Keywords: ERA; Sildenafil; Tadalafil; pharmacokinetics
Background:
Combination therapy, which involves targeting multiple pathogenic pathways, is now widely accepted as the standard of care for pulmonary arterial hypertension (PAH). Extensive support from randomized controlled trials (RCTs) and observational studies has solidified this approach. According to the European Society of Cardiology/European Respiratory Society (ESC/ERS) guidelines on pulmonary hypertension (PH), both initial and sequential combination therapy play a significant role in treatment[
1].
The two most exploited pathways are the endothelin (Endothelin receptor antagonist/ERA) and the nitric oxide pathway, and the most popular regimens used within these pathways, are Bosentan combined with Sildenafil[
2].
From a molecular and pharmacokinetic point of view, CYP3A4 induction, decreases sildenafil levels; sildenafil is a substrate of CYP3A4 competing with metabolism of Bosentan (also CYP3A4 substrate), resulting in increased bosentan levels with increased risk of hepatotoxicity and decreased desired effect on pulmonary vascular resistance[
3].
There is intriguingly very scarce research comparing the effectiveness of Bosentan-Sildenafil vs. Bosentan-Taladafil in control of pulmonary hypertension, and no meta-analysis has been performed on the available results.
This review aims at investigating which of the two regimens shows a better control of pulmonary hypertension, by gathering the available continuous data, and performing a meta-analysis on it.
Methodology
A thorough online literature search was performed to identify relevant primary research articles on the topic, utilizing databases such as Pubmed, Embase, Clarivate Analytics/Web of Science Core Collection, and Wiley/Cochrane Library. The search covered literature published up to July 2024 and focused on key terms associated with dual therapy for pulmonary hypertension.
Only articles published in English were included, consisting of guidelines, clinical trials, and retrospective studies. The selected studies provided data comparing ERA+Sildenafil to ERA and Tadalafil.
The two authors reviewed all potentially relevant titles and abstracts for eligibility and checked the full text of articles when necessary. The inclusion criteria stipulated that studies must: (1) compare the two specified treatment regimens, and (2) measure pulmonary vascular resistance and mean pulmonary artery pressure through invasive catheterization in both treatment approaches. Exclusions were made for: studies involving the two treatment regimens but lacking data that did not assess pulmonary pressure or pulmonary vascular resistance through invasive catheterization.
Statistical Analysis:
The final statistical outcome of this study was to construct a Forest Plot, to determine if there is any statistical significance in terms of pulmonary vascular resistance and mPAP between the ERA+Sildenafil group vs. ERA+Tadalafil group. MedCalc (Trial version) has been used, and meta-analysis function of continuous variables were used, where the ERA+Tadalafil group was chosen as the intervention group and ERA+Sildenafil group was used as the control group. In one of the two studies included ERA+Sildenafil and ERA+Tadalafil groups were split into subgroups according to the type of ERA used, which necessitated the calculation of the weighted mean and standard deviation from the subgroups of analysis[
4].
Results:
Our literature review yielded only two studies [
5,
6], retrospective in nature, no clinical trials were found to compare ERA+Sildenafil (ERA-S) vs. ERA+Tadalafil (ERA-T).
The two studies included collectively a total of 62 patients receiving the ERA+Tadalafil regimen, vs. 160 on the ERA+Sildenafil combination therapy. Only one of the two studies (Sitbon et al), reported the baseline pulmonary invasive hemodynamics before the start of treatment, while Grunig only showed the pulmonary pressures and vascular resistance on therapy.
We decided to compare the mean pulmonary pressure (mPAP) by cardiac catheterization (in mmHg) and the pulmonary vascular resistance (PVR), expressed in dynes × s × cm–5, in both study groups.
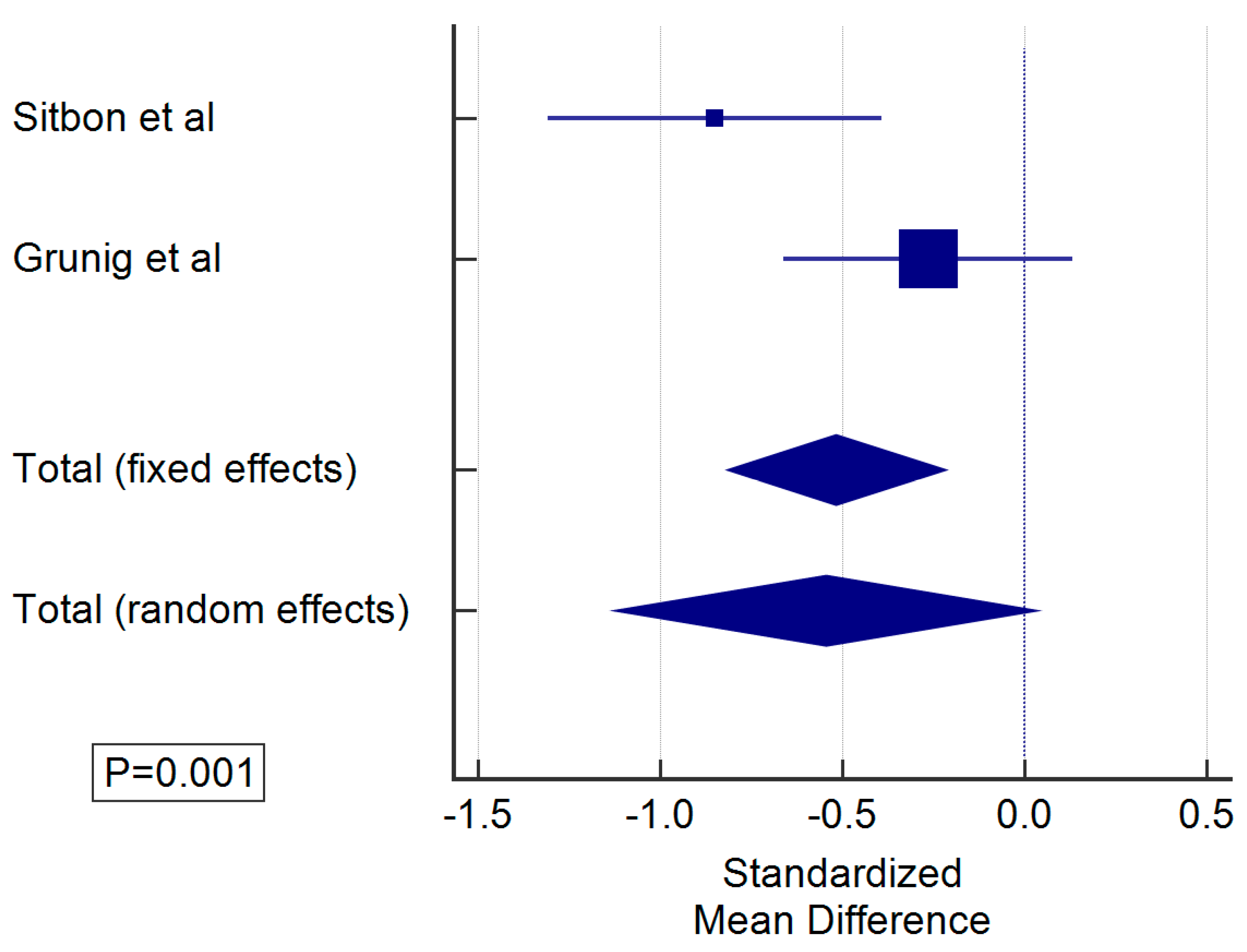
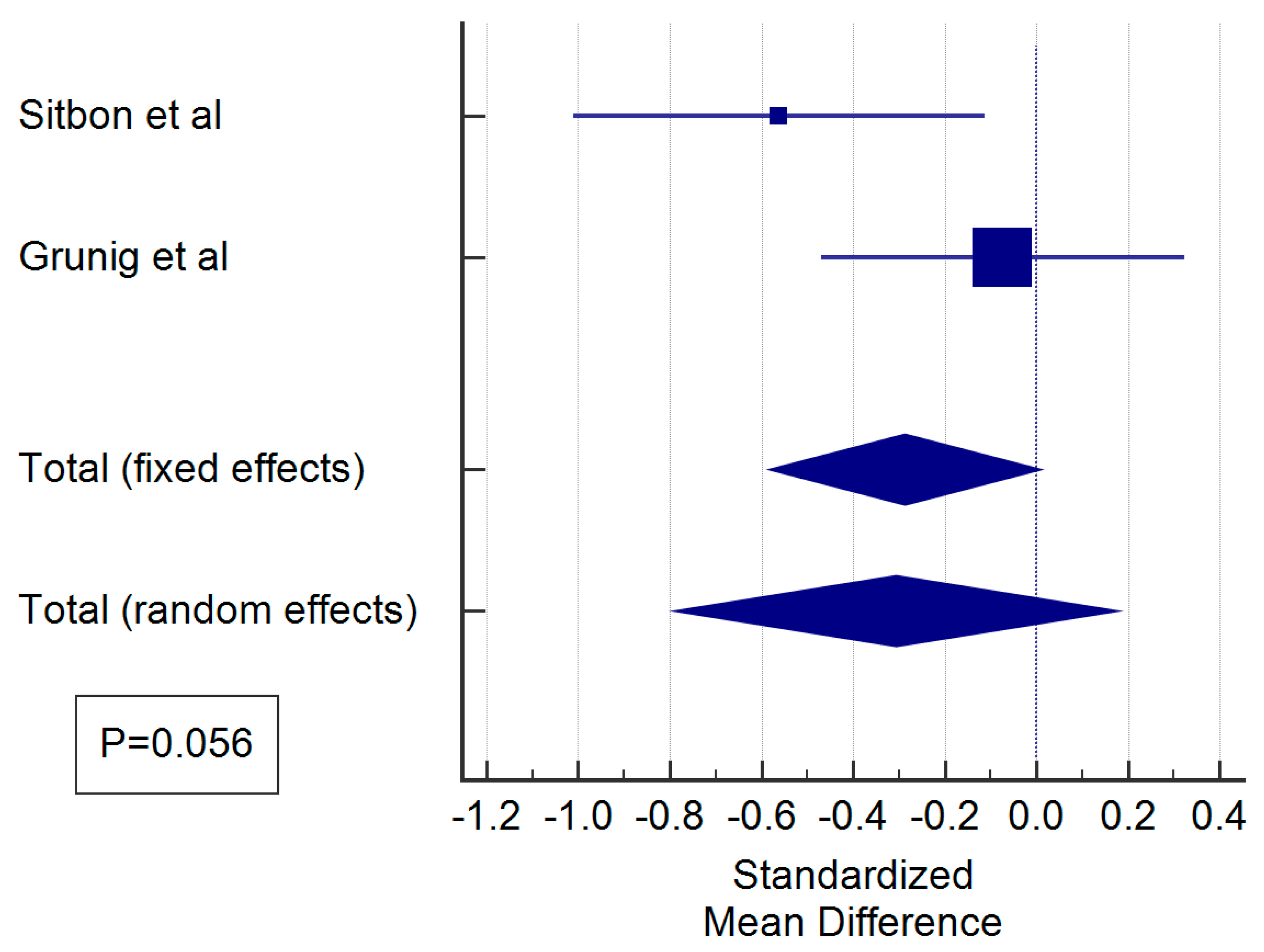
This was illustrated using a Forest plot for continuous variables in
Figure 1 (mPAP), and
Figure 2 (for PVR).
Figure 1 showed a significant difference in mPAP between the two groups in favor of the ERA+Tadalafil group.
Figure 2 displays the discrepancy in PVR between the two treatment regimens, and despite a difference in PVR in Sitbon et al report, the difference was less evident Grunig series, and the total effect was not statistically significant with a P value of 0.056.
Abbreviations: ERA: endothelin receptor antagonist, mPAP: mean pulmonary artery pressure
Abbreviations: ERA: endothelin receptor antagonist, PVR: pulmonary vascular resistance
Discussion:
Combination therapy is increasingly used in the management of pulmonary hypertension, particularly idiopathic PAH. There is increasing evidence that the earlier the implementation of aggressive dual therapy, the better is the prognosis and chances of improvement of functional status[
1,
7,
8,
9].
Some authors have highlighted the drug-drug interactions between the two classic members of combination therapy, namely Sildenafil and Bosentan. Both agents affect the serum levels of each other in a reversed fashion; it is thought that sildenafil decreases the metabolism of ERA, especially Bosentan via CYP3A4, in turn Bosentan reduces the serum level of Sildenafil by 50-60% via induction of CYP3A4 [
10].
Despite the latter pharmacokinetic evidence, no clinical trial to date has explored the effect of ERA+S vs. ERA+T on pulmonary invasive hemodynamics; highlighting a gap of literature that needs to be resolved.
Our literature search has depicted two retrospective studies only, where patients with pulmonary arterial hypertension, managed by different types of combination therapy were compared [
5,
6].
A meta-analysis of the retrieved results from Grunig and Sitbon et al reports, have showed a significantly lower mPAP in patients on ERA-T compared to ERA-S; this difference was less evident in terms of PVR with a P value 0f 0.056.
PVR is a static hemodynamic index based on Poiseuille's law and is calculated as (mPAP − PAWP)/CO (cardiac output). From this equation, we can conclude that PVR is not affected by changes in mPAP but also by an increase of CO. Pulmonary vasodilators improve forward flow by reducing afterload and manipulating hypoxic vasoconstriction[
11].
An interesting study by Farmakis and colleagues showed that CO contribution to PVR reduction is bound to the severity of initial PVR. The higher the initial mPAP, the more likely is to see a palpable effect of vasodilator therapy on CO, and subsequently on PVR[
12].
The effect of vasodilator therapy on CO is also dependent on the duration of therapy, requiring mostly longer duration to be achieved, compared to the immediate effect of vasodilators on the mPAP[
8,
9].
Failure to observe a frank statistical difference in PVR between the two treatment arms, might be attributed to a short duration of treatment, and also to the initial levels of mPAP.
A major limitation of this report is the absence of baseline hemodynamics in of the two studies included, meaning that the observed difference between the two regimens, might be due to a baseline difference in the mPAP before initiation of therapy.
Conclusion:
ERAs are substrates and induces of CYP3A4, their administration can reduce the bioavailability of Sildenafil, which is commonly used in conjunction with them in management of PAH; this interaction can be avoided by replacing tadalafil instead of sildenafil. This study goes in agreement with the pharmacokinetic facts, however the results are limited by the number of available reports and the limited outcome parameters in these reports.
More studies, particularly clinical trials, are needed to determine if there is an advantage of tadalafil over sildenafil, in combination with ERA.
Author Contributions
Conceptualization, AFA; Methodology, AFA, NS; software, AFA, NS; investigation, AFA, NS; resources, AFA, NS, data curation, AFA, NS; writing—original draft preparation, AFA, NS; writing—review and editing, AFA, NS; supervision, AFA; project administration, AFA; funding acquisition, (non-applicable). All authors have read and agreed to the published version of the manuscript.”
Institutional Review Board Statement
not applicable as this study is a hypothesis/Review article.
Informed Consent Statement
not applicable as this study is a viewpoint/editorial.
Data Availability Statement
All data is made available within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Acknowledgement
To researchers in developing countries who face the biased assessment of journals and the financial constraints of their economies.
The manuscript is submitted under Creative Commons Licensing CC-BY-NC-ND
List of abbreviations
| CO |
Cardiac output |
| ERA |
Endothelin receptor antagonist |
| mPAP |
mean pulmonary artery pressure |
| PAH |
Pulmonary arterial hypertension |
| PAWP |
Pulmonary artery wedge pressure |
| PVR |
Pulmonary vascular resistance |
References
- Buckley MS, Staib RL, Wicks LM (2013) Combination therapy in the management of pulmonary arterial hypertension. Int J Clin Pract 67:13–23. [CrossRef]
- Burks M, Stickel S, Galiè N (2018) Pulmonary Arterial Hypertension: Combination Therapy in Practice. Am J Cardiovasc Drugs 18:249–257. [CrossRef]
- Srinivas NR (2009) Substrate-specific pharmacokinetic interaction between endothelin receptor antagonists and phosphodiesterase-5 inhibitors – assembling the clues. Br J Clin Pharmacol 67:475–477. [CrossRef]
- Lee CH, Cook S, Lee JS, Han B (2016) Comparison of Two Meta-Analysis Methods: Inverse-Variance-Weighted Average and Weighted Sum of Z-Scores. Genomics Inform 14:173–180. [CrossRef]
- Grünig E, Ohnesorge J, Benjamin N, Burhenne J, Enderle Y, Egenlauf B, Fischer C, Harutyunova S, Huppertz A, Klose H, Haefeli WE (2017) Plasma drug concentrations in patients with pulmonary arterial hypertension on combination treatment. Respiration 94:26–37. [CrossRef]
- Sitbon O, Sattler C, Bertoletti L, Savale L, Cottin V, Jaïs X, De Groote P, Chaouat A, Chabannes C, Bergot E, Bouvaist H, Dauphin C, Bourdin A, Bauer F, Montani D, Humbert M, Simonneau G (2016) Initial dual oral combination therapy in pulmonary arterial hypertension. Eur Respir J 47:1727–1736. [CrossRef]
- Chin KM, Gaine SP, Gerges C, Jing Z-C, Mathai SC, Tamura Y, McLaughlin V V., Sitbon O (2024) Treatment algorithm for pulmonary arterial hypertension. Eur Respir J 64:2401325. [CrossRef]
- Baccelli A, Rinaldo R, Davies R, Lo Giudice F, Haji G, Vigo B, Mondoni M, Centanni S, Howard L (2023) Treatment-associated changes in cardiopulmonary exercise test variables: upfront combination vs monotherapy in pulmonary arterial hypertension. In: Pulmonary hypertension. European Respiratory Society, p PA1198.
- Fauvel C, Liu Y, Correa-Jaque P, Kanwar MK, Vizza CD, Lin S, Benza RL (2023) Do Patients With Low-Risk Pulmonary Arterial Hypertension Really Benefit From Upfront Combination Therapy? Chest 164:1518–1530. [CrossRef]
- Dai G, Tan W, Shen Y, Lin D, Xu R, Lin Q, Wei Z (2024) Differential inhibition of sildenafil and macitentan on saxagliptin metabolism. Toxicol Appl Pharmacol 486:116934. [CrossRef]
- Kovacs G, Bartolome S, Denton CP, Gatzoulis MA, Gu S, Khanna D, Badesch D, Montani D (2024) Definition, classification and diagnosis of pulmonary hypertension. Eur Respir J 64:2401324. [CrossRef]
- Farmakis IT, Baroutidou A, Patsiou V, Arvanitaki A, Doundoulakis I, Hobohm L, Zafeiropoulos S, Konstantinides S V., D’Alto M, Badagliacca R, Giannakoulas G (2024) Contribution of pressure and flow changes to resistance reduction after pulmonary arterial hypertension treatment: a meta-analysis of 3898 patients. ERJ Open Res 10:00706–02023. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).