1. Introduction
Robotic surgery has revolutionized modern medicine by introducing a more precise, minimally invasive alternative to traditional surgical techniques. The roots of robotic surgery trace back to the 1980s, but it gained significant mo-mentum with the introduction of the da Vinci Surgical System in 2000. The system allowed surgeons to perform complex procedures with enhanced preci-sion, dexterity, and control, all through small incisions [
1].
The da Vinci system’s introduction marked a pivotal moment in surgery, en-abling three-dimensional visualization and tremor filtration while replicating the surgeon’s hand movements in real-time. Over time, robotic systems have been refined to reduce patient trauma, minimize blood loss, and promote faster recovery. These technological advancements have broadened the scope of ro-botic surgery, making it a preferred choice in fields like urology, gynecology, and cardiothoracic surgery [
2].
Today, robotic surgery is not only known for improving patient outcomes but also for allowing surgeons to perform procedures with a greater range of motion and precision, surpassing the limitations of human hands. This innova-tion continues to evolve, with the latest advancements pushing the boundaries in minimally invasive surgery, particularly in procedures such as prostatectomy and other complex oncological surgeries.
Robotic-assisted surgery offers several key benefits over traditional open or laparoscopic procedures [
3]. The precision of robotic systems allows surgeons to perform intricate movements with greater accuracy, minimizing damage to surrounding tissues. This minimally invasive approach leads to smaller inci-sions, which can result in reduced pain, less blood loss, and quicker recovery times for patients. Additionally, robotic systems provide enhanced visualiza-tion, with high-definition 3D views, further aiding in the precision of surgical maneuvers. These advantages contribute to improved patient outcomes, such as shorter hospital stays and faster return to normal activities [
4].
Robotic surgery has become a critical tool in the field of urology, especially in the treatment of prostate cancer [
5]. One of the primary reasons for its importance is the precision required in performing prostatectomies, where preserving surrounding nerves and tissues is crucial to maintaining functions such as urinary control and sexual health post-surgery. Robotic systems, particularly the da Vinci Surgical System, offer enhanced dexterity and visualization, allowing surgeons to navigate complex anatomical structures with greater accuracy.
In prostate cancer treatment, robotic-assisted radical prostatectomy (RARP) has quickly become the preferred method over open surgery due to its minimally invasive nature. Patients benefit from smaller incisions, less pain, reduced risk of complications, and faster recovery times. The precision of robotic instruments also enhances the ability to remove cancerous tissues while preserving as much healthy tissue as possible, which is particularly important for prostate cancer given its proximity to nerves that control bladder and sexual function [
6]. The widespread adoption of robotic surgery in urology underscores its importance in improving patient outcomes and surgical efficiency in prostate cancer treatment.
2. History
Robotic surgery has undergone remarkable evolution since its inception in the 1980s, driven by advancements in artificial intelligence, computer systems, and robotics. Early milestones include the PUMA 560 robotic arm, successfully used in neurosurgical biopsy in 1985, and the AESOP system in the 1990s, which improved precision in laparoscopic surgeries [
7,
8].
A pivotal breakthrough came with the da Vinci Surgical System, FDA-approved in 2000, which revolutionized surgery with high-definition 3D visu-alization, advanced robotic arms, and real-time feedback [
9]. Initially focused on urology and cardiothoracic surgeries, its minimally invasive precision quick-ly established it as the gold standard for procedures like prostatectomy.
Recent developments include single-port (SP) robotic systems, enabling complex procedures through a single incision, reducing trauma, and accelerat-ing recovery [
10]. The integration of artificial intelligence has further enhanced real-time decision-making and precision in complex surgeries.
From the early robotic systems to the sophisticated technologies of today, robotic surgery continues to transform medicine, offering minimally invasive solutions and improved patient outcomes.
3. Single Port System
The SP (Single Port) robotic system represents a significant advancement in minimally invasive surgery by allowing surgeons to perform complex proce-dures through a single small incision, typically at the navel or another discrete entry point. This system is a further evolution of earlier multi-port robotic plat-forms like the da Vinci Surgical System. While the earlier versions of the da Vinci system required multiple incisions for separate robotic arms and a cam-era, the SP system consolidates these into one port, offering several advantages [
11].
The SP system, often an extension of the da Vinci robotic platform, is de-signed with a single arm that houses multiple instruments and a 3D camera, all of which are maneuvered through a single incision. These instruments can ar-ticulate within the body, allowing the surgeon to operate with the same level of precision as earlier versions of the da Vinci system but with fewer entry points. The system’s flexible instruments and enhanced optics provide the surgeon with an improved view of the surgical site, allowing for complex procedures to be performed with minimal invasiveness.
The primary difference between the SP system and earlier multi-port ver-sions of the da Vinci system is the reduction in the number of incisions. Earlier systems required separate entry points for each robotic arm and the camera, which, while minimally invasive, still involved multiple incisions. In contrast, the SP system allows for all necessary tools and the camera to be introduced through a single incision, simplifying the surgical process and potentially re-ducing post-operative recovery times, pain, and scarring [
12].
3.1. Advantages of the SP System
Reduced Trauma and Scarring: The use of a single port minimizes the num-ber of incisions, which can result in less trauma to surrounding tissues and re-duced scarring [
13].
Faster Recovery: With fewer incisions, patients often experience quicker re-covery times, less post-operative pain, and shorter hospital stays [
14].
Improved Cosmetic Outcomes: The single incision is typically made in a hidden or less visible area, such as the belly button, leading to more aesthetical-ly pleasing results [
15].
Precision in Complex Procedures: The SP system allows for precise move-ments in tight or difficult-to-reach areas, which is especially important in sur-geries like prostatectomies and urological procedures.
3.2. Potential Limitations
Learning Curve: Surgeons accustomed to multi-port robotic systems may need additional training to become proficient with the SP system’s unique sin-gle-arm structure and the different dynamics of maneuvering through one entry point [
16].
Limited Application: Not all procedures are suited for single-port surgery. Certain complex surgeries may still require multiple access points for optimal outcomes.
Reduced Instrument Movement: While the SP system offers excellent articu-lation, it may not provide the same degree of freedom for certain procedures as multi-port systems, where multiple arms can be positioned independently.
In conclusion, the SP system is an important advancement in robotic surgery, particularly for minimally invasive procedures that benefit from single-port ac-cess. While it offers many advantages in terms of patient outcomes, there are certain limitations to consider based on the complexity of the procedure and the experience of the surgeon. As the technology evolves, it is likely that the appli-cation and precision of the SP system will continue to expand.
4. Comprehensive Analysis of Prostate Cancer in the Context of Surgical Prostatectomy
Prostate cancer is one of the most common cancers among men globally, particularly in developed countries. It is the second most frequently diagnosed cancer in men, following lung cancer, and accounts for a significant percentage of cancer-related deaths [
17]. According to the World Health Organization (WHO), there are approximately 1.4 million new cases of prostate cancer diag-nosed each year, and nearly 375,000 deaths. The incidence of prostate cancer is higher in older men, with the majority of diagnoses occurring in men over the age of 65. Risk factors include age, family history, genetic predispositions, and lifestyle factors such as diet.
4.1. Importance of Prostatectomy in the Treatment of Localized Prostate Cancer
Prostatectomy, particularly radical prostatectomy, is a cornerstone in the treatment of localized prostate cancer, where the cancer is confined to the pros-tate gland and has not spread to other parts of the body. The primary goal of prostatectomy is to remove the cancerous prostate tissue to prevent metastasis and improve survival rates. In cases of localized prostate cancer, prostatectomy offers a potential cure, especially when the disease is detected early. For many patients, it provides an opportunity for long-term cancer control, with high survival rates. Prostatectomy is often recommended for men with a life expec-tancy of at least 10 years, where the benefits of surgery outweigh the risks.
4.2. Indications for Robotic-Assisted Radical Prostatectomy (RARP)
Robotic-assisted radical prostatectomy (RARP) has become the standard of care for many patients with localized prostate cancer due to its minimally inva-sive nature. Indications for RARP include:
Localized Prostate Cancer: RARP is typically indicated for patients with can-cer confined to the prostate (stages T1 and T2) and is considered when the cancer poses a significant risk of progression [
18].
Patient Health and Life Expectancy: RARP is ideal for patients who are healthy enough to undergo surgery and have a life expectancy of at least 10 years [
19]. It is also indicated for patients who prefer an active treatment ap-proach over watchful waiting or radiation.
Cancer Aggressiveness: For patients with intermediate or high-risk prostate cancer, RARP is often recommended to remove the cancer before it spreads be-yond the prostate [
20].
RARP offers several benefits over open surgery, including less blood loss, shorter recovery times, smaller incisions, and reduced risk of complications. The precision provided by robotic systems helps preserve vital structures like the neurovascular bundles, which are critical for maintaining urinary conti-nence and erectile function post-surgery.
5. Detailed Discussion on the SP System Used in Robotic Prostatectomy
Robotic-assisted radical prostatectomy (RARP) is a minimally invasive pro-cedure that involves the complete removal of the prostate gland and some sur-rounding tissue in patients with localized prostate cancer. This procedure is per-formed using a robotic system, typically the da Vinci Surgical System, which allows surgeons to operate with enhanced precision, dexterity, and control.
The surgical process begins with small incisions made in the patient’s abdo-men, through which the robotic arms and camera are inserted. These robotic instruments replicate the surgeon’s hand movements with precision, and the camera provides a high-definition, three-dimensional view of the surgical field. The surgeon, seated at a console, controls the robotic arms to delicately excise the prostate gland while minimizing trauma to surrounding tissues, particularly the nerves responsible for bladder control and erectile function [
21].
Comparison to Traditional Methods:
Open Radical Prostatectomy: In open surgery, the surgeon makes a large inci-sion in the lower abdomen to access and remove the prostate gland. While this approach allows direct visualization of the prostate, it is associated with more postoperative pain, a longer hospital stay, and a higher risk of complications. Open surgery also poses a greater challenge in preserving the delicate nerves involved in urinary and sexual function [
22].
Laparoscopic Prostatectomy: Laparoscopic prostatectomy, a less invasive method compared to open surgery, involves making small incisions through which instruments and a camera are inserted. However, it lacks the enhanced dexterity and visualization provided by the robotic system. While laparoscopic surgery offers some benefits in terms of recovery, it requires more technical expertise and is generally considered more difficult than RARP [
23].
In conclusion, robotic-assisted radical prostatectomy (RARP) has emerged as the gold standard for prostate cancer surgery, offering numerous advantages over traditional open and laparoscopic approaches. Its ability to combine preci-sion with a minimally invasive approach has significantly improved patient outcomes, particularly in terms of recovery, complication rates, and preserva-tion of quality of life.
The Single-Port (SP) robotic system represents a significant evolution in ro-botic surgery, designed to perform complex procedures through a single inci-sion. This development aims to further reduce patient trauma and enhance re-covery time compared to traditional multi-port robotic systems. In the context of robotic prostatectomy, the SP system allows surgeons to operate through a single small port, typically placed at the navel, through which the robotic in-struments and camera are inserted.
The SP system used for RARP consolidates the instruments and camera into one flexible robotic arm that can maneuver with the precision and dexterity re-quired for delicate procedures. This technology retains many of the benefits of earlier da Vinci systems, such as 3D high-definition visualization and tremor filtration, while significantly reducing the invasiveness of the surgery.
5.1. Comparison of Surgical Outcomes and Patient Benefits with the SP System Versus Earlier Robotic Platforms
The shift from multi-port robotic systems to the single-port SP system has brought about several important advantages for patients undergoing prostatec-tomy [
24]. Research comparing SP systems to earlier multi-port platforms has shown several key benefits:
Smaller Incision: The SP system utilizes a single incision, typically hidden in the navel, compared to multiple incisions in traditional robotic systems. This leads to:
Less Scarring: The use of one incision reduces visible scarring, contributing to a better cosmetic outcome.
Reduced Trauma: With fewer incisions, there is less disruption to the sur-rounding tissues, leading to less post-operative pain and faster recovery times.
Faster Recovery: Studies suggest that patients undergoing prostatectomy with the SP system experience faster recovery times than those using multi-port sys-tems. Shorter hospital stays and a quicker return to daily activities are common outcomes due to reduced trauma from surgery.
Enhanced Precision: The SP system retains the precision benefits of previous da Vinci platforms, enabling surgeons to perform delicate nerve-sparing prosta-tectomies, which are essential for preserving urinary and sexual function. While both multi-port and single-port systems offer excellent visualization and con-trol, the SP system’s reduced invasiveness may further aid in post-operative quality of life.
However, it is important to note that the clinical outcomes in terms of cancer control and long-term recovery are still being evaluated in large-scale studies to confirm whether the SP system offers significant benefits over traditional robotic platforms.
5.2. Technical Differences in Performing the Surgery Using the SP System
The most notable technical difference between the SP system and earlier multi-port systems is the use of a single incision for all robotic arms and the camera, as opposed to separate incisions for each instrument. This creates sev-eral unique surgical challenges and benefits:
Instrument Articulation: The SP system’s instruments are designed to be flex-ible within the body, allowing them to articulate and maneuver in confined spaces despite entering through a single port. This contrasts with the rigid in-struments used in multi-port systems that require independent incisions.
Visualization and Access: Although both systems offer high-definition 3D visualization, the SP system requires careful management of the instruments and camera since all components share the same entry point. Surgeons must adapt to the slightly different mechanics of working through a single port, which may involve a learning curve for those accustomed to multi-port sys-tems.
Docking and Setup: The docking process for the SP system is more stream-lined, as only one access point is needed. This can reduce the time spent on set-up and potentially shorten the overall duration of the surgery.
Range of Motion: While the SP system offers improved flexibility and re-duced invasiveness, some surgeons may find that the limited number of instru-ments working through one port reduces the range of motion compared to mul-ti-port systems. This can be a limitation in certain complex procedures that re-quire multiple angles of access.
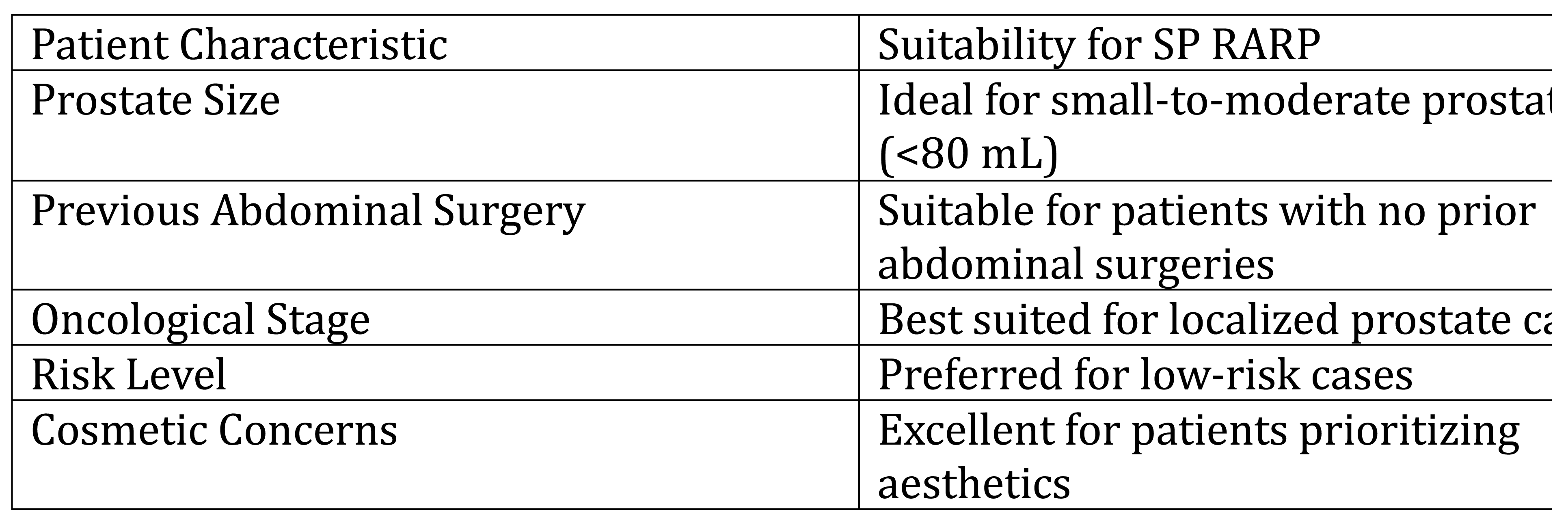
5.3. Indications for Prostatectomy with the SP
The adoption of the SP robotic system for RARP has extended its applicability across various patient profiles. While the general indications for RARP remain consistent, the SP system provides unique advantages in specific scenarios, par-ticularly those involving prostate volume and prior surgical history (
Table 1).
Prostate Volume
Small to Moderate Prostates (≤80 mL): The SP system is highly effective for patients with small to moderate prostate sizes. The 360° visualization and en-hanced precision allow for delicate dissection in confined spaces, ensuring op-timal oncological outcomes while preserving nerve structures.
Large Prostates (>80 mL): Although technically challenging, the SP system’s flexible instrumentation and panoramic view facilitate surgery in larger pros-tates. However, careful preoperative assessment is critical, as increased prostate volume may necessitate extended operative time and careful planning to man-age anatomical complexity.
Previous Surgeries
Patients with No Prior Abdominal Surgery: The SP system performs excep-tionally well in patients without prior surgical interventions, offering a straight-forward surgical approach with minimal adhesions.
Patients with Prior Pelvic or Abdominal Surgeries: Previous surgeries, such as hernia repair, may complicate SP system docking and instrument navigation due to adhesions. However, the SP system’s reduced port requirement and ver-satile instrumentation make it a viable option in many cases, provided the sur-geon is experienced and has accounted for these complexities during preopera-tive planning.
Clinical Considerations
Patients with large prostate volumes or significant surgical history may benefit from tailored approaches:
Preoperative Imaging: Detailed imaging, such as multiparametric MRI or CT scans, helps identify potential challenges, including anatomical distortions or adhesions.
Surgeon Expertise: A higher level of proficiency is required to navigate these cases, especially with the SP system’s single-access limitations.
These factors underline the importance of individualized patient selection and preoperative planning when utilizing the SP system for robotic-assisted prosta-tectomy. Future studies may help define additional criteria for its use in chal-lenging cases.
5.4. Nerve-Sparing Techniques and the Role of the SP System
One of the critical goals in RARP is the preservation of neurovascular bundles responsible for urinary continence and erectile function. The single-port (SP) robotic system, with its enhanced 360° visualization and flexible instrumentation, is particularly well-suited for delicate nerve-sparing techniques. The system’s high-definition 3D optics enable precise dissection in confined anatomical spaces, minimizing damage to adjacent structures.
However, the study by Noh, Kang, Shim, Kang, Cheon, Lee, Kang highlights a nuanced perspective on nerve-sparing outcomes when comparing SP and MP-RARP [
29]. While the SP-RARP approach demonstrated comparable perioper-ative outcomes overall, a notable finding was a lower proportion of complete nerve sparing in the SP group compared to the MP group.
This discrepancy may stem from the technical challenges posed by the SP system’s design. With all instruments passing through a single incision, the de-gree of articulation and maneuverability might be somewhat constrained com-pared to the independent instrument positioning allowed in MP systems. This limitation could make precise dissection of neurovascular bundles more chal-lenging, particularly in complex cases.
However, it is also suggested that with greater surgeon experience and im-proved SP system instrumentation, the potential for achieving nerve-sparing outcomes equivalent to those of MP systems remains promising. Future studies focusing on refining surgical techniques and advancing SP technology will be critical to addressing these limitations and enhancing functional outcomes for patients undergoing SP-RARP.
5.5. Extraperitoneal Approach with the SP System
A standout feature of the SP robotic system is its seamless adaptability to the extraperitoneal approach. Unlike transperitoneal methods, the extraperitoneal approach avoids entering the peritoneal cavity, reducing the risk of associated complications such as bowel injury and postoperative adhesions. The SP system’s single-incision access at the navel or pubic region aligns perfectly with the extraperitoneal technique, facilitating a minimally invasive procedure with reduced trauma.
A notable study by Kaouk, Sawczun, Wilson, Aminsharifi, Fareed, Garisto and Lenfant explored the use of single-port percutaneous transvesical simple prostatectomy using the SP robotic system, presenting promising initial clinical results [
33]. The procedure was performed through a single transvesical incision, showcasing its potential as a minimally invasive option for treating benign prostatic hyperplasia. Key outcomes included minimal blood loss, shorter hospital stays, and no significant perioperative complications. These findings highlight the feasibility and safety of this innovative approach, while the authors emphasize the need for further studies to validate its long-term efficacy and applicability across broader patient cohorts.
Zeinab, Kaviani, Ferguson, Beksac, Kaouk provides an in-depth analysis of a novel surgical approach using the da Vinci SP system [
34]. This technique emphasizes direct transvesical access through a single suprapubic incision, bypassing the peritoneal cavity and allowing for a minimally invasive procedure. The authors report favorable early outcomes, including reduced surgical trauma, shorter recovery times, and minimal perioperative complications. This approach also highlights potential benefits in terms of cosmetic outcomes and postoperative continence. The study underscores the need for further clinical trials to evaluate long-term efficacy and expand its applicability in urological surgeries.
This method has brought urology back to its origins—"the extraperitoneal space." With this approach, hospital stays are dramatically reduced, and in some cases, patients are discharged on the same day as surgery. Pioneers such as Kaouk, Crivellaro, and Patel have demonstrated the feasibility of same-day discharge, highlighting the potential for improved patient outcomes and cost-efficiency [
25]. This is possible due to the reduced invasiveness and streamlined recovery associated with the SP system.
In summary, the SP robotic system provides significant advancements in minimally invasive surgery, particularly in prostatectomy procedures. While both SP and multi-port systems offer high levels of precision, the SP system’s use of a single incision offers key benefits such as reduced trauma, better cos-metic outcomes, and faster recovery times. However, technical differences and the learning curve associated with the SP system must be taken into account, and more long-term studies are needed to confirm its superiority in clinical outcomes.
6. Comparative Analysis of Multi-Port (MP) and Single-Port (SP) Systems for RARP
Robotic-assisted radical prostatectomy (RARP) has evolved significantly over the past two decades, primarily with the advancement of multi-port (MP) and single-port (SP) robotic systems. The multi-port system, which has been the standard for many years, involves multiple incisions to accommodate the robotic arms and instruments. In contrast, the newer single-port system uses a single incision, offering the potential for less invasiveness, improved cosmetic results, and faster recovery. This comparative analysis explores the benefits and drawbacks of both systems in key surgical and patient-related outcomes.
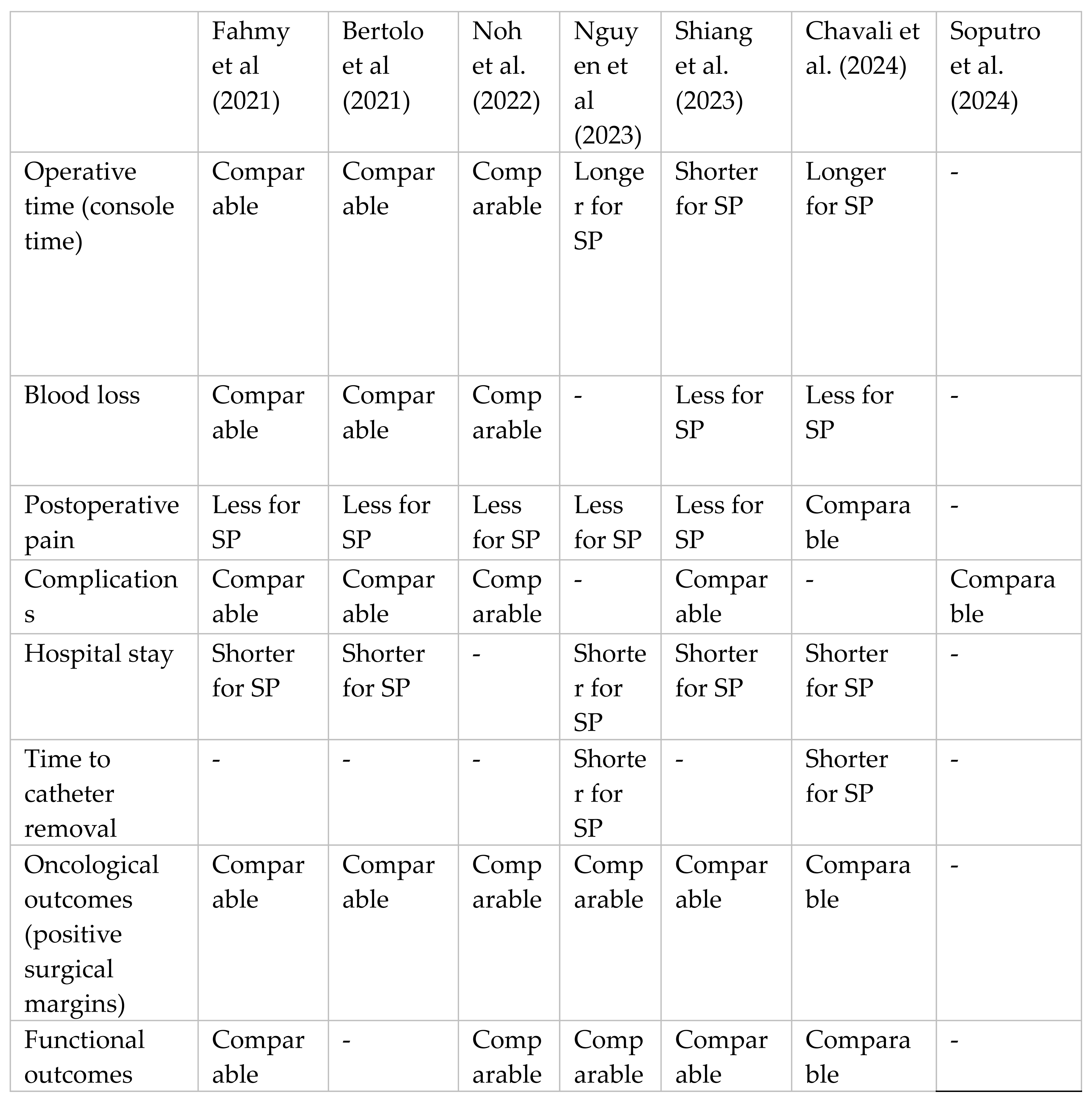
We conducted a comparative analysis of studies evaluating single-port (SP) and multi-port (MP) robotic systems for robotic-assisted radical prostatectomy (RARP), which is summarized in
Table 2.
Operative Time: The operative time is an important factor in RARP, as longer surgeries can increase anesthesia-related risks and postoperative complications. Several studies have shown mixed results in this regard. For example, Shiang, Palka, Balasubramanian, Figenshau ,Smith ,Kim reported that SP procedures had shorter operative times compared to MP [
26]. However, Chavali, Pedraza, Soputro, Ramos-Carpinteyro, Mikeseli ,Kaouk and Nguyen, Dobbs, Vuong, Quy, Ngo, Mai, Tuyet, Thai, Tiong ,Choi, Shahait, Lee found the opposite, not-ing longer operative times for SP, possibly due to the increased complexity of using fewer ports [
27,
28]. Other studies, such as those by Bertolo, Garisto, Bove, Mottrie, Rocco reported no significant differences between the two sys-tems [
29].
Blood Loss: Blood loss is another critical parameter in evaluating the efficiency of a surgical system. The SP system has consistently demonstrated lower blood loss compared to the MP system. Chavali et al and Shiang et al. both reported significantly reduced blood loss in SP procedures . This may be attributed to the minimally invasive nature of SP, which requires fewer incisions, resulting in less tissue trauma. However, Fahmy, Fahmy, Alhakamy, Ghani, Khairul-Asri and Noh et al. found no significant difference in operative time or blood loss [
30].
Postoperative Pain and Recovery: Postoperative pain and recovery times are closely related to the invasiveness of the procedure. Bertolo et al and Nguyen et al that SP systems lead to reduced postoperative pain and faster recovery times, likely due to the single incision as opposed to multiple incisions required in MP procedures. Other studies, such as Fahmy et al and Noh et al supported this, noting shorter hospital stays for SP patients compared to those undergoing MP procedures.
Complications and Oncological Outcomes: In terms of complications, SP sys-tems have been shown a comparable postoperative complications to MP sys-tems. Oncological outcomes—such as cancer control, positive surgical margins, and biochemical recurrence rates—were found to be comparable between SP and MP systems across all studies .
Learning Curve: The learning curve for transitioning from multi-port (MP) to single-port (SP) robotic systems in radical prostatectomy is noted to be steeper due to differences in instrument maneuverability and fewer arms used in SP. Surgeons often require more time to master the SP system, but with experience, comparable outcomes to MP are achieved. The complexity of using a single incision, especially with limited access and articulation, poses initial challenges but can result in benefits like reduced invasiveness and recovery time once proficiency is attained [
31].
Costs: Lenfant, Sawczyn, Kim, Aminsharifi and Kapok examines the cost im-plications of single-port (SP) robotic systems compared to multi-port (MP) systems [
32]. It highlights that while SP procedures may incur higher expenses for disposable materials, these are often balanced by reduced hospitalization costs due to shorter patient stays. This balance results in overall comparable costs between SP and MP robotic surgeries. However, the study emphasizes the need for further research to fully understand the economic impact of SP robotic surgery.
Conclusion: In summary, the comparative analysis of SP and MP systems for RARP shows that while both systems offer comparable oncological and func-tional outcomes, SP provides additional benefits such as reduced blood loss, less postoperative pain, and faster recovery times. Moreover, SP’s superior cosmetic results and patient satisfaction make it an appealing option for many patients. However, the learning curve for SP systems remains a challenge for surgeons accustomed to MP techniques. Further research and long-term studies will help clarify the long-term benefits and potential drawbacks of SP systems as they continue to evolve.
7. Discussion
The emergence of the single-port (SP) robotic system has revolutionized the field of minimally invasive surgery, particularly in robotic-assisted radical prostatectomy (RARP). By integrating advanced optics, precise instrument ar-ticulation, and a streamlined single-incision approach, the SP system represents a significant departure from traditional multi-port (MP) robotic platforms.
One of the most impactful benefits of the SP system is its potential to reduce patient trauma and enhance recovery outcomes. The consolidation of instru-ments and a high-definition 3D camera into a single port minimizes the number of incisions, leading to reduced scarring, shorter hospital stays, and improved cosmetic results. These advantages align with patient-centered care principles, offering not only clinical benefits but also greater satisfaction with the surgical experience.
Nerve-Sparing Capabilities: despite its benefits, the SP system introduces chal-lenges in specific surgical aspects, such as nerve-sparing techniques. The single-port design, while advantageous in terms of reduced invasiveness, can limit the degree of articulation compared to the independent arm positioning in MP sys-tems. This limitation has been associated with a lower proportion of complete nerve sparing in SP-RARP, particularly in complex cases. However, with in-creased surgeon experience and continual refinement of SP system technology, these challenges are being addressed, paving the way for comparable or superi-or functional outcomes.
Extraperitoneal Approach : a standout feature of the SP system is its compati-bility with the extraperitoneal approach. By avoiding the peritoneal cavity, this technique reduces the risk of complications such as bowel injury and adhesions. The extraperitoneal approach has also facilitated same-day discharges in select institutions, highlighting the potential for enhanced efficiency and cost savings. This method signifies a return to urology’s roots, emphasizing the clinical and historical relevance of the extraperitoneal space.
Limitations and Future Directions: while the SP system offers numerous ad vantages, its adoption is hindered by a steep learning curve and limited availa-bility. Surgeons transitioning from MP to SP systems must adapt to the unique dynamics of single-port access, which can initially prolong operative times. Additionally, larger prostate volumes and prior surgical adhesions may present challenges requiring further preoperative planning and imaging.
Given the technical constraints of the single-port (SP) system, such as limited instrument robustness and challenges with traction in complex cases, it is rec-ommended to prioritize its use for low-risk prostate cancer patients. These cases often involve smaller tumors and less complex anatomical considerations, where the minimally invasive nature of the SP system provides significant ben-efits, including reduced trauma, faster recovery, and improved cosmetic out-comes. Conversely, for high-risk cases involving advanced tumors or those re-quiring extensive dissection and manipulation, the multi-port (MP) system re-mains the preferred choice. The MP system’s enhanced traction capabilities and independent instrument positioning offer greater versatility and control, making it better suited for managing complex surgical challenges effectively.
This dual approach ensures optimal outcomes tailored to patient-specific risk profiles and procedural demands.
Future studies are necessary to evaluate long-term oncological and functional outcomes, particularly in the context of nerve-sparing techniques and patient quality of life. As the technology evolves, greater adoption of the SP system could redefine surgical norms and establish new standards for minimally inva-sive prostate cancer treatment.
8. Conclusions
The Da Vinci single-port (SP) system represents a breakthrough in minimally invasive prostatectomy, offering substantial advantages in terms of reduced trauma, quicker recovery, and superior cosmetic results compared to traditional methods. Although oncological outcomes remain similar to those of multi-port (MP) systems, the single-port approach provides significant patient benefits. However, the SP system requires a longer learning curve, which could pose challenges for surgeons transitioning from MP. As robotic surgery continues to evolve, the SP system shows promise as a leading technique in prostate cancer treatment, with the need for further research to validate its long-term outcomes.
In conclusion, the SP robotic system marks a paradigm shift in RARP, offering reduced invasiveness, quicker recovery, and innovative surgical techniques. While challenges remain, its potential to enhance patient care underscores its importance as a transformative tool in modern urological surgery.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all sub-jects involved in the study.
References
- Fairag M, Almahdi RH, Siddiqi AA, Alharthi FK, Alqurashi BS, Alzahrani NG, et al. Robotic Revolution in Surgery: Diverse Applications Across Specialties and Future Prospects Review Article. Cureus. 2024; [CrossRef]
- Rivero-Moreno Y, Echevarria S, Vidal-Valderrama C, Stefano-Pianetti L, Cordova-Guilarte J, Navarro-Gonzalez J, et al. Robotic Surgery: A Comprehensive Review of the Literature and Current Trends. Cureus. 2023; [CrossRef]
- Ho C, Tsakonas E, Tran K, Cimon K, Severn M, Mierzwinski-Urban M, et al. Robot-assisted surgery compared with open surgery and laparoscopic surgery. CADTH Technol Overv. 2012;2(2).
- Reddy K, Gharde P, Tayade H, Patil M, Reddy LS, Surya D. Advancements in Robotic Surgery: A Comprehensive Overview of Current Utilizations and Upcoming Frontiers. Cureus. 2023; [CrossRef]
- Franco A, Ditonno F, Manfredi C, Johnson AD, Mamgain A, Feldman-Schultz O, et al. Robot-assisted Surgery in the Field of Urology: The Most Pioneering Approaches 2015–2023. Vol. 15, Research and Reports in Urology. 2023. [CrossRef]
- Mian AH, Tollefson MK, Shah P, Sharma V, Mian A, Thompson RH, et al. Navigating Now and Next: Recent Advances and Future Horizons in Robotic Radical Prostatectomy. Vol. 13, Journal of Clinical Medicine. 2024. [CrossRef]
- Shah J, Vyas A, Vyas D. The History of Robotics in Surgical Specialties. Am J Robot Surg. 2015;1(1). [CrossRef]
- George EI, Brand TC, LaPorta A, Marescaux J, Satava RM. Origins of Robotic Surgery: From Skepticism to Standard of Care. JSLS. 2018;22(4). [CrossRef]
- Morrell ALG, Morrell-Junior AC, Morrell AG, Mendes JMF, Tustumi F, De-Oliveira-e-silva LG, et al. The history of robotic surgery and its evolution: When illusion becomes reality. Rev Col Bras Cir. 2021;48. [CrossRef]
- Francesco Celotto, Niccolò Ramacciotti, Alberto Mangano, Giacomo Danieli, Federico Pinto, Paula Lopez, et al. Da Vinci single-port robotic system current application and future perspective in general surgery: A scoping review. Surg Endosc. 2024 Aug 7;4814–30.
- Dobbs RW, Halgrimson WR, Talamini S, Vigneswaran HT, Wilson JO, Crivellaro S. Single-port robotic surgery: the next generation of minimally invasive urology. World J Urol. 2020;38(4).
- Arya Asadizeidabadi, Seyedmohammadamin Hosseini, Fedor Vetshev, Sergey Osminin, Seyedali Hosseini. Comparison of da Vinci 5 with previous versions of da Vinci and Sina: A review. Laparosc Endosc Robot Surg. 2024 Jun;7(2):60–5. [CrossRef]
- Wang P, Su YJ, Jia CY. Current surgical practices of robotic-assisted tissue repair and reconstruction. Vol. 22, Chinese Journal of Traumatology - English Edition. 2019. [CrossRef]
- Young Hwii Ko, Jae Youn Jang, Yeong Uk Kim, Sang Won Kim. Faster both in operative time and functional recovery by the extraperitoneal daVinci SP-based robot-assisted radical prostatectomy: a propensity score matching analysis compared to transperitoneal multiport counterpart. Faster both in operative time and functional recovery by the extraperitoneal daVinci SP-based robot-assisted radical prostatectomy: a propensity score matching analysis compared to transperitoneal multiport counterpart. 2024 May 8;
- Probst, P. A Review of the Role of Robotics in Surgery: To DaVinci and Beyond! Vol. 120, Missouri medicine. 2023.
- Soomro NA, Hashimoto DA, Porteous AJ, Ridley CJA, Marsh WJ, Ditto R, et al. Systematic review of learning curves in robot-assisted surgery. BJS Open. 2020;4(1).
- Wang L, Lu B, He M, Wang Y, Wang Z, Du L. Prostate Cancer Incidence and Mortality: Global Status and Temporal Trends in 89 Countries From 2000 to 2019. Front Public Health. 2022;10. [CrossRef]
- Knipper S, Ott S, Schlemmer HP, Grimm MO, Graefen M, Wiegel T. Options for curative treatment of localized prostate cancer. Dtsch Arztebl Int. 2021;118(13). [CrossRef]
- Karagiotis T, Witt JH, Jankowski T, Mendrek M, Wagner C, Schuette A, et al. Two-year quality of life after robot-assisted radical prostatectomy according to pentafecta criteria and cancer of the prostate risk assessment (CAPRA-S). Sci Rep. 2022;12(1). [CrossRef]
- Chen WH, Lee YK, Kuo HC, Wang JH, Jiang YH. Oncological and functional outcomes of high-risk and very high-risk prostate cancer patients after robot-assisted radical prostatectomy. PLoS One. 2023;18(3 March).
- Huynh LM, Ahlering TE. Robot-Assisted Radical Prostatectomy: A Step-by-Step Guide. J Endourol. 2018;32.
- Seo HJ, Lee NR, Son SK, Kim DK, Rha KH, Lee SH. Comparison of robot-assisted radical prostatectomy and open radical prostatectomy outcomes: A systematic review and meta-analysis. Yonsei Med J. 2016;57(5). [CrossRef]
- Ma J, Xu W, Chen R, Zhu Y, Wang Y, Cao W, et al. Robotic-assisted versus laparoscopic radical prostatectomy for prostate cancer: the first separate systematic review and meta-analysis of randomised controlled trials and non-randomised studies. Int J Surg. 2023;109(5).
- Fahmy O, Fahmy UA, Alhakamy NA, Khairul-Asri MG. Single-port versus multiple-port robot-assisted radical prostatectomy: A systematic review and meta-analysis. Vol. 10, Journal of Clinical Medicine. 2021. [CrossRef]
- Abou Zeinab M, Beksac AT, Ferguson E, Kaviani A, Moschovas MC, Joseph J, et al. Single-port Extraperitoneal and Transperitoneal Radical Prostatectomy: A Multi-Institutional Propensity-Score Matched Study. Urology. 2023;171.
- Shiang AL, Palka JK, Balasubramanian S, Figenshau RS, Smith ZL, Kim EH. Comparison of single-port and multi-port Retzius-sparing robot-assisted laparoscopic prostatectomy. J Robot Surg. 2023;17(3).
- Jaya, S. Chavali, Adriana M. Pedraza, Nicolas A. Soputro, Roxana Ramos-Carpinteyro, Carter D. Mikesell, Jihad Kaouk. Single-Port Extraperitoneal vs. Multiport Transperitoneal Robot-Assisted Radical Prostatectomy: A Propensity Score-Matched Analysis. Cancers (Basel). 2024 Aug;2994.
- Nguyen TT, Dobbs RW, Vuong HG, Quy K, Ngo HTT, Mai AT, et al. Single-port and multiport robot-assisted radical prostatectomy: A meta-analysis. Vol. 11, Prostate International. 2023. [CrossRef]
- Bertolo R, Garisto J, Bove P, Mottrie A, Rocco B. Perioperative Outcomes Between Single-Port and “Multi-Port” Robotic Assisted Radical Prostatectomy: Where do we stand? Urology. 2021;155.
- Noh T Il, Kang YJ, Shim JS, Kang SH, Cheon J, Lee JG, et al. Single-Port vs Multiport Robot-Assisted Radical Prostatectomy: A Propensity Score Matching Comparative Study. J Endourol. 2022;36(5).
- Kim JE, Kaldany A, Lichtbroun B, Singer EA, Jang TL, Ghodoussipour S, et al. Single-Port Robotic Radical Prostatectomy: Short-Term Outcomes and Learning Curve. J Endourol. 2022;36(10). [CrossRef]
- Lenfant L, Sawczyn G, Kim S, Aminsharifi A, Kaouk J. Single-institution Cost Comparison: Single-port Versus Multiport Robotic Prostatectomy. Eur Urol Focus. 2021;7(3). [CrossRef]
- Kaouk J, Sawczyn G, Wilson C, Aminsharifi A, Fareed K, Garisto J, et al. Single-Port Percutaneous Transvesical Simple Prostatectomy Using the SP Robotic System: Initial Clinical Experience. Urology. 2020;141. [CrossRef]
- Abou Zeinab M, Kaviani A, Ferguson E, Beksac AT, Kaouk J. Single-port transvesical robotic radical prostatectomy: Description of technique. Urol Video J. 2022;15. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).