1. Introduction
Hypercapnic respiratory failure (HRF) is a type of respiratory failure characterized by an increase in arterial carbon dioxide pressure (pCO2>45 mmHg) [
1]. HRF developing during acute exacerbations of chronic obstructive pulmonary disease (COPD) is a significant clinical condition associated with severe morbidity and mortality [
2]. Due to its frequent requirement for invasive or non-invasive mechanical ventilation, HRF is one of the major reasons for admission to intensive care units (ICUs) [
3]. Although numerous studies in the current literature focus on HRF-related mortality and the effects of non-invasive mechanical ventilation, data on the long-term prognosis of these patients remain limited. In particular, the fact that existing scoring systems are typically designed to evaluate short-term outcomes creates a significant gap in this area. There is a critical need to develop new scoring systems that include factors such as age, comorbidity burden, and their impact on long-term survival to enhance clinical decision-making processes.
In this context, the DECAF (Dyspnea, Eosinopenia, Consolidation, Acidemia and Atrial Fibrillation) score, which is widely used to predict mortality in acute exacerbations of COPD (AE-COPD) [
4], has not been adequately investigated for its effectiveness in predicting long-term prognosis. The DECAF score does not include age, an important prognostic factor, which poses significant limitations in estimating long-term survival, particularly in elderly patient populations. Many studies have emphasized that age is not only a risk factor for mortality but also a key determinant of long-term prognosis [
5]. The Age-Adjusted DECAF (A-DECAF) score was developed to improve the accuracy of survival predictions by incorporating age as a variable. It was designed to evaluate long-term survival predictions in patients who develop HRF due to COPD.
2. Materials and Methods
This study was conducted retrospectively between April 2022 and November 2023 on patients diagnosed with HRF in the pulmonary diseases intensive care unit of our hospital. The study was initiated with the approval of the Clinical Research Ethics Committee of Ankara Atatürk Sanatorium Training and Research Hospital (approval number: 187, dated 25.12.2024) and was carried out in accordance with the ethical principles outlined in the Declaration of Helsinki.
The medical treatment of the patients was planned based on national and international guidelines. Invasive or non-invasive mechanical ventilation methods were utilized for the treatment of HRF. Non-invasive mechanical ventilation (NIMV) was mostly applied using an oronasal mask. Tidal volumes were calculated based on the patients' estimated ideal body weight. Patients were continuously monitored, and oxygen support was adjusted to maintain arterial oxygen saturation within the range of 90-92%. The response to treatment was evaluated based on vital signs, such as respiratory rate, blood pressure, and heart rate, as well as arterial blood gas (ABG) parameters. Arterial blood gas results obtained at the time of ICU admission and prior to discharge were also recorded.
As part of the study, the demographic and clinical characteristics of the patients, such as age, gender, comorbidities, and medications, were thoroughly evaluated. Additionally, blood tests conducted within the first 24 hours of ICU admission, ABG results obtained at discharge, and applied treatment protocols were examined. The primary outcome of the study was defined as the time from the date of HRF diagnosis to the date of death. The relationship between the obtained parameters and one-year post-discharge survival was comprehensively analyzed.
2.1. Patient Selection
This study was planned to include patients diagnosed with hypercapnic respiratory failure (pCO2>45 mmHg) during the specified period.
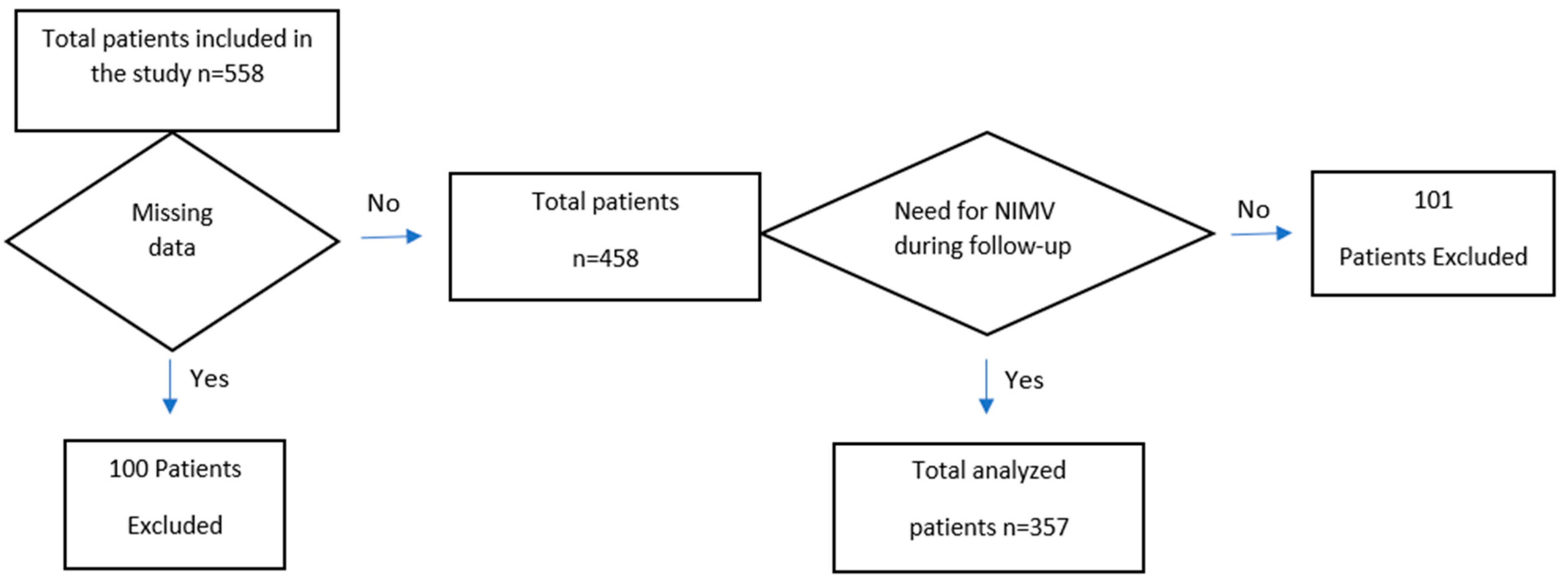
Figure 1 shows a flowchart detailing the patients included in and excluded from this study.
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
Patients who did not consent to participate in the study
Patients with HRF caused by procedures requiring general anesthesia and/or sedation
Patients with HRF attributed to cardiac causes
Patients with HRF resulting from interstitial lung disease
Patients with HRF due to neuromuscular diseases
Patients with HRF related to obstructive sleep apnea syndrome
Patients who no longer required NIMV during follow-up
Patients with a length of stay less than one day
Patients who died during the ICU follow-up period
Patients with incomplete data
2.1.3. Follow-Up Period
The follow-up period for the primary outcome was set at 1 year. Participants were monitored from the date of their initial HRF diagnosis until the date of death or December 1, 2024, whichever came first.
2.2. Calculation of the DECAF Score
The DECAF score is based on the assessment of five key clinical parameters, each represented by a specific point value:
Dyspnea: Assessed using British Medical Research Council (mMRC) dyspnea scale.
Eosinopenia: A point is added if the blood eosinophil level is below 0.05x10⁹/L.
Presence of Consolidation: A risk factor identified through clinical or radiological findings.
Acidosis: A pH < 7.30 on arterial blood gas analysis is considered a high-risk factor and is scored.
Atrial Fibrillation: The presence of atrial fibrillation is evaluated as an additional risk factor and scored.
The scores from each parameter were summed to calculate the total DECAF score. Based on the total score, patients were categorized into the following risk groups:
Low risk: 0-1 points
Moderate risk: 2 points
High risk: ≥3 points
2.3. Calculation of the A-DECAF Score
The A-DECAF score was developed by incorporating age as a factor into the original DECAF score. While the five core parameters of the DECAF score were preserved, age was added as an additional variable. In this modified system, 1 point is added to the score if the patient’s age is ≥65 years. With the integration of the age factor, the total A-DECAF score ranges from 0 to 6.
2.4. Statistical Analysis
The data collected in the study were analyzed using appropriate statistical methods to evaluate factors affecting survival. The normality of continuous variables was assessed using the Kolmogorov-Smirnov test. For variables with a normal distribution, the results were presented as mean ± standard deviation (Mean±SD), whereas for non-normally distributed variables, they were expressed as median (interquartile range). Categorical variables were reported as frequency and percentage (%).
For comparisons between groups, the Independent Samples t-test or Mann-Whitney U test was used for continuous variables, while the Chi-square test or Fisher’s Exact Test was applied for categorical variables. Survival analyses were conducted using the Kaplan-Meier method, and differences between groups were evaluated with the log-rank test. To assess the performance of APACHE-II, DECAF, and A-DECAF scores in predicting survival, Receiver Operating Characteristic (ROC) analysis was performed. The analysis provided values for the Area Under the Curve (AUC), cut-off points, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive/negative likelihood ratios (LR+/LR−). A significance level of p<0.05 was considered for all analyses, and statistical evaluations were performed using SPSS version 27.0.
3. Results
Initially, 558 patients were included in the study. However, 100 patients were excluded due to incomplete data. Additionally, 101 patients who no longer required NIMV during the follow-up period were also excluded. Consequently, the analyses were conducted on 357 patients. It was observed that 24.4% of the patients died within one year after discharge.
The results of the comparative analysis based on the survival status of the patients are presented in
Table 1. The mean age of deceased patients was statistically significantly higher compared to surviving patients (p<0.001). When evaluated in terms of scoring systems, the APACHE-II, DECAF, and A-DECAF scores of deceased patients were also found to be significantly higher (p<0.001;p<0.001;p<0.001).
The comparison of laboratory findings from blood tests based on the survival status of the patients is presented in
Table 2. According to arterial blood gas analysis, pH levels were found to be lower in deceased patients (p<0.001), while pCO2 levels were statistically significantly higher in deceased patients (p=0.003).
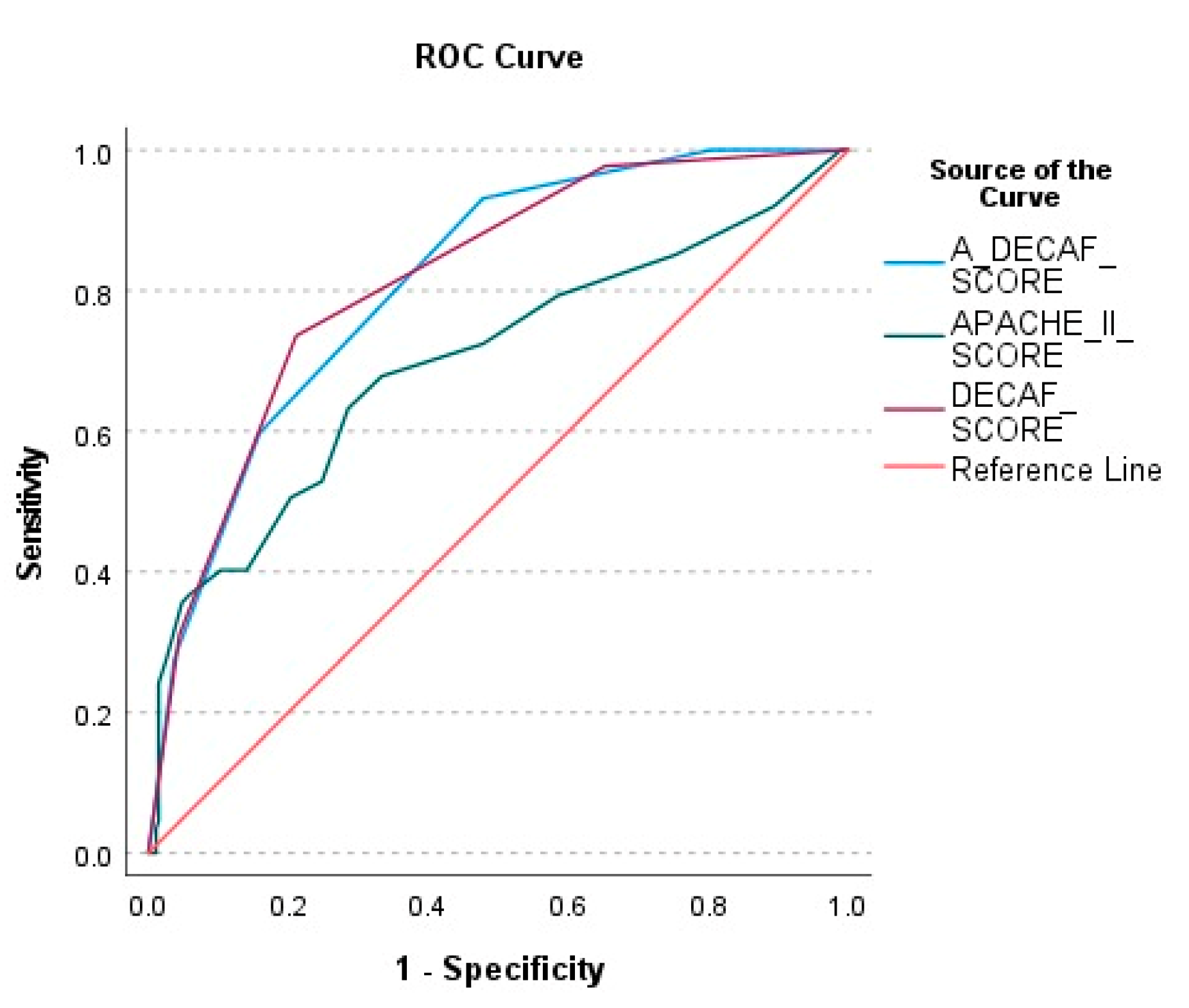
The performance of the A-DECAF, DECAF, and APACHE-II scores in predicting patient survival was evaluated using ROC analysis (
Figure 2). According to the ROC curve analysis, the A-DECAF score demonstrated the best performance in survival prediction, offering higher sensitivity and specificity compared to the other scores.
In the long-term survival analysis, age and the DECAF score were statistically shown to be significant prognostic factors for survival. To create a more effective prognostic model by combining these two strong variables, the A-DECAF score was developed. By integrating the individual effects of age and the DECAF score, the goal was to achieve greater accuracy in predicting long-term survival.
The performance of APACHE-II, DECAF, and A-DECAF scores in predicting survival was compared using ROC analysis and is presented in
Table 3. It was observed that the DECAF (AUC=0.816) and A-DECAF (AUC=0.813) scores provided higher accuracy compared to the APACHE-II score (AUC=0.699). The A-DECAF score demonstrated the highest sensitivity (93.1%) in determining survival.
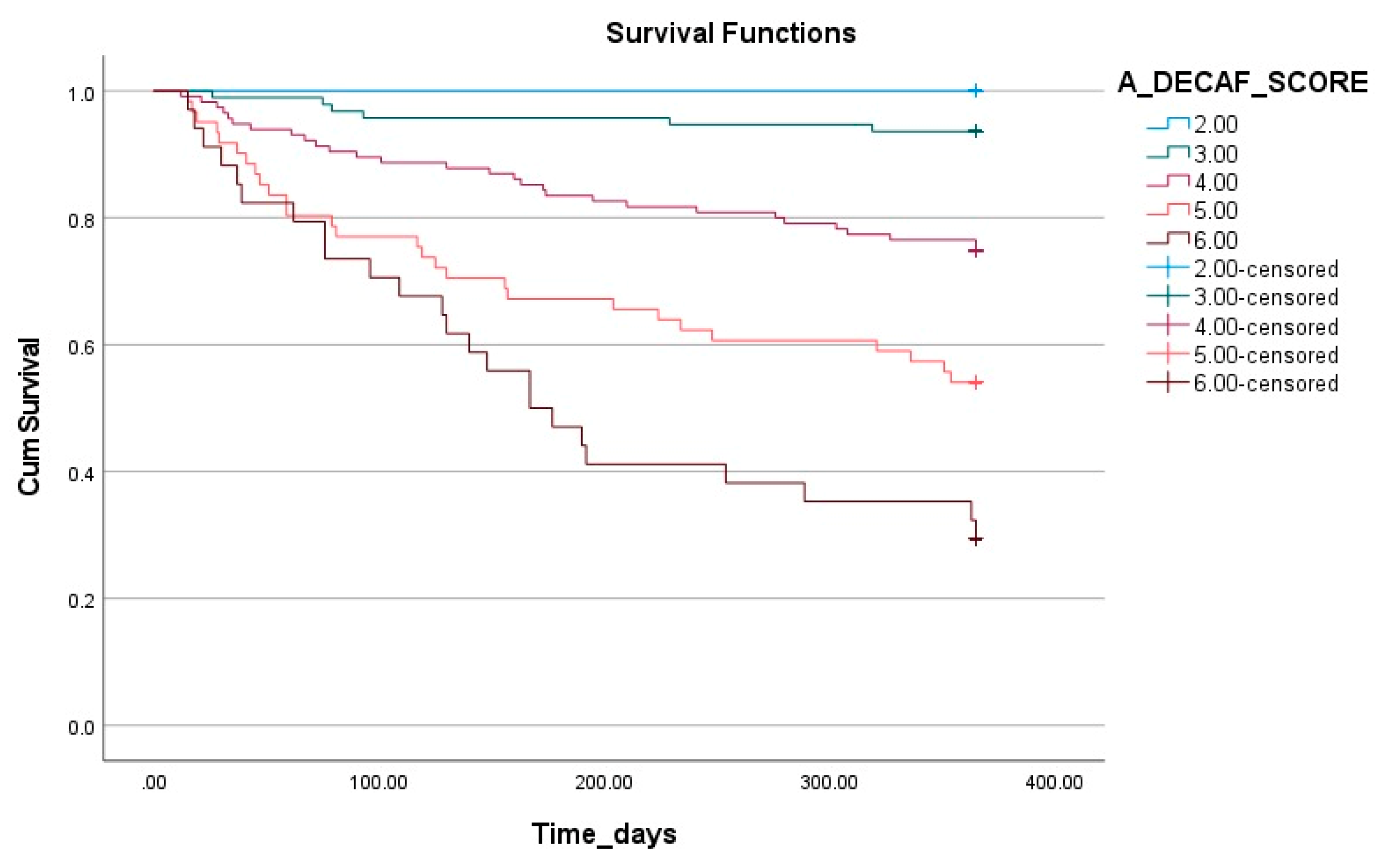
The impact of the A-DECAF score on survival is illustrated in
Figure 3 using Kaplan-Meier survival analysis. This analysis demonstrates that survival rates significantly decrease as the A-DECAF score increases. Patients with low scores had longer survival durations and higher survival rates, whereas those with high scores (particularly 5 and 6) showed a rapid decline in survival rates in the early period.
4. Discussion
This study aimed to evaluate prognostic factors affecting long-term survival in patients with HRF due to COPD who were followed in the ICU and to analyze the effectiveness of a new scoring system, the A-DECAF score. The findings of the study indicate that age, comorbidities, pH, pCO2, the need for invasive mechanical ventilation (IMV), APACHE-II, and DECAF scores have significant impacts on survival. Notably, the A-DECAF score stood out with the highest discriminatory power in survival prediction based on ROC analysis results. This suggests that the A-DECAF score, which combines the individual effects of age and the DECAF score, can serve as a more effective prognostic tool in clinical practice. The Kaplan-Meier analysis supports this finding, revealing that patients with lower A-DECAF scores have higher survival rates, while survival rates significantly decrease as the score increases. While this study highlights the prognostic power of the A-DECAF score, it also underscores the need for its validation in different patient populations and larger samples. Such validation studies could contribute to the acceptance of the A-DECAF score as a universal prognostic tool.
In recent years, advancements in critical care medicine have enabled not only the management of acute treatment processes but also the evaluation of long-term outcomes [
6]. In this context, post-ICU survival has emerged as a key metric for analyzing the long-term outcomes of chronic and critical illnesses [
7]. Although numerous studies in the literature focus on HRF-related mortality and the effects of NIMV applications, data on the long-term prognosis of this patient group remain limited. A recent study that thoroughly examined the underlying causes of HRF and their impact on survival reported a one-year survival rate of 81% [
8]. The same study emphasized that the underlying causes of HRF could significantly affect survival; patients with diagnoses such as neuromuscular diseases and congestive heart failure had the worst prognosis, whereas patients with HRF caused by factors such as opioid use showed the best outcomes. In our study, the one-year survival rate was calculated to be 75.6%. In our study, exclusion of etiological factors such as opioid use, which has a good prognosis and may cause HRF, may have contributed to the lower rate.
The aging population poses significant challenges for healthcare systems [
9]. This is reflected in the increasing admission rates of elderly patients to hospitals and ICUs [
10]. In a study conducted by Guillon et al. on patients aged ≥80 years, a significant increase in mortality was reported in this population following ICU admission [
11]. Similarly, in a study by Barisich et al. examining overall survival after ICU discharge, age was highlighted as an independent risk factor [
12]. In our study, age was also identified as a significant prognostic factor for long-term survival. This finding is associated with the negative impact of aging-related comorbidities and reduced physical reserves on the progression of critical illnesses, leading to lower survival rates. Therefore, age should be considered in clinical decision-making processes, and more tailored treatment and follow-up strategies should be developed for elderly individuals.
Comorbidities are known to have a significant impact on clinical course, complications, and patient outcomes in the ICU [
13]. In a large, multicenter observational study by Simpson et al., the effects of chronic conditions on ICU processes and long-term survival were clearly demonstrated [
14]. In our study, comorbidities were also found to have a significant impact on long-term survival. Cardiovascular diseases such as atrial fibrillation and lung cancer were identified at higher rates in deceased patients. This finding suggests that comorbidities not only negatively affect the clinical course of the illness but also limit physical reserves in critical situations, thereby reducing survival rates. Our study underscores the importance of effective management of chronic diseases and highlights the need for closer monitoring of patients with comorbidities.
The DECAF score was developed to predict disease severity and in-hospital mortality in AE-COPD [
15]. Patients with high DECAF scores may have increased ICU requirements and require closer monitoring [
16]. A recent study also indicated its association with readmissions within 90 days [
17]. Furthermore, a study conducted on AE-COPD patients monitored in the ICU demonstrated the superiority of the DECAF score over other scoring systems in predicting mortality [
18]. Considering this information, in this study, long-term survival was evaluated in patients followed up in the ICU with DECAF, AE-COPD and HRF. The findings showed that the DECAF score outperformed other scoring systems in predicting long-term survival in patients with AE-COPD. The DECAF score stands out as a reliable tool in determining not only short-term but also long-term prognosis, as it includes basic clinical parameters affecting mortality and survival. The ROC analysis performed in this study supported the accuracy of the DECAF score in predicting long-term survival and demonstrated that it provides higher prognostic accuracy compared to other commonly used systems. Additionally, the A-DECAF score, developed by incorporating the significant effect of age on prognosis, further enhanced the performance of the DECAF score. According to the analysis results, the A-DECAF score demonstrated the best performance in long-term survival prediction, achieving the highest sensitivity. Kaplan-Meier survival analysis clearly illustrated the impact of the A-DECAF score on survival rates, showing significantly lower survival rates in patients with high scores. These findings highlight that the A-DECAF score offers a significant advantage in clinical decision-making processes by improving prognostic accuracy, particularly in elderly patients.
The success of the A-DECAF score in predicting long-term survival stems from its ability to provide a more comprehensive assessment by incorporating age into the prognostic model. In elderly patients, the burden of comorbidities and diminished physiological reserves increases the risk of mortality during critical illness. Our study demonstrates that the A-DECAF score is a powerful tool for predicting survival rates, particularly in older patient populations. Additionally, it is believed that this scoring system could facilitate personalized approaches in patient management. However, further investigation into the validity of the A-DECAF score in different patient populations, along with comparative analyses with other scoring systems in larger-scale studies, is essential to strengthen its utility in clinical practice. Such studies could contribute not only to AE-COPD but also to the development of more effective treatment and monitoring strategies for patient groups experiencing HRF due to various underlying causes.
5. Limitations
Our study has some limitations. The retrospective design may pose challenges in ensuring the completeness of the data. Additionally, the fact that the research was conducted at a single center is a significant factor limiting the generalizability of the findings. The exclusion of factors associated with a favorable prognosis, such as opioid use, restricted the ability to fully evaluate their impact on survival rates. Furthermore, the lack of a detailed analysis regarding the severity of the included comorbidities made it difficult to fully assess their impact on long-term survival.
6. Conclusions
This study evaluated the prognostic factors affecting long-term survival in patients who developed HRF due to COPD. The findings revealed that age, comorbidities, pH, pCO₂, and the need for invasive mechanical ventilation significantly impact survival. The A-DECAF score, developed by incorporating age into the DECAF score, demonstrated superior performance among existing scoring systems by offering high sensitivity and accuracy in predicting long-term survival. The A-DECAF score emerges as an effective tool to guide clinical decision-making processes, particularly in elderly patients. While these results provide valuable insights for clinical practice, they also highlight the need for validating the A-DECAF score in different patient populations and larger cohorts.
Author Contributions
Conceptualization, M.A.; methodology, M.A.; software, E.A.; validation, E.A.; formal analysis, E.A.; investigation, M.A.; resources, M.A.; data curation, E.A.; writing—original draft preparation, M.A. and E.A.; writing—review and editing, M.A. and E.A.; visualization, M.A.; supervision, E.A. All authors have read and agreed to the published version of the manuscript.
Funding
No funding, grants, or other support was received for conducting this study.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical approval was obtained from the Clinical Research Ethics Committee of Ankara Ataturk Sanatorium Training and Research Hospital (decision date: December 25, 2024; approval number: 187).
Informed Consent Statement
Informed consent was not required due to the retrospective nature of the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
-
Vykopal M, Mizera J, Jakubec P, Genzor S, Pobeha P. Hypercapnic respiratory failure - review. Cas Lek Cesk. 2023, Cilt 162(1):13-18.
-
NR, MacIntyre. Acute Hypercapnic ResNR, MacIntyre. Acute Hypercapnic Respiratory Failure in COPD. Respir Care. 2023, Cilt 68(7):973-982.
-
Villgran VD, Lyons C, Nasrullah A et al. Acute Respiratory Failure. Crit Care Nurs Q. 2022, Cilt 01;45(3):233-247.
-
Candemir Ergene G, Doğan NÖ, Ergül T et al. Evaluating the prognostic value of DECAF score and procalcitonin in patients with COPD exacerbation. Am J Emerg Med. 2025, Cilt 6;90:23-30.
-
Chung E, Chung KS, Leem AY et al. Impact of age on mortality and transfer to long-term care in patients in an intensive care unit. BMC Geriatr. 2023, Cilt 12;23(1):839.
-
Rousseau AF, Prescott HC, Brett SJ et al. Long-term outcomes after critical illness: recent insights. Crit Care. 2021, Cilt 17;25(1):108.
-
Flaatten H, Jung C. Long-Term Outcomes After Critical Care: Another Brick in the Wall. Chest. 2021, Cilt 160(5):1587-1588.
-
Chung Y, Garden FL, Marks GB, Vedam H. Long-term cohort study of patients presenting with hypercapnic respiratory failure. BMJ Open Respir Res. 2024, Cilt 20;11(1):e002266.
-
United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019. Ten Key Findings. 2019.
-
Sjoding MW, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR. Longitudinal Changes in ICU Admissions Among Elderly Patients in the United States. Crit Care Med. 2016, Cilt 44(7):1353-60.
-
Guillon A, Hermetet C, Barker KA et al. Long-term survival of elderly patients after intensive care unit admission for acute respiratory infection: a population- based, propensity score-matched cohort study. Crit Care. 2020, Cilt 29;24(1):384.
-
Barisich PS, Ramírez-Santana M. One-year survival after admission in the intensive care unit: a retrospective cohort study. Rev Assoc Med Bras (1992). . 2024, Cilt 16;70(9):e20240463.
-
Ari M, Ozdemir T, Yildiz M et al. Factors Affecting the Length of Hospital Stay in Hypercapnic Respiratory Failure. Diagnostics (Basel). 2024, Cilt 25;15(1):14.
-
Simpson A, Puxty K, McLoone P et al. Comorbidity and survival after admission to the intensive care unit: A population-based study of 41,230 patients. J Intensive Care Soc. 2021, Cilt 22(2):143-151.
-
Echevarria C, Steer J, Heslop-Marshall K et al. Validation of the DECAF score to predict hospital mortality in acute exacerbations of COPD. Thorax. 2016, Cilt 71(2):133-40.
-
Hu X, Cai W, Xu D et al. Performance of the DECAF score in predicting hospital mortality due to acute exacerbations of COPD. Int J Tuberc Lung Dis. 2024 , Cilt 1;28(12):564-571.
-
Almarshoodi K, Echevarria C, Kassem A et al. An International Validation of the "DECAF Score" to Predict Disease Severity and Hospital Mortality in Acute Exacerbation of COPD in the UAE. Hosp Pharm. 2024, Cilt 59(2):234-240.
-
Jiang J, Yu X, Wang B, Ma L, Guan Y. DECAF: An interpretable deep cascading framework for ICU mortality prediction. Artif Intell Med. 2023, Cilt 138:102437.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).