Submitted:
30 December 2024
Posted:
30 December 2024
You are already at the latest version
Abstract
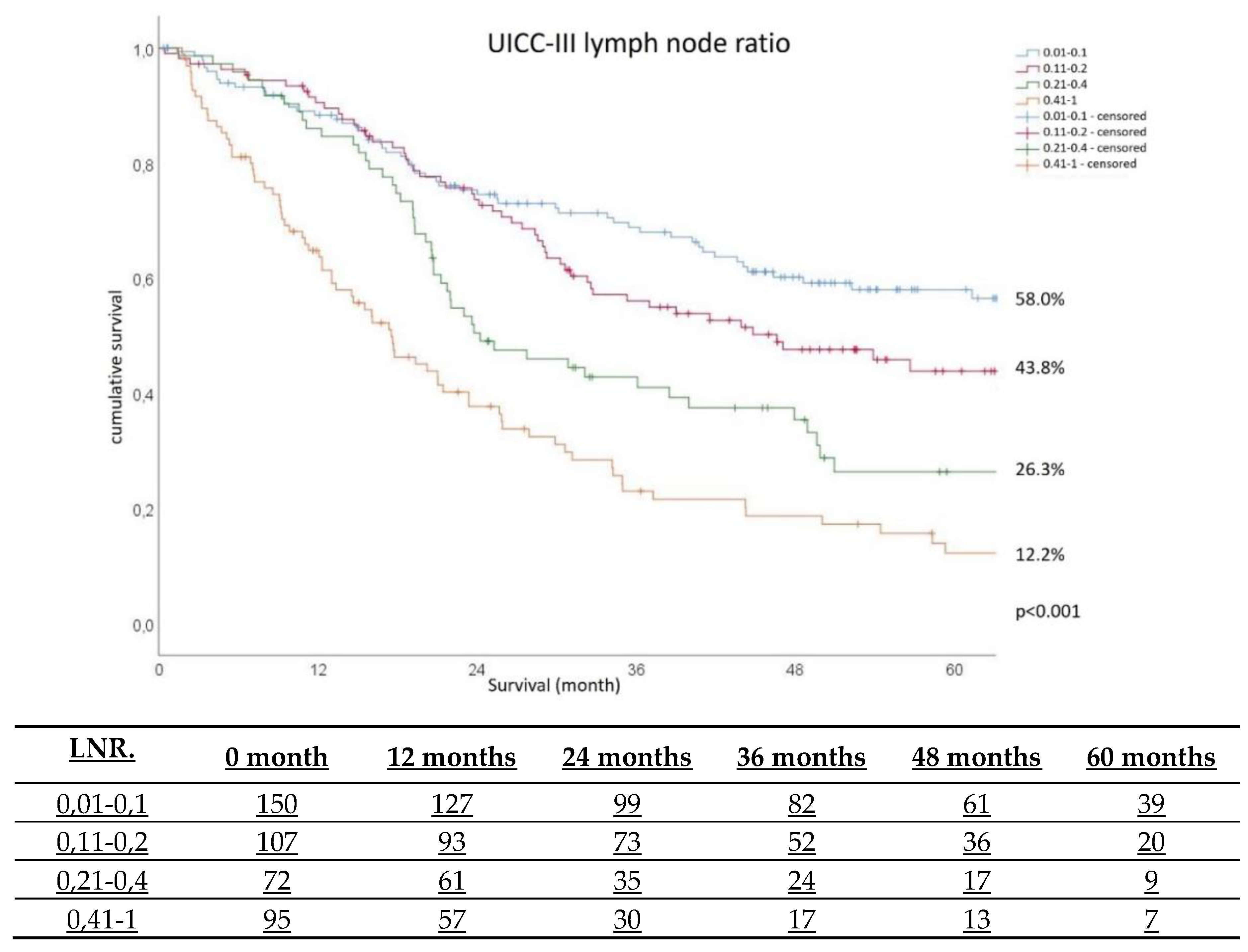
Background: Lymphadenectomy is fundamental part of surgical strategy in patients with gastric cancer. Lymph node (LN) status is a key point in assessment of prognosis in gastric cancer. The LN ratio (LNR) - number of positive LNs / number of sampled LNs, offers a new approach for predicting survival. The aim of the study was to find factors affecting LN yield and the impact of LNR on 5-year survival. Methods: Prospective multicentre quality assurance study. Only LN-positive patients were included in the LNR calculations. Results: 4946 patients from 149 hospitals were enrolled. The inclusion criteria were met by 1884 patients. Patients were divided into two groups: Group 1 (<16 LN) 456 patients and Group 2 (≥16 LN) 1428 patients. The multivariate analysis found G2 (OR 1.98; 95%CI 1.11-3.54), G3 (OR 2.15; 95%CI 1.212-3.829), UICC-stage II (OR 1.44; 95%CI 1.01-2.06) and III (OR 1.71; 95%CI 1.14-2.57), age <70 (OR 1.818 95%CI 1.19-2.78) and female gender ( OR 1.37; 95%CI 1.00-1.86) as independent factors of ≥16 LN yield. Patients with a LNR≥0.4 have a lower probability of survival (p=0.039 and <0.001) than patients with LNR=0.1. Patients with UICC-II have a lower probability of survival than UICC-I (p=0.023). Age 70-80 (p=0.045) and >80 years (p=0.003) were negative prognostic factors for long-term survival. Conclusion: Long-term survival is directly related to adequate lymphadenectomy. LNR could be superior to pN-stage for estimating survival, and adds remarkable nuances in prognosis compared to UICC-stage. LNR also appears valid, even in the case of insufficient LN yield.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients and Data Collection
2.2. Statistical Analysis
3. Results
3.1. Lymph Node Yield Analysis
3.2. Long Term Survival Analyses
4. Discussion
4.1. Lymph Node Yield
4.2. Lymph Node Ratio
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LNR | Lymph Node Ratio |
| TNM | Tumor Nodes Metastasis |
| LN | Lymph Node |
| BMI | Body Mass Index |
| UICC | Union for International Cancer Control |
| AJCC | American Joint Committee on Cancer |
| ASA | American Society of Anaesthesiology |
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Robert-Koch-Institute. Centre for Cancer Registry Data. 2020. Available online: www.rki.de/EN/Content/Health_Monitoring/Cancer_Registry/cancer_registry_node.html (accessed on 10 December 2023).
- Japanese Gastric Cancer Association. Japanese Gastric Cancer treatment Guidelines 2021 (6th edition). Gastric Cancer 2023, 26, 1–25. [Google Scholar] [CrossRef]
- Coburn, N.; Cosby, R.; Klein, L.; Knight, G.; Malthaner, R.; Mamazza, J.; Mercer, C.D.; Ringash, J. Staging and Surgical Approaches in Gastric Cancer: A Clinical Practice Guideline. Curr. Oncol. 2017, 24, 324–331. [Google Scholar] [CrossRef]
- Wu, W.; Dong, P.; Wu, X.; Li, M.; Ding, Q.; Zhang, L.; Yang, J.; Weng, H.; Ding, Q.; Tan, Z.; et al. Three-step method for systematic lymphadenectomy in gastric cancer surgery using the ‘curettage and aspiration dissection technique’ with Peng’s multifunctional operative dissector. World J. Surg. Oncol. 2014, 12, 322–322. [Google Scholar] [CrossRef]
- Lordick F, Al-Batran SE, Arnold D, Borner M, Bruns CJ, Eisterer W, Faber G, Gockel I, Köberle D, Lorenzen S, Möhler M, Pritzkuleit R, Stahl M, Thuss-Patience P, Wöll E, Zander T, In Kooperation mit der AIO. Onkopedia Leitlinen – Magenkarzinom 2023. Accessed at www.onkopedia.com/de/onkopedia/guidelines/magenkarzinom/, 2023-12-10.
- Yu, J.; Yang, D.; Wei, F.; Sui, Y.; Li, H.; Shao, F.; Li, Y. The staging system of metastatic lymph node ratio in gastric cancer. Hepatogastroenterology 2009, 55, 2287–90. [Google Scholar] [CrossRef]
- Lu, J.; Huang, C.-M.; Zheng, C.-H.; Li, P.; Xie, J.-W.; Wang, J.-B.; Lin, J.-X. Consideration of tumor size improves the accuracy of TNM predictions in patients with gastric cancer after curative gastrectomy. Surg Oncol. 2013, 22, 167–171. [Google Scholar] [CrossRef]
- Wang, W.; Li, Y.-F.; Sun, X.-W.; Chen, Y.-B.; Li, W.; Xu, D.-Z.; Guan, X.-X.; Huang, C.-Y.; Zhan, Y.-Q.; Zhou, Z.-W. Prognosis of 980 patients with gastric cancer after surgical resection. Chin. J. Cancer 2010, 29, 923–930. [Google Scholar] [CrossRef]
- Díaz Del Arco, C.; Ortega Medina, L.; Estrada Muñoz, L.; García Gómez de Las Heras, L.; Fernández Aceñero, M.J. Pathologic Lymph Node Staging of Gastric Cancer. Am J Clin Pathol. 2021, 156, 749–765. [Google Scholar] [CrossRef]
- Lee, S.R.; Kim, H.O.; Son, B.H.; Shin, J.H.; Yoo, C.H. Prognostic significance of the metastatic lymph node ratio in patients with gastric cancer. World J Surg. 2012, 36, 1096–101. [Google Scholar] [CrossRef]
- ALa-teng, B.L.; Li, Y.M.; Liu, C.G.; Wang, B.B.; Xu, H.M.; Chen, J.Q.; Wang, S.B.; Lu, P. Prognostic value of metastatic lymph node ratio in gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 2012, 15, 137–40. [Google Scholar]
- Chen, J.-X.; Sun, J.-W.; Wang, Y.; Pan, T.; Zhuang, L.-P.; Lin, L.-Z.; Lv, B.-C. Lymph node ratio-based the ypTNrM staging system for gastric cancer after neoadjuvant therapy: a large population-based study. Surg. Today 2021, 52, 783–794. [Google Scholar] [CrossRef]
- Karaca, C.A.; Coker, A. Prognostic Value of Metastatic Lymph Node Ratio in Pancreatic Cancer. Indian J. Surg. Oncol. 2018, 10, 50–54. [Google Scholar] [CrossRef]
- Mroczkowski, P.; Kim, S.; Otto, R.; Lippert, H.; Zajdel, R.; Zajdel, K.; Merecz-Sadowska, A. Prognostic Value of Metastatic Lymph Node Ratio and Identification of Factors Influencing the Lymph Node Yield in Patients Undergoing Curative Colon Cancer Resection. Cancers 2024, 16, 218. [Google Scholar] [CrossRef]
- German Cancer Society, German Cancer Aid, AWMF. Guideline programme on oncology: S3-Leitlinie Diagnostik und Therapie der Adenokarzinome des Magens und ösophagogastralen Übergangs (Version 2, 2019); AWMF Register Number: 032/009OL. Accessed at www.leitlinienprogramm-onkologie.de/leitlinien/magenkarzinom/, 2023-12-10.
- Ema, A.; Yamashita, K.; Sakuramoto, S.; Wang, G.; Mieno, H.; Nemoto, M.; Shibata, T.; Katada, N.; Kikuchi, S.; Watanabe, M. Lymph node ratio is a critical prognostic predictor in gastric cancer treated with S-1 chemotherapy. Gastric Cancer 2013, 17, 67–75. [Google Scholar] [CrossRef]
- Melis, M.; Masi, A.; Pinna, A.; Cohen, S.; Hatzaras, I.; Berman, R.; Pachter, L.H.; Newman, E. Does lymph node ratio affect prognosis in gastroesophageal cancer? Am J Surg. 2015, 210, 443–50. [Google Scholar] [CrossRef]
- Spychała, A.; Nowaczyk, P.; Murawa, D. Comparison of Lymphatic System Staging Classifications in Patients with Gastric Cancer. Pol. J. Surg. 2015, 87. [Google Scholar] [CrossRef] [PubMed]
- Kutlu, O.C.; Watchell, M.; Dissanaike, S. Metastatic lymph node ratio successfully predicts prognosis in western gastric cancer patients. Surg. Oncol. 2015, 24, 84–88. [Google Scholar] [CrossRef]
- Wu, X.-J.; Miao, R.-L.; Li, Z.-Y.; Bu, Z.-D.; Zhang, L.-H.; Wu, A.-W.; Zong, X.-L.; Li, S.-X.; Shan, F.; Ji, X.; et al. Prognostic value of metastatic lymph node ratio as an additional tool to the TNM stage system in gastric cancer. Eur J Surg Oncol. 2015, 41, 927–933. [Google Scholar] [CrossRef]
- Huang, C.-M.; Lin, J.-X.; Zheng, C.-H.; Li, P.; Xie, J.-W.; Lin, B.-J.; Wang, J.-B. Prognostic impact of metastatic lymph node ratio on gastric cancer after curative distal gastrectomy. World J. Gastroenterol. 2010, 16, 2055–2060. [Google Scholar] [CrossRef]
- Jiao, X.G.; Deng, J.Y.; Zhang, R.P.; Wu, L.L.; Wang, L.; Liu, H.G.; Hao, X.S.; Liang, H. Prognostic value of number of examined lymph nodes in patients with node-negative gastric cancer. World J Gastroenterol. 2014, 20, 3640–8. [Google Scholar] [CrossRef]
- Son, T.; Hyung, W.J.; Lee, J.H.; Kim, Y.M.; Kim, H.; An, J.Y.; Cheong, J.; Noh, S.H. Clinical implication of an insufficient number of examined lymph nodes after curative resection for gastric cancer. Cancer 2012, 118, 4687–4693. [Google Scholar] [CrossRef]
- Chen, C.Q.; Wu, X.J.; Yu, Z.; Bu, Z.D.; Zuo, K.Q.; Li, Z.Y.; Ji, J.F. Prognosis of patients with gastric cancer and solitary lymph node metastasis. World J Gastroenterol. 2013, 19, 8611–8. [Google Scholar] [CrossRef] [PubMed]
- Setälä, L.; Kosma, V.-M.; Marin, S.; Lipponen, P.; Eskelinen, M.; Syrjänen, K.; Alhava, E. Prognostic factors in gastric cancer: the value of vascular invasion, mitotic rate and lymphoplasmacytic infiltration. Br. J. Cancer 1996, 74, 766–772. [Google Scholar] [CrossRef]
- Liang, Y.X.; Deng, J.Y.; Guo, H.H.; Ding, X.W.; Wang, X.N.; Wang, B.G.; Zhang, L.; Liang, H. Characteristics and prognosis of gastric cancer in patients aged ≥ 70 years. World J Gastroenterol. 2013, 19, 6568–78. [Google Scholar] [CrossRef]
- Mayol-Oltra, A.; Martí-Obiol, R.; López-Mozos, F.; Báguena-Requena, G.; Ortega-Serrano, J. The influence of advanced age on the morbi-mortality of gastric cancer after curative surgery. Rev. espanola de enfermedades Dig. 2013, 105, 194–200. [Google Scholar] [CrossRef]
- Eom, B.W.; Jung, K.-W.; Won, Y.-J.; Yang, H.; Kim, Y.-W. Trends in Gastric Cancer Incidence According to the Clinicopathological Characteristics in Korea, 1999-2014. Cancer Res. Treat. 2018, 50, 1343–1350. [Google Scholar] [CrossRef]
- Li, Z.; Li, S.; Bu, Z.; Zhang, L.; Wu, X.; Shan, F.; Jia, Y.; Ji, X.; Ji, J. The effect of preoperative treatments on lymph node counts after total gastrectomy in esophagogastric adenocarcinoma. J. Surg. Oncol. 2018, 118, 657–663. [Google Scholar] [CrossRef]
- Zhang, Z.-X.; Gu, X.-Z.; Yin, W.-B.; Huang, G.-J.; Zhang, D.-W.; Zhang, R.-G. Randomized clinical trial on the combination of preoperative irradiation and surgery in the treatment of adenocarcinoma of gastric cardia (AGC) — report on 370 patients. Int. J. Radiat. Oncol. 1998, 42, 929–934. [Google Scholar] [CrossRef]
- Tsuburaya, A.; Mizusawa, J.; Tanaka, Y.; Fukushima, N.; Nashimoto, A.; Sasako, M. Neoadjuvant chemotherapy with S-1 and cisplatin followed by D2 gastrectomy with para-aortic lymph node dissection for gastric cancer with extensive lymph node metastasis. Br. J. Surg. 2014, 101, 653–660. [Google Scholar] [CrossRef]
- Zhao, L.-Y.; Li, C.-C.; Jia, L.-Y.; Chen, X.-L.; Zhang, W.-H.; Chen, X.-Z.; Yang, K.; Liu, K.; Wang, Y.-G.; Xue, L.; et al. Superiority of lymph node ratio-based staging system for prognostic prediction in 2575 patients with gastric cancer: validation analysis in a large single center. Oncotarget 2016, 7, 51069–51081. [Google Scholar] [CrossRef]
- Akar, E.; Tural, D.; Selçukbiricik, F.; Serdengeçti, S.; Büyükünal, E. Gastric cancer: A case study in Turkey. J. Cancer Res. Ther. 2013, 9, 644–648. [Google Scholar] [CrossRef]
- Wong, J.; Rahman, S.; Saeed, N.; Lin, H.-Y.; Almhanna, K.; Shridhar, R.; Hoffe, S.; Meredith, K.L. Prognostic Impact of Lymph Node Retrieval and Ratio in Gastric Cancer: a U.S. Single Center Experience. J. Gastrointest. Surg. 2013, 17, 2059–2066. [Google Scholar] [CrossRef] [PubMed]
- Jian-Hui, C.; Shi-Rong, C.; Hui, W.; Si-Le, C.; Jian-Bo, X.; Er-Tao, Z.; Chuang-Qi, C.; Yu-Long, H. Prognostic value of three different lymph node staging systems in the survival of patients with gastric cancer following D2 lymphadenectomy. Tumor Biol. 2016, 37, 11105–11113. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Xue, Z.; Zhang, S.; Guo, X.; Zhai, L.; Shang, S.; Zhang, Y.; Lu, H. Integrated analysis of the prognostic role of the lymph node ratio in node-positive gastric cancer: A meta-analysis. Int J Surg. 2018, 57, 76–83. [Google Scholar] [CrossRef]
- Chen, S.; Rao, H.; Liu, J.; Geng, Q.; Guo, J.; Kong, P.; Li, S.; Liu, X.; Sun, X.; Zhan, Y.; et al. Lymph nodes ratio based nomogram predicts survival of resectable gastric cancer regardless of the number of examined lymph nodes. Oncotarget 2017, 8, 45585–45596. [Google Scholar] [CrossRef] [PubMed]
- Topcu, R.; Şahiner, I.T.; Kendirci, M.; Erkent, M.; Sezikli, I.; Tutan, M.B. Does lymph node ratio (metastasis/total lymph node count) affect survival and prognosis in gastric cancer? Saudi Med J. 2022, 43, 139–145. [Google Scholar] [CrossRef]
- Huang, Z.; Chen, Y.; Zhang, W.; Liu, H.; Wang, Z.; Zhang, Y. Modified Gastric Cancer AJCC Staging with a Classification Based on the Ratio of Regional Lymph Node Involvement: A Population-Based Cohort Study. Ann. Surg. Oncol. 2019, 27, 1480–1487. [Google Scholar] [CrossRef]
- Zhang, Y.; Tian, S. Does D2 plus Para-Aortic Nodal Dissection surgery offer a better survival outcome compared to D2 surgery only for gastric cancer consistently? A definite result based on a hospital population of nearly two decades. Scand. J. Surg. 2013, 102, 251–257. [Google Scholar] [CrossRef]
- Deng, J.; Zhang, R.; Wu, L.; Zhang, L.; Wang, X.; Liu, Y.; Hao, X.; Liang, H. Superiority of the Ratio Between Negative and Positive Lymph Nodes for Predicting the Prognosis for Patients With Gastric Cancer. Ann. Surg. Oncol. 2014, 22, 1258–1266. [Google Scholar] [CrossRef]
| Group 1 (n/%) | Group 2 (n/%) | p-value* | ||
|---|---|---|---|---|
| Sex | Male | 213 / 68.6 | 868 / 60.9 | <0.001 |
| Female | 143 / 31.4 | 557 / 39.1 | ||
| ASA-classification | ASA I | 23 / 5.1 | 121 / 8.6 | < 0.001 |
| ASA II | 199 / 44.3 | 767 / 54.5 | ||
| ASA III | 214 / 47.7 | 495 / 35.2 | ||
| ASA IV | 13 / 2.9 | 24 / 1.7 | ||
| Grading | G1 | 39 / 8.6 | 59 / 4.1 | < 0.001 |
| G2 | 159 / 34.9 | 429 / 30.2 | ||
| G3 | 228 / 50.1 | 836 / 58.8 | ||
| G4 | 14 / 3.1 | 27 / 1,9 | ||
| Surgical approach | Laparotomy | 430 / 95.2 | 1411 / 99.1 | < 0.001 |
| Laparoscopic | 18 / 4.0 | 7 / 0.5 | ||
| Neoadjuvant treatment | No | 363 / 80.3 | 1054 / 74.3 | 0.009 |
| Yes | 89 / 19.7 | 365 / 25.7 | ||
| Localisation | gastroesophageal junction | 125 / 27.4 | 280 / 19.6 | < 0.001 |
| Fundus | 19 / 4.2 | 45 / 3.2 | 0.297 | |
| Corpus | 142 / 31.1 | 553 / 38.7 | 0.003 | |
| antral/pyloric region | 181 / 39.7 | 601 / 41.5 | 0.366 | |
| Invasion depth | pT0 | 0 / 0.0 | 2 / 0.1 | < 0.001 |
| pT1 | 200 / 44.0 | 460 / 32.3 | ||
| pT2 | 88 / 25.1 | 262 / 18.4 | ||
| pT3 | 167 / 36.7 | 699 / 49.1 | ||
| pN-stage | pN0 | 288 / 63.6 | 756 / 53.0 | < 0.001 |
| pN1 | 81 / 17.9 | 239 / 16.8 | ||
| pN2 | 52 / 11.5 | 203 / 14.2 | ||
| pN3 | 32 / 7.1 | 228 / 16.0 | ||
| UICC-stage | I | 249 / 54.6 | 578 / 40.5 | < 0.001 |
| II | 117 / 25.7 | 427 / 30.6 | ||
| III | 90 / 19.7 | 413 / 28.9 |
| LK-Quotient (mean±SD) | p-value | ||
|---|---|---|---|
| Sex | male | 0.11 ± 0.19 | 0.132** |
| female | 0.10 ± 019 | ||
| Age groups <70,70-80, >80 | <70 | 0.11 ± 0.19 | 0.213* |
| 70-80 | 0.11 ± 0.19 | ||
| >80 | 0.12 ± 0.21 | ||
| BMI | <18.5 | 0.15 ± 0.23 | 0.682* |
| 18.5 – 24.9 | 0.11 ± 0.20 | ||
| ≥ 25 | 0.10 ± 0.18 | ||
| Lauren classification | none | 0.11 ± 0.18 | <0.001* |
| intestinal | 0.08 ± 0.16 | ||
| diffues | 0.14 ± 0.23 | ||
| mixed | 0.10 ± 0.17 | ||
| Localisation | fundus | 0,12 ± 0.20 | 0.889** |
| gastroesophageal junction | 0.14 ± 0.20 | <0.001** | |
| corpus | 0.11 ± 0.20 | 0.923** | |
| antrum/pylorum | 0.10 ± 0.20 | 0.030** | |
| ASA-classification | I | 0.10 ± 0.19 | 0.440* |
| II | 0.11 ± 0.20 | ||
| III | 0.11 ± 0.19 | ||
| IV | 0.05 ± 0.10 | ||
| Neoadjuvant treatment | No | 0.10 ± 0.19 | <0.001** |
| yes | 0.12 ± 0.19 | ||
| Surgical approach | laparotomy | 0.11 ± 0.19 | 0.548** |
| laparoscopic | 0.07 ± 0.12 | ||
| Grading | G1 | 0.01 ± 0.07 | <0.001* |
| G2 | 0.08 ± 0.16 | ||
| G3 | 0.13 ± 0.21 | ||
| G4 | 0.11 ± 0.18 | ||
| pT-stage | pT0 | 0.06 ± 0.08 | <0.001* |
| pT1 | 0.02 ± 0.08 | ||
| pT2 | 0.08 ±0.15 | ||
| pT3 | 0.17 ± 0.23 | ||
| pN-stage | pN0 | 0.01 ± 0.03 | <0.001* |
| pN1 | 0.06 ± 0.05 | ||
| pN2 | 0.15 ± 0.07 | ||
| pN3 | 0.47 ± 0.22 | ||
| Lymphinvasion | L0 | 0.03 ± 0.09 | <0.001** |
| L1 | 0.20 ± 0.23 | ||
| Venous invasion | V0 | 0,09 ± 0,17 | <0.001** |
| V1 | 0,24 ± 0,27 | ||
| UICC-stage | I | 0.003 ± 0.01 | <0.001* |
| II | 0.05 ± 0.10 | ||
| III | 0.31 ± 0.24 |
| Odds ratio (95% CI) | p-value | ||
|---|---|---|---|
| Grading | G1 | 1 | |
| G2 | 1.982 (1.110-3.541) | 0.021 | |
| G3 | 2.154 (1.212-3.829) | 0.009 | |
| G4 | 0.739 (0.268-2.036) | 0.558 | |
| UICC-stage | I | 1 | |
| II | 1.441 (1.008-2.060) | 0.045 | |
| III | 1.707 (1.135-2.568) | 0.010 | |
| Age groups | >80 | 1 | |
| <70 | 1.818 (1.188-2.783) | 0.006 | |
| 70-80 | 1.358 (0.874-2.109) | 0.173 | |
| Sex | Men | 1 | |
| Women | 1.365 (1.000-1.863) | 0.050 | |
| Venous invasion | No (V0) | 1 | |
| Yes (V1) | 0.647 (0.411-1.016) | 0.059 |
| Hazard Ratio (95% CI) | p-value | ||
|---|---|---|---|
| Lymph node ratio | 0.01-0.1 | 1 | |
| 0.11-0.2 | 1.207 (0.770-1.893) | 0.413 | |
| 0.21-0.4 | 1.652 (1.027-2.659) | 0.039 | |
| 0.41-1 | 2.746 (1.740-4.333) | <0.001 | |
| UICC-stage | I | 1 | |
| II | 0.485 (0.260-0.905) | 0.023 | |
| III | 0.849 (0.436-1.654) | 0.630 | |
| Age groups | <70 | 1 | |
| 70-80 | 1,374 (1,008-1,874) | 0.045 | |
| >80 | 1,806 (1,225-2.663) | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





