Submitted:
25 December 2024
Posted:
26 December 2024
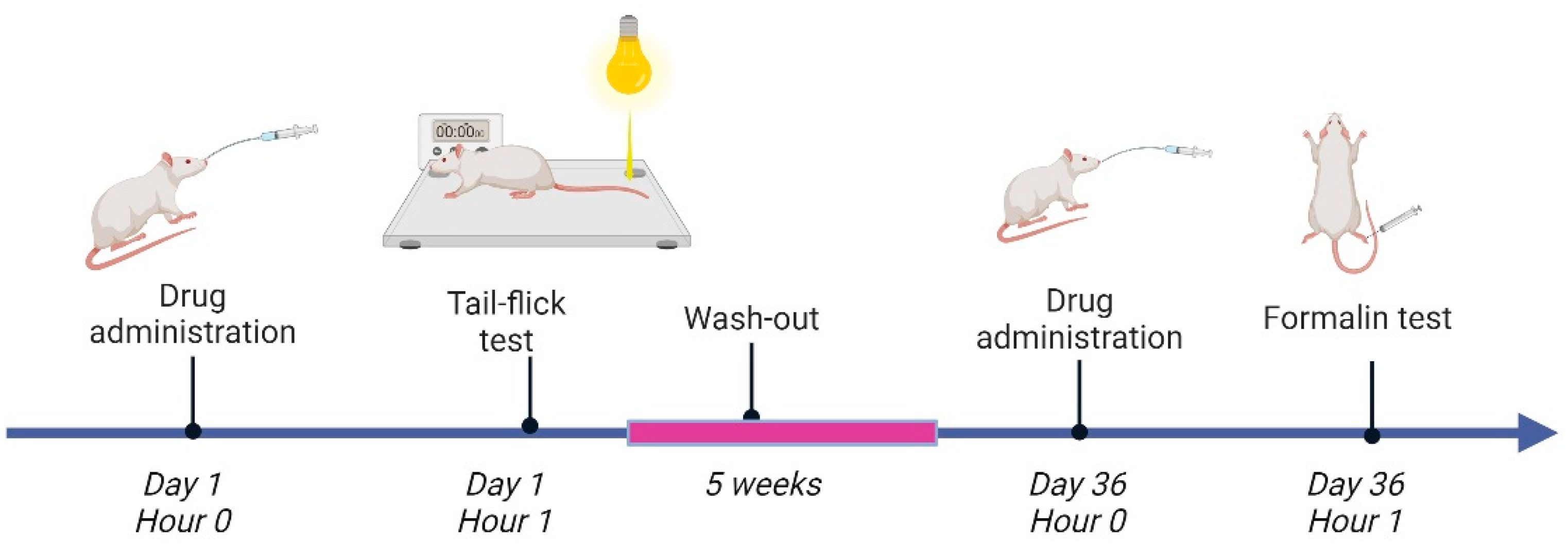
You are already at the latest version
Abstract
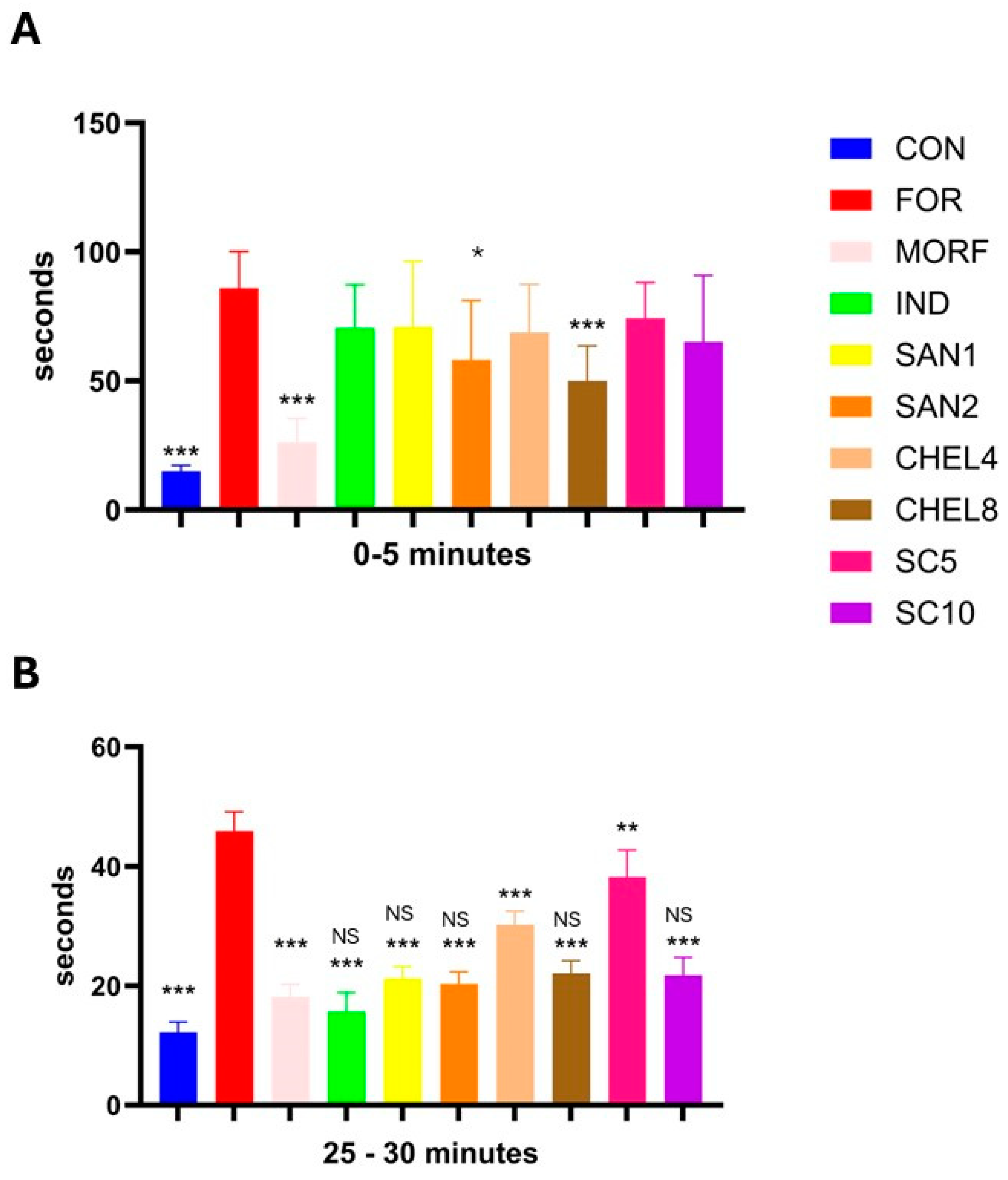
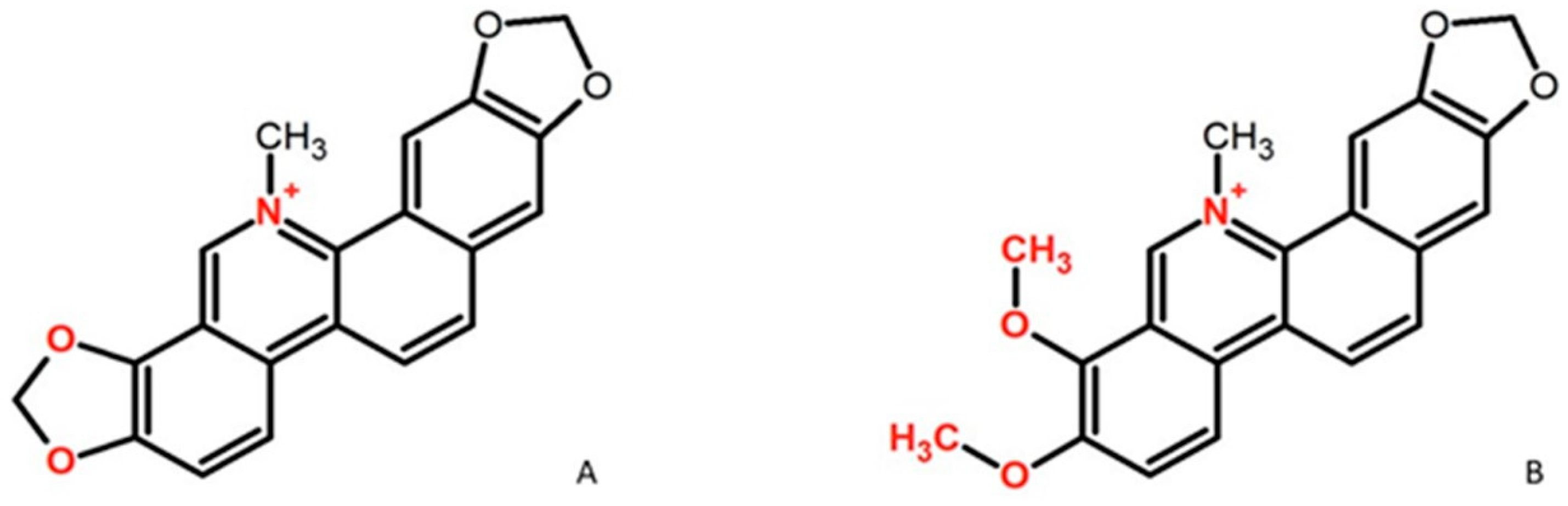
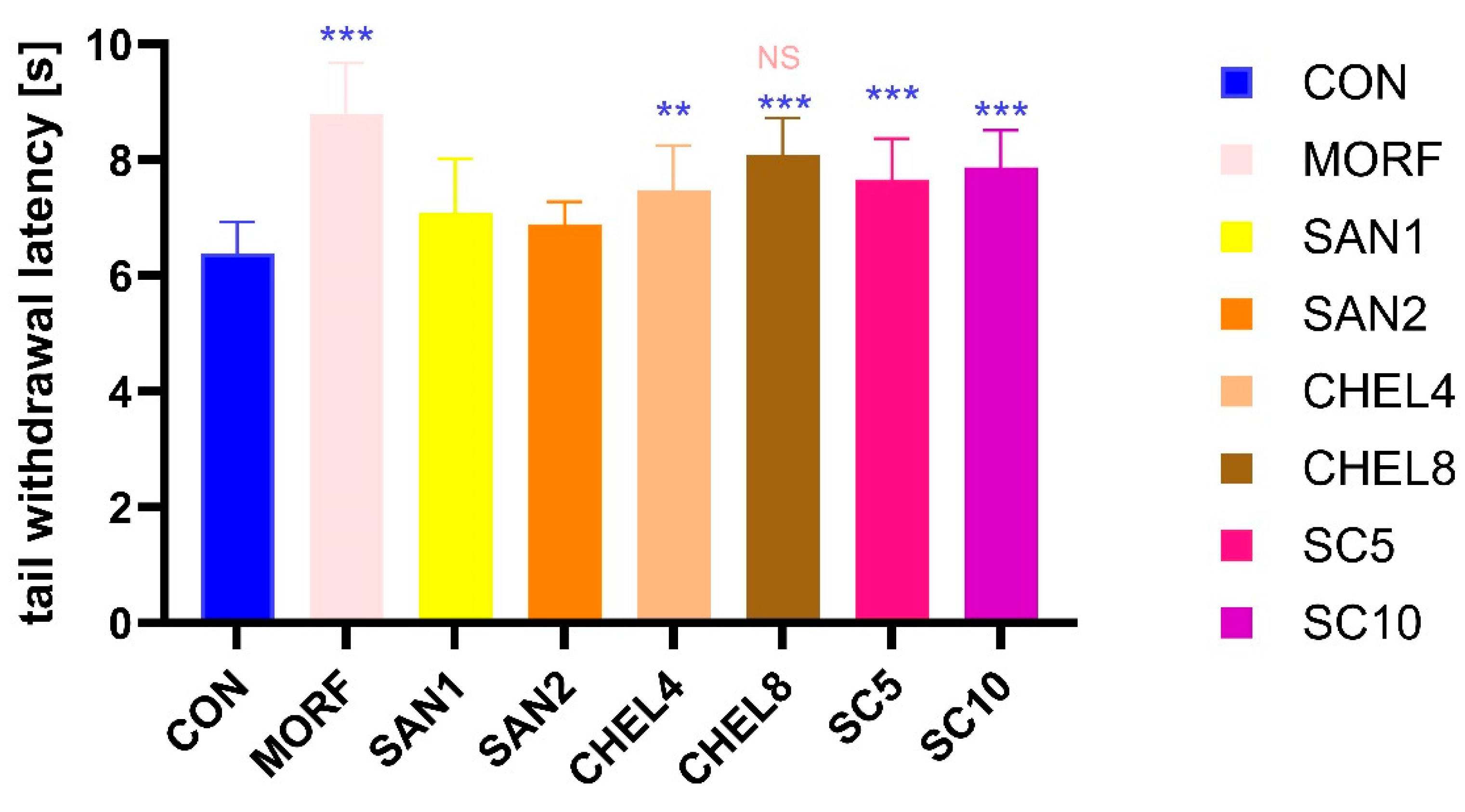
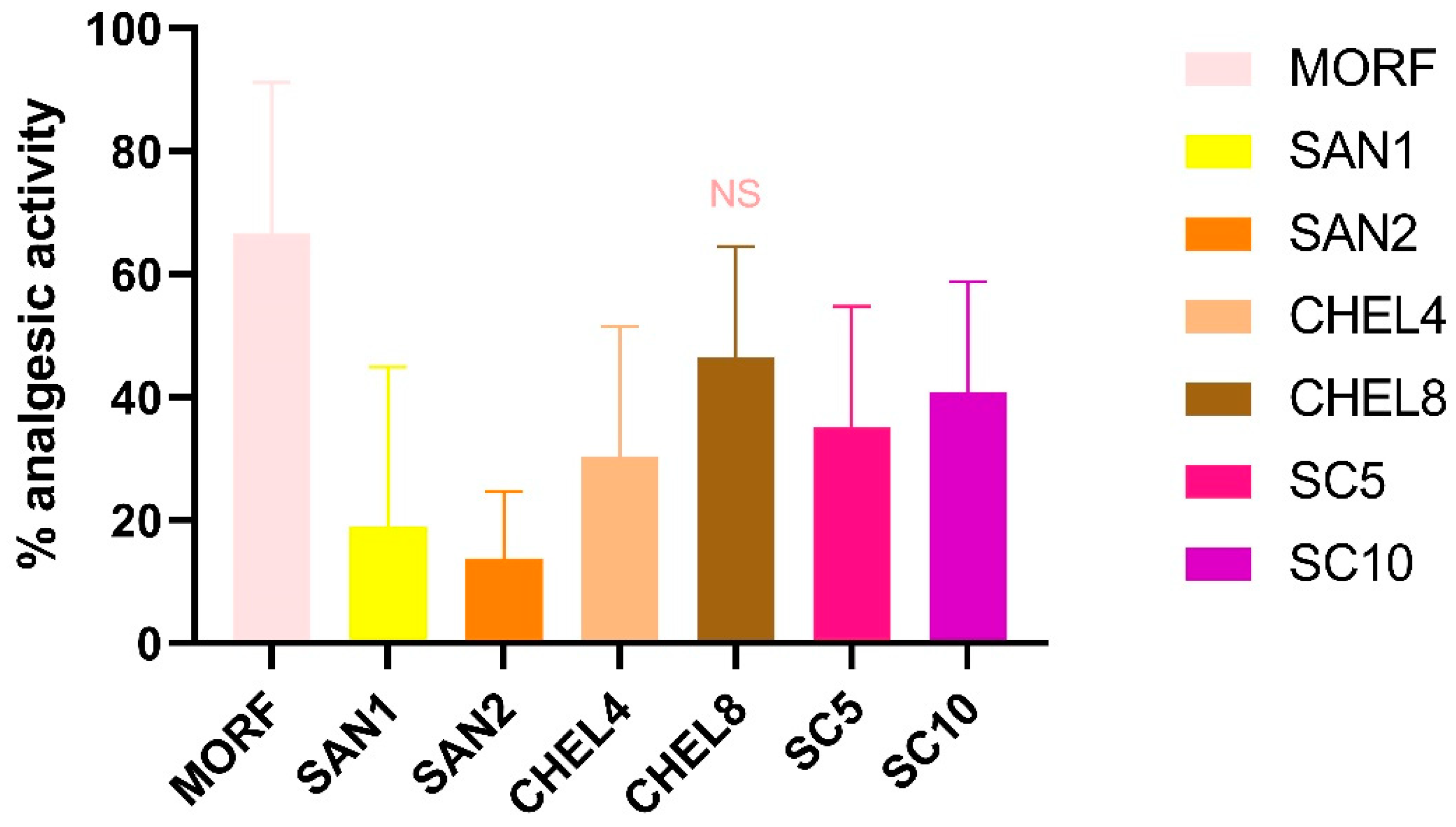
Background: Pain is a major clinical and socioeconomic problem worldwide and existing therapies are not always effective and are often associated with the burden of adverse effects that limit their usage. Natural compounds are an important group of pharmaceuticals that may be used in pain management. We aimed to investigate the analgesic activity of the sanguinarine-chelerythrine from C. chinensis. Methods: The analgesic and anti-inflammatory activity of sanguinarine-chelerythrine fraction of C. chinensis (SC 5 and10mg/kg), sanguinarine (SAN 1 and 2 mg/kg) and chelerythrine (CHEL 4 and 8 mg/kg ) was assessed in the tail-flick and formalin tests. Microscopic and macroscopic examination of stomach mucosae was performed. TNFα and MMP-9 levels were measured with ELISA kits. Results: Morfine (MORF), CHEL and SC prolongated the tail withdrawal latency and with comparable analgesic activity of MRF and CHEL 8 mg/kg. MORF, CHEL 8 mg/kg, and SAN 2 mg/kg ameliorated the pain reaction in the neurogenic phase of the formalin test. In the inflammatory phase of the formalin test, all tested substances exerted analgesic activity. SAN, CHEL and SC reduced additionally TNFα and MMP-9 secretion.. Conclusions: Our results confirmed analgesic effects of CHEL and SC with CHEL analgesic activity comparable to MORF. All investigated substances exerted significant anti-inflammatory activity without concomitant gastrotoxicity.
Keywords:
1. Introduction
2. Results
2.1. Tail-Flick Test
2.2. Formalin Test (Figure 4)
2.3. MMP-9 and TNFα in Paw Homogenates
2.4. Histopathological Assessment of Gastric Mucosa
3. Discussion
4. Materials and Methods
4.1. Chemicals and Materials
4.2. Plant Compounds Preparation
4.3. Animals
4.4. Drug Administration
4.5. Tail-Flick Test
4.6. Formalin-Test
4.7. Isolation of Right Hind Paw
4.8. Macro- and Microscopic Examination of Gastric Mucosa
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Henschke, N.; Kamper, S.J.; Maher, C.G. The epidemiology and economic consequences of pain. Mayo Clin. Proc. 2015, 90, 139–147. [CrossRef]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. [CrossRef]
- Yong, R.J.; Mullins, P.M.; Bhattacharyya, N. Prevalence of chronic pain among adults in the United States. Pain 2022, 163, E328–E332. [CrossRef]
- International Association for the Study of Pain Terminology Working Group IASP Revises Its Definition for the First Time Since 1979. Int. Assoc. Study Pain 2020, 4.
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [CrossRef]
- Meier, T.A.; Refahi, M.S.; Hearne, G.; Restifo, D.S.; Munoz-Acuna, R.; Rosen, G.L.; Woloszynek, S. The Role and Applications of Artificial Intelligence in the Treatment of Chronic Pain. Curr. Pain Headache Rep. 2024, 28, 769–784. [CrossRef]
- Tjong, Y.; Ip, S.; Lao, L.; Fong, H.H.S.; Sung, J.J.Y.; Berman, B.; Che, C. Analgesic Effect of Coptis chinensis rhizomes (Coptidis Rhizoma) Extract on Rat Model of Irritable Bowel Syndrome. J. Ethnopharmacol. 2011, 135, 754. [CrossRef]
- Yang, C. -N.; Kok, S. -H.; Wang, H. -W.; Chang, J.Z. -C.; Lai, E.H. -H.; Shun, C. -T.; Yang, H.; Chen, M. -H.; Hong, C. -Y.; Lin, S. -K. Simvastatin alleviates bone resorption in apical periodontitis possibly by inhibition of mitophagy-related osteoblast apoptosis. Int. Endod. J. 2019, 52, 676–688. [CrossRef]
- Guo, W.; Zhang, J.; Feng, Y. Treatment of neuropathic pain by traditional Chinese medicine: An updated review on their effect and putative mechanisms of action. Phyther. Res. 2024, 38, 2962–2992. [CrossRef]
- Lin, S.; Huang, J.; Zheng, L.; Liu, Y.; Liu, G.; Li, N.; Wang, K.; Zou, L.; Wu, T.; Qin, L.; et al. Glucocorticoid-Induced Osteoporosis in Growing Rats. Calcif. Tissue Int. 2014, 95, 362–373. [CrossRef]
- Park, S.M.; Min, B.G.; Jung, J.Y.; Jegal, K.H.; Lee, C.W.; Kim, K.Y.; Kim, Y.W.; Choi, Y.W.; Cho, I.J.; Ku, S.K.; et al. Combination of Pelargonium sidoides and Coptis chinensis root inhibits nuclear factor kappa B-mediated inflammatory response in vitro and in vivo. BMC Complement. Altern. Med. 2018, 18, 1–13. [CrossRef]
- Yang, Z.; Grinchuk, V.; Ip, S.P.; Che, C.-T.; Fong, H.H.S.; Lao, L.; Wu, J.C.; Sung, J.J.; Berman, B.; Shea-Donohue, T.; et al. Anti-Inflammatory Activities of a Chinese Herbal Formula IBS-20 In Vitro and In Vivo. Evidence-Based Complement. Altern. Med. 2012, 2012, 1–12. [CrossRef]
- Hashemzaei, M.; Rezaee, R. A review on pain-relieving activity of berberine. Phyther. Res. 2021, 35, 2846–2853. [CrossRef]
- Meng, J.; Qiu, S.; Zhang, L.; You, M.; Xing, H.; Zhu, J. Berberine Alleviate Cisplatin-Induced Peripheral Neuropathy by Modulating Inflammation Signal via TRPV1. Front. Pharmacol. 2022, 12, 1–14. [CrossRef]
- Laines-Hidalgo, J.I.; Muñoz-Sánchez, J.A.; Loza-Müller, L.; Vázquez-Flota, F. An Update of the Sanguinarine and Benzophenanthridine Alkaloids’ Biosynthesis and Their Applications. Molecules 2022, 27. [CrossRef]
- Valipour, M.; Zarghi, A.; Ebrahimzadeh, M.A.; Irannejad, H. Therapeutic potential of chelerythrine as a multi-purpose adjuvant for the treatment of COVID-19. Cell Cycle 2021, 20, 2321–2336. [CrossRef]
- Chi, H.; Zhang, X.; Chen, X.; Fang, S.; Ding, Q.; Gao, Z. Sanguinarine is an agonist of TRPA1 channel. Biochem. Biophys. Res. Commun. 2021, 534, 226–232. [CrossRef]
- Li, P.; Wang, Y.X.; Yang, G.; Zheng, Z.C.; Yu, C. Sanguinarine Attenuates Neuropathic Pain in a Rat Model of Chronic Constriction Injury. Biomed Res. Int. 2021, 2021, 2–9. [CrossRef]
- Yu, C.; Li, P.; Wang, Y.X.; Zhang, K.G.; Zheng, Z.C.; Liang, L.S. Sanguinarine Attenuates Neuropathic Pain by Inhibiting P38 MAPK Activated Neuroinflammation in Rat Model. Drug Des. Devel. Ther. 2020, 14, 4725–4733. [CrossRef]
- Jursky, F.; Baliova, M. Differential effect of the benzophenanthridine alkaloids sanguinarine and chelerythrine on glycine transporters. Neurochem. Int. 2011, 58, 641–647. [CrossRef]
- Danielewski, M.; Zielińska, S.; Matuszewska, A.; Słupski, W.; Włodarczyk, M.; Jęśkowiak, I.; Wiatrak, B.; Kowalski, K.; Jezierska-Domaradzka, A.; Ziółkowski, P.; et al. Sanguinarine-Chelerythrine Fraction of Coptis chinensis Exerts Anti-inflammatory Activity in Carrageenan Paw Oedema Test in Rats and Reveals Reduced Gastrotoxicity. Oxid. Med. Cell. Longev. 2022, 2022, 1–12. [CrossRef]
- Li, P.; Wang, Y.-X.; Yang, G.; Zheng, Z.-C.; Yu, C. Sanguinarine Attenuates Neuropathic Pain in a Rat Model of Chronic Constriction Injury. Biomed Res. Int. 2021, 2021, 1–8. [CrossRef]
- Wen Zhi-Hong, Chang Yi-Chen, W.C.-S. Implications of intrathecal pertussis toxin animal model on the cellular mechanism of neuropathic pain syndrome. Acta Anaesthesiol Sin 2003, 41, 187–196.
- Wu, G.J.; Wen, Z.H.; Chang, Y.C.; Yang, S.N.; Tao, P.L.; Wong, C.S. Protein kinase C inhibitor chelerythrine attenuates the morphine-induced excitatory amino acid release and reduction of the antinociceptive effect of morphine in rats injected intrathecally with pertussis toxin. Life Sci. 2006, 78, 1801–1807. [CrossRef]
- Matsushita, Y.; Ishikawa, M.; Abe, K.; Utsunomiya, I.; Chikuma, T.; Hojo, H.; Hoshi, K.; Quock, R.M.; Taguchi, K. Involvement of the protein kinase Cgamma isoform in development of tolerance to nitrous oxide-induced antinociception in mice. Neuroscience 2007, 148, 541–547. [CrossRef]
- Bohn, L.M.; Lefkowitz, R.J.; Caron, M.G. Differential Mechanisms of Morphine Antinociceptive Tolerance Revealed in βArrestin-2 Knock-Out Mice. J. Neurosci. 2002, 22, 10494–10500. [CrossRef]
- Hagel, J.M.; Beaudoin, G.A.W.; Fossati, E.; Ekins, A.; Martin, V.J.J.; Facchini, P.J. Characterization of a Flavoprotein Oxidase from Opium Poppy Catalyzing the Final Steps in Sanguinarine and Papaverine Biosynthesis. J. Biol. Chem. 2012, 287, 42972–42983. [CrossRef]
- Huang, F.C.; Kutchan, T.M. Distribution of morphinan and benzo[c]phenanthridine alkaloid gene transcript accumulation in Papaver somniferum. Phytochemistry 2000, 53, 555–564. [CrossRef]
- Alcantara, J.; Bird, D.A.; Franceschi, V.R.; Facchini, P.J. Sanguinarine biosynthesis is associated with the endoplasmic reticulum in cultured opium poppy cells after elicitor treatment. Plant Physiol. 2005, 138, 173–183. [CrossRef]
- Agarwal, P.; Pathak, S.; Lakhwani, D.; Gupta, P.; Asif, M.H.; Trivedi, P.K. Comparative analysis of transcription factor gene families from Papaver somniferum: identification of regulatory factors involved in benzylisoquinoline alkaloid biosynthesis. Protoplasma 2016, 253, 857–871. [CrossRef]
- Zulak, K.G.; Khan, M.F.; Alcantara, J.; Schriemer, D.C.; Facchini, P.J. Plant Defense Responses in Opium Poppy Cell Cultures Revealed by Liquid Chromatography-Tandem Mass Spectrometry Proteomics. Mol. Cell. Proteomics 2009, 8, 86–98. [CrossRef]
- Li, L.; Zhao, D.; Du, K. ze; Li, J.; Fang, S.; He, J.; Tian, F.; Chang, Y. A vortex-enhanced magnetic solid phase extraction for the selective enrichment of four quaternary ammonium alkaloids from Zanthoxyli Radix. J. Chromatogr. B. Analyt. Technol. Biomed. Life Sci. 2023, 1217. [CrossRef]
- Lin, Q.; Pu, H.; Guan, H.; Ma, C.; Zhang, Y.; Ding, W.; Cheng, X.; Ji, L.; Wang, Z.; Wang, C. Rapid identification and pharmacokinetic studies of multiple active alkaloids in rat plasma through UPLC-Q-TOF-MS and UPLC-MS/MS after the oral administration of Zanthoxylum nitidum extract. J. Pharm. Biomed. Anal. 2020, 186, 113232. [CrossRef]
- Yang, S.C.; Hsu, C.Y.; Chou, W.L.; Fang, J.Y.; Chuang, S.Y. Bioactive Agent Discovery from the Natural Compounds for the Treatment of Type 2 Diabetes Rat Model. Molecules 2020, 25, 5713. [CrossRef]
- Sun, Q.; Li, W.; Li, H.; Wang, X.; Wang, Y.; Niu, X. Preparation, Characterization and Anti-Ulcer Efficacy of Sanguinarine Loaded Solid Lipid Nanoparticles. Pharmacology 2017, 100, 14–24. [CrossRef]
- Fan, L.; Fan, Y.; Liu, L.; Tao, W.; Shan, X.; Dong, Y.; Li, L.; Zhang, S.; Wang, H. Chelerythrine Attenuates the Inflammation of Lipopolysaccharide-Induced Acute Lung Inflammation Through NF-κB Signaling Pathway Mediated by Nrf2. Front. Pharmacol. 2018, 9. [CrossRef]
- Mikołajczak, Ł.P.; Kędzia, B.; Ożarowski, M.; Kujawski, R.; Bogacz, A.; Bartkowiak-Wieczorek, J.; Białas, W.; Gryszczyńska, A.; Buchwald, W.; Szulc, M.; et al. Evaluation of anti-inflammatory and analgesic activities of extracts from herb of Chelidonium majus L. Cent. Eur. J. Immunol. 2015, 4, 400–410. [CrossRef]
- Lan, Y.; Wang, H.; Wu, J.; Meng, X. Cytokine storm-calming property of the isoquinoline alkaloids in Coptis chinensis Franch. Front. Pharmacol. 2022, 13. [CrossRef]
- Hu, S.; Wang, J.; Liu, E.; Zhang, X.; Xiang, J.; Li, W.; Wei, P.; Zeng, J.; Zhang, Y.; Ma, X. Protective effect of berberine in diabetic nephropathy: A systematic review and meta-analysis revealing the mechanism of action. Pharmacol. Res. 2022, 185. [CrossRef]
- Tong, Y.; Wang, R.; Liu, X.; Tian, M.; Wang, Y.; Cui, Y.; Zou, W.; Zhao, Y. Zuojin Pill ameliorates chronic atrophic gastritis induced by MNNG through TGF-β1/PI3K/Akt axis. J. Ethnopharmacol. 2021, 271. [CrossRef]
- Zhu, L.; Li, X. jia; Gu, C.; Gao, Y.; Zhang, C. sheng; Wang, L. yu; Chen, N. hong; Li, G. Mongolian medicine Wenguanmu ointment treats eczema by inhibiting the CKLF-1/NF-κB pathway. J. Ethnopharmacol. 2023, 313, 116549. [CrossRef]
- Al-Romaima, A.; Guan, X.; Qin, X.; Liao, Y.; Qin, G.; Tang, S.; Feng, J. Topical Application of Chinese Formula Yeliangen Promotes Wound Healing in Streptozotocin-Induced Diabetic Rats. J. Diabetes Res. 2022, 2022, 1193392. [CrossRef]
- Wang, Y.; Che, M.; Xin, J.; Zheng, Z.; Li, J.; Zhang, S. The role of IL-1β and TNF-α in intervertebral disc degeneration. Biomed. Pharmacother. 2020, 131. [CrossRef]
- Sethi, J.K.; Hotamisligil, G.S. Metabolic Messengers: tumour necrosis factor. Nat. Metab. 2021 310 2021, 3, 1302–1312. [CrossRef]
- Pan, H.; Li, H.; Guo, S.; Wang, C.; Long, L.; Wang, X.; Shi, H.; Zhang, K.; Chen, H.; Li, S. The mechanisms and functions of TNF-α in intervertebral disc degeneration. Exp. Gerontol. 2023, 174, 112119. [CrossRef]
- Duan, Y.; Li, Q.; Zhou, Y.; Chen, S.; Li, Y.; Zang, Y. Activation of the TNF-α-Necroptosis Pathway in Parvalbumin-Expressing Interneurons of the Anterior Cingulate Cortex Contributes to Neuropathic Pain. Int. J. Mol. Sci. 2023, 24. [CrossRef]
- Duan, Y.W.; Chen, S.X.; Li, Q.Y.; Zang, Y. Neuroimmune Mechanisms Underlying Neuropathic Pain: The Potential Role of TNF-α-Necroptosis Pathway. Int. J. Mol. Sci. 2022, Vol. 23, Page 7191 2022, 23, 7191. [CrossRef]
- Shibata, S.; Tagashira, H.; Nemoto, T.; Kita, S.; Kita, T.; Shinoda, Y.; Akiyoshi, K.; Yamaura, K.; Iwamoto, T. Perineural treatment with anti-TNF-α antibody ameliorates persistent allodynia and edema in novel mouse models with complex regional pain syndrome. J. Pharmacol. Sci. 2023, 153, 1–11. [CrossRef]
- Son, J.Y.; Ju, J.S.; Kim, Y.M.; Ahn, D.K. TNF-α-Mediated RIPK1 Pathway Participates in the Development of Trigeminal Neuropathic Pain in Rats. Int. J. Mol. Sci. 2022, 23. [CrossRef]
- Escolano-Lozano, F.; Gries, E.; Schlereth, T.; Dimova, V.; Baka, P.; Vlckova, E.; König, S.; Birklein, F. Local and Systemic Expression Pattern of MMP-2 and MMP-9 in Complex Regional Pain Syndrome. J. pain 2021, 22, 1294–1302. [CrossRef]
- An, J.; Yang, H.; Zhang, Q.; Liu, C.; Zhao, J.; Zhang, L.; Chen, B. Natural products for treatment of osteoporosis: The effects and mechanisms on promoting osteoblast-mediated bone formation. Life Sci. 2016, 147, 46–58.
- Tseng, K.Y.; Wang, H.C.; Cheng, K.F.; Wang, Y.H.; Chang, L.L.; Cheng, K.I. Sciatic Nerve Intrafascicular Injection Induces Neuropathy by Activating the Matrix Modulators MMP-9 and TIMP-1. Front. Pharmacol. 2022, 13. [CrossRef]
- Shih, Y.C.; Chen, P.Y.; Ko, T.M.; Huang, P.H.; Ma, H.; Tarng, D.C. Mmp-9 deletion attenuates arteriovenous fistula neointima through reduced perioperative vascular inflammation. Int. J. Mol. Sci. 2021, 22, 5448. [CrossRef]
- Kelppe, J.; Thorén, H.; Haglund, C.; Sorsa, T.; Hagström, J. MMP-7, -8, -9, E-cadherin, and beta-catenin expression in 34 ameloblastoma cases. Clin. Exp. Dent. Res. 2021, 7, 63–69. [CrossRef]
- Zhou, R.; Huang, Y.; Tian, C.; Yang, Y.; Zhang, Z.; He, K. Coptis chinensis and Berberine Ameliorate Chronic Ulcerative Colitis: An Integrated Microbiome-Metabolomics Study. Am. J. Chin. Med. 2023, 51, 2195–2220. [CrossRef]
- Zan, Y.; Kuai, C.X.; Qiu, Z.X.; Huang, F. Berberine Ameliorates Diabetic Neuropathy: TRPV1 Modulation by PKC Pathway. 2017, 45, 1709–1723. [CrossRef]
- Zhang, S.; Xu, P.; Zhu, Z.; Zhou, L.; Li, J.; Zhou, R.; Kan, Y.; Li, Y.; Yu, X.; Zhao, J.; et al. Acetylation of p65Lys310 by p300 in macrophages mediates anti-inflammatory property of berberine. Redox Biol. 2023, 62. [CrossRef]
- Li, Z.; Geng, Y.N.; Jiang, J.D.; Kong, W.J. Antioxidant and Anti-Inflammatory Activities of Berberine in the Treatment of Diabetes Mellitus. Evidence-Based Complement. Altern. Med. 2014, 2014, 289264. [CrossRef]
- Prieto, J.M.; Schinella, G.R. Anti-Inflammatory and Antioxidant Chinese Herbal Medicines: Links between Traditional Characters and the Skin Lipoperoxidation “Western” Model. Antioxidants (Basel, Switzerland) 2022, 11. [CrossRef]
- Shi, Y.; Liu, Y.; Xie, K.; Zhang, J.; Wang, Y.; Hu, Y.; Zhong, L. Sanguinarine Improves Intestinal Health in Grass Carp Fed High-Fat Diets: Involvement of Antioxidant, Physical and Immune Barrier, and Intestinal Microbiota. Antioxidants (Basel, Switzerland) 2023, 12. [CrossRef]
- Zielinska, S.; Wójciak-Kosior, M.; Dziagwa-Becker, M.; Glensk, M.; Sowa, I.; Fijalkowski, K.; Ruranska-Smutnicka, D.; Matkowski, A.; Junka, A. The activity of isoquinoline alkaloids and extracts from chelidonium majus against pathogenic bacteria and Candida sp. Toxins (Basel). 2019, 11. [CrossRef]
| CON | FOR | MORF | IND | SAN1 | SAN2 | CHEL4 | CHEL8 | SC5 | SC10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| MMP-9 [pg/ml] | 536.3 ± 84.8** | 805.9 ± 160.3 ^^ | 676.0 ± 131.2 | 551.9 ± 117.7 ** | 552.2 ± 136.4 **, NS | 528.6 ± 83.7 **, NS | 572.8 ± 125.2 *, NS | 526.4 ± 74.3 **, NS |
537.9 ± 172.6 **, NS | 592.3 ± 58.6 *, NS |
| TNFα [pg/ml] | 29.72 ± 12.39* | 43.09 ± 9.91 ^ | 34.11 ± 12.86 | 11.75 ± 2.81 *** | 24.07 ± 7.04 ** | 19.93 ± 3.42 ***, NS | 30.44 ± 8.58 * | 24.37 ± 4.91 **, NS | 23.30 ± 3.89 ** | 19.0.4 ± 2.70 ***, NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





