progression has been established in studies. In our study, thrombocytopenia was found to be associated with mortality in these critically ill IPF patients. Additionally, higher MPV levels were observed in patients with fatal outcomes.
MPR was first proposed as a survival marker in pancreatic cancer [
9]. It has since been evaluated as a predictive marker for prognosis in various diseases [
19,
20]. In our study, the use of MPR for mortality prediction was validated through ROC analysis. With the determined cut-off value for MPR (83.7% sensitivity, 63.64% specificity), it emerged as a significant indicator for predicting mortality. MPR was identified as a significant risk factor in univariate analysis; however, it did not reach statistical significance in multivariate analysis. This finding was associated with the need for IMV, which is another parameter in multiple regression, being a very strong independent risk factor for mortality. Our study can serve as a guide for further exploration of MPR's effectiveness in clinical practice, requiring validation and more detailed investigation through larger cohort studies and prospective research.
Our study has certain limitations. IPF is a rare disease, and with the introduction of antifibrotic therapies, acute exacerbations have become less common. This is thought to have contributed to the small sample size of our study. Additionally, respiratory function test (RFT) findings were not available for all patients, and compliance with RFTs was limited in end-stage patients. Therefore, RFT findings were not included in the analysis.
5. Conclusions
In our study of patients monitored in the intensive care unit for IPF-AE, we found that age and gender did not influence prognosis in acute exacerbations. However, the need for invasive mechanical ventilation and the radiological extent of the disease were associated with increased mortality. Additionally, the use of the MPR as a prognostic biomarker may offer a novel approach in the management of IPF patients. These findings could contribute to the development of strategies for early intervention in IPF patients. Further studies with larger sample sizes are needed to validate these results.
Author Contributions
Conceptualization, M.A., B.A.Ö. and M.Y.; formal analysis, K.E., M.H.E. and Ö.F.T.; data curation, K.E., M.H.E. and Ö.F.T.; visualization T.Ö. and D.H.; investigation, T.Ş.Ö. and G.E.D.; methodology, M.A. and B.A.Ö.; supervision, M.D. and O.M..; validation, D.H. and T.Ş.Ö.; writing—original draft, M.A. and B.A.Ö.; writing—review and editing, O.M., M.D. and D.Ç. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Institutional Review Board Statement
Ethical approval for the study was obtained from the Clinical Research Ethics Committee of Ankara Atatürk Sanatorium Training and Research Hospital (Decision No: 2840, dated November 22, 2023).
Informed Consent Statement
Informed consent was not required due to the retrospective nature of the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
-
Kropski JA, Blackwell TS. Progress in Understanding and Treating Idiopathic Pulmonary Fibrosis. Annu Rev Med. 2019, Cilt 27;70:211-24. [CrossRef]
-
Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am J Respir Crit Care Med. 2022, Cilt 1;205(9):e18-e47. [CrossRef]
-
Wang Y, Ji Z, Xu B, Li S, Xie Y. The incidence of acute exacerbation of idiopathic pulmonary fibrosis: a systematic review and meta-analysis. Sci Rep. 2024;14(1):21080. [CrossRef]
-
Zhuang Y, Zhou Y, Qiu X, Xiao Y, Cai H, Dai J. Incidence and impact of extra-pulmonary organ failures on hospital mortality in acute exacerbation of idiopathic pulmonary fibrosis. Sci Rep. 2020;10(1):10742. [CrossRef]
-
Polat G, Özdemir Ö, Ermin S et al. Predictive factors of mortality in patients with idiopathic pulmonary fibrosis treated with antifibrotics: a novel prognostic scoring system. Sarcoidosis Vasc Diffuse Lung Dis. 2024, Cilt 28;41(2):e2024021. [CrossRef]
-
Van der Meijden PEJ, Heemskerk JWM. Platelet biology and functions: new concepts and clinical perspectives. Nat Rev Cardiol. 2019, Cilt 16(3):166-79.
-
Korniluk A, Koper-Lenkiewicz OM, Kamińska J, Kemona H, Dymicka-Piekarska V. Mean Platelet Volume (MPV): New Perspectives for an Old Marker in the Course and Prognosis of Inflammatory Conditions. Mediators Inflamm. 2019, Cilt 17;2019:9213074. [CrossRef]
-
Doganci M, Eraslan Doganay G. Prognostic Significance of Thrombocytopenia and Mean Platelet Volume in COPD Patients with Acute Exacerbations in ICU Settings. Med Sci Monit. 2024, Cilt 9;30:e944946. [CrossRef]
-
Gong X, Zhang L, Yang D, et al. Mean Platelet Volume/Platelet Count Ratio is Associated With Prognosis in Patients With Pancreatic Cancer. Int J Clin Exp Med. 2016, Cilt 9:16379–86.
-
Altinbas A, Keles BO, Yilmaz ET, Coban S. Relationship of intensive care scoring systems with neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and mean platelet volume values. Bratisl Lek Listy. 2024, Cilt 125(6):371-75. [CrossRef]
-
Hassan M, Abdayem C, El Daouk S, Matar BF. Correlation of Hemoglobin Level With New Inflammatory Markers in the Emergency Department: A Retrospective Study Exploring Neutrophil-to-Lymphocyte, Monocyte-to-Lymphocyte, Platelet-to- Lymphocyte, and Mean Platelet Volume-to-Platelet Count Ratios. Cureus. 2024, Cilt 2;16(3):e55401. [CrossRef]
-
Charokopos A, Moua T, Ryu JH, Smischney NJ. Acute exacerbation of interstitial lung disease in the intensive care unit. World J Crit Care Med. 2022, Cilt 9;11(1):22-32. [CrossRef]
-
Ba C, Wang H, Jiang C, Shi X, Jin J, Fang Q. Clinical manifestations and prognostic factors analysis of patients hospitalised with acute exacerbation of idiopathic pulmonary fibrosis and other interstitial lung diseases. BMJ Open Respir Res. 2024, Cilt 27;11(1). [CrossRef]
-
Luo X, Xiang F. Acute exacerbation of idiopathic pulmonary fibrosis a narrative review primary focus on treatments. J Thorac Dis. 2024, Cilt 30;16(7):4727-4741.
-
Matsunashi A, Nagata K, Morimoto T, Tomii K. Mechanical ventilation for acute exacerbation of fibrosing interstitial lung diseases. Respir. Investig. 2023, Cilt 61:306–313. [CrossRef]
-
Martin MJ, Moua T. Mechanical Ventilation and Predictors of In-Hospital Mortality in Fibrotic Interstitial Lung Disease with Acute Respiratory Failure: A Cohort Analysis Through the Paradigm of Acute Respiratory Distress Syndrome. Crit. Care Med. 2020, Cilt 48:993. [CrossRef]
-
Carrington R, Jordan S, Wong YJ, Pitchford SC, Page CP. A novel murine model of pulmonary fibrosis: the role of platelets in chronic changes induced by bleomycin. J Pharmacol Toxicol Methods. 2021, Cilt 109:107057. [CrossRef]
-
Ntolios P, Papanas N, Nena E et al. Mean Platelet Volume as a Surrogate Marker for Platelet Activation in Patients With Idiopathic Pulmonary Fibrosis. Clin Appl Thromb Hemost. 2016, Cilt 22(4):346-50. [CrossRef]
-
Zhang H, Lin F, Wang Z. Mean platelet volume/platelet count ratio in combination with tumor markers in colorectal cancer: a retrospective clinical study. BMC Cancer. 2023, Cilt 7;23(1):124. [CrossRef]
-
Nurkoç SG, Yakışan T. Mean Platelet Volume/Platelet Count Ratio and Dipper/Non-Dipper Hypertensive Patients. Angiology. 2024, Cilt 22:33197241274825. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).