Submitted:
08 December 2024
Posted:
10 December 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
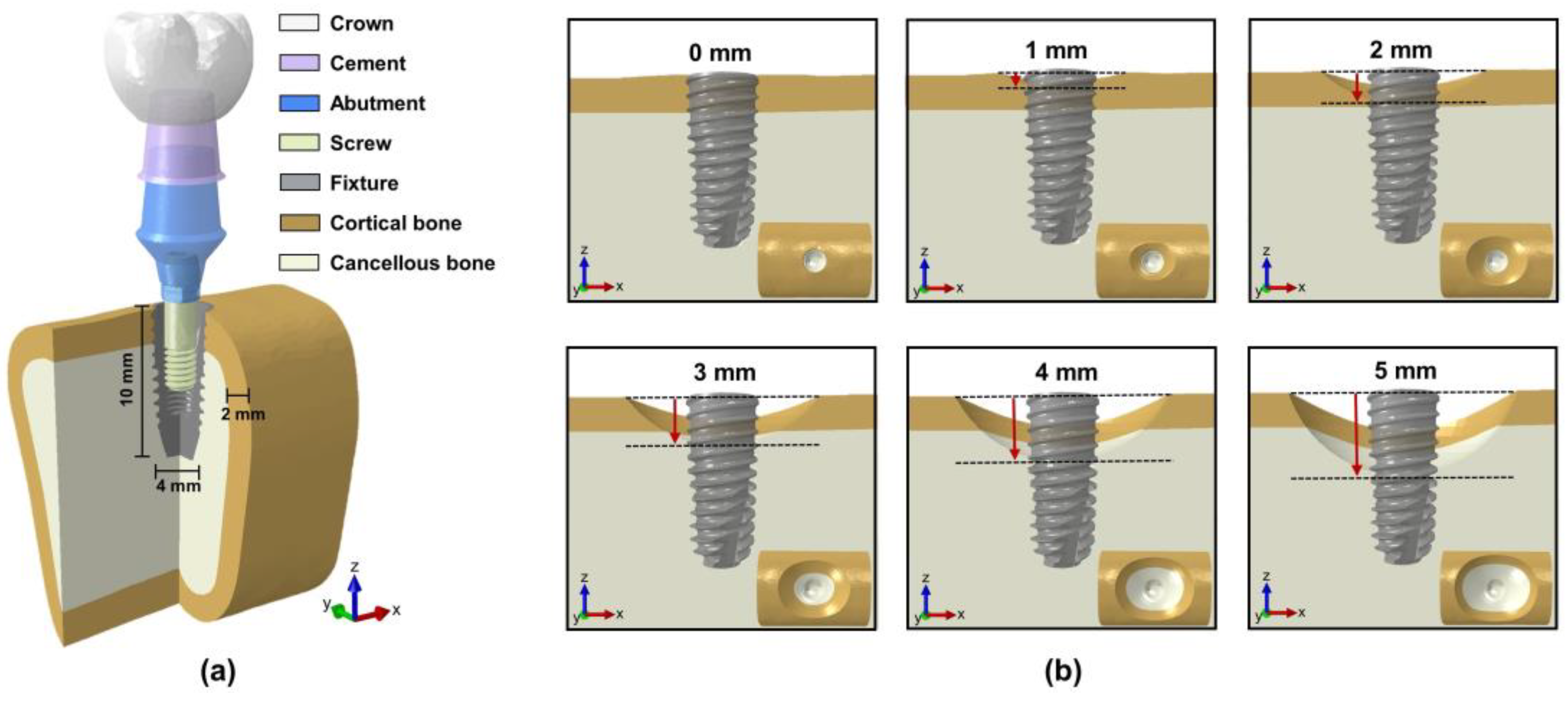
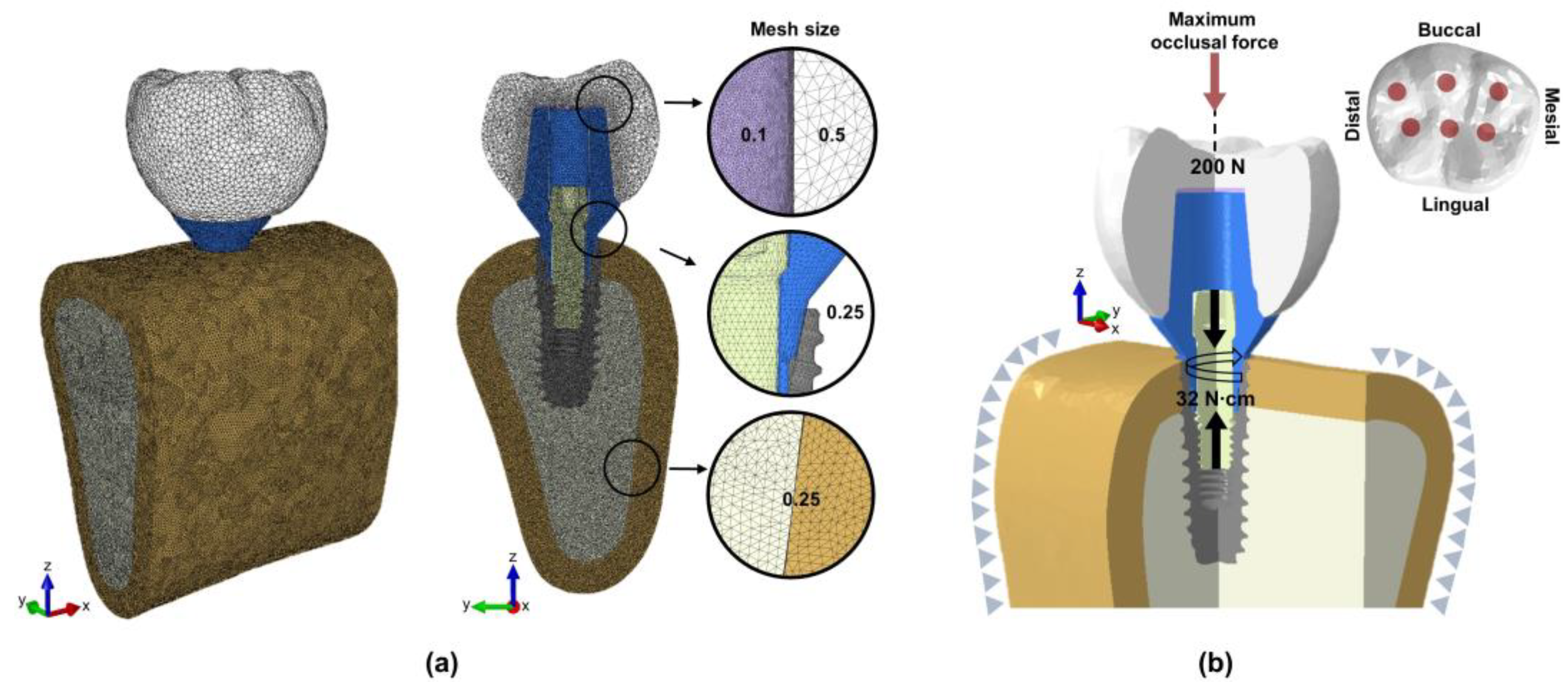
2. Materials and Methods
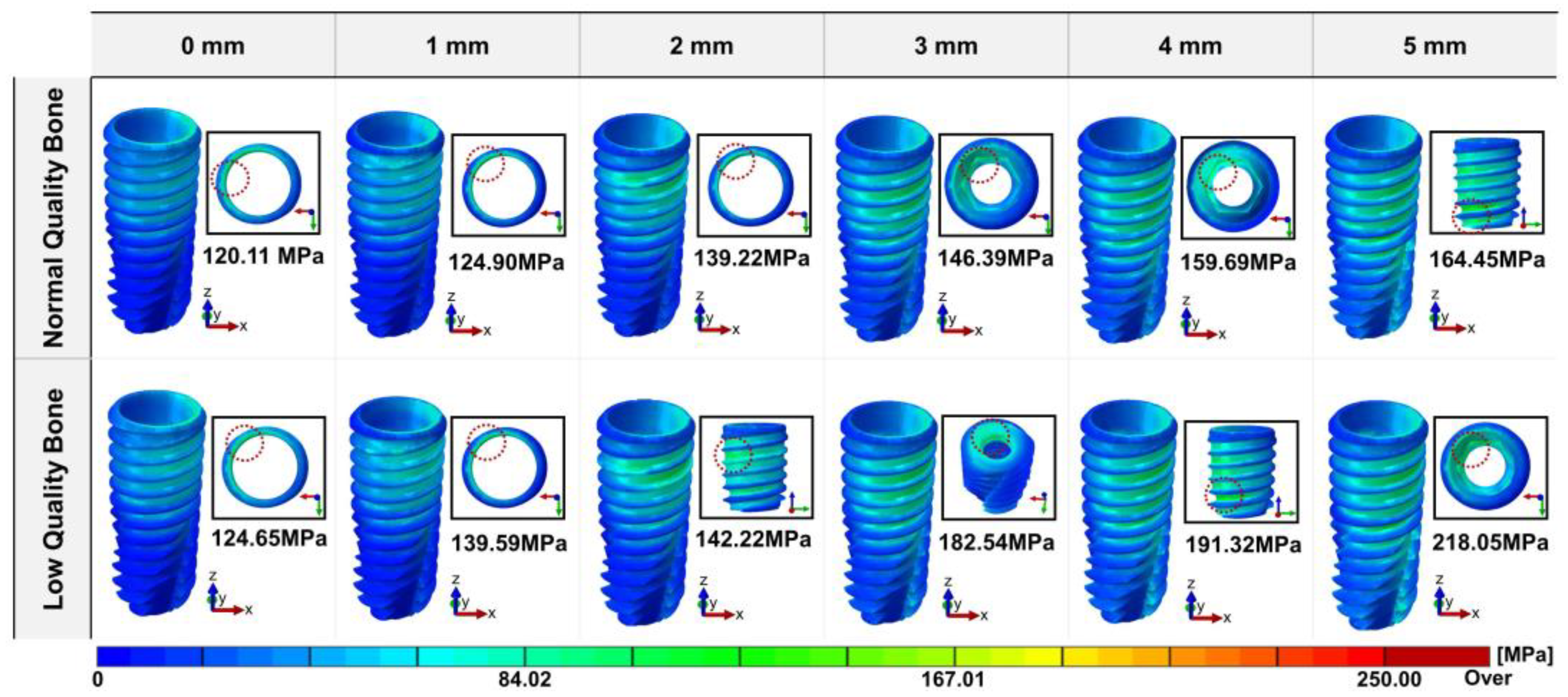
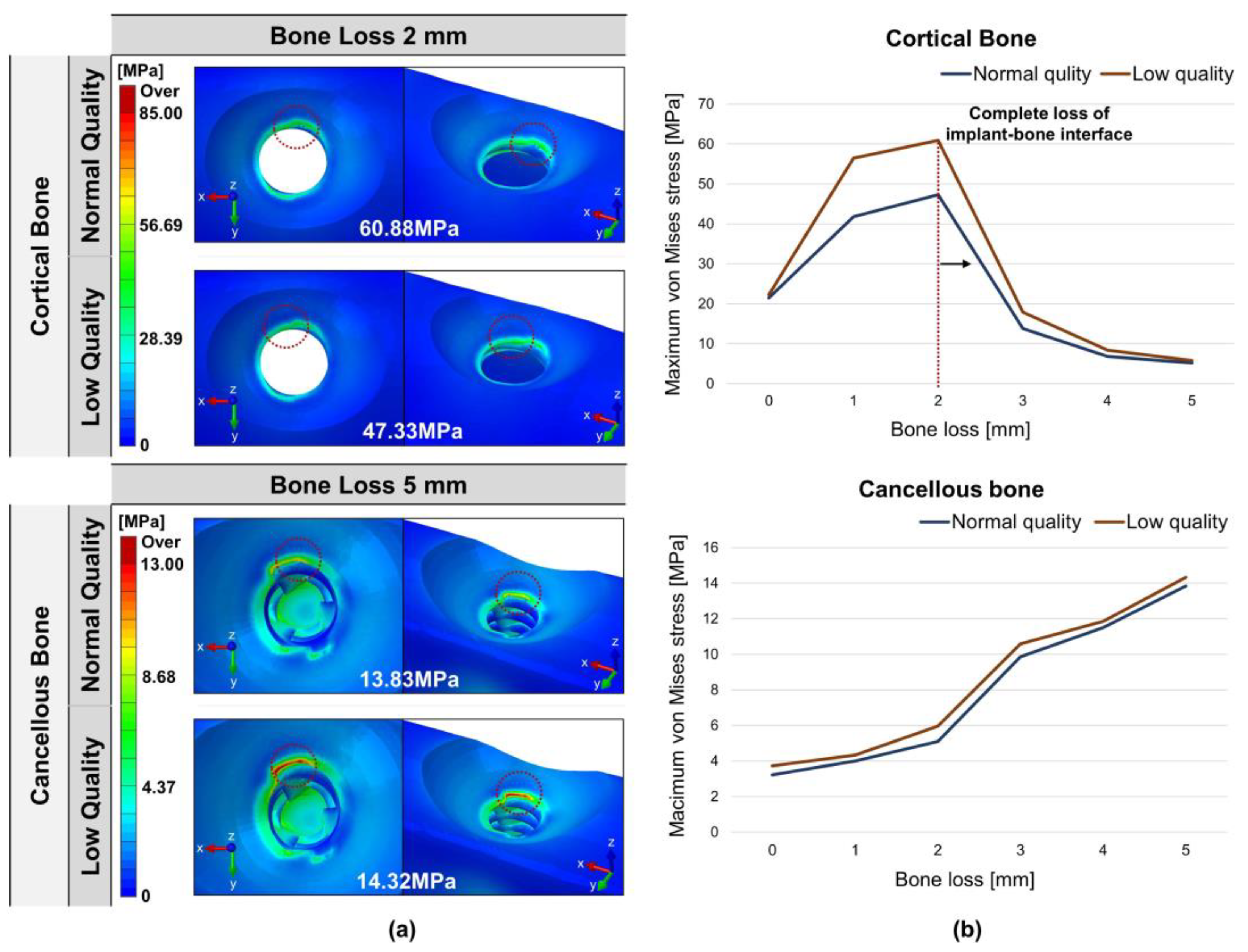
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Galindo-Moreno, P.; León-Cano, A.; Ortega-Oller, I.; Monje, A.; O'Valle, F.; Catena, A. Marginal bone loss as success criterion in implant dentistry: beyond 2 mm. Clin Oral Implan Res 2015, 26, e28–e34. [Google Scholar] [CrossRef] [PubMed]
- De Bruyn, H.; Christiaens, V.; Doornewaard, R.; Jacobsson, M.; Cosyn, J.; Jacquet, W.; Vervaeke, S. Implant surface roughness and patient factors on long-term peri-implant bone loss. Periodontol 2000 2017, 73, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Caricasulo, R.; Malchiodi, L.; Ghensi, P.; Fantozzi, G.; Cucchi, A. The influence of implant-abutment connection to peri-implant bone loss: A systematic review and meta-analysis. Clin Implant Dent Relat Res 2018, 20, 653–664. [Google Scholar] [CrossRef]
- Rokaya, D.; Srimaneepong, V.; Wisitrasameewon, W.; Humagain, M.; Thunyakitpisal, P. Peri-implantitis Update: Risk Indicators, Diagnosis, and Treatment. Eur J Dent 2020, 14, 672–682. [Google Scholar] [CrossRef]
- Vervaeke, S.; Collaert, B.; Cosyn, J.; Deschepper, E.; De Bruyn, H. A multifactorial analysis to identify predictors of implant failure and peri-implant bone loss. Clin Implant Dent Relat Res 2015, 17 Suppl 1, e298–307. [Google Scholar] [CrossRef]
- Jokar, H.; Rouhi, G.; Abolfathi, N. The Effects of Splinting on the Initial Stability and Displacement Pattern of Periodontio-Integrated Dental Implants: A Finite Element Investigation. J Med Biol Eng 2020, 40, 719–726. [Google Scholar] [CrossRef]
- Linetskiy, I.; Demenko, V.; Linetska, L.; Yefremov, O. Impact of annual bone loss and different bone quality on dental implant success - A finite element study. Comput Biol Med 2017, 91, 318–325. [Google Scholar] [CrossRef]
- Bing, L.; Mito, T.; Yoda, N.; Sato, E.; Shigemitsu, R.; Han, J.M.; Sasaki, K. Effect of peri-implant bone resorption on mechanical stress in the implant body: In vivo measured load-based finite element analysis. J Oral Rehabil 2020, 47, 1566–1573. [Google Scholar] [CrossRef]
- Lemos, C.A.A.; Verri, F.R.; Noritomi, P.Y.; Kemmoku, D.T.; Souza Batista, V.E.; Cruz, R.S.; de Luna Gomes, J.M.; Pellizzer, E.P. Effect of bone quality and bone loss level around internal and external connection implants: A finite element analysis study. J Prosthet Dent 2021, 125, 137–e131. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Souza Dos Santos Vianna, M.; Dedavid, B.A. Influence of bone insertion level of the implant on the fracture strength of different connection designs: an in vitro study. Clin Oral Investig 2014, 18, 715–720. [Google Scholar] [CrossRef]
- Tsouknidas, A.; Lympoudi, E.; Michalakis, K.; Giannopoulos, D.; Michailidis, N.; Pissiotis, A.; Fytanidis, D.; Kugiumtzis, D. Influence of Alveolar Bone Loss and Different Alloys on the Biomechanical Behavior of Internal-and External-Connection Implants: A Three-Dimensional Finite Element Analysis. Int J Oral Maxillofac Implants 2015, 30, e30–e42. [Google Scholar] [CrossRef] [PubMed]
- Merheb, J.; Temmerman, A.; Rasmusson, L.; Kubler, A.; Thor, A.; Quirynen, M. Influence of Skeletal and Local Bone Density on Dental Implant Stability in Patients with Osteoporosis. Clin Implant Dent Relat Res 2016, 18, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Moriyama, Y.; Takemura, Y.; Rokuta, M.; Ayukawa, Y. Influence of osteoporosis and mechanical loading on bone around osseointegrated dental implants: A rodent study. J Mech Behav Biomed Mater 2021, 123, 104771. [Google Scholar] [CrossRef]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Romanos, G.E.; Delgado-Ruiz, R.A.; Sacks, D.; Calvo-Guirado, J.L. Influence of the implant diameter and bone quality on the primary stability of porous tantalum trabecular metal dental implants: an in vitro biomechanical study. Clin Oral Implants Res 2018, 29, 649–655. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone Quality and Quantity and Dental Implant Failure: A Systematic Review and Meta-analysis. Int J Prosthodont 2017, 30, 219–237. [Google Scholar] [CrossRef]
- Lombardi, T.; Berton, F.; Salgarello, S.; Barbalonga, E.; Rapani, A.; Piovesana, F.; Gregorio, C.; Barbati, G.; Di Lenarda, R.; Stacchi, C. Factors Influencing Early Marginal Bone Loss around Dental Implants Positioned Subcrestally: A Multicenter Prospective Clinical Study. J Clin Med 2019, 8. [Google Scholar] [CrossRef]
- Pontes, A.E.; Ribeiro, F.S.; da Silva, V.C.; Margonar, R.; Piattelli, A.; Cirelli, J.A.; Marcantonio, E., Jr. Clinical and radiographic changes around dental implants inserted in different levels in relation to the crestal bone, under different restoration protocols, in the dog model. J Periodontol 2008, 79, 486–494. [Google Scholar] [CrossRef]
- Nimbalkar, S.; Dhatrak, P.; Gherde, C.; Joshi, S. A review article on factors affecting bone loss in dental implants. Mater Today-Proc 2021, 43, 970–976. [Google Scholar] [CrossRef]
- Do, T.A.; Le, H.S.; Shen, Y.W.; Huang, H.L.; Fuh, L.J. Risk Factors related to Late Failure of Dental Implant-A Systematic Review of Recent Studies. Int J Environ Res Public Health 2020, 17. [Google Scholar] [CrossRef]
- Geng, J.P.; Tan, K.B.; Liu, G.R. Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent 2001, 85, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Winter, W.; Klein, D.; Karl, M. Effect of model parameters on finite element analysis of micromotions in implant dentistry. J Oral Implantol 2013, 39, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Kayabasi, O.; Yüzbasioglu, E.; Erzincanli, F. Static, dynamic and fatigue behaviors of dental implant using finite element method. Adv Eng Softw 2006, 37, 649–658. [Google Scholar] [CrossRef]
- Goiato, M.C.; Andreotti, A.M.; Dos Santos, D.M.; Nobrega, A.S.; de Caxias, F.P.; Bannwart, L.C. Influence of length, diameter and position of the implant in its fracture incidence: A Systematic Review. J Dent Res Dent Clin Dent Prospects 2019, 13, 109–116. [Google Scholar] [CrossRef]
- Gupta, S.; Goyal, P.; Jain, A.; Chopra, P. Effect of peri-implantitis associated horizontal bone loss on stress distribution around dental implants - A 3D finite element analysis. Mater Today-Proc 2020, 28, 1503–1509. [Google Scholar] [CrossRef]
- Gupta, S.; Chopra, P.; Goyal, P.; Jain, A. Effect of vertical bone loss on stress distribution at the bone-implant interface around implants of varying diameters-an in silico 3D finite element analysis. Mater Today-Proc 2021, 45, 4581–4586. [Google Scholar] [CrossRef]
- Satpathy, M.; Duan, Y.; Betts, L.; Priddy, M.; Griggs, J.A. Effect of Bone Remodeling on Dental Implant Fatigue Limit Predicted Using 3D Finite Element Analysis. J Dent Oral Epidemiol 2022, 2. [Google Scholar] [CrossRef]
- Su, Y.H.; Peng, B.Y.; Wang, P.D.; Feng, S.W. Evaluation of the implant stability and the marginal bone level changes during the first three months of dental implant healing process: A prospective clinical study. J Mech Behav Biomed 2020, 110. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J Clin Periodontol 2018, 45 Suppl 20, S246–S266. [Google Scholar] [CrossRef]
- Oh, T.J.; Yoon, J.; Misch, C.E.; Wang, H.L. The causes of early implant bone loss: myth or science? J Periodontol 2002, 73, 322–333. [Google Scholar] [CrossRef]
- Liu, M.; Wang, S.; Chen, H.; Liu, Y. A pilot study of a deep learning approach to detect marginal bone loss around implants. BMC Oral Health 2022, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Park, J.; Kang, I.; Lee, H.; Noh, G. Effects of assessing the bone remodeling process in biomechanical finite element stability evaluations of dental implants. Comput Meth Prog Bio 2022, 221. [Google Scholar] [CrossRef] [PubMed]
- Santiago, J.F.; Verri, F.R.; Almeida, D.A.D.; Batista, V.E.D.; Lemos, C.A.A.; Pellizzer, E.P. Finite element analysis on influence of implant surface treatments, connection and bone types. Mat Sci Eng C-Mater 2016, 63, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Sugiura, T.; Yamamoto, K.; Horita, S.; Murakami, K.; Tsutsumi, S.; Kirita, T. The effects of bone density and crestal cortical bone thickness on micromotion and peri-implant bone strain distribution in an immediately loaded implant: a nonlinear finite element analysis. J Periodontal Implan 2016, 46, 152–165. [Google Scholar] [CrossRef]
- Vaillancourt, H.; Pilliar, R.M.; Mccammond, D. Finite-Element Analysis of Crestal Bone Loss around Porous-Coated Dental Implants. J Appl Biomater 1995, 6, 267–282. [Google Scholar] [CrossRef]
- Niinomi, M. Mechanical properties of biomedical titanium alloys. Mat Sci Eng a-Struct 1998, 243, 231–236. [Google Scholar] [CrossRef]
- Tolidis, K.; Papadogiannis, D.; Papadogiannis, Y.; Gerasimou, P. Dynamic and static mechanical analysis of resin luting cements. J Mech Behav Biomed 2012, 6, 1–8. [Google Scholar] [CrossRef]
- Anitua, E.; de Ibarra, N.L.S.; Martín, I.M.; Rotaeche, L.S. Influence of Dental Implant Diameter and Bone Quality on the Biomechanics of Single-Crown Restoration. A Finite Element Analysis. Dent J-Basel 2021, 9. [Google Scholar] [CrossRef]
- Torcato, L.B.; Pellizzer, E.P.; Verri, F.R.; Falcón-Antenucci, R.M.; Santiago, J.F.; Almeida, D.A.D. Influence of parafunctional loading and prosthetic connection on stress distribution: A 3D finite element analysis. Journal of Prosthetic Dentistry 2015, 114, 644–651. [Google Scholar] [CrossRef]
- Lee, H.; Jo, M.; Sailer, I.; Noh, G. Effects of implant diameter, implant-abutment connection type, and bone density on the biomechanical stability of implant components and bone: A finite element analysis study. Journal of Prosthetic Dentistry 2022, 128, 716–728. [Google Scholar] [CrossRef]
- Frost, H.M. The mechanostat: a proposed pathogenic mechanism of osteoporoses and the bone mass effects of mechanical and nonmechanical agents. Bone Miner 1987, 2, 73–85. [Google Scholar] [PubMed]
- Mattheos, N.; Janda, M.; Acharya, A.; Pekarski, S.; Larsson, C. Impact of design elements of the implant supracrestal complex (ISC) on the risk of peri-implant mucositis and peri-implantitis: A critical review. Clin Oral Implants Res 2021, 32 Suppl 21, 181–202. [Google Scholar] [CrossRef]
- Bragger, U.; Hirt-Steiner, S.; Schnell, N.; Schmidlin, K.; Salvi, G.E.; Pjetursson, B.; Matuliene, G.; Zwahlen, M.; Lang, N.P. Complication and failure rates of fixed dental prostheses in patients treated for periodontal disease. Clin Oral Implants Res 2011, 22, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.B.; Wu, T.X.; Guo, Y.C.; Zhou, X.D.; Lei, Y.L.; Xu, X.; Mo, A.C.; Wang, Y.Y.; Yuan, Q. Marginal bone loss around non-submerged implants is associated with salivary microbiome during bone healing. Int J Oral Sci 2017, 9, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Ravidà, A.; Samal, A.; Qazi, M.; Webber, L.P.; Wang, H.L.; Galindo-Moreno, P.; Borgnakke, W.S.; Saleh, M.H.A. Interproximal implant thread exposure after initial bone remodeling as a risk indicator for peri-implantitis. J Periodontol 2023, 94, 751–764. [Google Scholar] [CrossRef]
- Trombelli, L.; Farina, R.; Tomasi, C.; Vignoletti, F.; Paolantoni, G.; Giordano, F.; Ortensi, L.; Simonelli, A. Factors affecting radiographic marginal bone resorption at dental implants in function for at least 5 years: A multicenter retrospective study. Clin Oral Implan Res 2024, 35, 1406–1417. [Google Scholar] [CrossRef]
- Jin, Z.H.; Peng, M.D.; Li, Q. The effect of implant neck microthread design on stress distribution of peri-implant bone with different level: A finite element analysis. J Dent Sci 2020, 15, 466–471. [Google Scholar] [CrossRef]
- Ercal, P.; Taysi, A.E.; Ayvalioglu, D.C.; Eren, M.M.; Sismanoglu, S. Impact of peri-implant bone resorption, prosthetic materials, and crown to implant ratio on the stress distribution of short implants: a finite element analysis. Med Biol Eng Comput 2021, 59, 813–824. [Google Scholar] [CrossRef]
- Yoon, Y.; Kang, I.; Noh, G.; Kwon, Y.D. Biomechanical analysis of alveolar bones with compromised quality supporting a 4-unit implant bridge; a possible association with implant-related sequestration (IRS). Clin Oral Invest 2024, 28. [Google Scholar] [CrossRef]
- Valera-Jimenez, J.F.; Burgueno-Barris, G.; Gomez-Gonzalez, S.; Lopez-Lopez, J.; Valmaseda-Castellon, E.; Fernandez-Aguado, E. Finite element analysis of narrow dental implants. Dent Mater 2020, 36, 927–935. [Google Scholar] [CrossRef]
- Falcinelli, C.; Valente, F.; Vasta, M.; Traini, T. Finite element analysis in implant dentistry: State of the art and future directions. Dent Mater 2023, 39, 539–556. [Google Scholar] [CrossRef] [PubMed]
- Mehboob, H.; Ouldyerou, A.; Ijaz, M.F. Biomechanical Investigation of Patient-Specific Porous Dental Implants: A Finite Element Study. Appl Sci-Basel 2023, 13. [Google Scholar] [CrossRef]
- Callea, C.; Ceddia, M.; Piattelli, A.; Specchiulli, A.; Trentadue, B. Finite Element Analysis (FEA) for a Different Type of Cono-in Dental Implant. Appl Sci-Basel 2023, 13. [Google Scholar] [CrossRef]
- Han, J.Y.; Sun, Y.C.; Wang, C. Effect of Integration Patterns Around Implant Neck on Stress Distribution in Peri-Implant Bone: A Finite Element Analysis. J Prosthodont 2017, 26, 549–558. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Cappare, P.; Barbon, S.; Gherlone, E.F. Stability of Dental Implants and Thickness of Cortical Bone: Clinical Research and Future Perspectives. A Systematic Review. Materials 2021, 14. [Google Scholar] [CrossRef]
- Ausiello, P.; Tribst, J.P.M.; Ventre, M.; Salvati, E.; di Lauro, A.E.; Martorelli, M.; Lanzotti, A.; Watts, D.C. The role of cortical zone level and prosthetic platform angle in dental implant mechanical response: A 3D finite element analysis. Dental Materials 2021, 37, 1688–1697. [Google Scholar] [CrossRef]
- Cervino, G.; Romeo, U.; Lauritano, F.; Bramanti, E.; Fiorillo, L.; D'Amico, C.; Milone, D.; Laino, L.; Campolongo, F.; Rapisarda, S.; Cicciu, M. Fem and Von Mises Analysis of OSSTEM ((R)) Dental Implant Structural Components: Evaluation of Different Direction Dynamic Loads. Open Dent J 2018, 12, 219–229. [Google Scholar] [CrossRef]
- Elsayyad, A.A.; Abbas, N.A.; AbdelNabi, N.M.; Osman, R.B. Biomechanics of 3-implant-supported and 4-implant-supported mandibular screw-retained prostheses: A 3D finite element analysis study. Journal of Prosthetic Dentistry 2020, 124. [Google Scholar] [CrossRef]
| Composition of the model | Bone loss [mm] | Number of nodes | Number of elements | Mesh size [mm] |
|---|---|---|---|---|
| Cortical bone | 0 | 606119 | 3633156 | 0.25 |
| 1 | 603468 | 3616165 | ||
| 2 | 591059 | 3541116 | ||
| 3 | 571075 | 3417231 | ||
| 4 | 553668 | 3310603 | ||
| 5 | 537707 | 3212930 | ||
| Cancellous bone | 0-2 | 649562 | 4008793 | |
| 3 | 648601 | 4003423 | ||
| 4 | 637906 | 3937101 | ||
| 5 | 618668 | 3817243 | ||
| Crown | 43999 | 257435 | 0.25–0.5 | |
| Cement | 59496 | 215191 | 0.1 | |
| Abutment | 39671 | 224617 | 0.25 | |
| Screw | 9396 | 47628 | ||
| Fixture | 25835 | 130287 | ||
| Composition of the model | Young’s modulus [MPa] | Poisson’s ratio | Reference | |
|---|---|---|---|---|
| Cortical bone | Normal quality | 13700 | 0.3 | [34] |
| Low quality | 4140 | |||
| Cancellous bone | Normal quality | 1370 | ||
| Low quality | 259 | |||
| All-ceramic crown | 140000 | 0.28 | [35] | |
| Titanium * | 110000 | 0.34 | [36] | |
| Temporary cement | 10760 | 0.35 | [37] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





