Introduction
The hinotori™ surgical robot system (hinotori) is a Japanese surgical-assistance robot developed by Medicaroid Corporation (Kobe, Japan), a joint venture between Sysmex Corporation (Kobe, Japan) and Kawasaki Heavy Industries, Ltd. (Kobe, Japan).
It received the initial regulatory approval from the Pharmaceuticals and Medical Devices Agency of Japan in 2020 for clinical applications in urology. On the other hand, approval for use in gastrointestinal surgery was obtained in October 2022. In recent years, reports on the application of hinotori in gastrointestinal surgery have been made for gastric, colorectal, and pancreatic surgeries [
1,
2,
3,
4,
5,
6,
7,
8].
We started the hinotori liver resection program by the surgeon (ZM) who had more than 300 laparoscopic liver resection experience but none of robotic surgeries, selecting the initial cases which were assessed as moderately complicated procedures with possible advantages from robot-assistance. This report with review is the world-first report for hinotori liver surgery describing our initial experiences.
Materials and Methods
A retrospective observational examination was conducted to evaluate the safety and feasibility of our liver resection program using hinotori. The 10 first-consecutive patients, who were assessed preoperatively as the cases with moderate complexity and possible advantages from robot-assisted procedure, underwent liver resections using hinotori at Fujita health university Okazaki medical center between August 2023 and October 2024. Backgrounds of the cases (patient, tumor and liver functional conditions along with the surgical procedures) and short-term outcomes of the cases were evaluated.
The liver surgeon (ZM), who experienced a main surgeon of laparoscopic liver resection in more than 300 cases but had no experience for robot-assisted surgeries at all, was the main surgeon for the cases. In the first case, he was the main assistant and instructor of liver surgery for experienced robotic surgeon (IU). In the next 3 cases, the robotic surgeon (IU) was the proctor for the liver surgeon (ZM) as the robot operator, and the liver surgeon performed the surgeries independently in the remaining cases. For all cases, supporting staff, such as bed-side surgeons, medical engineers, and nurses, were well-experienced in robot-assisted surgeries using both hinotori and da VinciTM Surgical System (da Vinci, Intuitive Surgical Inc. CA).
We collected data from the prospective database and electronic medical records at our institution that included clinical data on patient demographics, preoperative assessments, surgical outcomes - including postoperative complications - and pathological results, all maintained at our institution. All patients were treated according to the Declaration of Helsinki, and this study was conducted after obtaining informed consent from each patient for the surgery and the study. The study was also approved from the Institutional Review Board (HM24-029).
Characteristics of the Patients and Short-Term Outcomes
Patients’ characteristics (age, gender, body mass index, American society of anesthesiologists-physical status (ASA-PS), diagnoses requiring liver resection, presence of liver fibrosis/cirrhosis and portal hypertension, previous surgical history, number and size of tumors, location of tumors, types of liver resections including the need for major vessel dissections) and short-term outcomes (operation time, blood loss, open conversion, post-operative complications, length of hospital stay, mortality) of the 10 first-consecutive patients were evaluated.
Hinotori™ Surgical Robot System
Hinotori is similar in design to da Vinci, which has four robotic arms and similar types of forceps. However, hinotori includes robotic arms with eight axes of motion, one more than da Vinci, allowing for more flexibility of arm movement and minimizing the risk of interference between the arms [
9,
10,
11].
Furthermore, hinotori features a docking-free design, with the pivot point (the center of the movement on the port site in the abdominal wall) of the instruments controlled by software (
Figure 2) [
7,
9]. Da Vinci arm grasps the trocar, whereas hinotori does not. This allows for a large space around the port and has the potential to reduce damage to the abdominal wall caused by port traction [
10,
11]. On the other hand, unlike da Vinci, original sealing devices, staplers, suction/irrigation devices and dual consoles have not yet been developed for hinotori [
12].
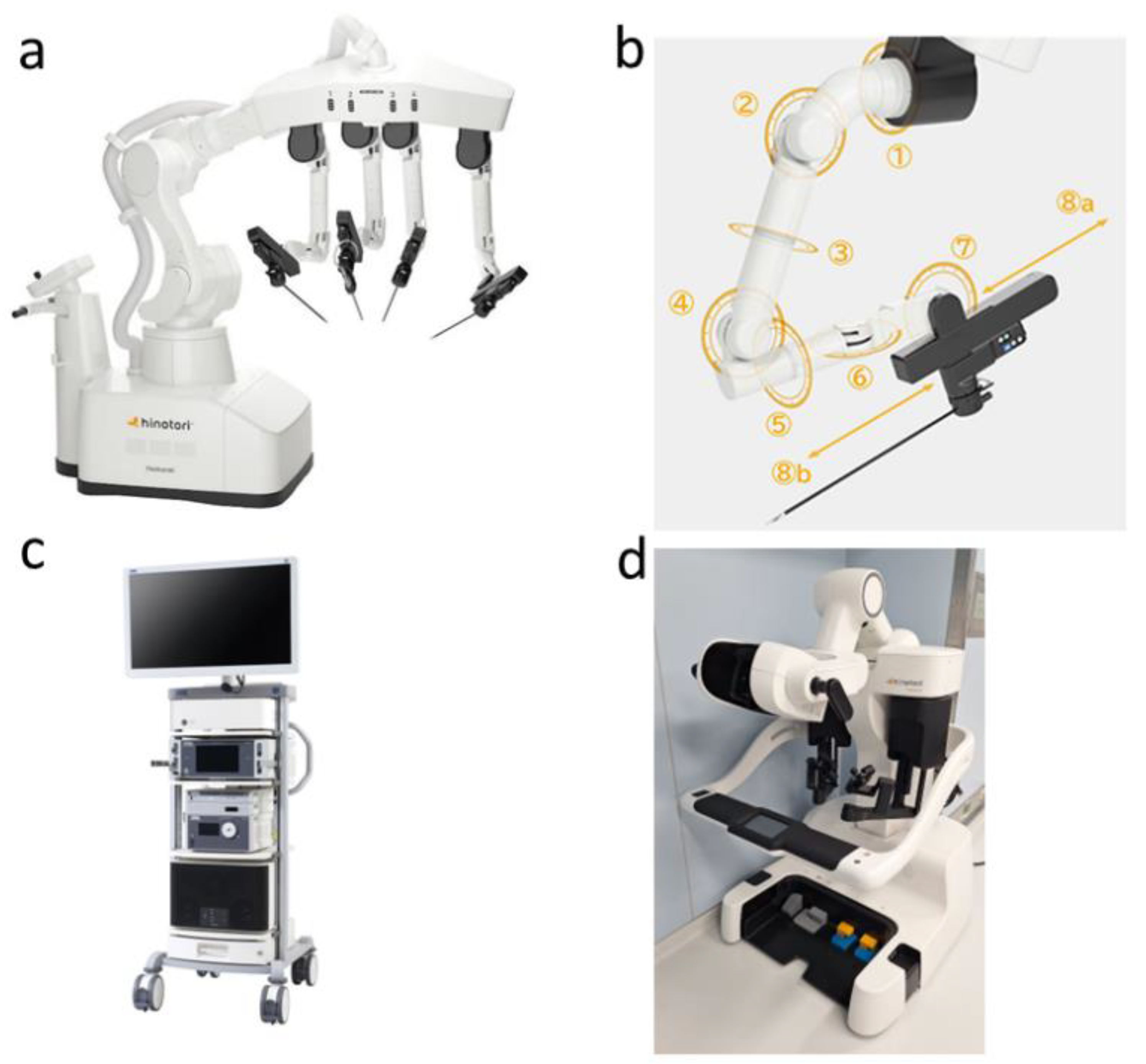
Figure 1.
The hinotori™ Surgical Robot System. a: Operation Unit with four robotic arms; The hinotori™ Surgical Robot System has four arms, similar to those of da Vinci™ Surgical System. However, manipulating arms do not require docking with the ports. b: Robotic arms with eight axes of motion; These arms have one more axis than the arms of the da Vinci™ Surgical System, allowing flexibility of arm movement and minimising the risk of interference between the arms. c: Monitor Cart and d: Surgeon Cockpit; The surgeon cockpit features a flexible 3D viewer that helps reduce neck and shoulder fatigue. The operating procedure is similar to that of da Vinci™ Surgical System.
Figure 1.
The hinotori™ Surgical Robot System. a: Operation Unit with four robotic arms; The hinotori™ Surgical Robot System has four arms, similar to those of da Vinci™ Surgical System. However, manipulating arms do not require docking with the ports. b: Robotic arms with eight axes of motion; These arms have one more axis than the arms of the da Vinci™ Surgical System, allowing flexibility of arm movement and minimising the risk of interference between the arms. c: Monitor Cart and d: Surgeon Cockpit; The surgeon cockpit features a flexible 3D viewer that helps reduce neck and shoulder fatigue. The operating procedure is similar to that of da Vinci™ Surgical System.
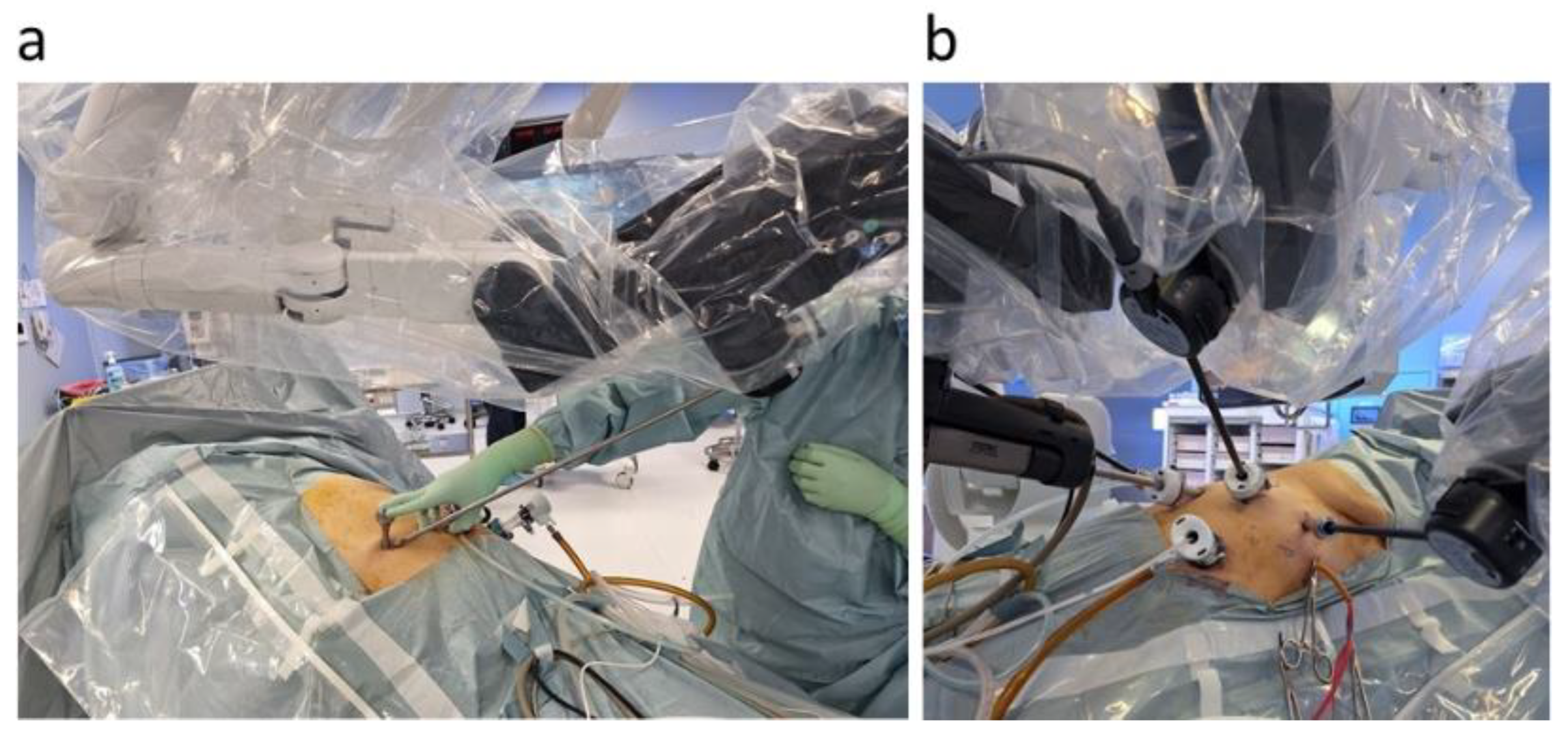
Figure 2.
A docking-free design of hinotori. a: Pivoting using a pivoter; The pivot point (the center of the movement on the abdominal wall) of the instruments is controlled by software. Therefore, no docking of port and arm is required. This has the potential to reduce damage to the abdominal wall caused by port traction. b: Large working space around the port; No docking of the port and the arm provides more space around the port, making external manipulation easier.
Figure 2.
A docking-free design of hinotori. a: Pivoting using a pivoter; The pivot point (the center of the movement on the abdominal wall) of the instruments is controlled by software. Therefore, no docking of port and arm is required. This has the potential to reduce damage to the abdominal wall caused by port traction. b: Large working space around the port; No docking of the port and the arm provides more space around the port, making external manipulation easier.
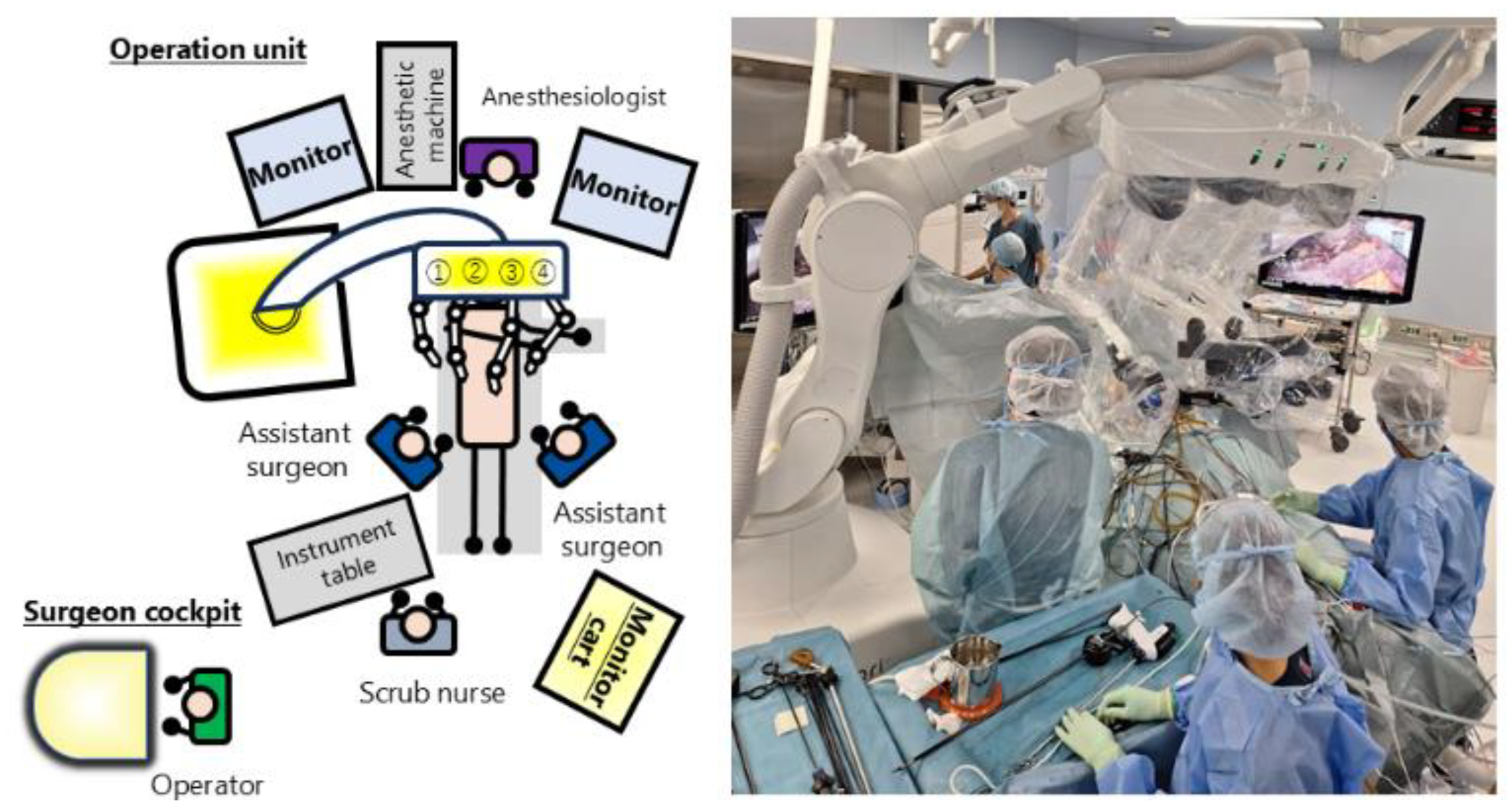
Figure 3.
Operating theater configuration. There are two assistant surgeons beside a patient who perform the extracorporeal intermittent Pringle maneuver, changing the robot's instruments, etc. In addition, the hinotori™ Surgical Robot System does not have the vessel sealing system and suction-irrigation device, so assistant surgeons use laparoscopic devices to assist.
Figure 3.
Operating theater configuration. There are two assistant surgeons beside a patient who perform the extracorporeal intermittent Pringle maneuver, changing the robot's instruments, etc. In addition, the hinotori™ Surgical Robot System does not have the vessel sealing system and suction-irrigation device, so assistant surgeons use laparoscopic devices to assist.
Operative Procedures
The patient was placed in the supine position or right lateral decubitus position. A 12 mm port with a ballon is placed in the umbilicus and the abdominal cavity is observed under a pneumo-peritoneum pressure of 10 mm Hg, followed by the insertion of five ports in the upper abdomen. The placement of the ports was decided depending on the tumor location, resection style and adhesion from previous surgery in each case. Our usual ports placement of laparoscopic liver resection was described previously [
13]. However, since robot ports should be at least 6.5 cm apart from each other and the distance between the ports and the target lesion should be also longer than laparoscopic setting, the ports in this series were placed generally more caudal sites and more apart from each other. A tube and a tape were inserted in the left subcostal area for the Pringle maneuver, if applicable. After all ports were set, the patient was put in a 12 degrees head-up position and hinotori was rolled in for the surgeries.
Fenestrated Bipolar Forceps (Medicaroid Inc., Kobe, Japan) for the left hand of the main surgeon was inserted from the most right-sided 8-mm port. Laparoscope was inserted from the second-right 12-mm port with a ballon. Monopolar Curved Scissors (Medicaroid Inc., Kobe Japan), Maryland Bipolar Forceps (Medicaroid Inc., Kobe, Japan), Clip appliers (Medicaroid Inc., Kobe, Japan), or Wide Needle Holder (Medicaroid Inc., Kobe, Japan) for the main right hand of the surgeon were inserted from the left-side 8 mm port next to the camera-port. A universal grasper (Medicaroid Inc., Kobe, Japan) for the right hand of the surgeon as a traction sub-arm was inserted from the most left-sided 8-mm port. Because the vessel sealing system and suction-irrigation device are not available, the assistant surgeons used Sonicision™ (Medtronic Inc, Minneapolis, MN, US) for dividing small vessels or BiClamp® (Erbe Elektromedizin, Germany) and IO advance electrode (AMCO, Japan) for hemostasis. A laparoscopic suction-irrigation device (Premium angle suction-irrigator, Heiwa medical instrument Co., Ltd., Japan) also used by the assistant surgeons. Those devices for the assistant surgeons were used through the port in the umbilicus or the other port placed between the main surgeon’s ports.
Liver parenchymal transection was mainly performed crushing, sweeping and dividing the liver tissue with the closed curved scissors or Maryland bipolar forceps on the robotic main right hand. The extent of liver resection was determined according to the Makuuchi criteria [
14]. Multi-detector row computed tomography images of the liver, including the tumor, was reconstructed in 3D preoperative simulation on Revoras
TM software (Ziosoft Inc, Japan), and the liver resection was performed on the basis of these images, confirmed by intraoperative ultrasound, with the Glissonian sheath and the hepatic veins as landmarks. Extracorporeal intermittent Pringle maneuver was applied with 15-minutes clamping time interrupted by 5 minutes of reperfusion each, except in case 8 where encircling hepato-duodenal ligament could not be achieved due to the thick adhesion from 3-times previous surgeries.
Results
The characteristics of the 10 cases are presented in Table 1.
8 cases of partial liver resection, 1 extended left medial sectionectomy, and 1 left hemi-hepatectomy were performed. The procedure was applied to 6 hepatocellular carcinomas arising from the liver cirrhosis/fibrosis backgrounds, and 3 cases had also portal hypertension indicated by esophageal varices formation or platelet count less than 100,000/microliter of the blood. Among them, there were 4 partial resections for deep tumors with the needs of major vessel dissection and 2 partial resections of segment 7-8dorsal. One case with a liver metastasis of pancreatic cancer underwent segment 3-4 partial resection behind the jejunum anastomoses after open pancreatoduodenectomy. Two cases of liver metastases from rectal cancer had multiple lesions and underwent extended left medial sectionectomy and 5 partial resections including a segment 8 resection. The procedure was applied for the other one case of left hepatectomy with hepatolithiasis in which the handling of the stenotic lesion in the bile duct was critical. There were 7 males and 3 females with the age of 70 (60-77), median (range). Three ASA-PS class III patients and 7 class II patients were included. The body mass index was 24 (15.2-31.2). 5 patients had previous upper abdominal surgical histories. Among them, there was one patient with the histories of two liver resections and a right-sided colectomy with postoperative major anastomosis-leakage.
The short-term outcomes are shown in Table 2.
Operation time was 419.5 (260-743) minutes. Intraoperative estimated blood loss was 276 (26-4081) ml. The longest operation time (743 minutes) occurred in one HCC patient with thick adhesion who underwent partial resection of the liver segment 7-8dorsal as a third liver resection after a right colectomy with postoperative major anastomosis-leakage. An open conversion in an HCC case (partial resection of segment 7-8dorsal) was experienced due to the bleeding from massive collateral vessels in the round ligament outside of the surgical area. The case was also the case with the largest volume of bleeding. Postoperative length of hospital stay was 7.5 (5-23) days. In the case of extended left medial sectionectomy, postoperative major complication (delayed bile leakage, IIIa in Clavien-Dindo classification) was developed and re-admission occurred. All patients with tumors received R0 resection. There was no mortality.
Discussion
This is the world’s first report of liver resections using a new Japanese surgical robot system, hinotori, describing our initial 10 consecutive robotic liver resections. Hinotori liver resection was shown to be feasible. All the cases, assessed and selected preoperatively as the cases expecting advantages from the usage of robot-assistance, were moderately complicated procedures such as repeat/redo surgeries (5 cases), liver resection for patients with liver cirrhosis (5 cases) and portal hypertension (3 cases), liver resections with wide range dissections of major vessels (4 cases), and segment 7-8dorsal liver resections (2 cases). They also included 2 multiple liver metastases, a 5cm-sized HCC, and a left hemi-hepatectomy with the dissection of Glissonian pedicle in order to handle the stenotic lesion in bile duct. They were safely completed by the liver surgeon (ZM) who had no experience for robot-assisted surgery at all, though he had experienced conventional laparoscopic liver resections in more than 300 cases. The supporting staff were well-experienced in robot-assisted surgeries. In the initial 4 cases, a proctor surgeon (IU, who had experiences for both robotic and liver surgery) supported the operations.
In our previous report [
15] of 231 conventional laparoscopic liver resections, the operation time and the intraoperative blood loss for all cases were 323 minutes and 108 ml (median). However, 133 among the 231 cases were the cases of simple partial resection and left lateral sectionectomy and the cases selected for robotic procedures in the present report were more complicated cases. The operation time (420 minutes) and blood loss (276 ml) of the cases in the present report are similar to those (414 minutes and 255 ml) of the cases excluding the simple partial resection and left lateral sectionectomy. The data is also within the range of outcomes from previous reports for robotic procedures using da Vinci [
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31]], though the operation time was relatively longer. (
Table 3 and Supplementary
Table 1, including 16 reports for various cases of liver resection comparing robotic and laparoscopic surgery between 2019 and 2024 retrieved from Pubmed, Embase and Cochrane Library, excluding systematic reviews and meta-analyses). The short-term outcomes of operation time and blood loss could improve, since the learning curve of the main surgeon (ZM) for robotic procedures might have had some impact on the results.
One case (10%) of open conversion was experienced. The rate is similar to those for right hemi-hepatectomy (8.3%), anterior sectionectomy (12.5%) and segment 7/8 segmentectomies (11.1%) in our previous report of conventional laparoscopic procedure [
15]. Also, it was within the range of the outcomes from previous reports for robotic procedures using da Vinci in which various cases of liver resection were included (
Table 3 and Supplementary
Table 1, [
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31]). The bleeding during the partial resection of segment 7-8dorsal was caused by an injury on the massive collateral vessels in the round ligament, outside of the surgical view for segment 7-8dorsal. The ligament had been transected and pulled downward to the left in order to move the liver and gain enough surgical space in the right subphrenic space. Since the bleeding point could not be identified, the open conversion of the operation was selected. The rigid hinotori scope needed to be placed more cranially for the resection of segment 7-8 dorsal and lost the view for the area of bleeding. In daVinci system, the camera port and the scope can be lifted-up to a higher position by pulling-up the abdominal wall and deeper views can be obtained. This is not possible on hinotori system due to the docking-free “PIVOT” design in which the port point is fixed and cannot be lifted-up. Although the much magnified and stable view is one of the strong points in robot-assisted procedure, the bird view of the whole surgical area often trades off for the advantage and needs to be cautious.
One case of postoperative bile leakage of Clavien-Dindo (CD) grade IIIa was experienced. The rate (10%) of morbidity CD III (and also II) or more was comparable to 7% for all cases in our previous report of conventional laparoscopic liver resection [
15] and also within the range of the outcomes from previous reports for robotic procedures using da Vinci (
Table 3, Supplementary
Table 1 [
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31]). In this case, extended left medial sectionectomy was performed for the 2 metastatic tumors close to the umbilical portion of Glissonian pedicle. Burned injury on the bile duct during the dissection of umbilical Glissonian pedicle might have occurred by the use of cautery, without original sealing devices not yet developed for hinotori [
12] nor CUSA/water jet not equipped on robotic systems.
The length of postoperative hospital stay was shorter than in our previous report of conventional laparoscopic liver resection (14 days for all cases and 12 days for simple cases). A reduction in wound pain compared to da Vinci has been reported in hinotori radical prostatectomy due to less damage to the abdominal wall by the “PIVOT” mechanism in which the robotic arms move around the center point set on the port site [
10]. Reduced wound pain may lead to earlier recovery and shorter length of hospital stay [
32]. However, the length of hospital stay of our conventional laparoscopic patients was relatively longer [
15] and the data was collected from the patients during a long time period. Since our hospitalization policy has been changing gradually with the tendency of shortening the hospital stay, this point should be further examined prospectively.
R status for tumors were well-secured and there was no mortality. Although long-term outcomes should be examined, hinotori liver resections in the present setting (for moderately complicated cases by the robotic-unexperienced surgeon) were feasible.
There is an increasing number of reports for robot-assisted liver resection using da Vinci [
33,
34,
35]. While da Vinci has long been highly competitive and the leading option for robotic surgery, several new platforms are now entering to the field and the Japanese hinotori is one of them. The studies comparing robot (da Vinci) -assisted to conventional laparoscopic liver resection generally showed possible advantages in short-term outcome, such as less blood loss and shorter hospital stay. Although operation time is generally longer, some studies showed less morbidity and a shorter learning curve. Its feasibility is evident; however, the studies have mostly retrospective features and there are still current discussions about its possible short-term advantages. Surgeons’ experiences in laparoscopic and robotic settings at the time of studies can impact the results. Experiences mean both handlings of laparoscopic settings (not open settings and the same in robotic settings for the view and approach) and robot mechanisms. In most studies, retrospective laparoscopic data could have contained historical data (from the lower-experienced era for the laparoscopic settings) or the data from institutions in their learning curve for complicated cases [
36]. On the other hand, the data for robotic procedures mostly came from a short duration and the institutions which had good experiences of both laparoscopic settings and robotic handling. There should be robotic advantages for specific procedures but might not for all procedures, when the current less-equipped (without CUSA, waterjet and other devises used in laparoscopic liver resection) and bulky settings of surgical robots (needed wider spaces between each port and to the target) are counted in. Our present report is important in the point that this is the world first report of hinotori liver resection and, also, showed the feasibility of performing robotic-surgeries of not simple cases by robotic-unexperienced surgeon (with the strong back-up from the team staff and large experiences of laparoscopic procedures).
In the current settings, the main advantages of hinotori over da Vinci may be the larger working space around the port and less abdominal wall damage due to the docking free design, besides the lower purchase price. In our present procedure, Pringle maneuver, traction of round ligament to move the liver, and usage of stapler (plus suction/irrigation/coagulation, sometimes) were performed by patient-side surgeons besides changing robot arms. It is beneficial to have a large space around the trocar. A reduction in wound pain has been reported due to less damage to the abdominal wall due to the “PIVOT” mechanism [
10]. In Japan, the list price of da Vinci (Xi, single console) is JPY 276,000,000, while the double console version is priced at JPY 334,000,000. The annual maintenance costs are JPY 14,000,000 for the single console and JPY 17,500,000 for the double console. In comparison, hinotori is priced at JPY 235,000,000, with a maintenance fee of JPY 13,000,000 [
12]. Hinotor also has a remote surgical function and some reports of its experiments including ours have been published in recent years [
37,
38,
39]. Hinotori was previously pointed out to have difficulty handling a floating sensation, excessive emergency stop function during arm collision and lack of hand clutch function as its drawbacks [
5,
9,
12]. The system has been improving with the updated software to reduce the floating sensation and mitigate the emergency stops and an added hand-clutch function [
5,
40]. Recent meta-analyses using da Vinci showed that robot surgery resulted in, at least, comparable or better short-term outcomes to conventional laparoscopic liver resection [
33,
34,
35]. Future prospective investigations of large numbers into the surgical outcomes of liver resection using hinotori should be also needed.
Conclusions
This is the world-first and a single institutional initial 10 case series report of hinotori liver resection. The number of cases is small. The settings of the surgeons and the cases were unique, which may have had an impact on the outcomes. However, hinotori liver resection was shown to be feasible.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
K.N and Z.M. performed the surgery. M.N. and A.N. made pathological diagnoses. K.N and Z.M. wrote the manuscript. K.N., M.A., T.H., Y.C., K.M., T.E., K.K., K.M., H.K., Y.T., and Z.M. contributed to patient treatment. All authors approved the final version of the manuscript.
Funding
This research received no external funding
Ethics approval and consent to participate
All procedures were completed following the Declaration of Helsinki. Informed consent was obtained from the patient for the publication of this case report.
Consent for publication
A written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Availability of data and materials
Not applicable.
Competing interest
Kenichi Nakamura, Tetsuya Koide, Takahiko Higashiguchi, Kazuhiro Matsuo, Tomoyoshi Endo, Koji Morohara, Kenji Kikuchi, Hidetoshi Katsuno, Ichiro Uyama, Koichi Suda, and Zenichi Morise have no commercial associations or financial involvement that might be construed as a conflict of interest in connection with the submitted article. Ichiro Uyama has received lecture fees from Intuitive Surgical, Inc., outside of the submitted work. Ichiro Uyama has been funded by Medicaroid, Inc. in relation to the Collaborative Laboratory for Research and Development in Advanced Surgical Technology, Fujita Health University. Koichi Suda has been funded by Sysmex, Co. in relation to the Collaborative Laboratory for Research and Development in Advanced Surgical Intelligence, Fujita Health University, and has also received advisory fees from Medicar oid, Inc., outside of the submitted work.
Acknowledgments
The authors thank Maruzen Co., Ltd. (Tokyo, Japan) for their English language review of this manuscript. This work was not supported by grants or funding.
Authors’ information
K.N. is an assistant professor, and Z.M. is a professor at Fujita Health University Okazaki Medical Center. Both are board-certified surgeons of the Japan Surgical Society and the Japanese Society of Gastroenterological Surgery, board-certified gastroenterologists of the Japanese Society of Gastroenterology, and Fellows of the American College of Surgeons.
References
- Miura, R.; Okuya, K.; Akizuki, E.; Miyo, M.; Noda, A.; Ishii, M.; Ichihara, M.; Korai, T.; Toyota, M.; Ito, T.; et al. World-first report of low anterior resection for rectal cancer with the hinotori™ Surgical Robot System: a case report. Surgical case reports 2023, 9, 156. [Google Scholar] [CrossRef] [PubMed]
- Miyo, M.; Okita, K.; Okuya, K.; Ito, T.; Akizuki, E.; Ogawa, T.; Ishii, M.; Miura, R.; Ichihara, M.; Korai, T.; et al. Right hemicolectomy for ascending colon cancer using the hinotori surgical robot system: The first ever case report for colon cancer. Asian journal of endoscopic surgery 2023, 16, 604–607. [Google Scholar] [CrossRef] [PubMed]
- Ide, T.; Ito, K.; Tanaka, T.; Noshiro, H. Robotic distal pancreatectomy using a docking-free system (the hinotori™ Surgical Robot System). Surgical oncology 2023, 50, 101974. [Google Scholar] [CrossRef] [PubMed]
- Inoue, S.; Nakauchi, M.; Umeki, Y.; Suzuki, K.; Serizawa, A.; Akimoto, S.; Watanabe, Y.; Tanaka, T.; Shibasaki, S.; Inaba, K.; et al. First clinical experiences of robotic gastrectomy for gastric cancer using the hinotori™ surgical robot system. Surgical endoscopy 2024, 38, 1626–1636. [Google Scholar] [CrossRef]
- Katsuno, H.; Morohara, K.; Endo, T.; Chikaishi, Y.; Kikuchi, K.; Nakamura, K.; Matsuo, K.; Higashiguchi, T.; Koide, T.; Hanai, T.; et al. A new era in surgical oncology: preliminary insights into the hinotori™ surgical robot system's role in rectal surgery using the double bipolar method. World journal of surgical oncology 2024, 22, 215. [Google Scholar] [CrossRef]
- Kitadani, J.; Ojima, T.; Hayata, K.; Goda, T.; Takeuchi, A.; Tominaga, S.; Fukuda, N.; Nakai, T.; Nagano, S.; Kawai, M. Robotic gastrectomy using hinotori™ Surgical Robot System: Initial case series. Asian journal of endoscopic surgery 2024, 17, e13349. [Google Scholar] [CrossRef]
- Okui, N.; Kawasaki, Y.; Matsumoto, R.; Okumura, T.; Oi, H.; Idichi, T.; Yamasaki, Y.; Mataki, Y.; Ohtsuka, T. First report of surgery for congenital biliary dilatation using the hinotori™ Surgical Robot System (with video). Asian journal of endoscopic surgery 2024, 17, e13385. [Google Scholar] [CrossRef]
- Noshiro, H.; Ide, T.; Nomura, A.; Yoda, Y.; Hiraki, M.; Manabe, T. Introduction of a new surgical robot platform "hinotori™" in an institution with established da Vinci surgery™ for digestive organ operations. Surgical endoscopy 2024, 38, 3929–3939. [Google Scholar] [CrossRef]
- Tomihara, K.; Ide, T.; Ito, K.; Tanaka, T.; Noshiro, H. Robotic spleen-preserving distal pancreatectomy using the first domestic surgical robot platform (the hinotori™ Surgical Robot System): a case report. Surgical case reports 2024, 10, 22. [Google Scholar] [CrossRef]
- Sasaki, Y.; Kusuhara, Y.; Oyama, T.; Nishiyama, M.; Kobayashi, S.; Daizumoto, K.; Tomida, R.; Ueno, Y.; Fukawa, T.; Yamaguchi, K.; et al. Radical prostatectomy using the Hinotori robot-assisted surgical system: Docking-free design may contribute to reduction in postoperative pain. The international journal of medical robotics + computer assisted surgery : MRCAS 2024, 20, e2648. [Google Scholar] [CrossRef]
- Togami, S.; Higashi, T.; Tokudome, A.; Fukuda, M.; Mizuno, M.; Yanazume, S.; Kobayashi, H. The first report of surgery for gynecological diseases using the hinotori™ surgical robot system. Japanese journal of clinical oncology 2023, 53, 1034–1037. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Kakutani, S.; Fujii, Y.; Kimura, N.; Hakozaki, Y.; Kamei, J.; Taguchi, S.; Niimi, A.; Yamada, D.; Kume, H. Retzius-Sparing Robot-Assisted Radical Prostatectomy Using the Hinotori Surgical Robot System Platform: Report of the First Series of Experiences. Current oncology (Toronto, Ont.) 2024, 31, 5537–5543. [Google Scholar] [CrossRef] [PubMed]
- Morise, Z.; Kawabe, N.; Tomishige, H.; Nagata, H.; Kawase, J.; Arakawa, S.; Isetani, M. How Far Can We Go with Laparoscopic Liver Resection for Hepatocellular Carcinoma? Laparoscopic Sectionectomy of the Liver Combined with the Resection of the Major Hepatic Vein Main Trunk. BioMed research international 2015, 2015, 960752. [Google Scholar] [CrossRef] [PubMed]
- Makuuchi, M.; Kosuge, T.; Takayama, T.; Yamazaki, S.; Kakazu, T.; Miyagawa, S.; Kawasaki, S. Surgery for small liver cancers. Seminars in surgical oncology 1993, 9, 298–304. [Google Scholar] [CrossRef]
- Morise, Z. Revisiting the Institut Mutualiste Montsouris Difficulty Classification of Laparoscopic Liver Resection with the Data from a Personal Series-Evaluations for the Difficulty of Left Medial Sectionectomy and Length of Hospital Stay. Journal of personalized medicine 2024, 14. [Google Scholar] [CrossRef]
- Sijberden, J.P.; Hoogteijling, T.J.; Aghayan, D.; Ratti, F.; Tan, E.K.; Morrison-Jones, V.; Lanari, J.; Haentjens, L.; Wei, K.; Tzedakis, S.; et al. Robotic Versus Laparoscopic Liver Resection in Various Settings: An International Multicenter Propensity Score Matched Study of 10.075 Patients. Annals of surgery 2024, 280, 108–117. [Google Scholar] [CrossRef]
- Krenzien, F.; Schmelzle, M.; Pratschke, J.; Feldbrügge, L.; Liu, R.; Liu, Q.; Zhang, W.; Zhao, J.J.; Tan, H.L.; Cipriani, F.; et al. Propensity Score-Matching Analysis Comparing Robotic Versus Laparoscopic Limited Liver Resections of the Posterosuperior Segments: An International Multicenter Study. Annals of surgery 2024, 279, 297–305. [Google Scholar] [CrossRef]
- Görgec, B.; Zwart, M.; Nota, CL.; Bijlstra, OD.; Bosscha, K.; de Boer, MT.; de Wilde, RF.; Draaisma, WA.; Gerhards, MF.; Liem, MS.; et al. Implementation and Outcome of Robotic Liver Surgery in the Netherlands: A Nationwide Analysis. Annals of surgery 2023, 277, e1269–e1277. [Google Scholar] [CrossRef]
- Huang, XK.; Lu, WF.; Liu, SY.; Fu, TW.; Jin, L.; Du, CF.; Gao, ZY.; Wang, KD.; Dai, MG.; Zhong, ZH.; et al. Multicenter propensity score-matched analysis to compare perioperative morbidity after laparoscopic or robotic complex hepatectomy for solitary hepatocellular carcinoma. HPB (Oxford) 2024, 26, 1062–1071. [Google Scholar] [CrossRef]
- Winckelmans, T.; Wicherts, D.A.; Parmentier, I.; De Meyere, C.; Verslype, C.; D'Hondt, M. Robotic Versus Laparoscopic Hepatectomy: A Single Surgeon Experience of 629 Consecutive Minimally Invasive Liver Resections. World journal of surgery 2023, 47, 2241–2249. [Google Scholar] [CrossRef]
- Di Benedetto, F.; Magistri, P.; Di Sandro, S.; Sposito, C.; Oberkofler, C.; Brandon, E.; Samstein, B.; Guidetti, C.; Papageorgiou, A.; Frassoni, S.; et al. Safety and Efficacy of Robotic vs Open Liver Resection for Hepatocellular Carcinoma. JAMA Surgery 2023, 158, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Schmelzle, M.; Feldbrügge, L.; Ortiz Galindo, S.A.; Moosburner, S.; Kästner, A.; Krenzien, F.; Benzing, C.; Biebl, M.; Öllinger, R.; Malinka, T.; et al. Robotic vs. laparoscopic liver surgery: a single-center analysis of 600 consecutive patients in 6 years. Surgical endoscopy 2022, 36, 5854–5862. [Google Scholar] [CrossRef] [PubMed]
- Sucandy, I; Shapera, E; Syblis, CC; Crespo, K; Przetocki, VA; Ross, SB; Rosemurgy, AS. Propensity score matched comparison of robotic and open major hepatectomy for malignant liver tumors. Surgical endoscopy 2022, 36, 6724–6732. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Meng, L.; Yu, S.; Zheng, H.; Yu, L.; Wang, H.; Ren, H.; Li, H.; Zhang, X.; Wang, Z.; et al. Efficacy and safety of robotic versus laparoscopic liver resection for hepatocellular carcinoma: a propensity score-matched retrospective cohort study. Hepatology international 2024, 18, 1271–1285. [Google Scholar] [CrossRef] [PubMed]
- Fukumori, D.; Tschuor, C.; Hamada, T.; Schultz, NA.; Krohn, PS.; Burgdorf, S.; Penninga, L.; Storkholm, JH.; Pedersen, CR.; Hillingsø, J.; et al. Short-Term Surgical Outcomes After Robotic Liver Surgery: A Propensity-Score Matched Analysis With Conventional Open Liver Surgery at a High-Volume Centre in Denmark. The International Journal of Medical Robotics and Computer Assisted Surgery 2024, 20, e70003. [Google Scholar] [CrossRef]
- Steinkraus, KC.; Traub, B.; Heger, P.; Zaimi, M.; Mihaljevic, AL.; Michalski, CW.; Kornmann, M.; Hüttner, FJ. Results of robotic liver surgery in association with IWATE criteria - the first 100 cases. Langenbeck's Archives of Surgery 2024, 409, 50. [CrossRef]
- Chong, C.C.N.; Lok, H.T.; Fung, A.K.Y.; Fong, A.K.W.; Cheung, Y.S.; Wong, J.; Lee, K.F.; Lai, P.B.S. Robotic versus laparoscopic hepatectomy: application of the difficulty scoring system. Surgical endoscopy 2020, 34, 2000–2006. [Google Scholar] [CrossRef]
- Yang, HY.; Rho, SY.; Han, DH.; Choi, JS.; Choi, GH. Robotic major liver resections: Surgical outcomes compared with open major liver resections. Annals of hepato-biliary-pancreatic surgery 2021, 25, 8-17. [CrossRef]
- Kwak, B.J.; Lee, J.H.; Chin, K.M.; Syn, N.L.; Choi, S.H.; Cheung, T.T.; Chiow, A.K.H.; Sucandy, I.; Marino, M.V.; Prieto, M.; et al. Robotic versus laparoscopic liver resections for hepatolithiasis: an international multicenter propensity score matched analysis. Surgical endoscopy 2023, 37, 5855–5864. [Google Scholar] [CrossRef]
- Chen, W.; Zhang, X.; Jiang, J.; Ye, Y.; Zhai, Z.; Hu, W.; Li, X.; Chen, Y.; Chen, Y.; Hong, Y.; et al. Robotic versus laparoscopic liver resection in posterosuperior region: a retrospective study of consecutive cases. Surgical endoscopy 2023, 37, 4728–4736. [Google Scholar] [CrossRef]
- Birgin, E.; Heibel, M.; Hetjens, S.; Rasbach, E.; Reissfelder, C.; Téoule, P.; Rahbari, N.N. Robotic versus laparoscopic hepatectomy for liver malignancies (ROC'N'ROLL): a single-centre, randomised, controlled, single-blinded clinical trial. The Lancet regional health. Europe 2024, 43, 100972. [Google Scholar] [CrossRef]
- Rawal, N. Current issues in postoperative pain management. European journal of anaesthesiology 2016, 33, 160–171. [Google Scholar] [CrossRef]
- Long, Z.T.; Li, H.J.; Liang, H.; Wu, Y.C.; Ameer, S.; Qu, X.L.; Xiang, Z.Q.; Wang, Q.; Dai, X.M.; Zhu, Z. Robotic versus laparoscopic liver resection for liver malignancy: a systematic review and meta-analysis of propensity score-matched studies. Surgical endoscopy 2024, 38, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Kamarajah, S.K.; Bundred, J.; Manas, D.; Jiao, L.; Hilal, M.A.; White, S.A. Robotic versus conventional laparoscopic liver resections: A systematic review and meta-analysis. Scandinavian journal of surgery : SJS : official organ for the Finnish Surgical Society and the Scandinavian Surgical Society 2021, 110, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Abu Hilal, M.; Wakabayashi, G.; Han, H.S.; Palanivelu, C.; Boggi, U.; Hackert, T.; Kim, H.J.; Wang, X.Y.; Hu, M.G.; et al. International experts consensus guidelines on robotic liver resection in 2023. World journal of gastroenterology 2023, 29, 4815–4830. [Google Scholar] [CrossRef] [PubMed]
- Morise, Z.; Aldrighetti, L.; Belli, G.; Ratti, F.; Belli, A.; Cherqui, D.; Tanabe, M.; Wakabayashi, G. Laparoscopic repeat liver resection for hepatocellular carcinoma: a multicentre propensity score-based study. The British journal of surgery 2020, 107, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Nakauchi, M.; Suda, K.; Nakamura, K.; Tanaka, T.; Shibasaki, S.; Inaba, K.; Harada, T.; Ohashi, M.; Ohigashi, M.; Kitatsuji, H.; et al. Establishment of a new practical telesurgical platform using the hinotori™ Surgical Robot System: a preclinical study. Langenbeck's archives of surgery 2022, 407, 3783–3791. [Google Scholar] [CrossRef]
- Ebihara, Y.; Oki, E.; Hirano, S.; Takano, H.; Ota, M.; Morohashi, H.; Hakamada, K.; Urushidani, S.; Mori, M. Tele-assessment of bandwidth limitation for remote robotics surgery. Surgery today 2022, 52, 1653–1659. [Google Scholar] [CrossRef]
- Takahashi, Y.; Hakamada, K.; Morohashi, H.; Akasaka, H.; Ebihara, Y.; Oki, E.; Hirano, S.; Mori, M. Verification of delay time and image compression thresholds for telesurgery. Asian journal of endoscopic surgery 2023, 16, 255–261. [Google Scholar] [CrossRef]
- Teishima, J.; Wakita, N.; Bando, Y.; Okamura, Y.; Suzuki, K.; Hara, T.; Terakawa, T.; Chiba, K.; Matsushita, K.; Nakano, Y.; et al. Effects of modifying hinotori™ surgical robot system on perioperative outcome of robot-assisted radical prostatectomy. International journal of urology : official journal of the Japanese Urological Association 2024. [CrossRef]
Table 1.
The characteristics of the 10 cases.
Table 1.
The characteristics of the 10 cases.
| Case |
Sex |
Age |
BMI |
ASA |
Disease |
Operation |
T number |
T size (mm) |
LC/LF+/-PH |
Surg Hx |
Vessel dissection |
| 1 |
M |
77 |
28.5 |
2 |
HCC |
Partial resection (S4) |
1 |
20 |
LC |
1 |
1 |
| 2 |
F |
60 |
31.2 |
2 |
HCC |
Partial resection (S5-6) |
1 |
14 |
LC+PH |
0 |
1 |
| 3 |
M |
69 |
24 |
2 |
hepatolithiasis |
Lt hemihepatectomy+C |
0 |
0 |
- |
0 |
1 |
| 4 |
M |
73 |
24 |
3 |
HCC |
Partial resection (S4) |
1 |
33 |
LC+PH |
0 |
1 |
| 5 |
M |
74 |
30.2 |
2 |
HCC |
Partial resection (S5)+C |
1 |
50 |
LF |
0 |
1 |
| 6 |
F |
72 |
15.2 |
3 |
met (pancreatic cancer) |
Partial resection (S3-4) |
1 |
10 |
- |
1 |
0 |
| 7 |
M |
67 |
22 |
3 |
met (rectal cancer) |
Ext left medial sectionectomy+C |
2 |
25 |
- |
1 |
1 |
| 8 |
M |
62 |
26.6 |
2 |
HCC |
Partial resection (S7-8d) |
2 |
10 |
LC |
1 |
0 |
| 9 |
M |
69 |
20.2 |
2 |
met (rectal cancer) |
Partial resection (S2,2,6,6,8) |
5 |
17 |
- |
1 |
0 |
| 10 |
F |
71 |
21.9 |
2 |
HCC |
Partial resection (S7-8d)+C |
2 |
11 |
LC+PH |
0 |
0 |
Table 2.
The short-term outcomes of the 10 cases.
Table 2.
The short-term outcomes of the 10 cases.
| Case |
Ope time |
Blood loss |
conversion |
LOS(day) |
Morbidity (II or above) |
| 1 |
260 |
26 |
0 |
5 |
0 |
| 2 |
327 |
80 |
0 |
7 |
0 |
| 3 |
577 |
330 |
0 |
7 |
0 |
| 4 |
433 |
212 |
0 |
7 |
0 |
| 5 |
402 |
1253 |
0 |
8 |
0 |
| 6 |
331 |
91 |
0 |
7 |
0 |
| 7 |
497 |
222 |
0 |
8 |
1 |
| 8 |
743 |
649 |
0 |
23 |
0 |
| 9 |
425 |
330 |
0 |
9 |
0 |
| 10 |
414 |
4081 |
1 |
9 |
0 |
Table 3.
Recent reports for short-term outcomes of robot-assisted liver resection [
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31].
Table 3.
Recent reports for short-term outcomes of robot-assisted liver resection [
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31].
| Author (year, number of case) |
Ope time (minutes) |
Blood loss (ml) |
Conversion (%) |
LOS (day) |
Mobidity (%) |
| Sijberden JP (2024,1507) |
190 (139–272) |
100 (50–280) |
3% |
4 (3–6) |
19% (III or above=6%) |
| Krenzien F (2024,461) |
189 (140–271) |
100 (50–200) |
2% |
5 (3–6) |
20% (III or above=6%) |
| Görgec B (2023,400) |
NA |
150 (50–350) |
6% |
4 (2–5) |
19% (III or above=7%) |
| Huang XK (2024,385) |
NA |
NA |
NA |
10 (3–59) |
47% (III or above=23%) |
| Winckelmans T (2023,177) |
145 (118-190) |
30 (10-90) |
1% |
3 (1-3) |
14% (III or above=7%) |
| Di Benedetto F (2023,158) |
290 (190-380) |
200 (100-500) |
3% |
4 (3-6) |
54% (III or above=6%) |
| Schmelzle M (2022,129) |
260 (83–568) |
NA |
5% |
8 (4–94) |
38% (III or above=23%) |
| Sucandy I (2022,125) |
296 +/- 117 |
253 +/- 254 |
NA |
5 +/- 3 |
6% (II or above=6%, III or above=1%) |
| Li H (2024,107) |
212 (153–300) |
100 (50–300) |
3% |
8 (7–9.5) |
II or above=4% |
| Fukumori D (2024,100) |
261 +/- 113 |
194 +/- 223 |
1% |
4 +/- 3 |
8% (III or above=5%) |
| Steinkraus KC (2024,100) |
180 (IQR 128.7) |
300 (IQR 550) |
6% |
6 (IQR4) |
21% (III or above=13%) |
| Chong CN (2020,91) |
259 +/- 127 |
275 +/- 568 |
8% |
4.8 +/- 1.8 |
10% (III or above=3%) |
| Yang HY (2021,70) |
472 +/- 203 |
270 +/- 354 |
7% |
10 +/- 6 |
31% (II or above=27%, III or above=3%) |
| Kwak BJ (2023,63) |
233 (188–305) |
100 (50–200) |
2% |
6 (5-8) |
27% (III or above=13%) |
| Chen W (2023,48) |
160 +/- 62 |
92 +/- 86 |
6% |
5.4 +/- 1.6 |
42% (II or above=35%, III or above=15%) |
| Birgin E (2024,41) |
223 (122 – 380) |
300 (100 – 500) |
5% |
5 (4 – 7) |
29% (III or above=0%) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).