The five sensors selected for this study were compared based on the key indicators discussed above. This comparative analysis led to important findings, which are presented in this section, along with summary tables highlighting the results.
4.1. Comparison of Measured Parameters and Sensor Functionality
The comparison of sensors across their ability to measure key health parameters reveals significant differences (
Table 1). EmotiBit stands out for its comprehensive measurement capabilities, tracking a wide array of physiological metrics. The PPG sensor allows for the extraction of several vital parameters, including interbeat interval (IBI), HR, heart rate variability (HRV), SpO2, RR, and fluctuations in BP. These metrics provide valuable insights into autonomic function, cardiovascular health, and respiratory patterns [
82,
83]. The EDA sensor can measure galvanic skin responses, reflecting sympathetic nervous system activity associated with emotional and cognitive arousal [
68,
84]. Furthermore, EmotiBit is equipped with a temperature sensor that monitors perspiration, body temperature, and overall physiological activation, providing further insights into the body’s responses to environmental and emotional stimuli. The device also includes a 9-axis IMU that allows the detection of a wide range of movement-related metrics, offering detailed information on activity patterns [
85]. Moreover, the combination of accelerometer and PPG signals can be used to estimate sleep stages [
86,
87].
In contrast, OpenGo Sensor Insoles are specifically designed to assess parameters such as pressure values, acceleration and angular rate along the x, y, and z axes, total force, and center of pressure (COP) values. These parameters are particularly useful for evaluating gait and balance [
56,
58,
63,
64].
NexRing is a comprehensive health monitoring device that monitors a range of vital signs, including HR (with updates every five minutes), HRV, HR dip, RR, SpO2, and finger temperature, along with activity-related metrics such as steps, distance and calories burned. It also offers detailed sleep tracking, including sleep stages, and personalized scores for readiness and sleep quality, although vital sign measurements, except for HR, are only available during sleep.
The 6-in-1 Remote Health Monitor measures systolic and diastolic BP using oscillometric technology, and employs pulse oximetry to provide SpO2 and HR measurements. Body temperature is assessed using infrared technology, while a 30-second ECG recording offers additional parameters, including average HR, HRV, RR, and maximum and minimum IBI.
Finally, the XeThru X4M200 respiration sensor focuses on measuring respiratory and movement data, including RR, breathing patterns, distance to the target, and movement history. Breathing data is detected only when the individual is stationary, typically while lying down or sitting. Additionally, the X4 module can be used to derive health metrics such as HR, HRV, and sleep stages [
88].
The devices exhibit differences also in terms of recording modes and functionality (
Table 2). All devices, with the exception of the 6-in-1 Remote Health Monitor, are designed for continuous monitoring, while the 6-in-1 Remote Health Monitor supports non-continuous monitoring, allowing users to track specific health metrics through specific measurements. Additionally, all devices, except for NexRing, require manual initiation for data recording. In contrast, NexRing automatically records data when worn and synced with its companion app. The only device that offers the option to select the sampling frequency is the OpenGo Sensor Insoles, while EmotiBit allows for an increased PPG frequency (100 Hz) through a specific firmware variant, making it suitable for applications requiring higher-resolution data, such as HRV analysis.
When using OpenGo Sensor Insoles, users can configure the sample rate and select channels for data recording. Channel selection can be made using predefined setups or by manually choosing specific channels. Additionally, the insoles offer three operational modes tailored to different use cases: (i) Live Capture Mode, which enables direct data transmission from the insoles to the OpenGo software using the mobile app as a hub, ideal for indoor lab environments as it does not store data on the onboard memory; (ii) Record Mode, which stores data directly on the insoles’ onboard memory, suitable for field use; and (iii) Smart Recording Mode, which activates recording only during user activity and making it ideal for long-term monitoring. Finally, a timer function for recording is available only for OpenGo Sensor Insoles. NexRing also offers predefined recording times, but only during app-guided workouts and mindfulness sessions. A predefined recording duration could useful when monitoring specific events, such as the effect of a medication or sessions of physical activity, eliminating the need for the user to manually stop the recording. Sessions with a predefined duration would also optimize battery life and memory management.
The XeThru X4M200 allows data recording based on four distinct respiratory profiles, tailored for specific use cases. Each profile corresponds to a defined RR range (e.g., 8 - 30 breaths per minute for adults, 15 - 65 breaths per minute for infants and children) and a duration of the Slow and Fast Pulse-Doppler algorithms (6 and 20 seconds, respectively, for adults; 6 and 15 seconds, respectively, for infants and children). The profiles also feature a specific detection zone, configurable from a minimum of 0.40 meters to a maximum of 5 meters, with an adjustable resolution of 1 cm and a step size of 5.14 cm. The device also allows users to adjust sensitivity, and it features noise map control with three modes: default noise map, stored noise map, and an adaptive noise map that dynamically adjusts to environmental changes. Furthermore, users can configure the radar’s frequency band (low: 6.0 - 8.5 GHz, or high: 7.25 - 10.2 GHz). Finally, the X4M200 radar can detect presence and vital signs through lightweight materials, such as blankets or clothing, adding versatility for applications such as sleep monitoring.
In terms of memory capacity, the devices with the largest storage appear to be EmotiBit and NexRing. Regarding calibration and initialization requirements, it should be noted that Montgomery [
45] recommends a 5-minute period before starting data collection with EmotiBit, allowing the sensors to settle for accurate readings. Before recording with OpenGo Sensor Insoles, it is required to warm up the insoles for few minutes and take some steps to facilitate the automated zeroing process, which eliminates pressure signal drifts caused by temperature variations or wear. Additionally, an initial user-specific weight calibration is required to enhance the accuracy of total force readings of the insoles. This process involves a 1.5-minute routine of specific movements (e.g., walking, standing still, and shifting body weight), slowly performed and step-by-step guided.
The accuracy of each sensor can be influenced by specific factors. For example, proper attachment of the EmotiBit to the body is critical to minimize motion artifacts, particularly since the PPG signal is highly susceptible to disturbances. However, the device should not be worn too tightly, as this could constrict underlying vascular systems, potentially affecting blood flow and distorting the signal [
82,
89]. Additionally, the sensor’s accuracy may be influenced by the wearer’s body position [
76,
82]. Regarding OpenGo Sensor Insoles and NexRing, data accuracy may be impacted by improper sizing (e.g., incorrect fit), and, for the 6-in-1 Remote Health Monitor, measurement accuracy may be affected by an incorrect device placement, subject’s conditions (e.g., sweat or creams on the forehead can affect body temperature readings, while wet fingers can influence ECG accuracy), movement, or improper posture (e.g., not aligning the BP cuff with heart level). The performance of the XeThru X4M200 can be influenced by vibrations, indirect reflections, surrounding surface material properties, and nearby metallic objects.
Finally, most devices appear suitable for both indoor and outdoor use. The 6-in-1 Remote Health Monitor is specifically designed for indoor environments, particularly in healthcare settings or homes, where measurements should be taken in stable conditions. For added durability, users can attach a protective case to the EmotiBit for safer use.
4.2. Assessment of Sensor Comfort, Design, and Usability
Selected sensors feature significant differences in terms of comfort, design, and usability, as described in
Table 3. EmotiBit offers great flexibility in placement and orientation due to its adjustable straps, allowing it to be used on various body parts, from a child’s wrist to an adult’s head. Placement examples for EmotiBit include the middle finger [
45], the ankle [
51], and the upper arm [
47]. On the other hand, OpenGo Sensor Insoles and NexRing are intended for use on specific body parts. For optimal use, NexRing is recommended to be worn on the index finger of the non-dominant hand, with the sensors facing the palm, while avoiding pairing it with other rings to prevent discomfort or damage. NexRing is durable, waterproof, and suitable for daily activities such as showering or hand washing, although it is best avoided during activities involving friction or when handling heavy metal, ceramic, or stone objects to prevent scratches. OpenGo Sensor Insoles are easy to put on and provide a natural fit with minimal interference with natural movement. Some users may experience mild initial discomfort when wearing the insoles, particularly in the elevated medial midfoot area of the insoles, which houses the electronics and power supply. Both insoles and the ring seamlessly integrate into daily clothing, while EmotiBit, although its stretchable design makes it easy to attach, is less discreet and may not blend smoothly with everyday attire, appearing more as an additional accessory. However, to enhance integration and reduce visibility of EmotiBit, users can customize a strap-and-go case to hold the device.
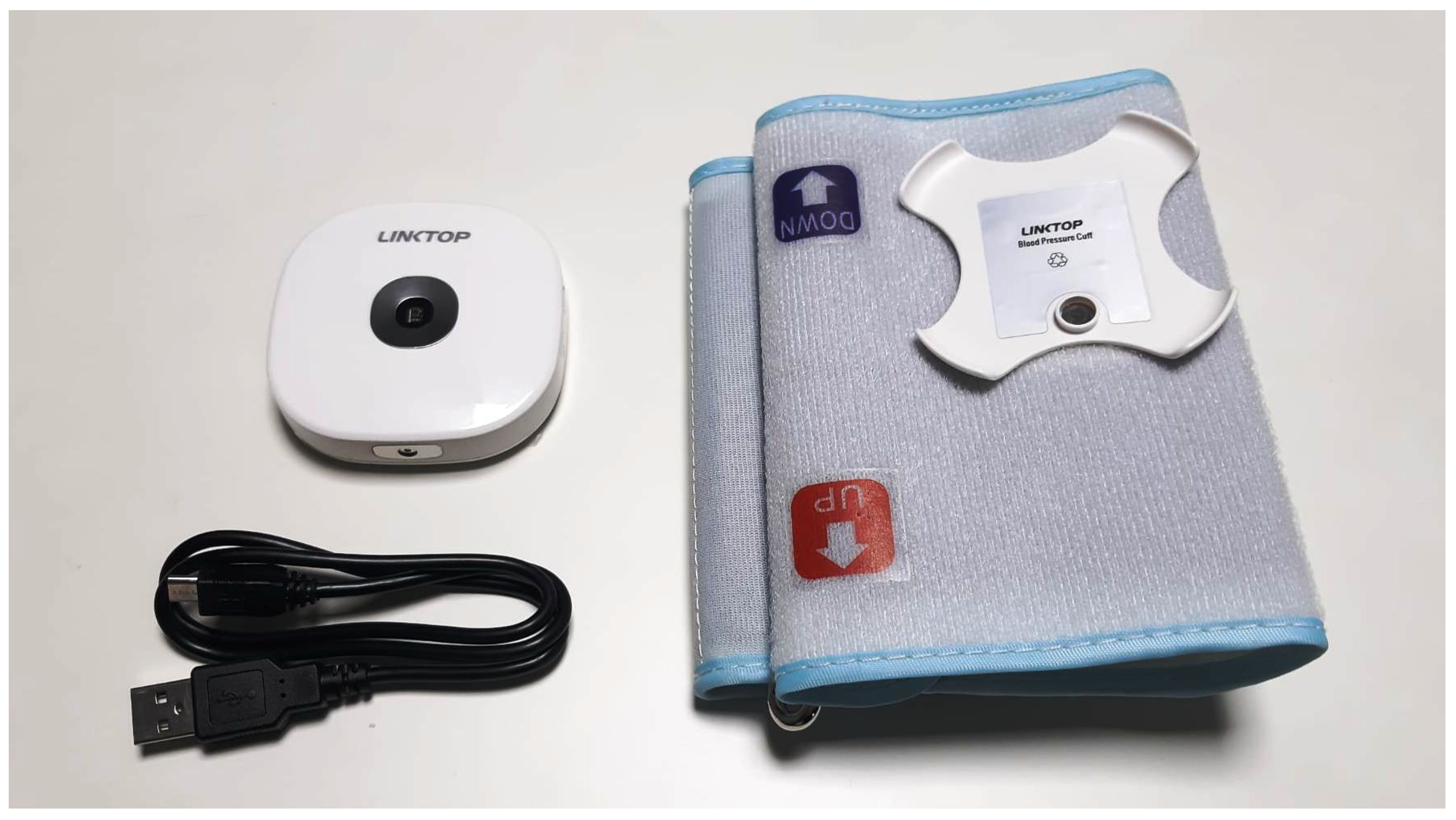
The 6-in-1 Remote Health Monitor can measure multiple vital parameters from specific body locations with minimal invasiveness. Body temperature is taken from the center of the forehead, maintaining a distance of 1-2 cm, while BP is measured with the cuff positioned 1-2 cm above the left elbow joint. To facilitate proper use, the BP cuff is equipped with clear indicators for correct placement. SpO2 and ECG readings are obtained by interacting directly with the device. For SpO2, the left middle finger should rest on the sensor with the fingertip touching the probe, while for ECG measurements, the device is held in the left hand, with the thumb placed on the oxygen sensor and the other fingers touching the metallic label on the back. The right hand is then placed on the body temperature sensor, with the two hands not touching each other [
90]. While practical for most measurements, the ECG function requires the use of both hands, which may pose difficulties for individuals with limited hand mobility or those without assistance.
The XeThru X4M200 respiration sensor is entirely non-contact, and can be positioned on surfaces including desks, walls, or ceilings, and even placed behind obstacles such as walls or ceilings, depending on material properties. A potential constraint to consider when positioning the device is the stability of the surface on which it is placed. Additionally, its small size and unobtrusive design make it ideal for integration into home environments.
All selected devices are compact and portable, and, except for the radar, offer adaptable solutions for users with different body sizes. OpenGo Sensor Insoles, although available in a wide range of sizes (EU 32/33 to 48/49; US 1/2 to 12½/13½) and covering 98% of adult sizes [
91], are not suitable for users with custom orthotics or with a body weight exceeding 120 kg. Additionally, the product guidelines caution against use with open wounds, unhealthy foot skin, or severe gait impairments. The insoles must be worn with socks to avoid direct skin contact and are not suitable for wet conditions (e.g., rain or excessive foot sweat) or activities that may excessively bend or twist the insole, such as driving or climbing ladders. Regarding reusability and cleaning, all devices are designed for reuse by different users or in various settings, although cleaning methods vary.
4.3. Analysis of Sensor Platforms and Support Resources
Table 4 compares selected devices across various categories related to sensor platforms and support resources. Devices such as EmotiBit and XeThru X4M200 respiration sensor offer software-based solutions: the EmotiBit Oscilloscope and DataParser for EmotiBit, and the XeThru Explorer for the XeThru X4M200. The EmotiBit Oscilloscope is designed for real-time visualization of signals, including PPG, HR, EDA, accelerometer, gyroscope, and magnetometer data, as well as temperature and frequency of skin conductance responses. It also allows users to record data onto the onboard SD card, manage power modes to conserve battery, annotate data for further analysis, and stream data. The DataParser complements this by processing recorded data offline, allowing to convert raw files into parsed data files for detailed analysis. XeThru Explorer enables the visualization and management of sensor data, offering advanced real-time metrics such as RR, breathing patterns, movement history, and radar data (e.g., pulse-Doppler data and baseband signals). It also allows users to select suitable respiration profiles, adjust settings, and record or replay measurements.
In contrast, NexRing and the 6-in-1 Remote Health Monitor operate exclusively via dedicated mobile apps. The NexRing App allows users to track daily activity, sleep patterns, and health metrics over time, presenting data through graphs and enabling customization with tags. The Linktop Health Monitor App for the 6-in-1 device records health data and provides real-time visualization of measurements such as SpO2, HR, and ECG waveforms, along with parameters of HRV and RRI. It also features historical data visualization and data export capabilities.
OpenGo Sensor Insoles provide the most comprehensive platform, offering both a desktop software (OpenGo Software) and a mobile app (OpenGo Mobile App) [
92]. The mobile app manages insole configuration, initiates and stops measurements, previews live data, and calibrates force readings, while the desktop software provides data analysis, customizable dashboards, and data export options. Furthermore, for OpenGo Sensor Insoles, as well as for NexRing, the 6-in-1 Remote Health Monitor, and XeThru X4M200, only one device can be managed at a time. Whit EmotiBit, instead, it is possible to connect multiple devices individually by using separate Oscilloscope instances.
Regarding usability and accessibility, platforms of OpenGo Sensor Insoles, NexRing, and the 6-in-1 Remote Health Monitor feature intuitive and user-friendly interfaces. OpenGo Software supports customizable dashboards, while the Linktop Health Monitor App provides clear measurement blocks, with seconds left until completion of ECG recordings and physiological reference values for some health parameters. NexRing offers effortless tracking of health trends via detailed graphs. In contrast, EmotiBit and XeThru X4M200 may require technical expertise for data interpretation as both devices focus on signal trends rather than easily interpretable parameters, which may be challenging for non-expert users. Additionally, while platforms’ installation procedures are relatively straightforward and includes step-by-step guidance for most devices, installing EmotiBit’s software and firmware, as well as assembling the device and waking it from the Sleep Mode - despite being thoroughly detailed in the provided documentation [
93] - may present challenges for users with limited technological proficiency or reduced manual dexterity.
All devices are equipped with operational indicators and alerts to assist users. OpenGo Sensor Insoles excel in this area, offering various features such as readiness indicators for zeroing (displaying different colors to indicate whether the process is successful), pre-measurement pop-ups for assigning measurement labels, and biofeedback alerts via beeps or flashes to facilitate synchronization with other systems. However, it is worth noting that associated platforms do not provide users with comprehensive guidance regarding proper positioning during measurements. Such guidance could be particularly beneficial for complex procedures, such as for the ECG reading with the 6-in-1 Remote Health Monitor, that requires precise hands placement on the device. In this case, the only on-screen instruction advises users to ensure contact with the lead films on the back of the device, with also displaying the signal quality. The user manual for the 6-in-1 Remote Health Monitor suggests that an inverted waveform during ECG readings may indicate improper hand positioning, but these observations rely on the user’s ability to recognize errors and make necessary adjustments, which may demand professional knowledge. Similarly, the device notifies if a BP measurement is initiated without the device being inserted into the cuff, but it does not confirm whether the cuff is correctly positioned.
The devices are accompanied by documentation and user instructions; however, only EmotiBit and OpenGo Sensor Insoles provide dedicated libraries for advanced data processing. Language support also differs; resources of EmotiBit and XeThru X4M200 are available exclusively in english, while NexRing and the 6-in-1 app support multiple languages. OpenGo offers multiple languages only for its software, as the mobile app and documentation are available exclusively in english. Finally, devices provide developer tools to support custom solutions. While EmotiBit offers open-source software, the other devices provide SDKs or APIs for integration and advanced customization.
4.4. Evaluation of Data Transfer, Accessibility and Export Features
All devices support automatic data transfer to their respective platforms, though with different methods (
Table 5). EmotiBit uses Wi-Fi, NexRing and the 6-in-1 Remote Health Monitor rely on Bluetooth, while the XeThru X4M200 requires a micro USB connection. EmotiBit offers additional flexibility by supporting OSC, UDP, and LSL protocols for transmitting data from the software to user-defined output channels.
Data transfer from OpenGo Sensor Insoles to mobile app is via Bluetooth, while that from mobile app to desktop software is supported by Wi-Fi, with transfer time ranging from seconds to minutes depending on the amount of data and recording mode. This transfer can occur automatically or by manual initiation, depending on user settings for recording data.
Data accessibility is robust across all devices, with data recordings remaining accessible after disconnection. However, for OpenGo Sensor Insoles, this applies only if data has been transferred to the software, and for NexRing, data can only be viewed through the mobile app.
Regarding raw data export, significant differences exist among the devices. EmotiBit and OpenGo Sensor Insoles allow raw data export in .csv and .txt formats, respectively. EmotiBit’s data is fully user-owned and stored on the onboard SD card. The simplest method to access the data is by connecting the SD card to a computer. Raw data is saved as a single file per session, along with an information file (.json) detailing recording settings. Parsed data files (.csv) specific to individual sensors of EmotiBit can also be generated using the DataParser tool. OpenGo Sensor Insoles’ raw data can be exported via its software, and, in total, each raw data file provides one timestamp channel and the following sensor channels for each insole: 16 pressure channels, 3 acceleration channels, 3 angular rate channels, 1 total force channel (computed onboard), and 2 COP channels in X and Y directions (computed onboard). Also X4M200 sensor allows for raw data export. Such data, in .dat format, is automatically stored in a user-defined directory after recording. The desktop software allows users to configure file storage preferences and data segmentation by time or file size. By default, the Xethru module generates 17 baseband data frames per second, offering raw I/Q (In-Phase and Quadrature) or Amplitude/Phase data for customized analyses. Additional data types include Pulse Doppler (Float and Byte), Noise Map (Float and Byte), and Generic Data (Float, Byte, and String), along with application-specific outputs such as respiration, sleep, and presence data, all in .csv format. In contrast, NexRing and the 6-in-1 Remote Health Monitor do not support raw data export.
Reporting capabilities also vary significantly. Only OpenGo Sensor Insoles and the 6-in-1 Remote Health Monitor generate automated reports. OpenGo offers extensive reporting options, including .pdf and .xlsx reports tailored to different analyses, such as gait and balance assessments. These reports include both graphical and numerical representations and allow for the comparison of multiple measurements [
94]. The 6-in-1 Remote Health Monitor generates basic reports for individual health parameters. Reports for metrics such as BP, HR, and SpO2 include only numerical values and encompass all recorded sessions. The ECG report, instead, combines numerical data with waveform graphs, but only supports one measurement per report.
4.5. Examination of Battery Performance and Power Management
Table 6 provides an overview of how battery-related features vary across selected devices. Wearable devices demonstrate significant differences in battery life, with NexRing emerging as the most durable, followed by OpenGo Sensor Insoles and EmotiBit. The battery life of OpenGo Sensor Insoles is influenced by factors such as operation mode, sampling frequency, and the number of active sensor channels. For data stored on the onboard memory of OpenGo Sensor Insoles, battery life is generally not the limiting factor; instead, the available memory determines the recording duration. The 6-in-1 Remote Health Monitor features a 400 mAh rechargeable lithium battery designed for up to 500 charge cycles under optimal conditions, while the XeThru X4M200 respiration sensor does not feature an internal battery and relies entirely on external power sources. It can be powered either through a micro USB cable or via pins 1 and 2 on the 16-pin interface connector. If both power sources are connected simultaneously, the USB connection takes precedence.
In terms of charging methods, EmotiBit and the 6-in-1 Remote Health Monitor rely on a simple micro USB connection to a computer or a compatible power source, offering a practical and portable solution for daily recharging. NexRing also requires a USB charging connected to a wireless charging dock where the ring is placed. For NexRing, it is recommended to maintain the battery level above 30% before bedtime for an uninterrupted sleep tracking. Similarly, OpenGo Sensor Insoles use a charging dock; however, recharging requires removing the coin cell batteries from the insoles and placing them in the dedicated charging slot, which connects via USB to the power source.
Recharge time also highlights key differences between the devices. NexRing is the fastest to recharge, followed by EmotiBit and OpenGo Sensor Insoles, with the 6-in-1 Remote Health Monitor taking the longest. Most devices incorporate power-saving features to enhance energy efficiency. EmotiBit offers multiple options, including a Low Power Mode, for data recording without real-time transmission; a Wi-Fi Off Mode, which disables the onboard Wi-Fi shield for extended recording sessions; a Sleep Mode, where the device stops all tasks and enters a low-power state ideal for short inactivity; and a Hibernate switch for maximum power conservation during prolonged inactivity. For OpenGo Sensor Insoles, Sleep Mode is recommended during extended periods of inactivity, and optimizing sensor setups further conserves battery life and maximizes storage efficiency. NexRing also features a Power Saving Mode to preserve battery capacity and prevent deterioration during non-use. Similarly, the 6-in-1 Remote Health Monitor includes a low-performance mode designed specifically for ECG measurements, optimizing power consumption during operation. These variations in battery life, charging methods, and power management reflect the distinct design priorities and intended use cases for each device.