Submitted:
02 January 2025
Posted:
04 January 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Mean Percentages of Routine Measles Vaccination Coverage in Regions of the WHO in 2023
2.2. Mean Vaccination Coverage with Zero, One and Two Doses of Measles Vaccine in the WHO Regions in 2023
2.3. Anti-Measles Herd Immunity Levels in the Target Vaccination Population in the WHO Regions in 2023
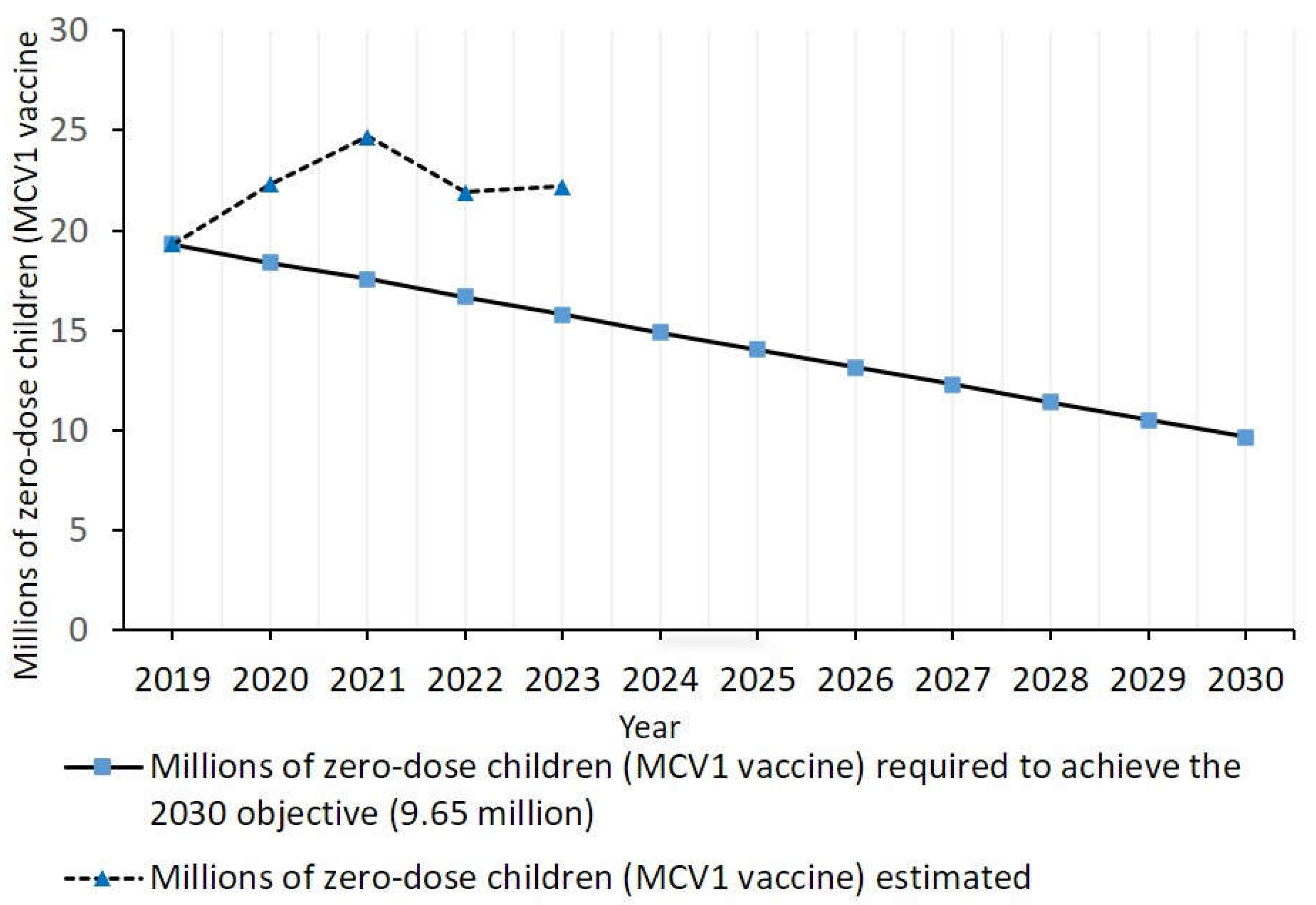
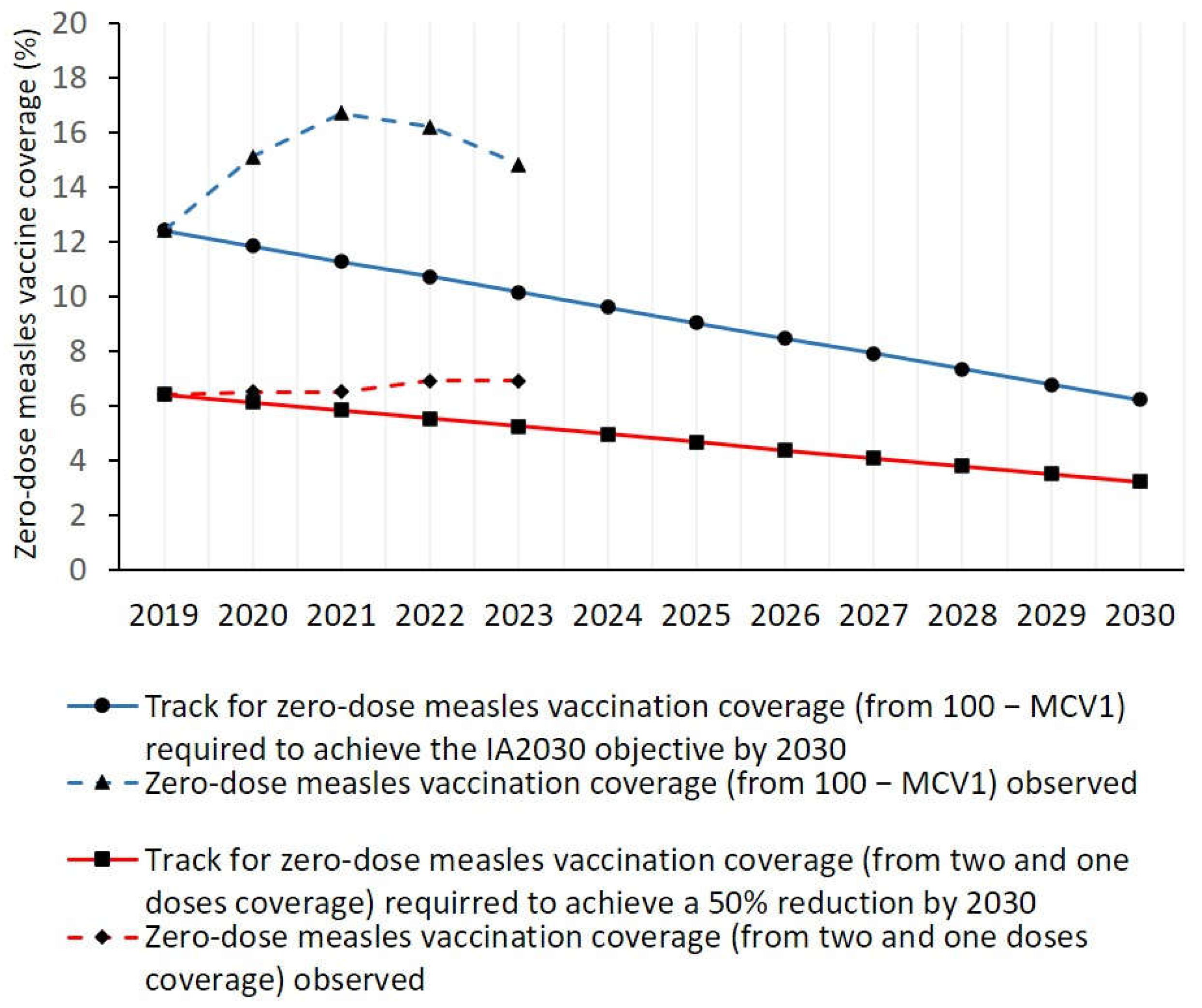
2.4. Assessment of Whether Zero-Dose Measles Vaccination Indicators in 2023 Were on Track to Achieve the Immunization Agenda 2030 Objective
2.5. Statistical Analysis
3. Results
3.1. Mean Percentages of Routine Measles Vaccination Coverage in Countries of the World and Regions of the WHO in 2023
3.2. Mean Percentages of Vaccination Coverage with Two, One and Zero Doses of Measles Vaccines in the World and Regions of the WHO in 2023
3.3. Anti-Measles Herd Immunity Levels in Countries of the World and Regions of the WHO in 2023
3.4. Variation for Routine Measles Vaccination-Related indicators in Countries of the World and Regions of the WHO from 2019 to 2023
3.5. Variation for Anti-Measles herd Immunity-Related Indicators in Countries of the World and Regions of the WHO from 2019 to 2023
3.6. Assessment of Whether Zero-Dose Measles Vaccination Indicators in 2023 Were on Track to Achieve the IA2030 Objective Reduction by 2030
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Global Vaccine Action Plan; WHO: Geneve, Switzerland, 2020. Available online: https://www.who.int/publications/i/item/global-vaccine-action-plan-2011-2020 (accessed on 15 October 2024).
- WHO/UNICEF. Immunization Agenda 2030. A global strategy to leave no one behind. 5389. Available online: https://cdn.who.int/media/docs/default-source/immunization/strategy/ia2030/ia2030-draft-4-wha_b8850379-1fce-4847-bfd1-5d2c9d9e32f8.pdf?sfvrsn=5389656e_69&download=true (accessed on 15 October 2024).
- World Health Organization (WHO). Global Vaccine Action Plan: Monitoring, Evaluation and Accountability; Secretariat Annual Report 2020; WHO: Geneve, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/global-vaccine-action-plan-monitoring-evaluationaccountability-secretariat-annual-report-2020.
- Minta, A.A.; Ferrari, M.; Antoni, S.; Portnoy, A.; Sbarra, A.; Lambert, B.; Hatcher, C.; Hsu, C.H.; Ho, L.L.; Steulet, C.; Gacic-Dobo, M.; Rota, P.A.; Mulders, M.N.; Bose, A.S.; Caro, W.P.; O’Connor, P.; Crowcroft, N.S. Progress Toward Measles Elimination - Worldwide, 2000-2022. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 1262–1268. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, P.; Masresha, B.; Pastor, D.; Musa, N.; Hagan, J.; Khanal, S.; Lee, C.-W.; Crowcroft, N. Global Status Report for the Verification of Measles and Rubella Elimination, 2022. Vaccines 2024, 12, 947. [Google Scholar] [CrossRef] [PubMed]
- WHO; Centralized Information System for Infectious Diseases (CISID). Measles-number of cases, 2015–2023. Available online: http://data.euro.who.int/cisid/?TabID=523870 (accessed on 7 October 2024).
- WHO; Centralized Information System for Infectious Diseases (CISID). Measles-Number of hospitalizations. 2023. Available online: http://data.euro.who.int/cisid/?TabID=523869 (accessed on 7 September 2024).
- WHO; Centralized Information System for Infectious Diseases (CISID). Measles-Number of deaths. 2023. Available online: http://data.euro.who.int/cisid/?TabID=523871 (accessed on 7 October 2024).
- World Health Organization (WHO). Strategic Plan. for Measles and Congenital Rubella Infection in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2003. [Google Scholar]
- Plans-Rubió, P. Vaccination Coverage for Routine Vaccines and Herd Immunity Levels against Measles and Pertussis in the World in 2019. Vaccines 2021, 9, 256. [Google Scholar] [CrossRef]
- Plans-Rubió, P. Are the Objectives Proposed by the WHO for Routine Measles Vaccination Coverage and Population Measles Immunity Sufficient to Achieve Measles Elimination from Europe? Vaccines 2020, 8, 218. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Strategic plan for measles and congenital rubella infection in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2003. Available online: https://iris.who.int/handle/10665/107526 (accessed on 7 October 2024).
- European Centre for Disease Prevention and Control (ECDC). Measles: Recommended Vaccination. Available online: https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=8&SelectedCountryIdByDisease=-1 (accessed on 2 December 2024).
- Vanderslott, S.; Dathui, S.; Spooner, F.; Roser, M. Our World in Data. Vaccination. Available online: https://ourworldindata.org/vaccination (accessed on 2 December 2024).
- Rosenthal SR, Clements CJ. Two-dose measles vaccination schedules. Bull. World Health Organ 1993, 71, 421–428.
- Gay, N.J. The theory of measles elimination: implications for the design of elimination strategies. J Infect Dis 2004, 189 (Suppl 1), S27. [Google Scholar]
- UNICEF. WHO/UNICEF Estimates of Routine Vaccination Coverage. 2023. Available online: https://data.unicef.org/topic/child-health/immunization/ (accessed on 9 September 2024).
- Burton, A.; Monasch, R.; Lautenbach, B.; Gacic-Dobo, M.; Maryanne, N.; Karimov, R.; Wolfson, L.; Jones, G.; Birmingham, M. WHO and UNICEF estimates of national infant immunization coverage: Methods and processes. Bull. World Health Organ. 2009, 87, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Demicheli, V.; Rivetti, A.; Debalini, M.G.; Di Pietrantonj, C. Vaccines for Measles, Mumps and Rubella in Children (Review). The Cochrane Library 2012, Issue 2. Available online: https://www.princeton.edu/~{}sswang/demicheli_pietrantonj12_cochrane_ report_MMR-risks.pdf (accessed on 22 July 2024).
- WHO-UNICEF. Progress and challenges with achieving universal immunization coverage. 9141. Available online: https://cdn.who.int/media/docs/default-source/immunization/wuenic-progress-and-challenges.pdf?sfvrsn=b5eb9141_12&download=true.
- Minta, A.A.; Ferrari, M.; Antoni, S.; Portnoy, A.; Sbarra, A.; Lambert, B.; Hauryski, S.; Hatcher, C.; Nedelec, Y.; Datta, D.; Ho, L.L.; Steulet, C.; Gacic-Dobo, M.; Rota, P.A.; Mulders, M.N.; Bose, A.S.; Perea, W.A.; O’Connor, P. Progress Toward Regional Measles Elimination - Worldwide, 2000-2021. MMWR Morb. Mortal. Wkly. Rep 2022, 71, 1489–1495. [Google Scholar] [CrossRef]
- Orenstein, W., A.; Cairns, L.; Hinman, A.; Nkowane, B.; Olivé, J.M.; Reingold, A.L. Measles and Rubella Global Strategic Plan 2012-2020 midterm review report: Background and summary. Vaccine 2018, 36 Suppl 1, A35–A42. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Measles vaccines: position paper − Aprl 2017. Wkly. Epidemiol. Rep. 2017, 92, 205–227. [Google Scholar]
- Winter, A.K.; Moss, W.J. Possible Paths to Measles Eradication: Conceptual Frameworks, Strategies, and Tactics. Vaccines 2024, 12, 814. [Google Scholar] [CrossRef]
- Plans, P. New preventive strategy to eliminate measles, mumps and rubella from Europe based on the serological assessment of herd immunity levels is the population. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 961–996. [Google Scholar] [CrossRef]
- Pavia, G.; Branda, F.; Ciccozzi, A.; Romano, C.; Locci, C.; Azzena, I.; Pascale, N.; Marascio, N.; Quirino, A.; Matera, G.; Giovanetti, M.; Casu, M.; Sanna, D.; Ceccarelli, G.; Ciccozzi, M.; Scarpa, F. Integrating digital health solutions with immunization strategies: Improving immunization coverage and monitoring in the post-COVID-19 era. Vaccines 2024, 12, 847. [Google Scholar] [CrossRef]
- Stockwell, M.S.; Fiks, A.G. Utilizing health information technology to improve vaccine communication and coverage. Hum. Vaccin. Immunother. 2013, 9, 1802–1811. [Google Scholar] [CrossRef] [PubMed]
- Rabil, M.J.; Tunc, S.; Bish, D.R.; Bish, E.K. Benefits of integrated screening and vaccination for infection control. PLoS One 2022, 17, e0267388. [Google Scholar] [CrossRef] [PubMed]
- Rachlin, A.; Hampton, L.M.; Rota, P.A.; Mulders, M.N.; Papania, M.; Goodson, J.L.; Krause, L.K.; Hanson, M.; Osborn, J.; Kelly-Cirino, C.; et al. Use of Measles and Rubella Rapid Diagnostic Tests to Improve Case Detection and Targeting of vaccinations. Vaccines 2024, 12, 823. [Google Scholar] [CrossRef] [PubMed]
- Mokdad, A.H.; Gagnier, M.C.; Colson, K.E.; Dansereau, E.; Zuniga-Brenes, P.; Rios-Zertuche, D.; Haakenstad, A.; Johanns, C.K.; Palmisano, E.B.; Hernandez, B.; et al. Missed opportunities for measles, mumps, and rubella (MMR) immunization in Mesoamerica: Potential impact on coverage and days at risk. PLoS ONE 2015, 10, e0139680. [Google Scholar] [CrossRef]
- Ropero Alvarez, A.M.; Jane Kurtis, H.; Vulanovic, L.; Hasan, H.; Ruiz, C.; Thrush, E. The evolution of Vaccination Week in the Americas. Rev. Panam. Salud Publica 2017, 41, e150. [Google Scholar] [CrossRef]
- Szilagyi, P.G.; Schaffer, S.; Shone, L.; Barth, R.; Humiston, S.G.; Sandler, M.; Rodewald, L.E. Reducing geographical, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics 2002, 110, e58. [Google Scholar] [CrossRef]
- Kaufman, J.; Rak, A.; Vasiliadis, S.; Brar, N.; Atif, E.; White, J.; Danchin, M.; Durrheim, D.N. The Case for Assessing the Drivers of Measles Vaccine Uptake. Vaccines 2024, 12, 692. [Google Scholar] [CrossRef]
- Higgins, D.M.; O’Leary, S.T. A World without Measles and Rubella: Addressing the Challenge of Vaccine Hesitancy. Vaccines 2024, 12, 694. [Google Scholar] [CrossRef] [PubMed]
- Wilder-Smith, A.B.; Qureshi, K. Resurgence of measles in Europe: A systematic review on parental attitudes and beliefs of measles vaccine. J. Epidemiol. Glob. Health 2020, 10, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control (CDC). National Immunization Awareness Month. Available online: https://www.cdc.gov/vaccines/events/niam/index.html (accessed on 3 November 2024).
- Poland CM, Ratishvili T. Vaccine hesitancy and health care providers: Using the preferred cognitive styles and decision- making model and empathy tool to make progress. Vaccine X 2022, 11, 100174. [CrossRef]
- Salmon, D.A.; Teret, S.P.; Macintyre, C.R.; Salisbury, D.; Burgess, M.A.; Halsey, N.A. Compulsory vaccination and conscientious or philosophical exemptions: Past, present, and future. Lancet 2006, 367, 436–442. [Google Scholar] [CrossRef]
- Haverkate, M.; D’Ancona, F.; Giambi, C.; Lopalco, P.L.; Cozza, V.; Appelgren, E. Mandatory and recommended vaccination in the EU, Iceland and Norway: Results of the VENICE 2010 survey on the ways of implementing national vaccination programmes. EuroSurveill. 2010, 17, p. 20183. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?Articleld=20183 (accessed on 29 November 2024).
- Pannuti, C.S.; Morello, R.J.; De Moraes, J.C.; Curti, S.P.; Afonso, A.M.S.; Camargo, M.C.C.; De Souza, V.A.U.F. Identification of primary and secondary measles vaccine failures by measurement of immunoglobulin G avidity in measles cases during the 1997 São Paulo Epidemic. Clin. Diagn. Lab. Immunol. 2004, 11, 119–122. [Google Scholar] [CrossRef]
- Danovaro-Holliday, M.C.; Koh, M.; Steulet, C.; Rhoda, D.A.; Trimner, M.K. Lessons from Recent Measles Post-Campaign Coverage Surveys Worldwide. Vaccines 2024, 12, 1257. [Google Scholar] [CrossRef] [PubMed]
- O’Leary ST, Opel DJ, Cataldi JR, Hackell JM; Committee on Infectious Diseases; Committee on Practice and Ambulatory Medicine; Committee on Bioethics. Strategies for Improving Vaccine Communication and Uptake. Pediatrics. 2024, 153, e2023065483. [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Catalogue of interventions addressing vaccine hesitancy; ECDC: Stockholm, Sweden, 2017. [Google Scholar]
- Crowcroft, N.S.; Minta, A.A.; Bolotin, S.; Cernuschi, T.; Ariyarajah, A.; Antoni, S.; Mulders, M.N.; Bose, A.S.; O’Connor, P.M. The Problem with Delaying Measles Elimination. Vaccines 2024, 12, 813. [Google Scholar] [CrossRef]
- WHO-UNICEF. WHO UNICEF immunization coverage estimates 2023 revision (released 15 July 2024). Available online: https://www.who.int/publications/m/item/WUENIC_notes (accessed on 29 November 2024).
- Guerra, F.; Bolotin, S.; Lim, G.; Heffernan, J.; Deeks, S.L.; Li, Y.; Crowcroft, N.S. The basic reproduction number (Ro) of measles: A systematic review. Lancet Infect. Dis. 2017, 17, e420–e428. [Google Scholar] [CrossRef] [PubMed]
| MCV1 vaccine 2023 |
MCV2 Vaccine 2023 |
MCV1 vaccine 2021 |
n | |
| % | % | % | ||
| World | 85.2 | 77.1 | 83.3 | 195 |
| African region (AFR) | 71.5 | 62.0 | 65.0 | 47 |
| Americas region (AMR) | 93.0 | 83.0 | 87.5 | 35 |
| Eastern Mediterranean region (EMR) | 91.5 | 86.5 | 80.0 | 22 |
| European region (EUR) | 90.5 | 92.5 | 93.0 | 53 |
| South East Asia region (SEAR) | 62.5 | 54.5 | 98.0 | 11 |
| Western Pacific region (WPR) | 97.0 | 95.5 | 97.5 | 27 |
| World | African region | Americas region | Eastern Mediterranean region |
European region | South-East Asia region | Western Pacific region |
|
|---|---|---|---|---|---|---|---|
| No. of countries | 195 | 47 | 35 | 22 | 53 | 11 | 27 |
| Routine measles vaccination-related indicators | |||||||
| Mean vaccination coverage (%) with two, one and zero doses of measles vaccine | |||||||
| 2 doses | 65.3 | 48.1 | 72.5 | 69.1 | 86.0 | 53.0 | 93.2 |
| 1 dose | 27.8 | 30.7 | 25.5 | 28.2 | 13.5 | 46.5 | 6.7 |
| 0 doses | 6.9 | 21.1 | 2.0 | 2.6 | 0.5 | 0.5 | 0.2 |
| Percentage of countries with two-dose measles vaccination coverage ≥ 95% and ≥ 90% | |||||||
| ≥ 95% | 8.7 | 0 | 2.9 | 22.7 | 9.4 | 18.2 | 14.8 |
| ≥ 90% | 21.0 | 0 | 8.6 | 40.9 | 30.2 | 36.4 | 33.3 |
| Percentage of countries where all children had received one or two doses of measles vaccine (0% of zero-dose children) | |||||||
| 9.7 | 0 | 5.7 | 22.7 | 9.4 | 18.2 | 18.5 | |
| Anti-measles herd immunity-related indicators | |||||||
| Mean prevalence (%) of individuals in the target vaccination population with vaccine-induced measles immunity | |||||||
| Measles immunity | 87.6 | 74.0 | 92.3 | 91.6 | 94.1 | 93.1 | 94.6 |
| Percentage of countries with herd immunity against measles viruses with Ro from 10 to ≥ 20 | |||||||
| Ro ≤ 10 | 66.1 | 40.4 | 62.9 | 68.2 | 92.4 | 72.7 | 59.3 |
| Ro ≤ 12 | 59.0 | 27.6 | 54.3 | 59.1 | 88.7 | 63.6 | 59.3 |
| Ro ≤ 15 | 41.5 | 10.6 | 25.7 | 50.0 | 66.0 | 63.6 | 51.8 |
| Ro ≤ 18 | 23.1 | 0 | 8.6 | 45.4 | 35.8 | 36.4 | 33.3 |
| Ro ≤ 19 | 0 | 0 | 5.7 | 31.8 | 13.2 | 27.3 | 22.2 |
| Ro ≥ 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| World | African region | Americas region | Eastern Mediterranean region |
European region | South-East Asia region | Western Pacific region |
|
|---|---|---|---|---|---|---|---|
| No. of countries | 195 | 47 | 35 | 22 | 53 | 11 | 27 |
| Routine measles vaccination-related indicators | |||||||
| Mean vaccination coverage (%) with two. one and zero doses of measles vaccine | |||||||
| 2 doses | -3.7 | 24.0 | -1.0 | -3.2 | 2.5 | -35.0 | 30.9 |
| 1 dose | 7.8 | -30.7 | 5.8 | 27.6 | -11.2 | 171.9 | -71.0 |
| 0 doses | 7.8 | 24.9 | -25.9 | -60.0 | -44.4 | -64.3 | -96.5 |
| Percentage of countries with two-dose measles vaccination coverage ≥ 95% and ≥ 90% | |||||||
| ≥ 95% | -39.6 | -100.0 | -79.7 | -4.6 | -37.7 | -33.3 | -33.3 |
| ≥ 90% | -18.6 | -100.0 | -62.4 | 7.3 | -15.6 | 0.0 | -10.0 |
| Percentage of countries where all children had received one or two doses of measles vaccine (0% of zero-dose children) | |||||||
| -24.8 | -100.0 | -60.1 | -20.6 | 0.0 | -33.3 | 0.0 | |
| Anti-measles herd immunity-related indicators | |||||||
| Mean prevalence (%) of individuals in the target vaccination population with vaccine-induced measles immunity | |||||||
| Measles immunity | -0.6 | -4.6 | 0.5 | 3.9 | 0.4 | -0.1 | 6.5 |
| Percentage of countries with herd immunity against measles viruses with Ro from 10 to ≥ 20 | |||||||
| Ro ≤ 10 | -6.4 | 0.0 | -15.3 | 2.2 | -2.0 | -11.1 | -15.8 |
| Ro ≤ 12 | -7.7 | -7.4 | -17.4 | -4.5 | -2.1 | -12.5 | -11.1 |
| Ro ≤ 15 | -19.4 | -28.9 | -43.8 | -4.6 | -18.6 | 16.7 | -17.8 |
| Ro ≤ 18 | -28.9 | -100.0 | -62.4 | 19.2 | -13.7 | -33.2 | -18.2 |
| Ro ≤ 19 | -100.0 | -100.0 | -66.7 | 11.2 | -22.4 | 0.0 | 0.0 |
| Ro ≥ 20 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





