1. Introduction
Although human immunodeficiency virus (HIV) infection is preventable, it still remains a challenge worldwide even in the era of antiretroviral therapy (ART), with a disease prevalence of 39.9 million affected persons [
1]. The virus attacks the immune system, probably due to the fact that chemokine receptors are also co-receptors for HIV entry into cells and can inhibit or enhance viral replication [
2]. This results in immune activation, and dysfunction or suppression of the immune system, with an increase in systemic inflammatory cytokine levels [
3].
Cytokines, which are dissolvable low molecular weight proteins produced by body cells, are mediators of the immune system, with a primary role of regulating inflammation in health and disease. Some of the cytokines that have shown direct correlation with diseases include Interleukin-6 (IL-6), C-reactive protein (CRP), Monocyte chemo-attractant protein-1 (MCP-1, also CCL2), Interleukin-18, and D-dimer. Some diseases associated with these cytokines include cardiovascular disease, diabetes, coronary artery disease and atherosclerosis [
4,
5,
6]. High expression of MCP-1 has also been reported in people with systemic and oral diseases including HIV and periodontal disease [
7,
8]. Though immune activation in HIV is not fully understood, one of the mechanisms by which immune activation is believed to occur, is when microbial products (in this case the HIV lentivirus) encased within macrophages/monocytes, cross the gut mucosa, enabling viral entry into systemic circulation. The microbial product is able to cross the gut mucosa because of depletion in gut CD4+ T lymphocytes within the gut-associated lymphoid tissue (GALT), the most abundant site of CD4+ T-cells in the body [
9,
10]. The entry of microbial products into systemic circulation, also known as microbial translocation, then results in release of proinflammatory cytokines and systemic immune activation, causing high systemic expression levels [
9,
11] .
ART therapy decreases systemic cytokine levels [
12], increases CD4+ T cell counts and lowers viral load [
3]. Despite the effectiveness of ART, the virus remains persistent in the cellular environment, with continuing persistent inflammation and immune activation (PIIA) [
13]. The underlying mechanism is still unclear but has been attributed to cytokine regulation [
14] and genetics [
12,
15,
16].
PIIA has also been correlated with non-infectious comorbid conditions among people with HIV (PWH), with inflammatory biomarkers/cytokine levels reportedly higher among PWH when compared to people without HIV [
9,
16,
17]. However, there is limited literature, comparing 2 groups of PWH: those with comorbid conditions (PWH +NCD) and those without (PWH -NCD)
PIIA is assessed by measuring cytokine levels in biological fluids like plasma, sweat and serum [
18,
19]. Cytokine levels can therefore be used to monitor the immune status of patients with chronic diseases, like cardiovascular disease, HIV, depression, hyperlipidemia, etc. [
18].
Most studies on inflammatory cytokine analysis for systemic diseases use either plasma or serum, or both fluids. However, for clinical and translational studies with cost constraints and multiple sample types available to test same analytes, it may become necessary to choose only one sample type/biologic fluid that gives the best results.
The objective of this study was to compare cytokine levels in serum and plasma of PWH on ART based on presence or absence of comorbid disorders (+NCD and -NCD respectively). The goal is to determine whether plasma or serum will be a preferred biological sample for determination of cytokine levels, and further explore the relationship with presence or absence of NCD.
2. Materials and Methods
This study was approved by the University of Pennsylvania Institutional Review Board (IRB). Patient informed consent was obtained, and the study was conducted according to the ethical principles and standards in accordance with the 1975 Declaration of Helsinki. Medical history, current laboratory study results including viral load and CD4+ T cell count obtained within 1 year of study visit, demographic information including biological sex, age and race were obtained from the first fourteen participants enrolled in an ongoing prospective longitudinal clinical and translational study titled ‘The Impact of Oral Health on Metabolism and Persistent Inflammation in HIV Patients on Antiretroviral Therapy (OHART) [
17].
Medical history for NCDs included in this analysis were cardiovascular diseases (including hypertension, coronary artery disease, irregular heartbeat, cardiomyopathy, ventricular tachycardia, myocardial infarction, ventricular fibrillation, atrial fibrillation, peripheral vascular diseases and supraventricular tachycardia), diabetes, psychiatric conditions, and hyperlipidemia. These NCDs were diagnosed by physicians and obtained from electronic medical records and are systemic outcomes the OHART study focuses on. Psychiatric conditions included depression and anxiety only. Participants were divided into two groups: 1) those that presented with at least one of the above NCDs (+NCD) and 2) those that did not have any NCDs (-NCD). Paired serum and plasma levels were obtained via venipuncture from each participant. Plasma and serum sample preprocessing was conducted by centrifuging samples at 1000g for 15mins at room temperature. Plasma samples were pre-processed within 30 minutes of collection while serum samples were pre-processed within 30-60 minutes. Aliquots of 100μl and 1000μl supernatants were stored at -80 ºC for batched processing [
17] and cytokine analysis.
Quantification of soluble immune mediators Interleukin-6 (IL-6), Interleukin-8 (IL-8), Interleukin-18 (IL-18), Monocyte Chemoattractant Protein-1 (MCP-1), and Tumor Necrosis Factor- alpha (TNF-α) were measured in both serum and plasma, with Luminex kit “Milliplex Human Cytokine/Chemokine/Growth Factor Panel A” (Millipore Sigma, USA), Cat. No. HCY-TA-60K-07, QC Cat. No. HCYTA-6060-2). Luminex assay protocol for Millipore Sigma, HCYTA-60K Rev. 12/21 was performed according to manufacturer’s recommendation using “FLEXMAP 3D” instrument and “Luminex® xPONENT® 4.2; Bio-Plex Manager™ Software 6.1”. Samples were assessed in duplicate 25 µl samples including kit-specific standards S1-S7 based on five-fold dilution. Absolute cytokine concentrations were quantified including standard deviation. Averages of each duplicate sample were used in analysis. Percent Intra-assay coefficient of variation (% CV) was acceptable at less than 20%, with 24 of the 28 samples being in this range. Four samples had % CV >20% (20.47%, 27.77%, 28.69%, and 79.71%), three of which were plasma samples.
Statistical Analysis
Clinical data was compared with absolute values of immune mediators using descriptive statistics. Continuous variables were summarized by mean and standard deviation, while dichotomous variables were described using count and percentage. Pairwise Pearson correlation was assessed between each cytokine and each participant in the +/- NCD groups and two-sided t-test was used to assess significance. Statistical significance was set at p < 0.05. All data analysis was performed with Excel v2410, (Build 18129.20158). Of all the cardiovascular diseases, only hypertension and coronary artery diseases were included in the final analysis, as the individual counts of the other CVDs were insignificant (mostly no counts).
3. Results
3.1. Participant Characteristics
Study participants consisted of 14 PWH either with NCDs (+NCD = 9) or without NCD (-NCD = 5). The average age was 56.6 years (range 45-65 years) in the +NCD group compared to 51.8 years (range 32-70 years) in the -NCD group (
Table 1). Average CD4 cell count was 857.5 cells/mm3 in the +NCD group and 602.6 cells/mm3 in the -NCD group (
Table 1). In addition, 9 out of the 14 participants were African Americans, of which 55.5% did not present with any comorbid condition. Highest viral load in the -NCD group was 464 copies/ml, while in the +NCD group was 85 copies/ml.
3.2. Distribution of Non-Communicable Diseases in PWH
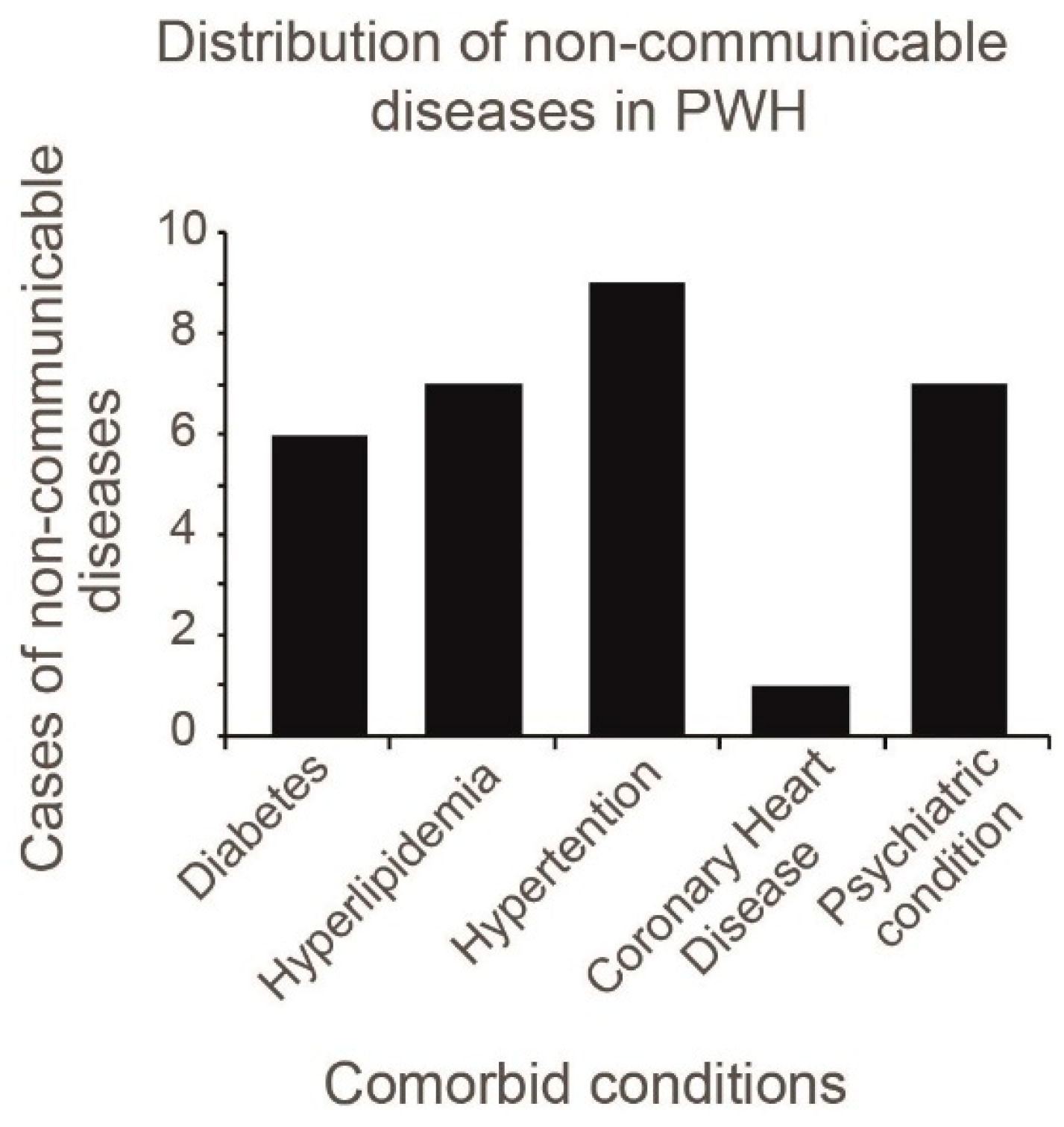
Based on the distribution of NCDs, hypertension was the most common (n=9) (
Figure 1). However, some PWH presented with more than one comorbid condition. One hundred percent of Caucasians enrolled in the study, presented with at least 1 +NCD.
3.3. Elevated MCP-1 and IL-18 Levels in Serum and Plasma of PWH
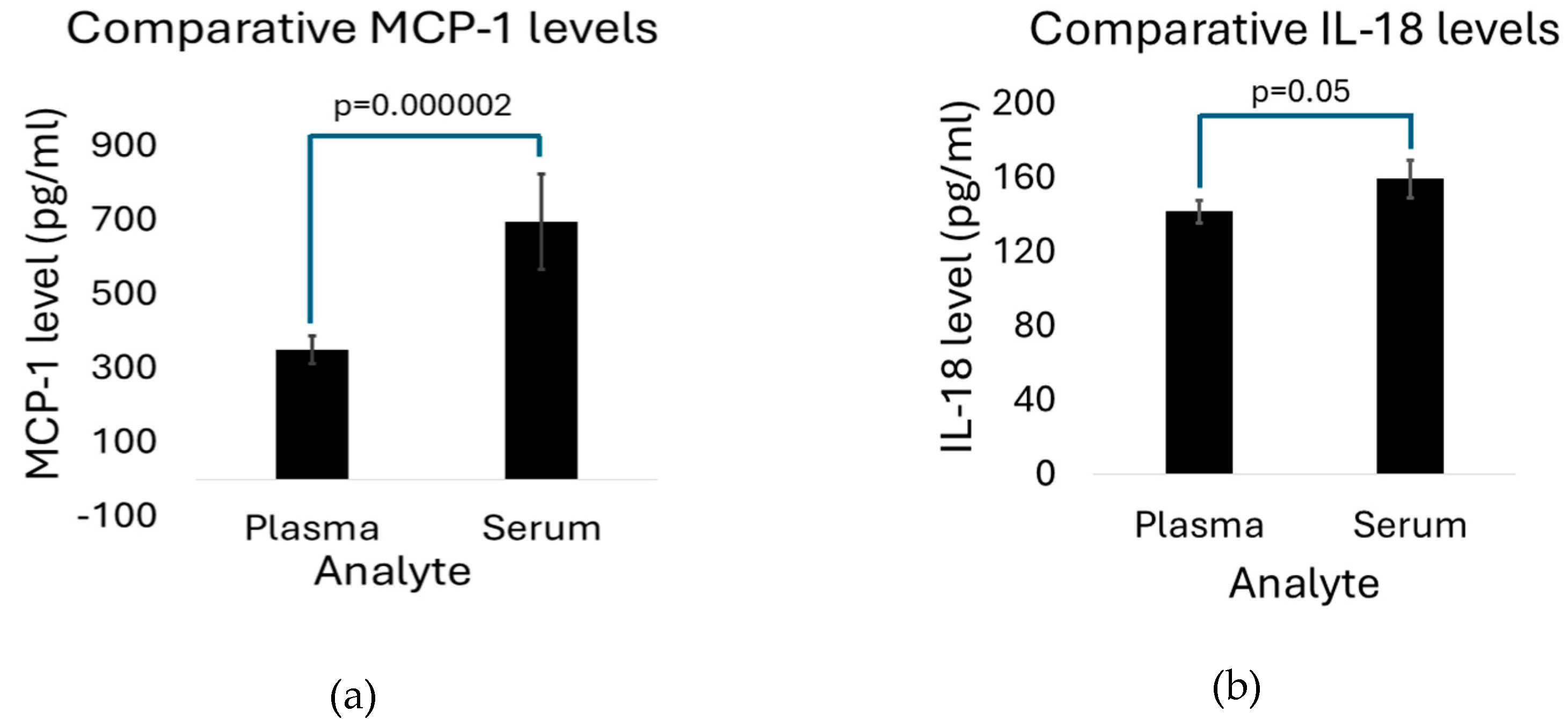
MCP-1 serum (694.60 pg/ml, SD 128.95) and plasma (349.87pg/ml (SD 37.91) expression levels were 4 to 188-fold and 2.5 to 140-fold higher than other analyzed cytokines (
Table 2). MCP-1 serum levels were also significantly higher in serum than in plasma (p= 0.000002) (
Figure 2a). IL-18 expression levels were also comparably high, though not as high as in MCP-1. IL-18 expression was also significantly higher in serum compared to plasma (159.33pg/ml SD 10.20 versus 141.81pg/ml SD 5.93; p=0.05) (
Figure 2b).
Expression levels of serum and plasma IL-6, IL-8 and TNF-α where relatively low (<40pg/ml) compared to MCP-1 and IL-18. In addition, serum levels of all the 3 cytokines and chemokine were higher in plasma, however, only IL-8 of the 3 analytes showed a significantly higher serum level (7.96 pg/ml, SD 0.49 versus 2.50pg/ml, SD 0.11 in plasma; p=0.000005) (Table2).
3.4. IL-6 Level in PWH with NCD Is Significantly Higher than in Those Without NCD
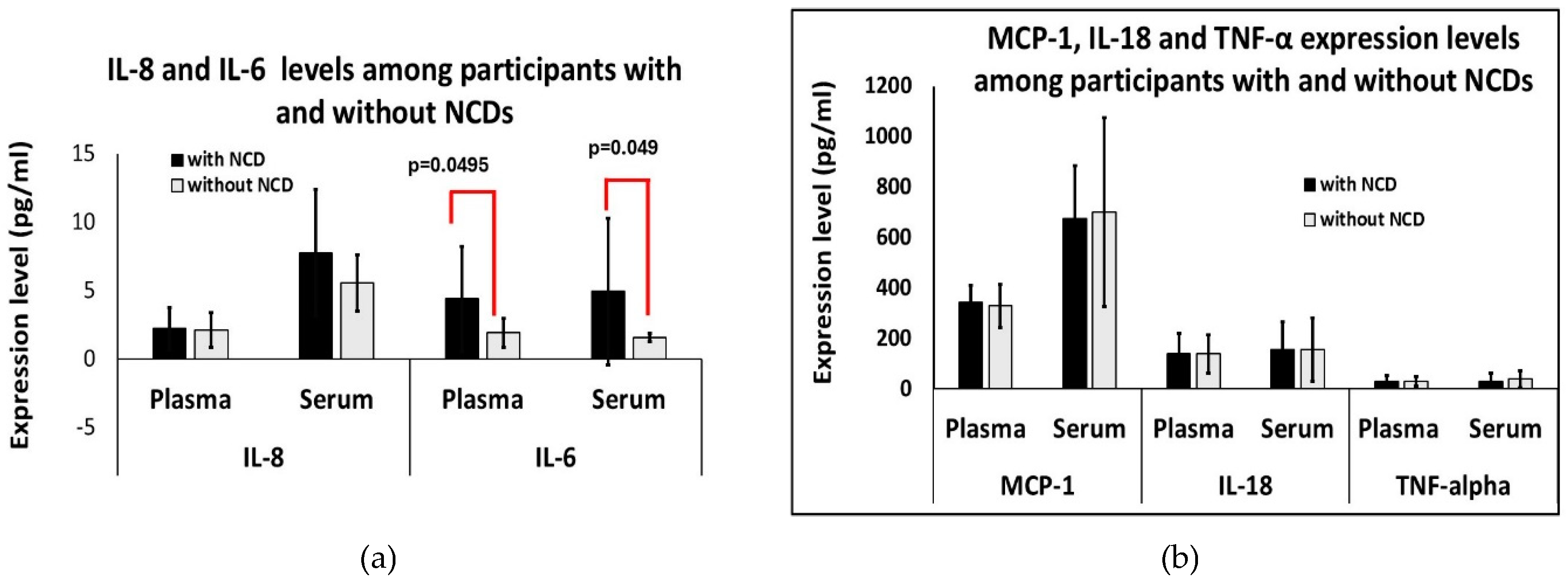
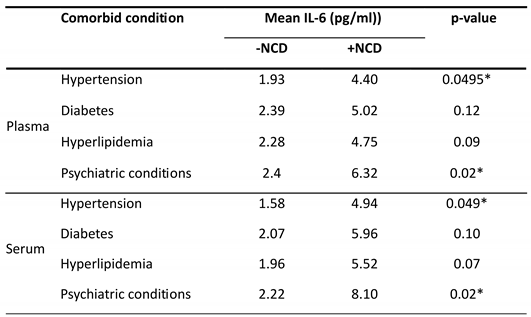
A significant difference was noted in IL-6 expression in the group of PWH with +NCD compared to -NCD group (p=0.0489 in serum and p=0.0495 in plasma) (
Figure 3A), with serum levels of 4.94pg/ml (+NCD)versus 1.58pg/ml (-NCD) and plasma levels of 4.40pg/ml (+NCD) versus 1.93pg/ml (-NCD). The pattern of higher IL-6 expression in each +NCD type considered was also noted when comparing each disease type to those without the specific disease (e.g. PWH with hypertension versus those without hypertension (
Table 3).
However, as noted in
Figure 3A and
Figure 3B, there was no significant difference between the expression levels of MCP-1, IL-18, TNF-α and IL-8 among those with and without NCD (+NCD and -NCD respectively).
4. Discussion
This study describes the pilot analysis of serum and plasma samples from PWH on ART with and without comorbid conditions. Th goal was to compare absolute concentration of inflammatory cytokines in serum and plasma of PWH on ART, to determine the more viable biological fluid for evaluating analytes of PIIA, as well as to compare cytokine concentration in those with and without NCD (+NCD and -NCD respectively). Our results showed that the choice of biological fluid was dependent on the analyte of interest. More remarkably, we noted elevated expression levels of MCP-1 in PWH, making MCP-1 (also known as CCL2) and IL-18 possible diagnostic and precision medicine intervention targets. IL-6 was also noted as a possible predictor of comorbidity in PWH on ART irrespective of whether serum or plasma is the analyte of choice.
The demographic profile of the participants aligned with that of Greater Philadelphia area residents, with majority of enrolled participants being males of African American decent. This is comparable to the 2021 data for PWH in Philadelphia, which shows that 63.7% of the population are of African American origin, and 72.2% were males [
20]. The age group trend among participants included on this study was also comparable with the population of PWH in Philadelphia with an average age of 54.6 years noted in our population, and majority of the population of patients with HIV in Philadelphia in the 45-59 years age group [
20].
When we compared the 2 study groups, categorized based on presence or absence of NCDs, we noted that average age was higher in the +NCD group. This is expected, as comorbidities tend to increase with age, and as PWH are living longer, a similar trend is expected [
21]. It is important to note that comorbid conditions tend to occur at an earlier age among PWH, when compared with age- matched counterparts without HIV [
22]. In addition, we noted that all 5 Caucasian PWH enrolled in our study had at least one comorbid condition, whereas only 44.4% of African Americans presented with NCD. This was surprising and not representative of what has been reported in literature [
23,
24]. Currently published evidence points to African Americans with HIV being disproportionately affected with comorbid conditions. These studies were conducted in Southeastern [
24] and Northeastern [
25] regions of the United States America. Based on the fact that these were old studies, it would be interesting to see if these trends in disparity have changed over time in the Northeastern USA or if this is restricted to the Philadelphia region only.
While majority of our cohorts were well controlled on ART based on an undetectable viral load, we noted a higher upper limit of viral load in the group of PWH without NCD (-NCD). This result supports the role of ART in increasing NCDs.
Results on +NCD cases in this pilot study also showed that hypertension was the most common +NCD among our population of PWH, followed by hyperlipidemia and psychiatric conditions. This corroborates findings in literature of the prevalence of hypertension among PWH [
26]. Also important to note is that of the psychiatric conditions, depression was the most common (n=6) in our study, which is validated by findings in literature [
27,
28].
Cytokine expression levels of paired plasma and serum were compared in each individual and across the fourteen individuals. With regards to sample collection and processing, a recent study by Liu et al reports that with use of EDTA tubes for plasma sample collection, cytokine levels are very similar to those obtained with serum [
18]. This was somewhat true for our study, where we noted no significant difference in analyte expression between serum and plasma samples for TNF-α and IL-6. However, MCP-1, IL-18 and IL-8, were all significantly elevated in serum relative to plasma. The results obtained from our study are suggestive of the fact that the choice of plasma or serum for evaluation of PIIA among PWH, is dependent on the analyte that is being considered.
IL-8, a proinflammatory cytokine, is also suggested as a marker of chronic inflammation among PWH on ART [
29]. However, relative to MCP-1 and IL-18, the expression level based on our study findings was relatively low.
The study by Liu et al (2021) [
18], also noted the importance of using EDTA tubes for plasma sample collection, as heparin and lithium heparin affect the concentration of the analytes. The study further emphasized the need for timely processing of plasma samples to obtain reliable results. In pre-processing samples for this pilot study, we ensured that EDTA tubes were used for all plasma sample collection and obtained plasma samples were processed within less than 30 minutes of sample collection, while serum samples were processed after at least 30 minutes but not more than an hour after collection.
Notably, there is an interaction between immune and coagulation systems and plasma contains coagulation factors. It is therefore important to consider a possible interaction between coagulation proteins and plasma when considering the body fluid type for cytokine analysis.
Our findings of elevated MCP-1 levels corroborate with reports of elevated CCL2 in PWH despite ART, with this chemokine closely associated with prominent inflammation and immune activation in this population [
19]. For this reason, it has been suggested that the MCP-1 receptor is targeted for HIV- therapeutics.
Elevated IL-18 levels have also been associated with HIV-infection. However, most reports have associated elevated IL-18 with anti-retroviral treatment failure or comorbid conditions, such as lipodystrophy in PWH [
20,
21,
22]. This does not seem to be the case in this study, as most of our participants had good viremia control, and IL-18 levels were similar in those with and without NCDs.
IL-6 is both a pro and anti-inflammatory cytokine, produced by CD4+ T-helper 2 cells [
30,
31], and is believed to activate immune response [
31,
32]. We noted higher expression levels of plasma and serum IL-6 in the +NCD group, with a high correlation noted between presence of NCDs (+NCD) and relatively higher expression of IL-6. This was especially significant for participants with hypertension and psychiatric conditions. Our study also noted a moderate correlation between serum IL-6 expression level and number of NCDs (ρ=0.63), alluding to the fact that IL-6 is a predictor of both presence and number of NCDs in PWH. This result can be corroborated with the findings of Borges et al in 2015, which reported a higher level of IL-6 not only in those with lower CD4 nadir and in PWH generally even those with good viremia control on HIV, but also in those with comorbid conditions including hypertension, hepatitis B and C, diabetes mellitus and tobacco use [
33].
Based on findings on
Table 1, CD4+ T cell count was higher in patients with +NCD, and the maximum HIV RNA viral load was also lower in this group. This suggests that PWH, with better control of their viral disease with higher CD4 and lower viral load are more likely to have NCDs. which is a likely pointer to the role of ART, in addition to the suspected role of PIIA in contributing to non-infectious comorbid conditions in HIV.
5. Conclusions
The findings on this pilot study suggest that the choice of plasma or serum for evaluation of PIIA among PWH, is dependent on the analyte being evaluated. We also observed that MCP-1 especially, and IL-18 are potential diagnostic markers for HIV even in PWH well controlled on ART. Finally, IL-6 may be used as possible predictors of comorbid conditions among PWH, but further studies using larger number of patients is needed to confirm these findings. It will be interesting to evaluate the role of cytokines in common oral diseases noted in PWH, in the ART era. In addition, compare blood and saliva cytokine levels, and correlate findings with oral disease manifestations like periodontal disease and changes in quality of saliva among PWH on ART.
The goal of future research is focused on evaluating the oral-systemic disease link. Since oral diseases noted in PWH have changed since the advent of ART, with dental caries and human papilloma virus seemingly more prevalent, we will focus on exploring the role of local and systemic inflammation on the pathogenesis of these oral diseases in PWH who are well controlled on ART. We are hopeful that in the process we will discover the mechanisms underlying the development of oral and hopefully systemic diseases conditions in this patient population. This will help guide the development of preventive strategies, as well as therapeutic targets that will improve oral health and oral health quality of life, as well as systemic health, in PWH on ART.
Author Contributions
Conceptualization, T.O.; methodology, T.O and S.O.; software, D.S.; validation, T.O and S.O.; formal analysis, D.S.; investigation, A.K and L.V.; resources, T.O.; data curation, L.V,A. K.; writing—original draft preparation, T.O, S.O.; writing—review and editing, T.O, A.K, L.V, D.S, S.O.; visualization, T.O, S.O.; supervision, T.O.; project administration, T.O; funding acquisition, T.O, S.O. All authors have read and agreed to the published version of the manuscript.”
Funding
This research was funded by the National Institute of Dental and Craniofacial Research/National Institute of Health/DHHS, grant number R01-DE029648-01 and “The APC was funded by NIDCR”.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of The University of Pennsylvania (protocol code/#: 834892 and date of approval:13th of May, 2020.
Informed Consent Statement
Written and signed informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
We acknowledge the support of the OHART study team.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| HIV |
Human Immunodeficiency Virus |
| PWH |
Persons with HIV |
| PIIA |
Persistent Inflammation and Immune Activation |
| NCD |
Non-infectious comorbid disease |
| +NCD |
Presence of non-infectious comorbid diseases |
| -NCD |
Absence if non-infectious comorbid diseases |
| ART |
Antiretroviral therapy |
| OHART |
Oral Health on Metabolism and Persistent Inflammation in HIV Patients on Antiretroviral Therapy |
References
- Organization, W.H. HIV and AIDS. Newsroom factsheet detail 2023 [cited 2024 2/27/2024]; July 13 2023: [Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
- Covino, D.A. Sabbatucci, and L. Fantuzzi, The ccl2/ccr2 axis in the pathogenesis of hiv-1 infection: A new cellular target for therapy? Current Drug Targets, 2016. 17(1): p. 76-110.
- Okay, G. , et al., The effect of antiretroviral therapy on IL-6, IL-1β, TNF-α, IFN-γ levels and their relationship with HIV-RNA and CD4+ T cells in HIV patients. Current HIV Research, 2020. 18(5): p. 354-361.
- Chukwuanukwu, R.C.; Nwosu, N.B.; Ifeanyichukwu, M.O.; Nsonwu-Anyanwu, A.C.; Manafa, P.O. Evaluation of some immune and inflammatory responses in diabetes and HIV co-morbidity. Afr. Heal. Sci. 2023, 23, 120–128. [Google Scholar] [CrossRef]
- Niu, J.; Kolattukudy, P.E. Role of MCP-1 in cardiovascular disease: molecular mechanisms and clinical implications. Clin. Sci. 2009, 117, 95–109. [Google Scholar] [CrossRef] [PubMed]
- O'Connor, T. Borsig, and M. Heikenwalder, CCL2-CCR2 Signaling in Disease Pathogenesis. Endocr Metab Immune Disord Drug Targets, 2015. 15(2): p. 105-18.
- Pradeep, A.; Daisy, H.; Hadge, P. Serum levels of monocyte chemoattractant protein-1 in periodontal health and disease. Cytokine 2009, 47, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Hanazawa, S.; Kawata, Y.; Takeshita, A.; Kumada, H.; Okithu, M.; Tanaka, S.; Yamamoto, Y.; Masuda, T.; Umemoto, T.; Kitano, S. Expression of monocyte chemoattractant protein 1 (MCP-1) in adult periodontal disease: increased monocyte chemotactic activity in crevicular fluids and induction of MCP-1 expression in gingival tissues. Infect. Immun. 1993, 61, 5219–5224. [Google Scholar] [CrossRef] [PubMed]
- Ashuro, A.A.; Zhang, S.; Wang, T.; Chu, Q.; Fu, Y.; Fan, Y.; Ye, D. The effect of protease inhibitors-based antiretroviral therapy on serum/plasma interleukin-6 levels among PLHIV: a systematic review and meta-analysis. J. Med Virol. 2022, 94, 4669–4676. [Google Scholar] [CrossRef] [PubMed]
- Vijayan, K.K.V.; Karthigeyan, K.P.; Tripathi, S.P.; Hanna, L.E. Pathophysiology of CD4+ T-Cell Depletion in HIV-1 and HIV-2 Infections. Front. Immunol. 2017, 8, 580. [Google Scholar] [CrossRef] [PubMed]
- Leal, V.N.C.; Reis, E.C.; Pontillo, A. Inflammasome in HIV infection: Lights and shadows. Mol. Immunol. 2020, 118, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Baker, J.V.; Sharma, S.; Grund, B.; Rupert, A.; A Metcalf, J.; Schechter, M.; Munderi, P.; Aho, I.; Emery, S.; Babiker, A.; et al. Systemic Inflammation, Coagulation, and Clinical Risk in the START Trial. Open Forum Infect. Dis. 2017, 4, ofx262. [Google Scholar] [CrossRef] [PubMed]
- Grozdeva, R.; Ivanov, D.; Strashimirov, D.; Kapincheva, N.; Yordanova, R.; Mihailova, S.; Georgieva, A.; Alexiev, I.; Grigorova, L.; Partsuneva, A.; et al. Relationship between Modern ART Regimens and Immunosenescence Markers in Patients with Chronic HIV Infection. Viruses 2024, 16, 1205. [Google Scholar] [CrossRef]
- Vandergeeten, C.; Fromentin, R.; Chomont, N. The role of cytokines in the establishment, persistence and eradication of the HIV reservoir. Cytokine Growth Factor Rev. 2012, 23, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Mu, W.; Patankar, V.; Kitchen, S.; Zhen, A. Examining Chronic Inflammation, Immune Metabolism, and T Cell Dysfunction in HIV Infection. Viruses 2024, 16, 219. [Google Scholar] [CrossRef]
- Peterson, T.E.; Baker, J.V. Assessing inflammation and its role in comorbidities among persons living with HIV. Curr. Opin. Infect. Dis. 2019, 32, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Omolehinwa, T.T.; Akintoye, S.O.; Gabinskiy, M.; Re, V.L.; Mupparapu, M.; Urbina, R.; Schaubel, D.E.; Corby, P.M. Oral health outcomes in an HIV cohort with comorbidities- implementation roadmap for a longitudinal prospective observational study. BMC Oral Heal. 2023, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Chu, D.; Kalantar-Zadeh, K.; George, J.; Young, H.A.; Liu, G. Cytokines: From Clinical Significance to Quantification. Adv. Sci. 2021, 8, 2004433. [Google Scholar] [CrossRef]
- Duque, G.A.; Descoteaux, A. Macrophage Cytokines: Involvement in Immunity and Infectious Diseases. Front. Immunol. 2014, 5, 491. [Google Scholar] [CrossRef]
- AIDSVu, Local Data Philadelphia, E. University, Editor. 2024: AIDSVu is presented by Emory University’s Rollins School of Public Health in partnership with Gilead Sciences, Inc. and the Center for AIDS Research at Emory University (CFAR).
- Paudel, M.; Prajapati, G.; Buysman, E.K.; Goswami, S.; Mao, J.; McNiff, K.; Kumar, P. Comorbidity and comedication burden among people living with HIV in the United States. Curr. Med Res. Opin. 2022, 38, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Maciel, R.A.; Klück, H.M.; Durand, M.; Sprinz, E. Comorbidity is more common and occurs earlier in persons living with HIV than in HIV-uninfected matched controls, aged 50 years and older: A cross-sectional study. Int. J. Infect. Dis. 2018, 70, 30–35. [Google Scholar] [CrossRef]
- Muiruri, C.; Longenecker, C.T.; Meissner, E.G.; Okeke, N.L.; Pettit, A.C.; Thomas, K.; Velazquez, E.; Bloomfield, G.S. Prevention of cardiovascular disease for historically marginalized racial and ethnic groups living with HIV: A narrative review of the literature. Prog. Cardiovasc. Dis. 2020, 63, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Burkholder, G.A.; Tamhane, A.R.; Safford, M.M.; Muntner, P.M.; Willig, A.L.; Willig, J.H.; Raper, J.L.; Saag, M.S.; Mugavero, M.J. Racial disparities in the prevalence and control of hypertension among a cohort of HIV-infected patients in the southeastern United States. PLOS ONE 2018, 13, e0194940. [Google Scholar] [CrossRef]
- Wong, C.; Gange, S.J.; Buchacz, K.; Moore, R.D.; Justice, A.C.; Horberg, M.A.; Gill, M.J.; Koethe, J.R.; Rebeiro, P.F.; Silverberg, M.J.; et al. First Occurrence of Diabetes, Chronic Kidney Disease, and Hypertension Among North American HIV-Infected Adults, 2000–2013. Clin. Infect. Dis. 2017, 64, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Todowede, O.O.; Mianda, S.Z.; Sartorius, B. Prevalence of metabolic syndrome among HIV-positive and HIV-negative populations in sub-Saharan Africa—a systematic review and meta-analysis. Syst. Rev. 2019, 8, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Huang, Y.; Peng, J.; Tang, R.; Luo, B.; Xia, Z. Association between depression and HIV infection vulnerable populations in United States adults: a cross-sectional analysis of NHANES from 1999 to 2018. Front. Public Heal. 2023, 11, 1146318. [Google Scholar] [CrossRef] [PubMed]
- Fuenmayor, A.; Cournos, F. Addressing depressive disorders among people with HIV. . 2022, 30, 454–463. [Google Scholar]
- Ellwanger, J.H.; Valverde-Villegas, J.M.; Kaminski, V.d.L.; de Medeiros, R.M.; Almeida, S.E.d.M.; Santos, B.R.; de Melo, M.G.; Hackenhaar, F.S.; Chies, J.A.B. Increased IL-8 levels in HIV-infected individuals who initiated ART with CD4+ T cell counts <350 cells/mm3 – A potential hallmark of chronic inflammation. Microbes Infect. 2020, 22, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Rose-John, S. Interleukin-6 signalling in health and disease. F1000Research 2020, 9, 1013. [Google Scholar] [CrossRef] [PubMed]
- Scheller, J.; Chalaris, A.; Schmidt-Arras, D.; Rose-John, S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim. Biophys. Acta 2011, 1813, 878–888. [Google Scholar] [CrossRef] [PubMed]
- Aliyu, M.; Zohora, F.T.; Anka, A.U.; Ali, K.; Maleknia, S.; Saffarioun, M.; Azizi, G. Interleukin-6 cytokine: An overview of the immune regulation, immune dysregulation, and therapeutic approach. Int. Immunopharmacol. 2022, 111, 109130. [Google Scholar] [CrossRef] [PubMed]
- Borges. H.; O'Connor, J.L.; Phillips, A.N.; Rönsholt, F.F.; Pett, S.; Vjecha, M.J.; French, M.A.; Lundgren, J.D. Factors Associated With Plasma IL-6 Levels During HIV Infection. J. Infect. Dis. 2015, 212, 585–595. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).